Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study
Abstract
1. Introduction
2. Materials and methods
2.1. Implants
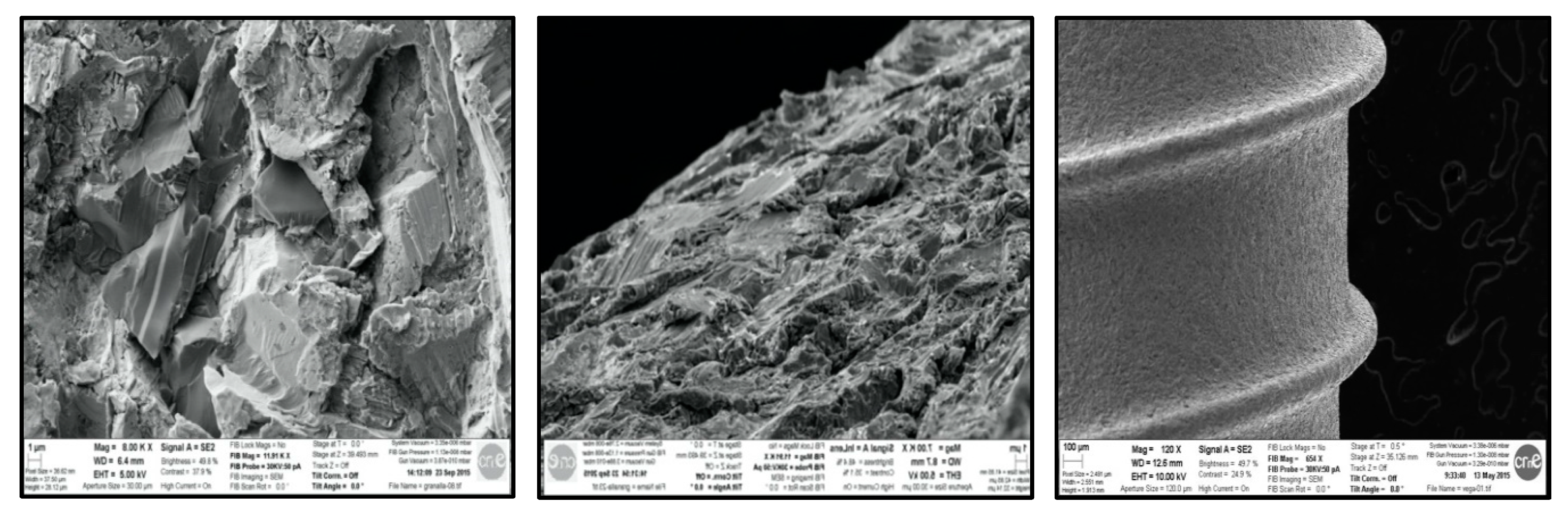
2.2. Bone
2.3. Sample Size
2.4. Ethical Committee
