Predicting Professional Quality of Life and Life Satisfaction in Spanish Nurses: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Procedure, and Participants
2.2. Instruments
- The Short version of the Nursing Stress Scale (Short NSS). The Nursing Stress Scale (NSS) was designed to hospital nurses in 1981 [51] and was validated into Spanish in 1999 [52]. It assesses six dimensions of nurses’ occupational stress with 34 items: coping with death and dying process, conflict with physicians, lack of staff support, conflict with other nurses, workload, uncertainty concerning treatment, and work role setting. The short version uses one indicator per dimension, and respondents scores range from 0 (never) to 3 (always). In this study the research team have used a short version and the reliability of this scale in this sample was 0.701.
- The Short version of the Practice Environment Scale of the Nursing Work Index (PES-NWI). The Practice Environment Scale of the Nursing Work Index (PES-NWI) was developed by Lake [53] and, ten years later, it was validated into Spanish [54]. The scale evaluates five dimensions of nursing work environment with 31 items: nurse participation in hospital affairs; nursing foundations for quality of care; nurse manager ability, leadership and support for nurses; staffing and resource adequacy; collegial nurse–physician relations. The short version uses one indicator per dimension, and respondents scores range from 1 (totally disagree) to 4 (totally agree). The internal consistency estimate of the short version used in the study was 0.740.
- The Professional Self-Care Scale (PSCS) [37]. The original Spanish version was used. It is composed by nine items and assesses three dimensions of professionals’ self-care: physical, which refers to the implication in activities that helps to maintain a healthy body; inner, which is related to activities that help to keep a healthy mind; and social, regarded to activities related to social activities that help the individual to maintain social health. Items score in a 5-point Likert-type scale, from 1 (totally disagree) to 5 (totally agree). The reliability of the scale in this sample was 0.730.
