Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Self-Administered Questionnaire
2.2. Setting
- “Do you consider yourself an advocate or opponent of vaccination?”
- “Have you been vaccinated within the last three years?”
- “Are you vaccinated against seasonal influenza?”
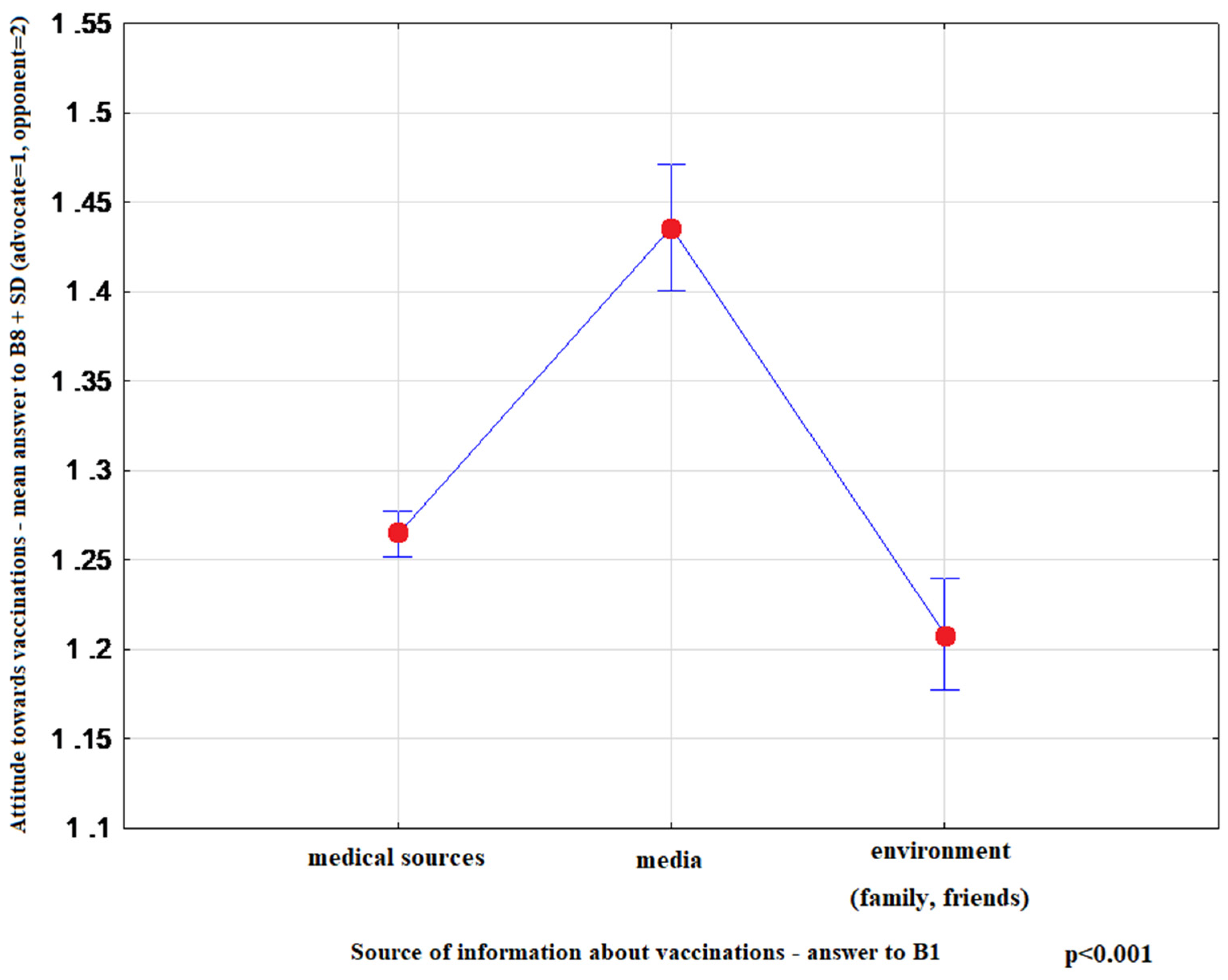
- “Please indicate one source of information about vaccinations that you find most convincing” (1)-medical sources (doctor, nurse, pharmacist) (2)-media (press, radio, television, Internet) (3)-environment (family, friends)