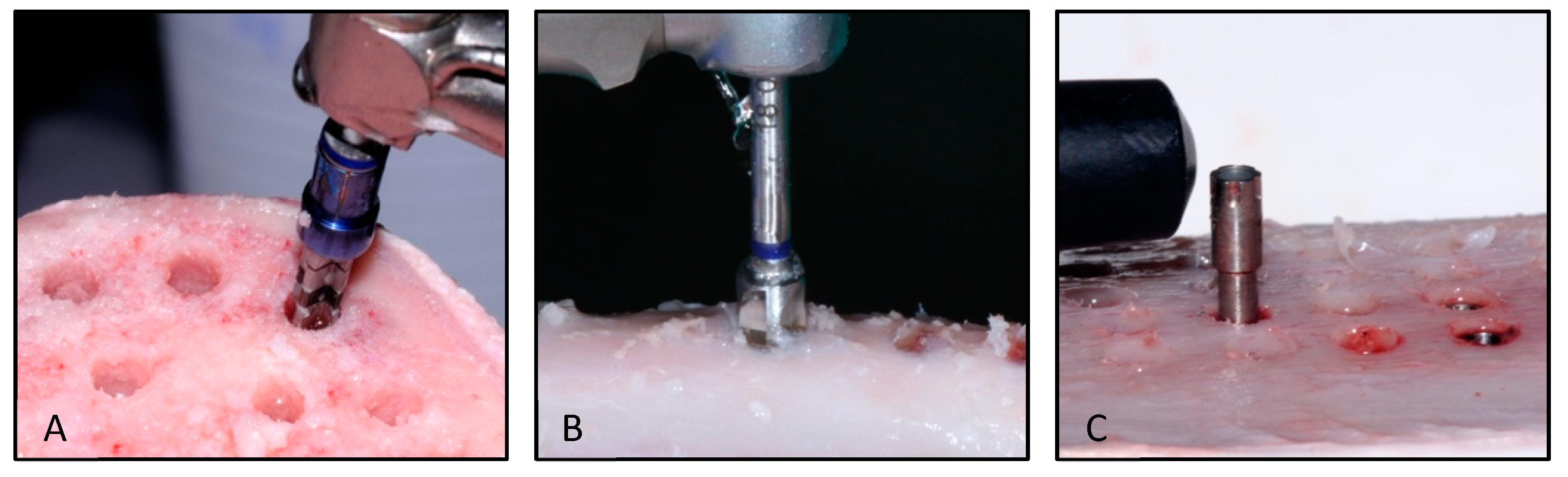
2.5. Implant Site Preparation
2.6. Study Groups
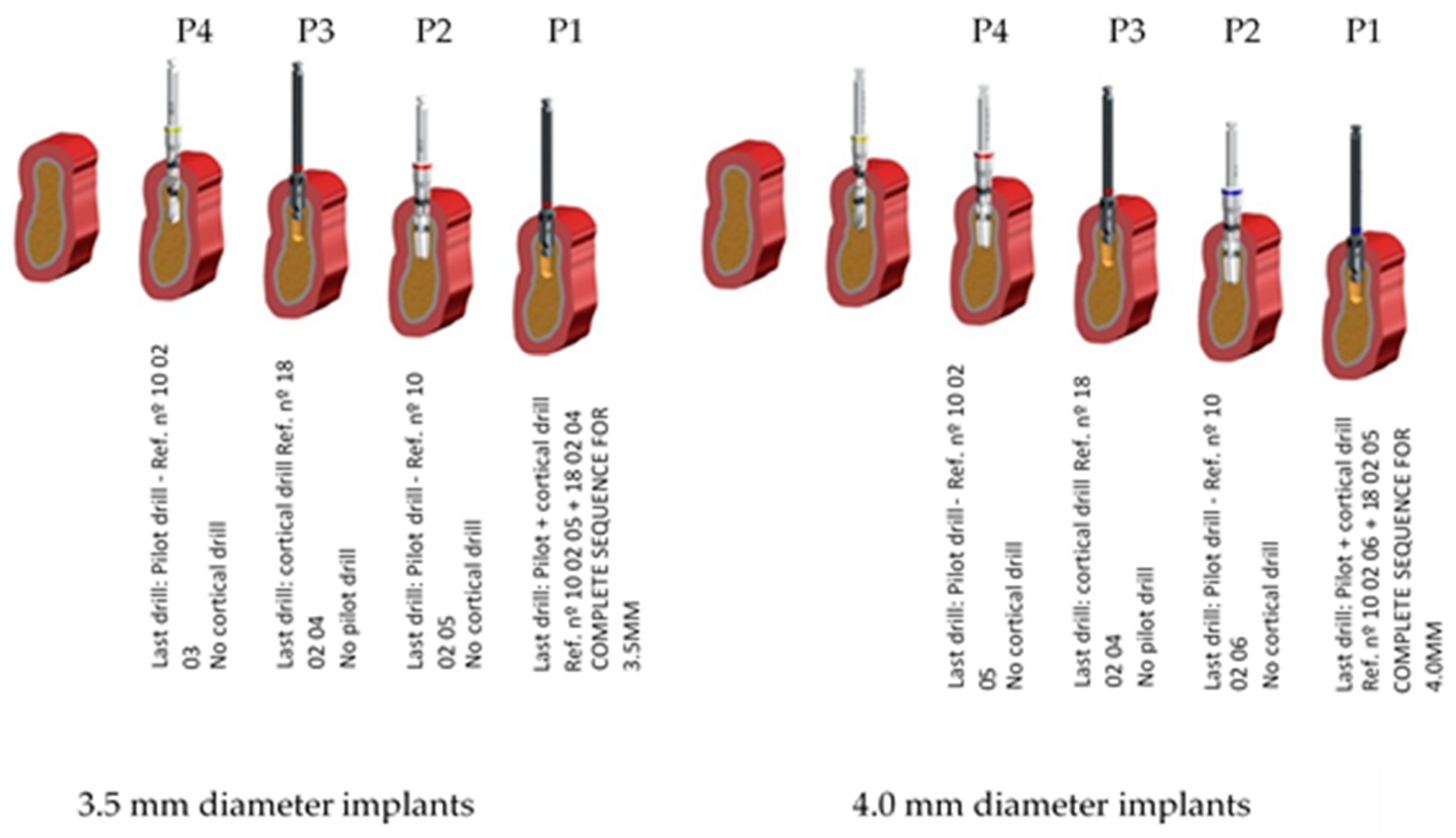
- P1: standard preparation and the recommended one by the company—control group.