- The Self-Compassion Scale (SCS) [55]. In this case, the short version validated into Spanish in 2014 [56] was used. The SCS is formed by 12 items assessing three main components of self-compassion and their opposites: self-kindness/self-judgment, common humanity/isolation, and mindfulness/over-identification. Items score in a 5-point Likert-type scale, from 1 (totally disagree) to 5 (totally agree). The Cronbach’s alpha in this sample was 0.848.
- The Professional Quality of Life Scale (ProQoL) [9]. The ProQOL has been recently validated in Spanish [57]. This scale evaluates three dimensions of quality of life: compassion satisfaction, compassion fatigue, and burnout syndrome, with ten items per factor. In current research, a short version of three items per factor was used. Items score in a 6-point Likert-type scale, from 0 (never) to 5 (always). Internal consistency estimates were 0.872, 0.812, and 0.646. It has to be borne in mind that quality of life was modeled as a latent factor and, consequently, estimated free of error for the prediction purpose.
- Satisfaction with Life Scale [47]. The Spanish version was used [58]. The scale assesses subjective well-being, specifically global satisfaction with life, with five items. Items score in a 5-point Likert-type scale, from 1 (totally disagree) to 5 (totally agree). The internal consistency in this sample was 0.911.
2.3. Ethical Considerations
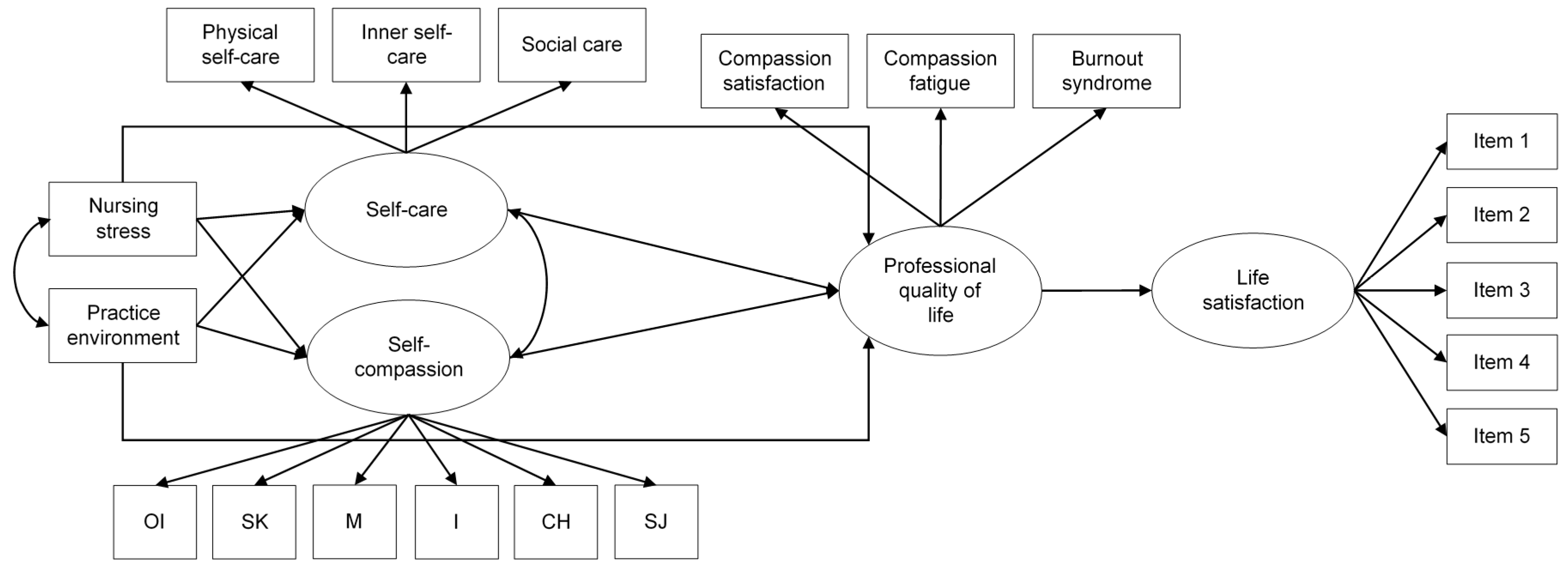
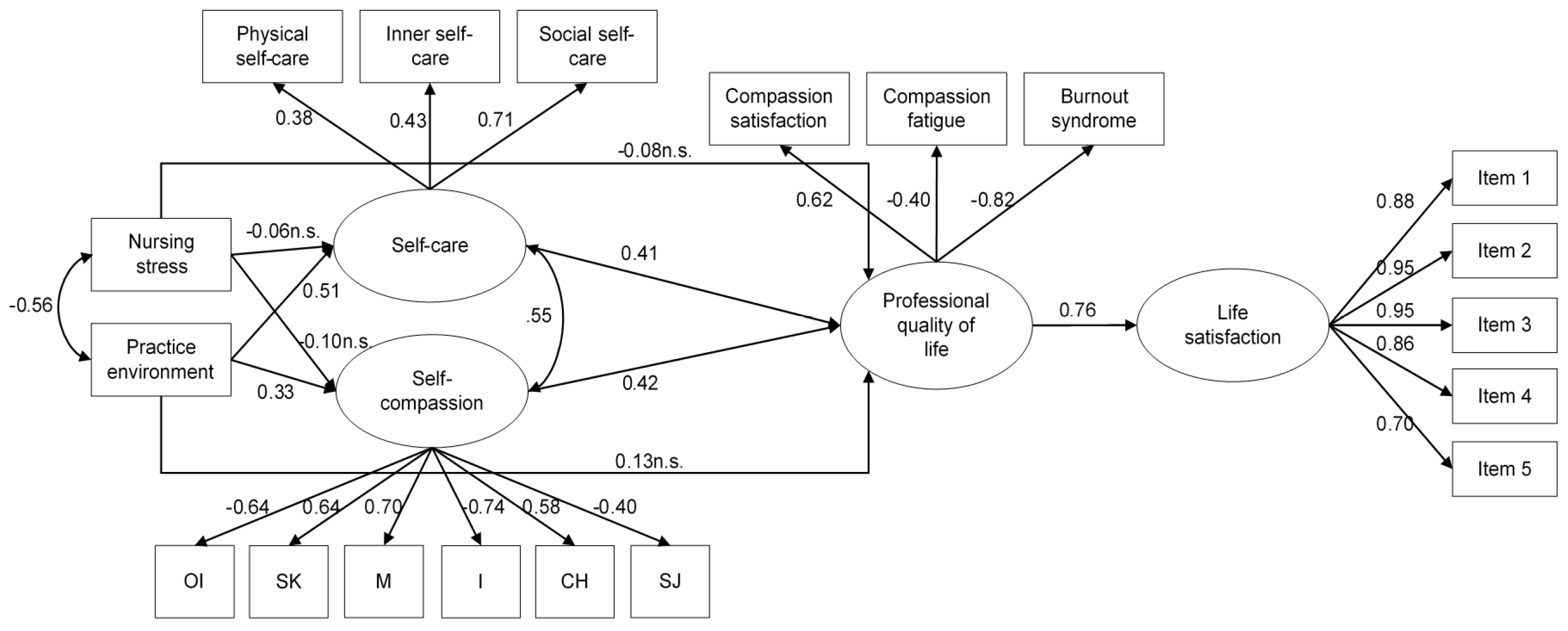
2.4. Data Analyses
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yh, M.K.; Chong, P.H.; Neo, P.S.H.; Ong, Y.J.; Yong, W.C.; Ong, W.Y.; Shen, M.L.J.; Hum, A.Y.M. Burnout, Psychological Morbidity and Use of Coping Mechanisms Among Palliative Care Practitioners: A Multi-Centre Cross-Sectional Study. Available online: https://journals.sagepub.com/doi/10.1177/0269216315575850 (accessed on 19 May 2020).