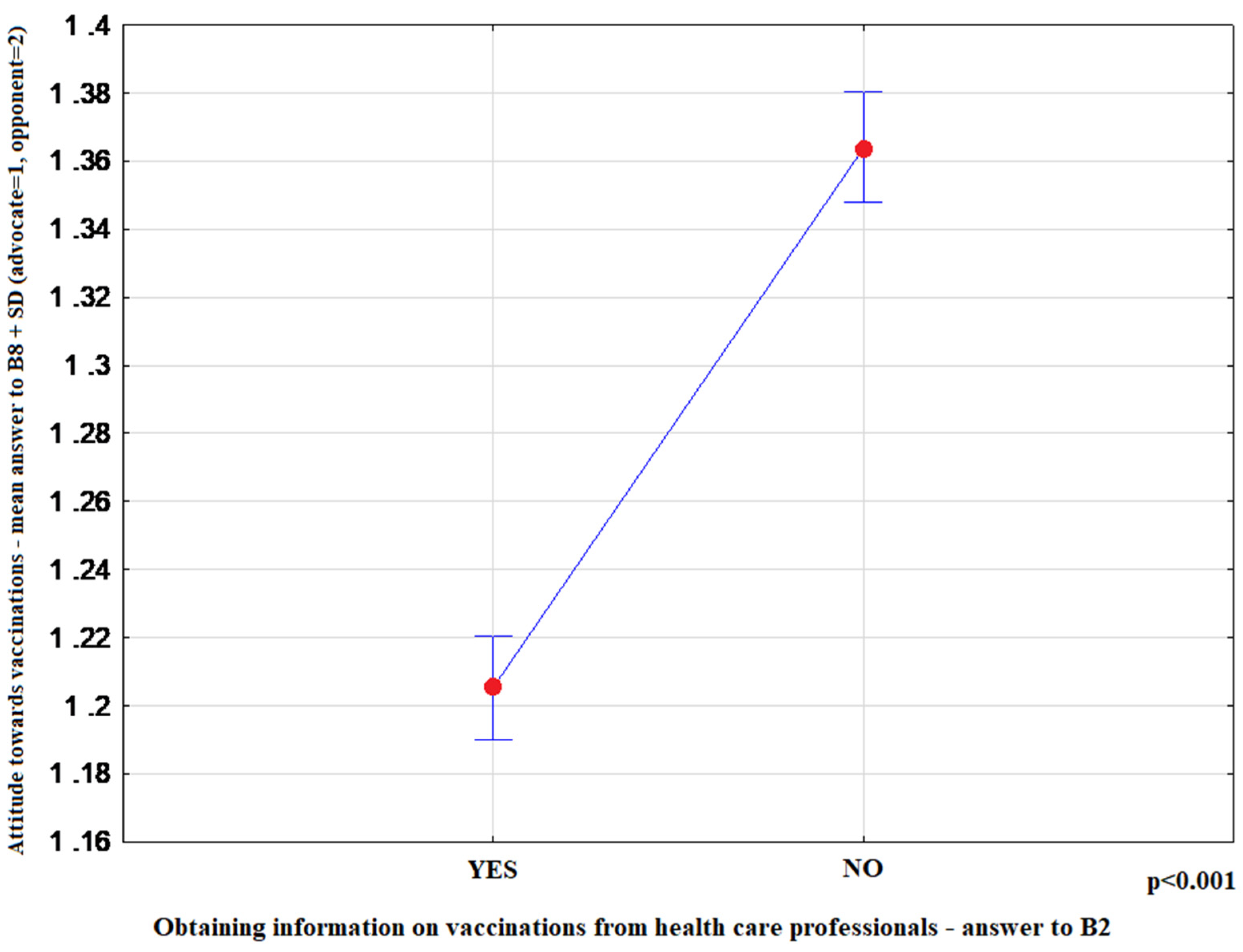
- “Did you obtain information on vaccination from healthcare professionals during visits to primary care physicians (PCP) or specialist outpatient clinic?”: (1)-Yes, (2)-no.
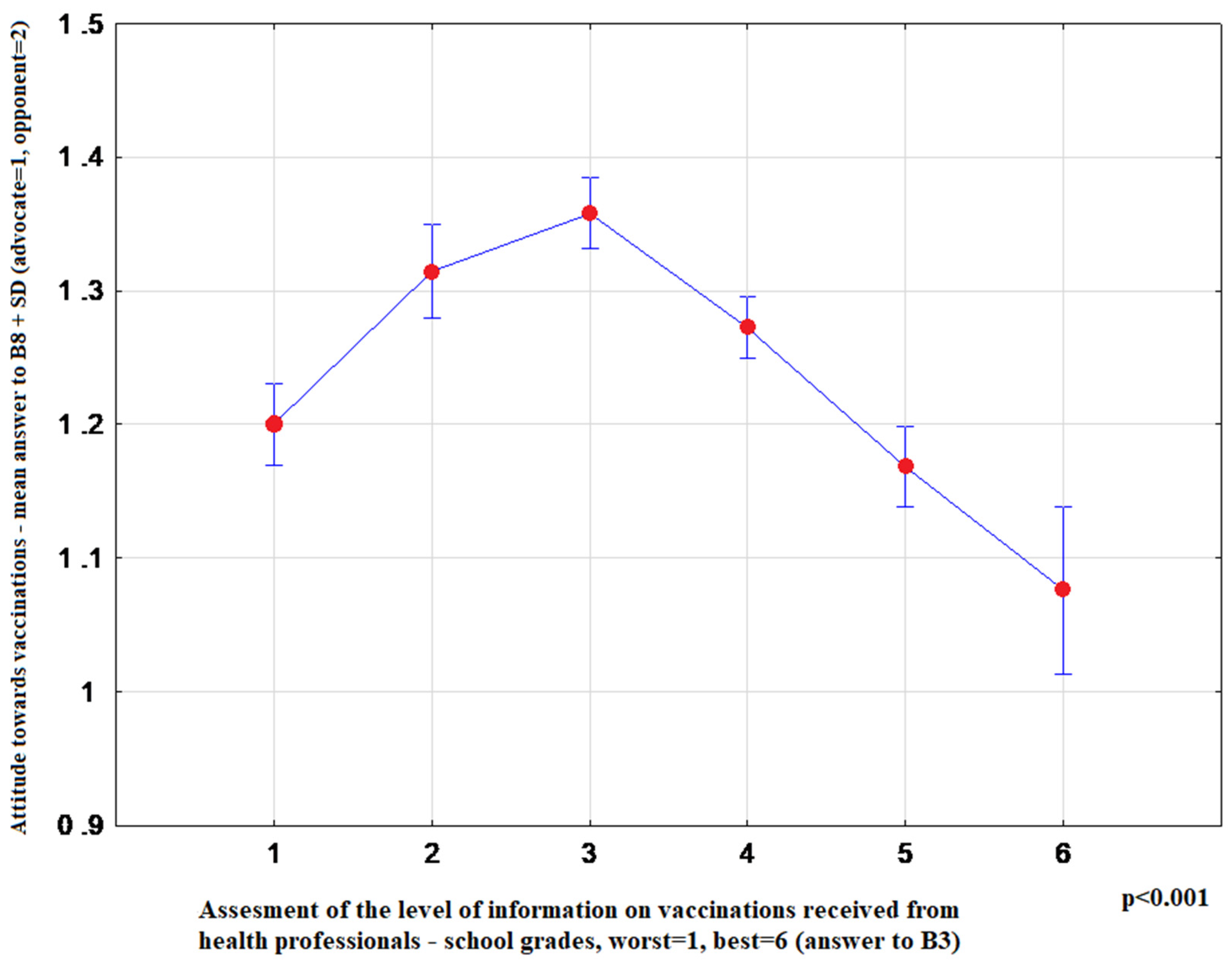
- “Using the school grade system, assess the level of vaccination information provided by health professionals” (1 worst–6 best)
- “What was the most important source of negative opinions about vaccinations?”: (1)-medical sources, (2)-media, (3)-environment