- P2: the same as P1 but does not include the cortical drill (ref nº 18 02 04—3.5 mm ø implants/ref. 18 02 05—4.0 mm ø implants).
- P3: horizontal under-preparation technique that does not include the last full-length drill (ref nº 10 02 05 for 3.5 mm ø and ref. nº 10 02 06 for 4.0 mm diameter implants) but includes the cortical one.
- P4: horizontal under-preparation technique like P3 but without cortical drill (ref nº 18 02 04—3.5 mm ø implants/ref 18 02 05—4.0 mm ø implants).
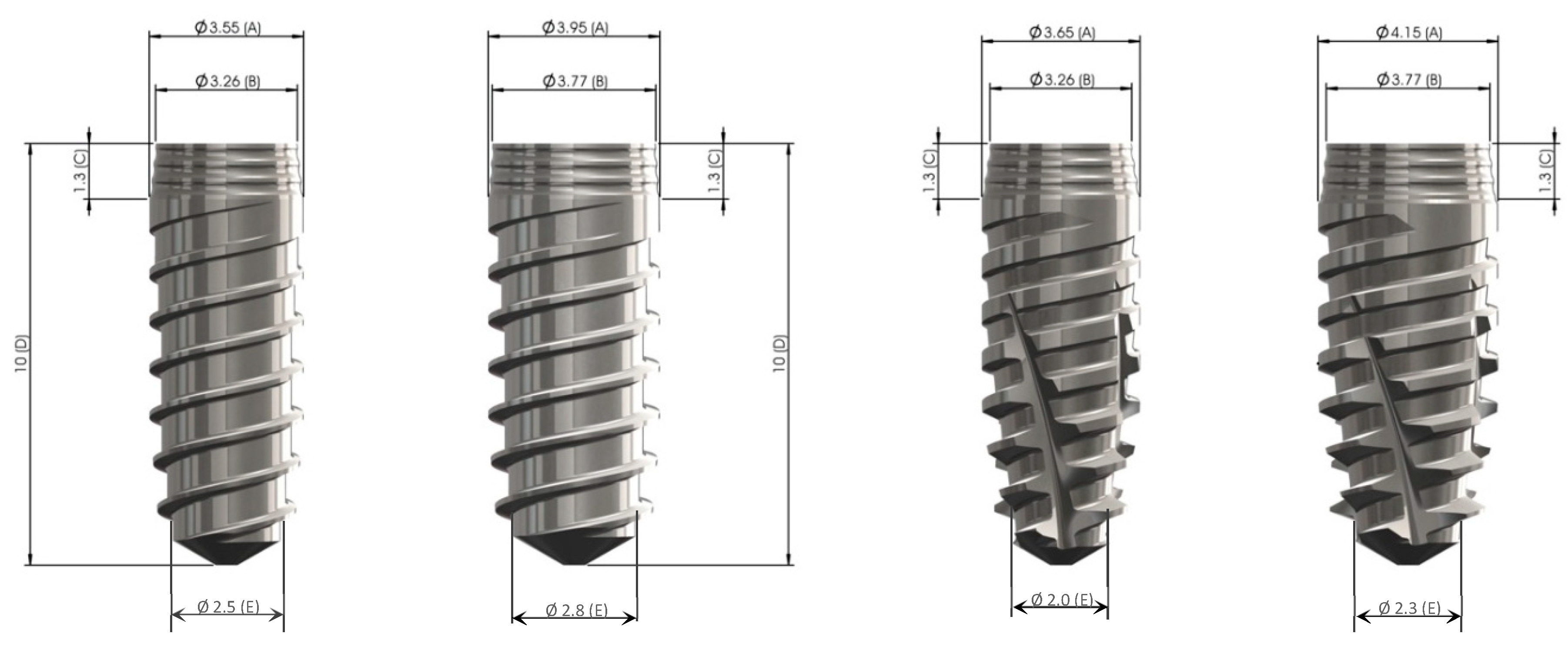
- A. Cylindrical—VEGA implant
- ○
- 3.5 mm implant diameter
- ○
- 4.0 mm implant diameter
- B. Tapered - VEGA X implant
- ○
- 3.5 mm implant diameter
- ○
- 4.0 mm implant diameter
2.7. Implant Stability Measurements
2.8. Drilling Sequences
- Lanceolate drill/decortication for the first 6 mm (ref. nº 10 02 01)
- 2.35 mm diameter (ø) initiation drill (ref. nº 10 02 02)
- 2.8 mm ø pilot drill (ref. nº 10 02 03)
- 3.5 mm ø cortical drill (ref. nº 18 02 04)
- 3.3 mm ø pilot drill (ref. nº 10 02 05)—last of 3.5 mm diameter implant
- 4.0 mm ø cortical drill (ref. nº 18 02 05)
- 3.6 mm ø pilot drill (ref. nº 10 02 06)—last of 4.0 mm diameter implant
2.9. Statistical Analysis
- For data meeting a normal distribution, two independent data groups were compared using a parametric t-student test, while three or more data groups were compared using ANOVA.
- For data not distributed normally, a Mann–Whitney test was used to compare two data groups and the Kruskall–Wallis test was used to compare three or more data groups. Non-parametric tests were also used to compare data groups meeting a normal distribution with data groups not meeting a normal distribution.
3. Results
4. Discussion
5. Conclusions
- Under-preparation of the implant site can be a viable method to improve the implant primary stability on both ISQ and IT, since there is an increase of implant surface in contact with bone.
- The use of a tapered shaped implant can improve the implant stability when comparing to a cylindrical shaped implant, leading to the fact that it is not necessary to use of an under-preparation of the site combining the use of tapered implants on low density bone (type III/IV).
- The removing of the cortical drill from the standard preparation was the implant site protocol that showed the biggest improvement of the implant stability.
- At the same time the clinician must evaluate the density of the present bone and carefully judge the type of protocol for each case.
Clinical Implications
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Anonymous. Oral implantology. Glossary of implant terms. J. Oral. Implantol. 2007, (Suppl. 1), 2–14. [Google Scholar]
- Lioubavina-Hack, N.; Lang, N.P.; Karring, T. Significance of primary stability for osseointegration of dental implants. Clin. Oral. Implants Res. 2006, 17, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Branemark, P.I.; Hansson, H.A.; Lindstrom, J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop. Scand. 1981, 52, 155–170. [Google Scholar] [CrossRef]