- Clegg, A. Occupational stress in nursing: A review of the literature. J. Nurs. Manag. 2001, 9, 101–106. [Google Scholar] [CrossRef] [PubMed]
- McGrath, A.; Reid, N.; Boore, J. Occupational stress in nursing. Int. J. Nurs. Stud. 1989, 26, 343–358. [Google Scholar] [CrossRef]
- Maslach, C. Job burnout: New directions in research and intervention. Curr. Dir. Psychol. Sci. 2003, 12, 189–192. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Shirom, A. Job-related burnout: A review of major research foci and challenges. In Handbook of Occupational Health Psychology, 2nd ed.; Quick, J.C., Tetrick, L.E., Eds.; American Psychological Association: Washington, DC, USA, 2011; pp. 223–241. ISBN 978-1-4338-0776-3. [Google Scholar]
- Salyers, M.P.; Bonfils, K.A.; Luther, L.; Firmin, R.L.; White, D.A.; Adams, E.L.; Rollins, A.L. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J. Gen. Intern. Med. 2016, 32, 475–482. [Google Scholar] [CrossRef]
- Figley, C.R. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized; Figley, C.R., Ed.; Brunner/Mazel psychological stress series, No. 23; Brunner/Mazel: Philadelphia, PA, USA, 1995; ISBN 978-0-87630-759-5. [Google Scholar]
- Stamm, B.H. The Concise ProQOL Manual; ProQOL.org: Pocatello, ID, USA, 2010. [Google Scholar]
- Bride, B.E.; Radey, M.; Figley, C.R. Measuring Compassion Fatigue. Clin. Soc. Work. J. 2007, 35, 155–163. [Google Scholar] [CrossRef]
- Breath of Relief: Transforming Compassion Fatigue into Flow by Larowe, Karl: Very Good Soft Cover. First Printing—Yes Books. 2005. Available online: https://www.abebooks.com/first-edition/Breath-Relief-Transforming-Compassion-Fatigue-Flow/8402401530/bd (accessed on 19 May 2020).
- Quitangon, G.; Evces, M.R. Vicarious Trauma and Disaster Mental Health: Understanding Risks and Promoting Resilience; Quitangon, G., Evces, M.R., Eds.; Psychosocial stress series; Routledge/Taylor & Francis Group: New York, NY, USA, 2015; ISBN 978-1-138-79329-3. [Google Scholar]
- Najjar, N.; Davis, L.W.; Beck-Coon, K.; Doebbeling, C.C. Compassion Fatigue. J. Heal. Psychol. 2009, 14, 267–277. [Google Scholar] [CrossRef]
- Coetzee, S.K.; Klopper, H.C. Compassion fatigue within nursing practice: A concept analysis. Nurs. Health Sci. 2010, 12, 235–243. [Google Scholar] [CrossRef]
- Nolte, A.G.; Downing, C.; Temane, A.; Hastings-Tolsma, M. Compassion fatigue in nurses: A metasynthesis. J. Clin. Nurs. 2017, 26, 4364–4378. [Google Scholar] [CrossRef]
- Dominguez-Gomez, E.; Rutledge, D.N. Prevalence of Secondary Traumatic Stress Among Emergency Nurses. J. Emerg. Nurs. 2009, 35, 199–204. [Google Scholar] [CrossRef]
- Hooper, C.; Craig, J.; Janvrin, D.R.; Wetsel, M.A.; Reimels, E. Compassion Satisfaction, Burnout, and Compassion Fatigue Among Emergency Nurses Compared with Nurses in Other Selected Inpatient Specialties. J. Emerg. Nurs. 2010, 36, 420–427. [Google Scholar] [CrossRef]
- Young, J.L.; Derr, D.M.; Cicchillo, V.J.; Bressler, S. Compassion Satisfaction, Burnout, and Secondary Traumatic Stress in Heart and Vascular Nurses. Crit. Care Nurs. Q. 2011, 34, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Perry, B.; Toffner, G.; Merrick, T.; Dalton, J. An exploration of the experience of compassion fatigue in clinical oncology nurses. Can. Oncol. Nurs. J. 2011, 21, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Potter, P.; Deshields, T.; Kuhrik, M. Delegation practices between registered nurses and nursing assistive personnel. J. Nurs. Manag. 2010, 18, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Beaumont, E.; Durkin, M.; Martin, C.J.H.; Carson, J. Compassion for others, self-compassion, quality of life and mental well-being measures and their association with compassion fatigue and burnout in student midwives: A quantitative survey. Midwifery 2016, 34, 239–244. [Google Scholar] [CrossRef]