- “What opinion about vaccination was provided by health professionals?”: (1)-fully positive, (2)-questioning the validity of certain vaccinations, (3)-strongly negating the purposefulness of vaccinations
- The following questions were used to assess the level of knowledge of respondents about vaccinations:
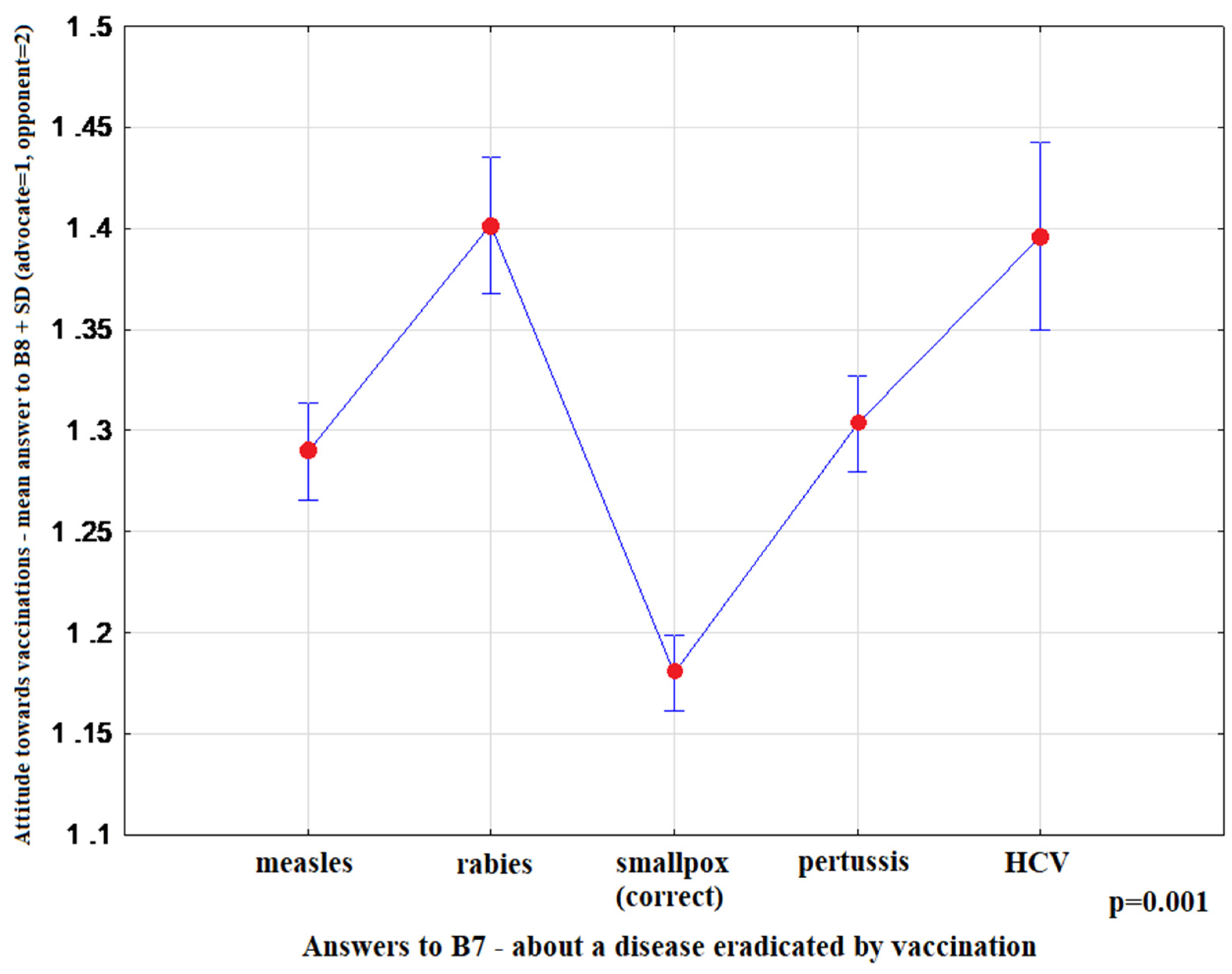
- “Which of the infectious diseases has been completely eliminated by vaccination?” (1)-measles, (2)-rabies, (3)-smallpox, (4)-whooping cough, (5)-hepatitis C