- Buser, D.; Sennerby, L.; de Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol. 2000 2017, 73, 7–21. [Google Scholar] [CrossRef]
- Wismeijer, D.; Vermeeren, J.I.; van Waas, M.A. Patient satisfaction with overdentures supported by one-stage TPS implants. Int J. Oral Maxillofac. Implants 1992, 7, 51–55. [Google Scholar]
- Buser, D.; von Arx, T. Surgical procedures in partially edentulous patients with ITI implants. Clin. Oral Implants Res. 2000, 11 (Suppl. 1), 83–100. [Google Scholar] [CrossRef]
- Bernard, J.P.; Belser, U.C.; Martinet, J.P.; Borgis, S.A. Osseointegration of Branemark fixtures using a single-step operating technique. A preliminary prospective one-year study in the edentulous mandible. Clin. Oral Implants Res. 1995, 6, 122–129. [Google Scholar] [CrossRef]
- Atieh, M.A.; Tawse-Smith, A.; Alsabeeha, N.H.M.; Ma, S.; Duncan, W.J. The one abutment-one time protocol: A systematic review and meta-analysis. J. Periodontol. 2017, 88, 1173–1185. [Google Scholar] [CrossRef]
- de Bruyn, H.; Raes, S.; Ostman, P.O.; Cosyn, J. Immediate loading in partially and completely edentulous jaws: A review of the literature with clinical guidelines. Periodontol. 2000 2014, 66, 153–187. [Google Scholar] [CrossRef]
- Chen, J.; Cai, M.; Yang, J.; Aldhohrah, T.; Wang, Y. Immediate versus early or conventional loading dental implants with fixed prostheses: A systematic review and meta-analysis of randomized controlled clinical trials. J. Prosthet. Dent. 2019, 122, 516–536. [Google Scholar] [CrossRef] [PubMed]
- Londhe, S.M.; Gowda, E.M.; Mandlik, V.B.; Shashidhar, M.P. Factors associated with abutment screw loosening in single implant supported crowns: A cross-sectional study. Med. J. Armed Forces India 2020, 76, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Ohlmann, B.; Waldecker, M.; Leckel, M.; Bomicke, W.; Behnisch, R.; Rammelsberg, P.; Schhmitter, M. Correlations between sleep bruxism and temporomandibular disorders. J. Clin. Med. 2020, 9, 611. [Google Scholar] [CrossRef] [PubMed]
- Bilhan, H.; Geckili, O.; Mumcu, E.; Bozdag, E.; Sunbuloglu, E.; Kutay, O. Influence of surgical technique, implant shape and diameter on the primary stability in cancellous bone. J. Oral. Rehabil. 2010, 37, 900–907. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Karl, M.; Grobecker-Karl, T. Effect of bone quality, implant design, and surgical technique on primary implant stability. Quintessence Int. 2018, 189–198. [Google Scholar] [CrossRef]
- Molly, L. Bone density and primary stability in implant therapy. Clin. Oral Implants Res. 2006, 17 (Suppl. 2), 124–135. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Piattelli, A. Primary stability determination by means of insertion torque and RFA in a sample of 4,135 implants. Clin. Implant. Dent. Relat. Res. 2012, 14, 501–507. [Google Scholar] [CrossRef]
- Han, J.; Lulic, M.; Lang, N.P. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: II. Implant surface modifications and implant diameter. Clin. Oral Implants Res. 2010, 21, 605–611. [Google Scholar] [CrossRef]