- Sacco, T.L.; Ciurzynski, S.M.; Harvey, M.E.; Ingersoll, G.L. Compassion Satisfaction and Compassion Fatigue Among Critical Care Nurses. Crit. Care Nurs. 2015, 35, 32–42. [Google Scholar] [CrossRef]
- Berger, J.; Polivka, B.; Smoot, E.A.; Owens, H. Compassion Fatigue in Pediatric Nurses. J. Pediatr. Nurs. 2015, 30, e11–e17. [Google Scholar] [CrossRef]
- Drury, V.; Craigie, M.; Francis, K.; Aoun, S.; Hegney, D. Compassion satisfaction, compassion fatigue, anxiety, depression, and stress in registered nurses in Australia: Phase 2 results. J. Nurs. Manag. 2014, 22, 519–531. [Google Scholar] [CrossRef]
- Hegney, D.; Craigie, M.; Hemsworth, D.; Osseiran-Moisson, R.; Aoun, S.; Francis, K.; Drury, V. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J. Nurs. Manag. 2013, 22, 506–518. [Google Scholar] [CrossRef]
- Austin, W.; Goble, E.; Leier, B.; Byrne, P. Compassion Fatigue: The Experience of Nurses. Ethic Soc. Welf. 2009, 3, 195–214. [Google Scholar] [CrossRef]
- Duffy, E.; Avalos, G.; Dowling, M. Secondary traumatic stress among emergency nurses: A cross-sectional study. Int. Emerg. Nurs. 2015, 23, 53–58. [Google Scholar] [CrossRef]
- Mathias, C.T.; Wentzel, D. Descriptive study of burnout, compassion fatigue and compassion satisfaction in undergraduate nursing students at a tertiary education institution in KwaZulu-Natal. Curationis 2017, 40, 6. [Google Scholar] [CrossRef] [PubMed]
- Durkin, M.; Smith, J.; Powell, M.; Howarth, J.; Carson, J. Wellbeing, compassion fatigue and burnout in APs. Br. J. Heal. Assist. 2013, 7, 456–459. [Google Scholar] [CrossRef]
- Giarelli, E.; de Nigris, J.; Fisher, K.; Maley, M.; Nolan, E. Perceived Quality of Work Life and Risk for Compassion Fatigue Among Oncology Nurses: A Mixed-Methods Study. Oncol. Nurs. Forum 2016, 43, E121–E131. [Google Scholar] [CrossRef] [PubMed]
- Mason, V.M.; Leslie, G.; Clark, K.; Lyons, P.; Walke, E.; Butler, C.; Griffin, M. Compassion Fatigue, Moral Distress, and Work Engagement in Surgical Intensive Care Unit Trauma Nurses. Dimens. Crit. Care Nurs. 2014, 33, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Maytum, J.C.; Heiman, M.B.; Garwick, A.W. Compassion fatigue and burnout in nurses who work with children with chronic conditions and their families. J. Pediatr. Heal. Care 2004, 18, 171–179. [Google Scholar] [CrossRef]
- Smart, D.; English, A.; James, J.; Wilson, M.; Daratha, K.B.; Childers, B.; Magera, C. Compassion fatigue and satisfaction: A cross-sectional survey among US healthcare workers. Nurs. Heal. Sci. 2013, 16, 3–10. [Google Scholar] [CrossRef]
- Kearney, M.K.; Weininger, R.B.; Vachon, M.L.S.; Harrison, R.L.; Mount, B.M. Self-care of Physicians Caring for Patients at the End of Life “Being Connected. A Key to My Survival. JAMA J. Am. Med. Assoc. 2009, 301, 1155–1164. [Google Scholar] [CrossRef]
- Mills, J.; Wand, T.; Fraser, J.A. On self-compassion and self-care in nursing: Selfish or essential for compassionate care? Int. J. Nurs. Stud. 2015, 52, 791–793. [Google Scholar] [CrossRef]