- “The statement that “vaccines cause autism” is:” (1)-true, (2)-false
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Data
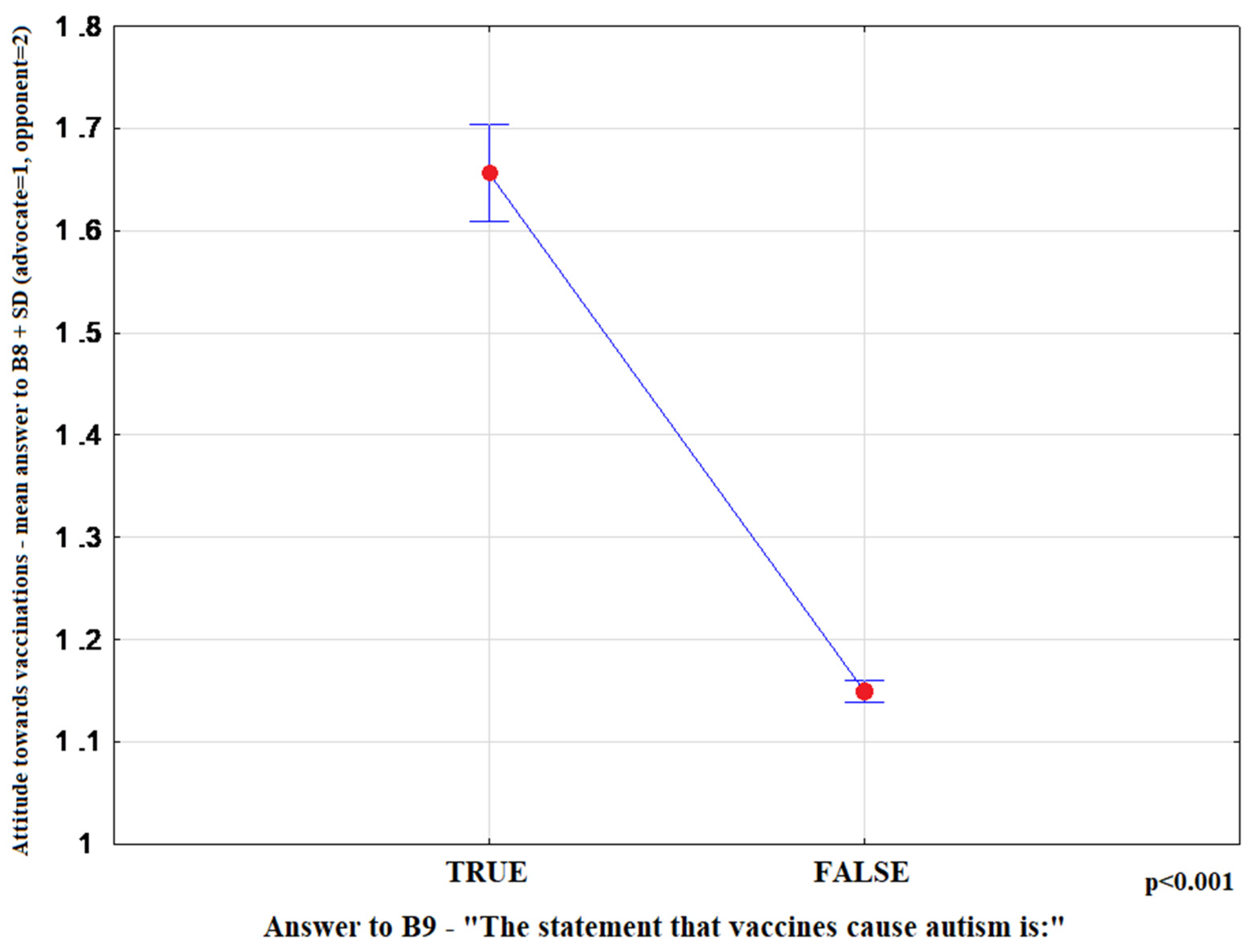
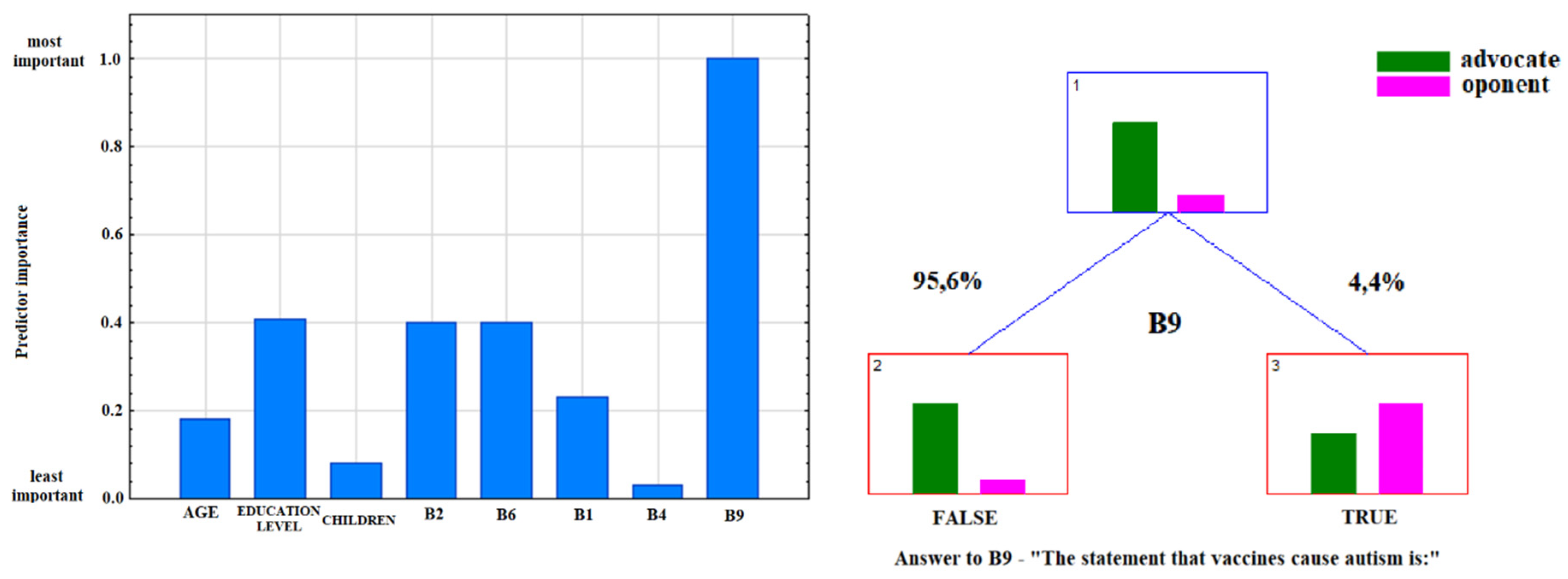
3.2. Analysis of the Answers to the Question: “Do You Consider Yourself An Advocate or Opponent of Vaccination?”
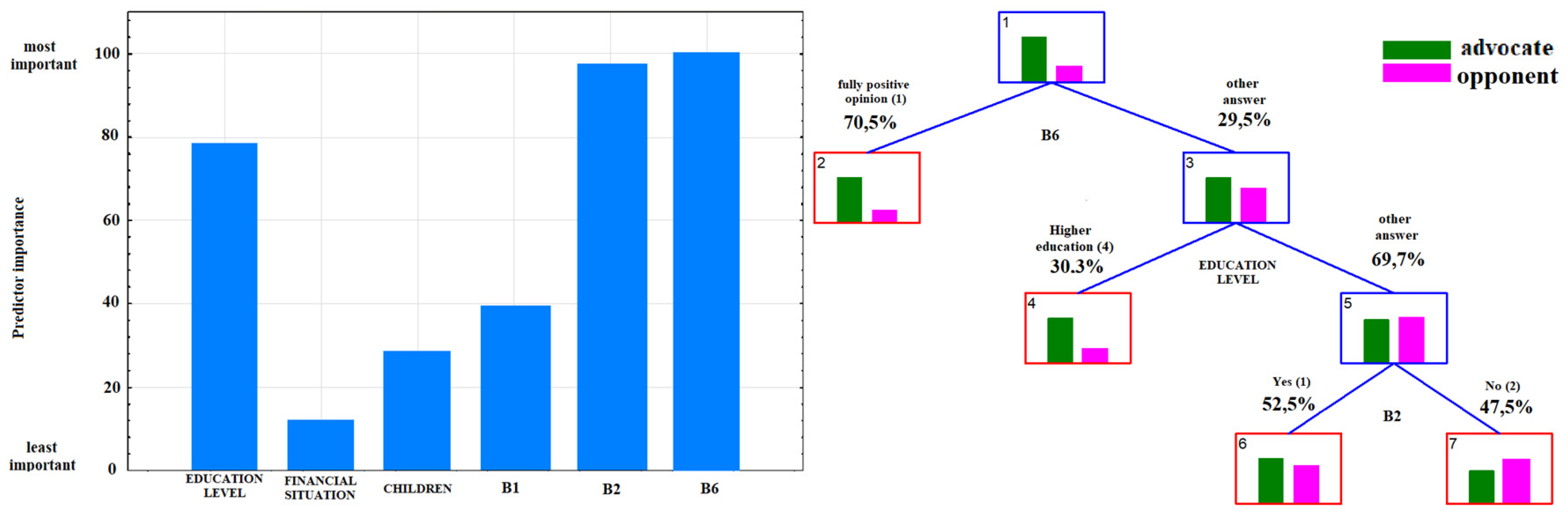
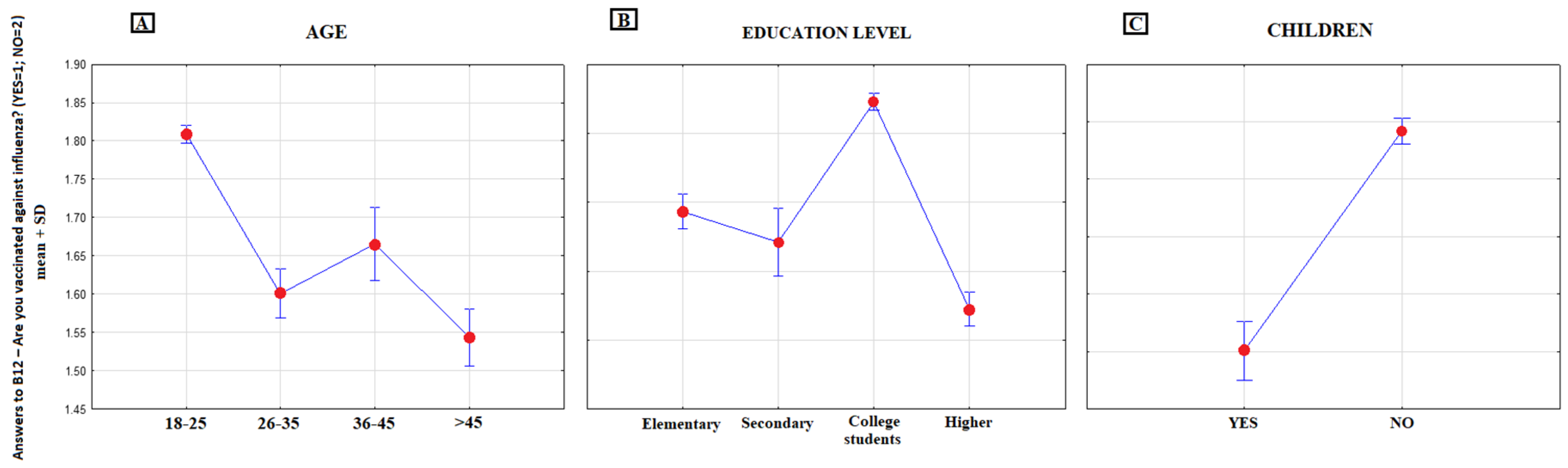
3.3. Analysis of the Answer to the Question: “Are you Vaccinated Against Seasonal Influenza?”
4. Discussion
4.1. Advocates and Potential Opponents of Vaccination in the Study Population
4.2. Influenza Vaccinations
4.3. Knowledge on Vaccines and Their Public Perception
4.4. Local Situation in Poland
4.5. Study Limitations
5. Conclusions
Practical Implications and Future Research
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention Ten Great Public Health Achievements—United States, 1900–1999. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm (accessed on 14 April 2020).