- Romanos, G.E.; Basha-Hijazi, A.; Gupta, B.; Ren, Y.F.; Malmstrom, H. Role of clinician’s experience and implant design on implant stability. An ex vivo study in artificial soft bones. Clin. Implant Dent. Relat. Res. 2014, 16, 166–171. [Google Scholar] [CrossRef]
- Wilson, T.G.J.; Miller, R.J.; Trushkowsky, R.; Dard, M. Tapered implants in dentistry: Revitalizing concepts with technology: A review. Adv. Dent. Res. 2016, 28, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lim, Y.J.; Kim, M.J.; Kwon, H.B. The effect of various thread designs on the initial stability of taper implants. J. Adv. Prosthodont. 2009, 1, 19–25. [Google Scholar] [CrossRef]
- Ryu, H.S.; Namgung, C.; Lee, J.H.; Lim, Y.J. The influence of thread geometry on implant osseointegration under immediate loading: A literature review. J. Adv. Prosthodont. 2014, 6, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Leesungbok, R.; Lee, S.W.; Heo, Y.K.; Kang, K.L. Differences in implant stability associated with various methods of preparation of the implant bed: An in vitro study. J. Prosthet. Dent. 2012, 107, 366–372. [Google Scholar] [CrossRef]
- Tabassum, A.; Meijer, G.J.; Wolke, J.G.; Jansen, J.A. Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: A laboratory study. Clin. Oral Implants Res. 2010, 21, 213–220. [Google Scholar] [CrossRef]
- Friberg, B.; Grondahl, K.; Lekholm, U.; Branemark, P.I. Long-term follow-up of severely atrophic edentulous mandibles reconstructed with short Branemark implants. Clin. Implant. Dent. Relat. Res. 2000, 2, 184–189. [Google Scholar] [CrossRef]
- Jimbo, R.; Tovar, N.; Anchieta, R.B.; Machado, L.S.; Marin, C.; Teixeira, H.S.; Coelho, P.G. The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: An experimental study. Int. J. Oral Maxillofac. Surg. 2014, 43, 1269–1275. [Google Scholar] [CrossRef]
- Duyck, J.; Corpas, L.; Vermeiren, S.; Ogawa, T.; Quirynen, M.; Vandamme, K.; Jacobs, R.; Naert, I. Histological, histomorphometrical, and radiological evaluation of an experimental implant design with a high insertion torque. Clin. Oral Implants Res. 2010, 21, 877–884. [Google Scholar] [CrossRef]
- Monje, A.; Ravida, A.; Wang, H.L.; Helms, J.A.; Brunski, J.B. Relationship Between Primary/Mechanical and Secondary/Biological Implant Stability. Int. J. Oral Maxillofac. Implants 2019, 34, s7–s23. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.; Duncan, W.J. Stability of tapered and parallel-walled dental implants: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2018, 20, 634–645. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Lopez-Jarana, P.; Lemos, B.F.; Gil, F.J.; Falcao, C.; Rios-Santos, J.V.; Rios, B. Relevant design aspects to improve the stability of titanium dental implants. Materials (Basel) 2020, 13, 1910. [Google Scholar] [CrossRef] [PubMed]
- di Stefano, D.A.; Arosio, P.; Perrotti, V.; Iezzi, G.; Scarano, A.; Piattelli, A. Correlation between implant geometry, bone density, and the insertion torque/depth integral: A study on bovine ribs. Dent. J. (Basel) 2019, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Leocadio, A.C.S.; Junior, M.S.; Oliveira, G.; Pinto, G.; Faeda, R.S.; Padovan, L.E.M.; Junior, E.M. Evaluation of implants with different macrostructures in Type I bone-pre-clinical study in rabbits. Materials 2020, 13, 1521. [Google Scholar] [CrossRef] [PubMed]