- Sanchez-Reilly, S.; Morrison, L.; Carey, E.; Bernacki, R.; O’Neill, L.; Kapo, J.; Periyakoil, V.; Thomas, J. Carin for oneself to care for others: Physicians and their self-care. J. Support. Oncol. 2013, 11, 75–81. [Google Scholar] [CrossRef]
- Galiana, L.; Oliver, A.; Sansó, N.; Oliver, E.B. Validation of a New Instrument for Self-care in Spanish Palliative Care Professionals Nationwide. Span. J. Psychol. 2015, 18. [Google Scholar] [CrossRef]
- Neville, K.; Cole, D.A. The Relationships Among Health Promotion Behaviors, Compassion Fatigue, Burnout, and Compassion Satisfaction in Nurses Practicing in a Community Medical Center. JONA J. Nurs. Adm. 2013, 43, 348–354. [Google Scholar] [CrossRef]
- Sorenson, C.; Bolick, B.; Wright, K.; Hamilton, R. Understanding Compassion Fatigue in Healthcare Providers: A Review of Current Literature. J. Nurs. Sch. 2016, 48, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Neff, K. Self-Compassion: The Proven Power of Being Kind to Yourself; HarperCollins e-Books: New York, NY, USA, 2011. [Google Scholar]
- Raab, K. Mindfulness, Self-Compassion, and Empathy Among Health Care Professionals: A Review of the Literature. J. Heal. Care Chaplain. 2014, 20, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Gustin, L.W.; Wagner, L. The butterfly effect of caring—Clinical nursing teacher’s understanding of self-compassion as a source to compassionate care. Scand. J. Caring Sci. 2012, 27, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Durkin, M.; Beaumont, E.; Martin, C.J.H.; Carson, J. A pilot study exploring the relationship between self-compassion, self-judgement, self-kindness, compassion, professional quality of life and wellbeing among UK community nurses. Nurse Educ. Today 2016, 46, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Mahon, M.A.; Mee, L.; Brett, D.; Dowling, M. Nurses’ perceived stress and compassion following mindfulness meditation and self-compassion training. J. Res. Nurs. 2017, 22. [Google Scholar] [CrossRef]
- Duarte, J.; Pinto-Gouveia, J.; Cruz, B. Relationships between nurses’ empathy, self-compassion, and dimensions of professional quality of life: A cross-sectional study. Int. J. Nurs. Stud. 2016, 60, 1–11. [Google Scholar] [CrossRef]
- Neff, K.D.; Pommier, E. The Relationship between Self-compassion and Other-focused Concern among College Undergraduates, Community Adults, and Practicing Meditators. Self Identit. 2013, 12, 160–176. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Shin, D.C.; Johnson, D.M. Avowed happiness as an overall assessment of the quality of life. Soc. Indic. Res. 1978, 5, 475–492. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E. Review of the Satisfaction with Life Scale. Psychol. Assess. 1993, 5, 164–172. [Google Scholar] [CrossRef]
- Kline, R.B. Methodology in the Social Sciences. In Principles, and Practice of Structural Equation Modeling, 3rd ed.; Guilford Press: New York, NY, USA, 2011; ISBN 978-1-60623-876-9. [Google Scholar]
- Gray-Toft, P.; Anderson, J.G. The Nursing Stress Scale: Development of an instrument. J. Psychopathol. Behav. Assess. 1981, 3, 11–23. [Google Scholar] [CrossRef]
- Escribà, V.; Mas, R.; Cardenas, M.; Pérez, S. Validación de la escala de estresores laborales en personal de enfermería: «The nursing stress scale». Gac. Sanit. 1999, 13, 191–200. [Google Scholar] [CrossRef]