- Kempe, A.; Daley, M.F.; McCauley, M.M.; Crane, L.A.; Suh, C.A.; Kennedy, A.M.; Basket, M.M.; Stokley, S.K.; Dong, F.; Babbel, C.I.; et al. Prevalence of Parental Concerns About Childhood Vaccines. Am. J. Prev. Med. 2011, 40, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.M.; St. Sauver, J.L.; Finney Rutten, L.J. Vaccine hesitancy. Mayo Clin. Proc. 2015, 90, 1562–1568. [Google Scholar] [CrossRef] [PubMed]
- Kestenbaum, L.A.; Feemster, K.A. Identifying and addressing vaccine hesitancy. Pediatr. Ann. 2015, 44, e71–e75. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Charron, J.; Gautier, A.; Jestin, C. Influence of information sources on vaccine hesitancy and practices. Médecine Mal. Infect. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, C.K.; Patel, J.; Zhan, X. Trend of influenza vaccine Facebook posts in last 4 years: A content analysis. Am. J. Infect. Control 2020, 48, 361–367. [Google Scholar] [CrossRef]
- Boyle, J.; Berman, L.; Nowak, G.J.; Iachan, R.; Middleton, D.; Deng, Y. An assessment of parents’ childhood immunization beliefs, intentions, and behaviors using a smartphone panel. Vaccine 2020, 38, 2416–2423. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; Nickels, E.; Jeram, S.; Schuster, M. Mapping vaccine hesitancy-Country-specific characteristics of a global phenomenon. Vaccine 2014, 32, 6649–6654. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; et al. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Smith, T.C. Vaccine Rejection and Hesitancy: A Review and Call to Action. Open Forum Infect. Dis. 2017, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Bettinger, J.; Fisher, W.; Naus, M.; Mahmud, S.; Hilderman, T. Vaccine acceptance, hesitancy and refusal in Canada: Challenges and potential approaches. Can. Commun. Dis. Rep. 2016, 42, 246–251. [Google Scholar] [CrossRef]
- Nowicka, P.M.; Izdebski, R.; Kitowska, W.; Janiec, J.; Radziszewski, F.; Henszel, Ł. Review of measles-related events recorded by the National IHR Focal Point in Poland in the years 2016–2018. Przegl. Epidemiol. 2019, 73, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Arede, M.; Bravo-Araya, M.; Bouchard, É.; Gill, G.S.; Plajer, V.; Shehraj, A.; Shuaib, Y.A. Combating vaccine hesitancy: Teaching the next generation to navigate through the post truth era. Front. Public Heal. 2019, 6, 1–6. [Google Scholar] [CrossRef]
- Kowalska, M.; Gajda, M.; Barański, K.; Braczkowska, B. Sources of parental knowledge about the safety of vaccinations in Poland. Health Promot. Int. 2019, 34, 1191–1199. [Google Scholar] [CrossRef]
- Augustynowicz, A.; Wrześniewska-Wal, I. Legal aspects of compulsory immunization of children. Pediatr. Pol. 2013, 88, 120–126. [Google Scholar] [CrossRef][Green Version]
- Główny Inspektor Sanitarny do RPO: 43 tys. osób bez obowiązkowych szczepień. Available online: https://www.rpo.gov.pl/pl/content/GIS-do-RPO-43-tys.-osob-odmawia-obowiazkowych-szczepien (accessed on 5 June 2020).
- CBOS (Centrum Badania Opinii Społecznej) Polacy o obowiązku szczepienia dzieci. Available online: https://www.cbos.pl/SPISKOM.POL/2017/K_100_17.PDF (accessed on 5 June 2020).
- Facciolà, A.; Visalli, G.; Orlando, A.; Bertuccio, M.P.; Spataro, P.; Squeri, R.; Picerno, I.; Di Pietro, A. Vaccine hesitancy: An overview on parents’ opinions about vaccination and possible reasons of vaccine refusal. J. Public health Res. 2019, 8, 30–33. [Google Scholar] [CrossRef]
- Gust, D.; Woodruff, R.; Kennedy, A.; Brown, C.; Sheedy, K.; Hibbs, B. Parental perceptions surrounding risks and benefits of immunization. Semin. Pediatr. Infect. Dis. 2003, 14, 207–212. [Google Scholar] [CrossRef]
- Shui, I.M.; Weintraub, E.S.; Gust, D.A. Parents Concerned About Vaccine Safety. Am. J. Prev. Med. 2006, 31, 244–251. [Google Scholar] [CrossRef]
- Kennedy, A.M.; Brown, C.J.; Gust, D.A. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005, 120, 252–258. [Google Scholar] [CrossRef]
- Shen, S.C.; Dubey, V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can. Fam. Phys. 2019, 65, 175–181. [Google Scholar] [PubMed]
- Berry, N.J.; Danchin, M.; Trevena, L.; Witteman, H.O.; Kinnersley, P.; Snelling, T.; Robinson, P.; Leask, J. Sharing knowledge about immunisation (SKAI): An exploration of parents’ communication needs to inform development of a clinical communication support intervention. Vaccine 2018, 36, 6480–6490. [Google Scholar] [CrossRef] [PubMed]
- Gowda, C.; Schaffer, S.E.; Kopec, K.; Markel, A.; Dempsey, A.F. A pilot study on the effects of individually tailored education for MMR vaccine-hesitant parents on MMR vaccination intention. Hum. Vaccin. Immunother. 2013, 9, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Hviid, A.; Hansen, J.V.; Frisch, M.; Melbye, M. Measles, Mumps, Rubella Vaccination and Autism. Ann. Intern. Med. 2019, 170, 513. [Google Scholar] [CrossRef] [PubMed]
- Smeeth, L.; Cook, C.; Fombonne, E.; Heavey, L.; Rodrigues, L.C.; Smith, P.G.; Hall, A.J. MMR vaccination and pervasive developmental disorders: A case-control study. Lancet 2004, 364, 963–969. [Google Scholar] [CrossRef]