- de Bruyn, H.; Christiaens, V.; Doornewaard, R.; Jacobsson, M.; Cosyn, J.; Jacquet, W.; Vervaeke, S. Implant surface roughness and patient factors on long-term peri-implant bone loss. Periodontol. 2000 2017, 73, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Albrektsson, T. Suggested guidelines for the topographic evaluation of implant surfaces. Int. J. Oral Maxillofac. Implants. 2000, 15, 331–344. [Google Scholar]
- Juodzbalys, G.; Kubilius, M. Clinical and radiological classification of the jawbone anatomy in endosseous dental implant treatment. J. Oral Maxillofac. Res. 2013, 4, e2. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Santos-Garcia, R.; Jaramillo-Santos, R.; Romero-Ruiz, M.M.; Fernandez-Palacin, A.; Lazaro-Calvo, P.; Bullon, P.; Rios-Santos, J.-V. Assessment of Osstell ISQ’s reliability for implant stability measurement: A cross-sectional clinical study. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, e877–e882. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Albertini, M.; Rios-Santos, J.V.; Lazaro-Calvo, P.; Fernandez-Palacin, A.; Bullon, P. Resonance frequency analysis-reliability in third generation instruments: Osstell mentor(R). Med. Oral Patol. Oral Cir. Bucal. 2012, 17, e801–e806. [Google Scholar] [CrossRef]
- Stocchero, M.; Toia, M.; Cecchinato, D.; Becktor, J.P.; Coelho, P.G.; Jimbo, R. Biomechanical, biologic, and clinical outcomes of undersized implant surgical preparation: A systematic review. Int. J. Oral Maxillofac. Implants 2016, 31, 1247–1263. [Google Scholar] [CrossRef]
- Baldi, D.; Lombardi, T.; Colombo, J.; Cervino, G.; Perinetti, G.; di Lenarda, R.; Stacchi, C. Correlation between insertion torque and implant stability quotient in tapered implants with knife-edge thread design. Biomed. Res. Int. 2018, 2018, 7201093. [Google Scholar] [CrossRef]
- Kim, Y.K.; Lee, J.H.; Lee, J.Y.; Yi, Y.J. A randomized controlled clinical trial of two types of tapered implants on immediate loading in the posterior maxilla and mandible. Int. J. Oral Maxillofac. Implants. 2013, 28, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
- Andres-Garcia, R.; Vives, N.G.; Climent, F.H.; Palacin, A.F.; Santos, V.R.; Climent, M.H.; Bullon, P. In vitro evaluation of the influence of the cortical bone on the primary stability of two implant systems. Med. Oral Patol. Oral Cir. Bucal. 2009, 14, E93–E97. [Google Scholar] [PubMed]
- Garcia-Vives, N.; Andres-Garcia, R.; Rios-Santos, V.; Fernandez-Palacin, A.; Bullon-Fernandez, P.; Herrero-Climent, M.; Herrero-Climent, F. In vitro evaluation of the type of implant bed preparation with osteotomes in bone type IV and its influence on the stability of two implant systems. Med. Oral. Patol. Oral Cir. Bucal. 2009, 14, e455–e460. [Google Scholar] [PubMed]