- Lake, E.T. Development of the practice environment scale of the nursing work index. Res. Nurs. Heal. 2002, 25, 176–188. [Google Scholar] [CrossRef]
- de Pedro-Gómez, J.; Morales-Asencio, J.M.; Sesé, A.; Bennasar-Veny, M.; Pericas-Beltrán, J.; Miguélez-Chamorro, A. Psychometric testing of the Spanish version of the Practice Environment Scale of the Nursing Work Index in a primary healthcare context. J. Adv. Nurs. 2011, 68, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D. The Development and Validation of a Scale to Measure Self-Compassion. Self Identit. 2003, 2, 223–250. [Google Scholar] [CrossRef]
- García-Campayo, J.; Navarro-Gil, M.; Andrés-Esteban, E.M.; Montero-Marin, J.; López-Artal, L.; DeMarzo, M. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion Scale (SCS). Heal. Qual. Life Outcomes 2014, 12, 4. [Google Scholar] [CrossRef]
- Galiana, L.; Oliver, E.B.; de Simone, G.; Linzitto, J.P.; Benito, E.; Sansó, N. A Brief Measure for the Assessment of Competence in Coping with Death: The Coping with Death Scale Short Version. J. Pain Symptom Manag. 2019, 57, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Pons, D.; Atienza, F.; Balaguer, I.; García-Merita, M.L. Satisfaction with Life Scale: Analysis of Factorial Invariance for Adolescents and Elderly Persons. Percept. Mot. Ski. 2000, 91, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Bentler, P.M.; Hu, L.-T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Enders, C.K. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychol. Methods 2001, 6, 352–370. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.; Sermeus, W.; Heede, K.V.D.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344, e1717. [Google Scholar] [CrossRef] [PubMed]
- Sansó, N.; Galiana, L.; Oliver, A.; Pascual, A.; Sinclair, S.; Benito, E.; Oliver, E.B. Palliative Care Professionals’ Inner Life: Exploring the Relationships Among Awareness, Self-Care, and Compassion Satisfaction and Fatigue, Burnout, and Coping With Death. J. Pain Symptom Manag. 2015, 50, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Burridge, L.H.; Winch, S.; Kay, M.; Henderson, A. Building compassion literacy: Enabling care in primary health care nursing. Coll 2017, 24, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Sansó, N.; Galiana, L.; Oliver, A.; Cuesta, P.; Sánchez, C.; Benito, E. Evaluación de una Intervención Mindfulness en Equipos de Cuidados Paliativos. Psychosoc. Interv. 2018, 27, 081–088. [Google Scholar] [CrossRef]
- Sansó, N.; Galiana, L.; González, B.; Sarmentero, J.; Reynes, M.; Oliver, A.; Garcia-Toro, M. Differential Effects of Two Contemplative Practice-based Programs for Health Care Professionals. Psychosoc. Interv. 2019, 28, 131–138. [Google Scholar] [CrossRef]
- Lizano, E.L. Examining the Impact of Job Burnout on the Health and Well-Being of Human Service Workers: A Systematic Review and Synthesis. Hum. Serv. Organ. Manag. Leadersh. Gov. 2015, 39, 167–181. [Google Scholar] [CrossRef]
- Pipe, T.B.; Bortz, J.J.; Dueck, A.; Pendergast, D.; Buchda, V.; Summers, J. Nurse Leader Mindfulness Meditation Program for Stress Management. JONA J. Nurs. Adm. 2009, 39, 130–137. [Google Scholar] [CrossRef]
| Variables | M (SD) | |
| Age | 40.24 (9.78) | |
| Years in nursing | 3.75 (2.05) | |
| Years in current area/specialty | 2.40 (1.74) | |