- Taylor, L.E.; Swerdfeger, A.L.; Eslick, G.D. Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine 2014, 32, 3623–3629. [Google Scholar] [CrossRef]
- Marotta, C.; Raia, D.D.; Ventura, G.; Casuccio, N.; Dieli, F.; D’Angelo, C.; Restivo, V.; Costantino, C.; Vitale, F.; Casuccio, A. Improvement in vaccination knowledge among health students following an integrated extra curricular intervention, an explorative study in the University of Palermo. J. Prev. Med. Hyg. 2017, 58, E93–E98. [Google Scholar] [CrossRef]
- Mizuta, A.H.; De Menezes Succi, G.; Montalli, V.A.M.; De Menezes Succi, R.C. Perceptions on the importance of vaccination and vaccine refusal in a medical school. Rev. Paul. Pediatr. 2019, 37, 34–40. [Google Scholar] [CrossRef]
- Bonaccorsi, G.; Santomauro, F.; Porchia, B.R.; Niccolai, G.; Pellegrino, E.; Bonanni, P.; Lorini, C. Beliefs and opinions of health care workers and students regarding influenza and influenza vaccination in Tuscany, Central Italy. Vaccines 2015, 3, 137–147. [Google Scholar] [CrossRef]
- Mitilian, E.; Malli, F.; Verger, P. Image of the new vaccination obligation through the media. Vaccine 2020, 38, 498–511. [Google Scholar] [CrossRef]
- Donzelli, G.; Palomba, G.; Federigi, I.; Aquino, F.; Cioni, L.; Verani, M.; Carducci, A.; Lopalco, P. Misinformation on vaccination: A quantitative analysis of YouTube videos. Hum. Vaccines Immunother. 2018, 14, 1654–1659. [Google Scholar] [CrossRef] [PubMed]
- Hussain, H.; Omer, S.B.; Manganello, J.A.; Kromm, E.E.; Carter, T.C.; Kan, L.; Stokley, S.; Halsey, N.A.; Salmon, D.A. Immunization safety in US print media, 1995–2005. Pediatrics 2011, 127. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.; LaVail, K.; Nowak, G.; Basket, M.; Landry, S. Confidence About Vaccines in The United States: Understanding Parents’ Perceptions. Health Aff. 2011, 30, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.; Chapman, S.; Leask, J. Antivaccination activists on the world wide web. Arch. Dis. Child. 2002, 87, 22–25. [Google Scholar] [CrossRef]
- Gowda, C.; Dempsey, A.F. The rise (and fall?) of parental vaccine hesitancy. Hum. Vaccines Immunother. 2013, 9, 1755–1762. [Google Scholar] [CrossRef]
- Stager, M. News & Views: Using Social Media as a Healthcare Provider—What Role Do You Play? Available online: https://www.chop.edu/news/news-views-using-social-media-healthcare-provider-what-role-do-you-play (accessed on 5 June 2020).
- Vivion, M.; Hennequin, C.; Verger, P.; Dubé, E. Supporting informed decision-making about vaccination: An analysis of two official websites. Public Health 2020, 178, 112–119. [Google Scholar] [CrossRef]
- Kieslich, K. Addressing vaccination hesitancy in Europe: A case study in state–society relations. Eur. J. Public Health 2018, 28, 30–33. [Google Scholar] [CrossRef]
- Kuchar, E.; Ludwikowska, K.; Szenborn, L.; Antczak, A.; Mastalerz–Migas, A.; Nitsch–Osuch, A. Knowledge Regarding Influenza and Influenza Vaccination in General Population: Results of a National Survey in Poland. Adv. Exp. Med. Biol. 2018, 1108, 55–61. [Google Scholar]
- Stefanoff, P.; Sobierajski, T.; Bulinska-Stangrecka, H.; Augustynowicz, E. Exploring factors improving support for vaccinations among Polish primary care physicians. PLoS ONE 2020, 15, e0232722. [Google Scholar] [CrossRef]
| No. | Question | Answers |
|---|---|---|
| B1 | Please indicate one source of information about vaccinations that you find most convincing | (1) medical sources (doctor, nurse, pharmacist) (2) media (press, radio, television, Internet) (3) environment (family, friends) |
| B2 | Did you obtain information on vaccination from healthcare professionals during visits to primary care physicians (PCP) or specialist outpatient clinic? | (1) Yes, (2) No |
| B3 | Using the school grade system, assess the level of vaccination information provided by health professionals | (1 worst–6 best) |
| B4 | What was the most important source of negative opinions about vaccinations? | (1) medical sources, (2) media, (3) environment |
| B6 | What opinion about vaccination was provided by health professionals? | (1) fully positive, (2) questioning the validity of certain vaccinations, (3) strongly negating the purposefulness of vaccinations |
| B7 | Which of the infectious diseases has been completely eliminated by vaccination?” | (1) measles, (2) rabies, (3) smallpox, (4) whooping cough, (5) hepatitis C |
| B8 | Do you consider yourself an advocate or opponent of vaccination? | (1) advocate, (2) opponent |
| B9 | The statement that “vaccines cause autism” is:” | (1) true, (2) false |
| B10 | In your opinion, should one be given mandatory, mandatory and recommended vaccines or not be given any vaccinations? | (1) mandatory, (2) mandatory and recommended vaccines, (3) no vaccinations |
| B11 | Have you been vaccinated in the last three years? | (1) Yes, (2) No |
| B12 | Are you vaccinated against seasonal influenza? | (1) Yes, (2) No |
| B13 | What do you consider when choosing additional prophylaxis for yourself or your child? | (1) I want to immunize myself/child against all possible diseases, (2) I want to immunize myself/child against serious life-threatening diseases, (3) I want to vaccinate myself/child with advertised (“fashionable”) vaccines, (4) I would like to vaccinate myself/child with additional vaccines but this is beyond my budget, (5) I don’t think additional vaccinations are necessary, (6) I think vaccinations are harmful. |