- Herrero-Climent, M.; Falcao, A.; Lopez-Jarana, P.; Diaz-Castro, C.M.; Rios-Carrasco, B.; Rios-Santos, J.V. In vitro comparative analysis of two resonance frequency measurement devices: Osstell implant stability coefficient and Penguin resonance frequency analysis. Clin. Implant Dent. Relat. Res. 2019, 21, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.H.; Um, H.S.; Lee, J.K.; Chang, B.S.; Lee, M.K. The effect of implant shape and bone preparation on primary stability. J. Periodontal. Implant. Sci. 2010, 40, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Piattelli, A. Influence of stepped osteotomy on primary stability of implants inserted in low-density bone sites: An in vitro study. Int. J. Oral Maxillofac. Implants. 2017, 32, 37–41. [Google Scholar] [CrossRef]
- Boustany, C.M.; Reed, H.; Cunningham, G.; Richards, M.; Kanawati, A. Effect of a modified stepped osteotomy on the primary stability of dental implants in low-density bone: A cadaver study. Int. J. Oral Maxillofac. Implants 2015, 30, 48–55. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Piattelli, A. Determination of primary stability: A comparison of the surgeon’s perception and objective measurements. Int. J. Oral Maxillofac. Implants. 2010, 25, 558–561. [Google Scholar]
- da Cunha, H.A.; Francischone, C.E.; Filho, H.N.; de Oliveira, R.C. A comparison between cutting torque and resonance frequency in the assessment of primary stability and final torque capacity of standard and TiUnite single-tooth implants under immediate loading. Int. J. Oral Maxillofac. Implants 2004, 19, 578–585. [Google Scholar]
- Nkenke, E.; Hahn, M.; Weinzierl, K.; Radespiel-Troger, M.; Neukam, F.W.; Engelke, K. Implant stability and histomorphometry: A correlation study in human cadavers using stepped cylinder implants. Clin. Oral Implants Res. 2003, 14, 601–609. [Google Scholar] [CrossRef]
- Brizuela-Velasco, A.; Alvarez-Arenal, A.; Gil-Mur, F.J.; Herrero-Climent, M.; Chavarri-Prado, D.; Chento-Valiente, Y.; Dieguez-Pereira, M. Relationship between insertion torque and resonance frequency measurements, performed by resonance frequency analysis, in micromobility of dental implants: An in vitro study. Implant Dent. 2015, 24, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Blanco, J.; Suarez, J.; Novio, S.; Villaverde, G.; Ramos, I.; Segade, L.A. Histomorphometric assessment in human cadavers of the peri-implant bone density in maxillary tuberosity following implant placement using osteotome and conventional techniques. Clin. Oral Implants Res. 2008, 19, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Shalabi, M.M.; Wolke, J.G.; de Ruijter, A.J.; Jansen, J.A. A mechanical evaluation of implants placed with different surgical techniques into the trabecular bone of goats. J. Oral Implantol. 2007, 33, 51–58. [Google Scholar] [CrossRef] [PubMed]
| Prep. | Implant | IT—N/cm | ISQ | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| 3.5 mm | |||||
| P1 | Cylindrical | 34.6 | 15.4 | 74.9 | 5.3 |
| Tapered | 54.2 | 22.6 | 78.2 | 7.5 | |
| P2 | Cylindrical | 44.1 | 12.4 | 78.2 | 6.5 |
| Tapered | 57.3 | 15.2 | 78.6 | 3.9 | |
| P3 | Cylindrical | 63.7 | 18.7 | 76.4 | 6.8 |