| Years in current job position | 1.86 (1.49) | |
| Variables | Categories | N (%) |
| Gender | Women | 158 (75.2) |
| Men | 29 (13.8) | |
| Missing data | 23 (11.0) | |
| Shifts | Without shifts | 97 (46.2) |
| With shifts | 88 (41.9) | |
| Missing data | 25 (11.9) | |
| Working day duration | 8 h | 153 (72.9) |
| 10 h | 5 (2.4) | |
| 12 h | 24 (11.4) | |
| Missing data | 28 (13.3) | |
| Job situation | Public worker | 119 (56.7) |
| Acting official | 29 (13.8) | |
| Temporary worker | 39 (18.6) | |
| Missing data | 23 (11.0) | |
| Variable | M | SD | Min. | Max. | S | K |
|---|---|---|---|---|---|---|
| Nursing stress (scale 0–3) | 1.34 | 0.48 | 0.33 | 2.67 | 0.39 | −0.41 |
| Practice environment (scale 1–4) | 2.68 | 0.53 | 1.17 | 4.00 | −0.28 | −0.09 |
| Physical self-care (scale 1–5) | 3.63 | 0.86 | 1.33 | 5.00 | −0.36 | −0.68 |
| Inner self-care (scale 1–5) | 2.61 | 0.93 | 1.00 | 5.00 | 0.47 | −0.35 |
| Social self-care (scale 1–5) | 3.93 | 0.64 | 2.00 | 5.00 | −0.74 | 0.66 |
| Over-identification (scale 1–5) | 3.01 | 1.01 | 1.00 | 5.00 | −0.02 | −0.75 |
| Self-kindness (scale 1–5) | 3.24 | 0.83 | 1.50 | 5.00 | −0.06 | −0.35 |
| Mindfulness (scale 1–5) | 3.58 | 0.84 | 1.00 | 5.00 | −0.33 | −0.19 |
| Isolation (scale 1–5) | 2.70 | 1.02 | 1.00 | 5.00 | 0.17 | −0.57 |
| Common humanity (scale 1–5) | 3.22 | 0.84 | 1.00 | 5.00 | −0.17 | −0.18 |
| Self-judgement (scale 1–5) | 2.81 | 1.00 | 1.00 | 5.00 | −0.01 | −0.60 |
| Compassion satisfaction (scale 0–15) | 12.02 | 2.82 | 3.00 | 15.00 | −1.22 | 1.28 |
| Compassion fatigue (scale 0–15) | 3.49 | 2.95 | 0.00 | 11.00 | 0.72 | −0.40 |
| Burnout (scale 0–15) | 6.43 | 3.79 | 0.00 | 15.00 | 0.35 | −0.58 |
| Life satisfaction—item 1 (scale 1–5) | 2.90 | 1.14 | 1 | 5 | 0.14 | −0.77 |
| Life satisfaction—item 2 (scale 1–5) | 3.54 | 1.01 | 1 | 5 | −0.58 | −0.30 |
| Life satisfaction—item 3 (scale 1–5) | 3.10 | 0.97 | 1 | 5 | −0.01 | −0.32 |
| Life satisfaction—item 4 (scale 1–5) | 3.11 | 1.00 | 1 | 5 | −0.10 | −0.54 |
| Life satisfaction—item 5 (scale 1–5) | 3.88 | 1.05 | 1 | 5 | −0.76 | −0.12 |
| Life satisfaction (scale 1–5) | 3.30 | 0.89 | 1 | 5 | −0.17 | −0.49 |
| Variable | Gender | Shifts | Working Day Duration | Job Situation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | Without | With | 8 h | 10 h | 12 h | Public Worker | Acting Official | Temporary Working | |
| Nursing stress (scale 0–3) | 1.36(0.47) | 1.25(0.53) | 1.23(0.46) | 1.47(0.48) | 1.33(0.47) | 1.33(0.62) | 1.51(0.53) | 1.36(0.50) | 1.32(0.43) | 1.30(0.45) |
| Practice environment (scale 1–4) | 2.70(0.53) | 2.59(0.55) | 2.85(0.43) | 2.50(0.59) | 2.69(0.53) | 2.71(0.82) | 2.60(0.58) | 2.68(0.56) | 2.63(0.44) | 2.74(0.55) |
| Physical self-care (scale 1–5) | 3.62(0.87) | 3.70(0.84) | 3.79(0.90) | 3.47(0.78) | 3.64(0.87) | 3.92(0.83) | 3.45(0.84) | 3.68(0.87) | 3.82(0.85) | 3.35(0.82) |
| Inner self-care (scale 1–5) | 2.58(0.90) | 2.76(1.09) | 2.69(0.93) | 2.55(0.92) | 2.64(0.90) | 3.13(1.17) | 2.52(1.11) | 2.64(0.96) | 2.50(0.77) | 2.64(0.99) |
| Social self-care (scale 1–5) | 3.98(0.64) | 3.71(0.66) | 4.03(0.53) | 3.84(0.75) | 3.92(0.65) | 4.00(0.86) | 3.93(0.68) | 3.93(0.67) | 3.87(0.71) | 4.02(0.54) |
| Over-identification (scale 1–5) | 3.08(0.97) | 2.67(3.19) | 2.92(0.95) | 3.11(1.09) | 3.01(1.00) | 3.13(1.49) | 2.96(1.11) | 3.01(1.01) | 2.98(1.07) | 3.06(1.03) |