| B14 | If you consider vaccination to be harmful, which of the following diseases is in your opinion caused by vaccination: | (1) allergy, (2) neurological disorders, (3) autism, (4) diabetes, (5) immunosuppression, (6) myocarditis, (7) sudden infant death, (8) all of the above-mentioned diseases. |
| Determinants | Number (n) | Percentage (%) | t-Statistics (p Value) | |
|---|---|---|---|---|
| Respondents in general | 6432 | 100 | ||
| Gender | Female | 4303 | 66.9 | 93.25 (0.000) |
| Male | 2129 | 33.1 | 93.26 (0.000) | |
| Age | 18–25 | 4995 | 77.68 | 32.46 (0.000) |
| 26–35 | 697 | 10.06 | 131.85 (0.000) | |
| 36–45 | 302 | 4.7 | 3.85 (0.000) | |
| >45 | 488 | 7.58 | 6.326 (0.000) | |
| Education | Elementary | 1031 | 16.1 | 14.07 (0.000) |
| Secondary | 272 | 4.2 | 3.45 (0.000) | |
| College students | 4048 | 62.9 | 82.84 (0.000) | |
| Higher | 1081 | 16.8 | 14.77 (0.000) | |
| Financial status | Bad | 97 | 1.5 | 1.22 (0.112) |
| Medium | 3039 | 47.2 | 52.12 (0.000) | |
| Good | 3296 | 51.2 | 58.81 (0.000) | |
| Having children | Yes | 1038 | 16.1 | 14.11 (0.000) |
| Variable | β | SE β | Wald’s χ2 | eβ OR (95% CI) | p |
|---|---|---|---|---|---|
| Constant | 1.16 | 0.80 | 2.09 | NA | 0.14 |
| Sex (1-female, 2-male) | 0.08 | 0.12 | 0.49 | 1.09 (0.86–1.36) | 0.48 |
| Age | −0.43 | 0.11 | 16.29 | 0.28 (0.53–0.80) | <0.001 |
| Level of education (elementary (1)–higher education (4)) | 0.14 | 0.08 | 2.87 | 1.53 (0.98–1.36) | 0.09 |
| Financial situation (bad (1)–good (3)) | −0.06 | 0.11 | 0.27 | 0.90 (0.77–1.16) | 0.60 |
| Children (yes (1), no (2)) | −0.09 | 0.23 | 0.14 | 0.92 (0.59–1.43) | 0.71 |
| Fact of obtaining information on vaccinations from health care professionals [B2] (1- yes, 2- no) | 0.69 | 0.12 | 33.41 | 2.00 (1.58–2.53) | <0.001 |
| Level of information on vaccination received from health professionals [B3] (worst (1)–best (6)) | −0.01 | 0.05 | 0.03 | 0.96 (0.9–1.09) | 0.87 |
| Opinion on vaccination that you obtained from health care providers [B6] (positive (1)–fully negative (3)) | 0.65 | 0.10 | 44.41 | 3.67 (1.58–2.32) | <0.001 |
| “Which of the infectious diseases has been eliminated thanks to vaccinations?” [B7] wrong answer (0), correct answer (1) | −0.80 | 0.11 | 45.44 | 0.45 (0.09–0.18) | <0.001 |
| “Vaccines cause autism” [B9] true (1), false (2) | −2.06 | 0.19 | 113.37 | 0.13 (0.36–0.57) | <0.001 |
| For the entire model: χ2 = 344.18 p = 0.0000 | |||||
| Variable | β | SE β | Wald’s χ2 | eβ OR (95% CI) | p |
|---|---|---|---|---|---|
| Constant | 0.31 | 0.59 | 0.27 | NA | 0.60 |
| Sex (1-female, 2-male) | −0.12 | 0.09 | 1.69 | 0.89 (0.74–1.06) | 0.19 |
| Age | −0.40 | 0.06 | 42.76 | 0.30 (0.59–0.76) | <0.001 |
| Level of education (elementary (1)–higher education (4)) | 0.21 | 0.05 | 15.14 | 1.85 (1.1–1.36) | <0.001 |
| Financial situation (bad (1)–good (3)) | 0.00 | 0.02 | 0.01 | 1.00 (0.96–1.03) | 0.93 |
| Children (yes (1), no (2)) | 0.42 | 0.14 | 8.39 | 1.51 (1.14–2.01) | 0.004 |
| Fact of obtaining information on vaccinations from health care professionals [B2] (yes (1), no (2)) | 0.44 | 0.10 | 19.91 | 1.55 (1.28–1.88) | <0.001 |
| Level of information on vaccination received from health professionals [B3] (worst (1)–best (6)) | 0.07 | 0.03 | 4.59 | 1.41 (1.01–1.14) | 0.032 |
| Opinion on vaccination that you obtained from health care providers [B6] (positive (1)–fully negative (3)) | 0.12 | 0.08 | 2.31 | 1.27 (0.97–1.31) | 0.13 |
| “Which of the infectious diseases has been eliminated thanks to vaccinations?” [B7] wrong answer (0), correct answer (1) | −0.39 | 0.08 | 20.86 | 0.68 (0.58–0.80) | <0.001 |
| “Vaccines cause autism” [B9] true (1), false (2) | −0.39 | 0.19 | 4.14 | 0.68 (0.47–0.99) | 0.04 |
| For the entire model: χ2 = 270.86 p = 0.0000 | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czajka, H.; Czajka, S.; Biłas, P.; Pałka, P.; Jędrusik, S.; Czapkiewicz, A. Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations? Int. J. Environ. Res. Public Health 2020, 17, 4461. https://doi.org/10.3390/ijerph17124461
Czajka H, Czajka S, Biłas P, Pałka P, Jędrusik S, Czapkiewicz A. Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations? International Journal of Environmental Research and Public Health. 2020; 17(12):4461. https://doi.org/10.3390/ijerph17124461
Chicago/Turabian StyleCzajka, Hanna, Szymon Czajka, Paweł Biłas, Paulina Pałka, Szczepan Jędrusik, and Anna Czapkiewicz. 2020. "Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations?" International Journal of Environmental Research and Public Health 17, no. 12: 4461. https://doi.org/10.3390/ijerph17124461
APA StyleCzajka, H., Czajka, S., Biłas, P., Pałka, P., Jędrusik, S., & Czapkiewicz, A. (2020). Who or What Influences the Individuals’ Decision-Making Process Regarding Vaccinations? International Journal of Environmental Research and Public Health, 17(12), 4461. https://doi.org/10.3390/ijerph17124461