| Tapered | 75.9 | 16.2 | 79.0 | 7.3 | |
| P4 | Cylindrical | 66.4 | 24.4 | 76.2 | 11.2 |
| Tapered | 68.8 | 21.7 | 79.6 | 5.2 | |
| 4.0 mm | |||||
| P1 | Cylindrical | 43.6 | 25.5 | 76.0 | 5.0 |
| Tapered | 64.7 | 22.8 | 78.5 | 3.2 | |
| P2 | Cylindrical | 45.2 | 15.2 | 79.1 | 4.8 |
| Tapered | 65.7 | 19.2 | 79.9 | 2.5 | |
| P3 | Cylindrical | 52.5 | 20.4 | 76.2 | 5.9 |
| Tapered | 60.3 | 24.0 | 76.1 | 6.6 | |
| P4 | Cylindrical | 54.5 | 22.9 | 76.8 | 6.7 |
| Tapered | 65.0 | 27.4 | 76.3 | 8.0 | |
| Implant Diameter | Prep. Technique | IT | Distribution | ISQ A | Distribution | ISQ B | Distribution | ISQ X | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 3.5 mm | P1 | V < VX p = 0.000 | V(N) | VX(NO) | V < VX p = 0.000 | V(NO) | VX(NO) | V < VX p = 0.000 | V(NO) | VX(NO) | V < VX |
| P2 | V < VX p = 0.000 | V(N) | VX(NO) | V = VX p = 0.422 | V(NO) | VX(NO) | V = VX p = 0.610 | V(NO) | VX(NO) | V = VX | |
| P3 | V < VX p = 0.002 | V(N) | VX(NO) | V < VX p = 0.000 | V(NO) | VX(NO) | V < VX p = 0.000 | V(NO) | VX(NO) | V < VX | |
| P4 | V = VX p = 0.711 | V(NO) | VX(NO) | V = VX p = 0.082 | V(NO) | VX(NO) | V = VX p = 0.351 | V(NO) | VX(NO) | V = VX | |
| 4.0 mm | P1 | V < VX p = 0.000 | V(NO) | VX(NO) | V < VX p = 0.016 | V(N) | VX(NO) | V < VX p = 0.039 | V(N) | VX(NO) | V < VX |
| P2 | V < VX p = 0.000 | V(NO) | VX(N) | V = VX p = 0.965 | V(NO) | VX(NO) | V = VX p = 0.684 | V(NO) | VX(NO) | V = VX | |
| P3 | V = VX p = 0.127 | V(N) | VX(N) | V = VX p = 1.000 | V(NO) | VX(NO) | V = VX p = 0.348 | V(NO) | VX(NO) | V = VX | |
| P4 | V < VX p = 0.038 | V(N) | VX(NO) | V = VX p = 0.358 | V(NO) | VX(NO) | V = VX p = 0.942 | V(NO) | VX(NO) | V = VX | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrero-Climent, M.; Lemos, B.F.; Herrero-Climent, F.; Falcao, C.; Oliveira, H.; Herrera, M.; Gil, F.J.; Ríos-Carrasco, B.; Ríos-Santos, J.-V. Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. Int. J. Environ. Res. Public Health 2020, 17, 4436. https://doi.org/10.3390/ijerph17124436
Herrero-Climent M, Lemos BF, Herrero-Climent F, Falcao C, Oliveira H, Herrera M, Gil FJ, Ríos-Carrasco B, Ríos-Santos J-V. Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. International Journal of Environmental Research and Public Health. 2020; 17(12):4436. https://doi.org/10.3390/ijerph17124436
Chicago/Turabian StyleHerrero-Climent, Mariano, Bernardo Ferreira Lemos, Federico Herrero-Climent, Carlos Falcao, Helder Oliveira, Manuela Herrera, Francisco Javier Gil, Blanca Ríos-Carrasco, and José-Vicente Ríos-Santos. 2020. "Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study" International Journal of Environmental Research and Public Health 17, no. 12: 4436. https://doi.org/10.3390/ijerph17124436
APA StyleHerrero-Climent, M., Lemos, B. F., Herrero-Climent, F., Falcao, C., Oliveira, H., Herrera, M., Gil, F. J., Ríos-Carrasco, B., & Ríos-Santos, J.-V. (2020). Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. International Journal of Environmental Research and Public Health, 17(12), 4436. https://doi.org/10.3390/ijerph17124436