| Self-kindness (scale 1–5) | 3.25(0.82) | 3.19(0.94) | 3.34(0.89) | 3.16(0.75) | 3.23(0.83) | 3.13(0.85) | 3.37(0.98) | 3.28(0.84) | 3.37(0.86) | 3.06(0.82) |
| Mindfulness (scale 1–5) | 3.53(0.86) | 3.84(0.78) | 3.66(0.86) | 3.51(0.84) | 3.57(0.84) | 3.50(0.71) | 3.74(0.98) | 3.58(0.88) | 3.85(0.72) | 3.40(9.82) |
| Isolation (scale 1–5) | 2.77(1.00) | 2.36(1.04) | 2.56(0.92) | 3.88(1.11) | 2.74(1.02) | 3.13(1.31) | 2.30(1.00) | 2.73(1.06) | 2.69(1.05) | 2.64(0.88) |
| Common humanity (scale 1–5) | 3.22(0.85) | 3.23(0.79) | 3.31(0.91) | 3.14(0.76) | 3.20(0.85) | 3.25(0.87) | 3.35(0.90) | 3.29(0.78) | 3.20(1.09) | 3.04(0.82) |
| Self-judgement (scale 1–5) | 2.88(0.95) | 2.51(1.23) | 2.69(1.00) | 3.97(1.01) | 2.80(0.99) | 2.13(1.31) | 2.87(1.04) | 2.85(1.04) | 2.52(0.89) | 2.94(0.97) |
| Compassion satisfaction (scale 0–15) | 12.09(2.78) | 11.68(3.04) | 12.38(2.33) | 11.66(3.28) | 11.92(2.80) | 13.00(2.71) | 12.09(3.12) | 11.94(2.86) | 12.79(2.32) | 11.69(3.04) |
| Compassion fatigue (scale 0–15) | 3.55(2.94) | 3.21(3.06) | 3.15(2.68) | 3.89(3.24) | 3.66(2.91) | 3.00(3.56) | 2.96(3.21) | 3.59(3.07) | 3.32(2.60) | 3.31(2.91) |
| Burnout (scale 0–15) | 6.61(3.70) | 5.56(4.21) | 5.90(3.46) | 7.03(4.12) | 6.62(3.69) | 5.25(4.57) | 5.70(4.15) | 6.85(3.79) | 4.75(3.00) | 6.51(4.10) |
| Life satisfaction—item 1 (scale 1–5) | 2.87(1.12) | 3.04(1.23) | 3.13(1.13) | 2.67(1.10) | 2.89(1.19) | 2.75(0.96) | 3.04(0.98) | 2.92(1.19) | 3.21(1.03) | 2.60(1.04) |
| Life satisfaction—item 2 (scale 1–5) | 3.54(0.99) | 3.54(1.11) | 3.69(0.92) | 3.38(1.10) | 3.53(1.03) | 3.25(0.50) | 3.57(1.04) | 3.54(1.02) | 3.68(1.02) | 3.43(1.01) |
| Life satisfaction—item 3 (scale 1–5) | 3.10(0.93) | 3.11(1.23) | 3.29(0.86) | 2.89(1.06) | 3.07(0.99) | 3.00(0.82) | 3.30(1.02) | 3.14(0.96) | 3.14(1.08) | 2.94(0.95) |
| Life satisfaction—item 4 (scale 1–5) | 3.06(0.97) | 3.32(1.16) | 3.27(0.98) | 2.94(0.99) | 3.09(1.02) | 2.50(0.58) | 3.30(0.97) | 3.16(1.01) | 3.21(1.10) | 2.86(0.91) |
| Life satisfaction—item 5 (scale 1–5) | 3.90(1.03) | 3.82(1.19) | 4.03(0.99) | 3.72(1.12) | 3.82(1.10) | 3.50(0.58) | 4.17(0.83) | 3.94(1.03) | 3.96(1.14) | 3.63(1.06) |
| Life satisfaction (scale 1–5) | 3.29(0.87) | 3.36(1.04) | 3.48(0.85) | 3.12(0.91) | 3.29(0.93) | 3.00(0.37) | 3.48(0.80) | 3.34(0.90) | 3.44(0.92) | 3.08(0.84) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansó, N.; Galiana, L.; Oliver, A.; Tomás-Salvá, M.; Vidal-Blanco, G. Predicting Professional Quality of Life and Life Satisfaction in Spanish Nurses: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4366. https://doi.org/10.3390/ijerph17124366
Sansó N, Galiana L, Oliver A, Tomás-Salvá M, Vidal-Blanco G. Predicting Professional Quality of Life and Life Satisfaction in Spanish Nurses: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(12):4366. https://doi.org/10.3390/ijerph17124366
Chicago/Turabian StyleSansó, Noemí, Laura Galiana, Amparo Oliver, Macià Tomás-Salvá, and Gabriel Vidal-Blanco. 2020. "Predicting Professional Quality of Life and Life Satisfaction in Spanish Nurses: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 12: 4366. https://doi.org/10.3390/ijerph17124366
APA StyleSansó, N., Galiana, L., Oliver, A., Tomás-Salvá, M., & Vidal-Blanco, G. (2020). Predicting Professional Quality of Life and Life Satisfaction in Spanish Nurses: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(12), 4366. https://doi.org/10.3390/ijerph17124366






