Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis
Abstract
1. Introduction
2. Materials and Methods
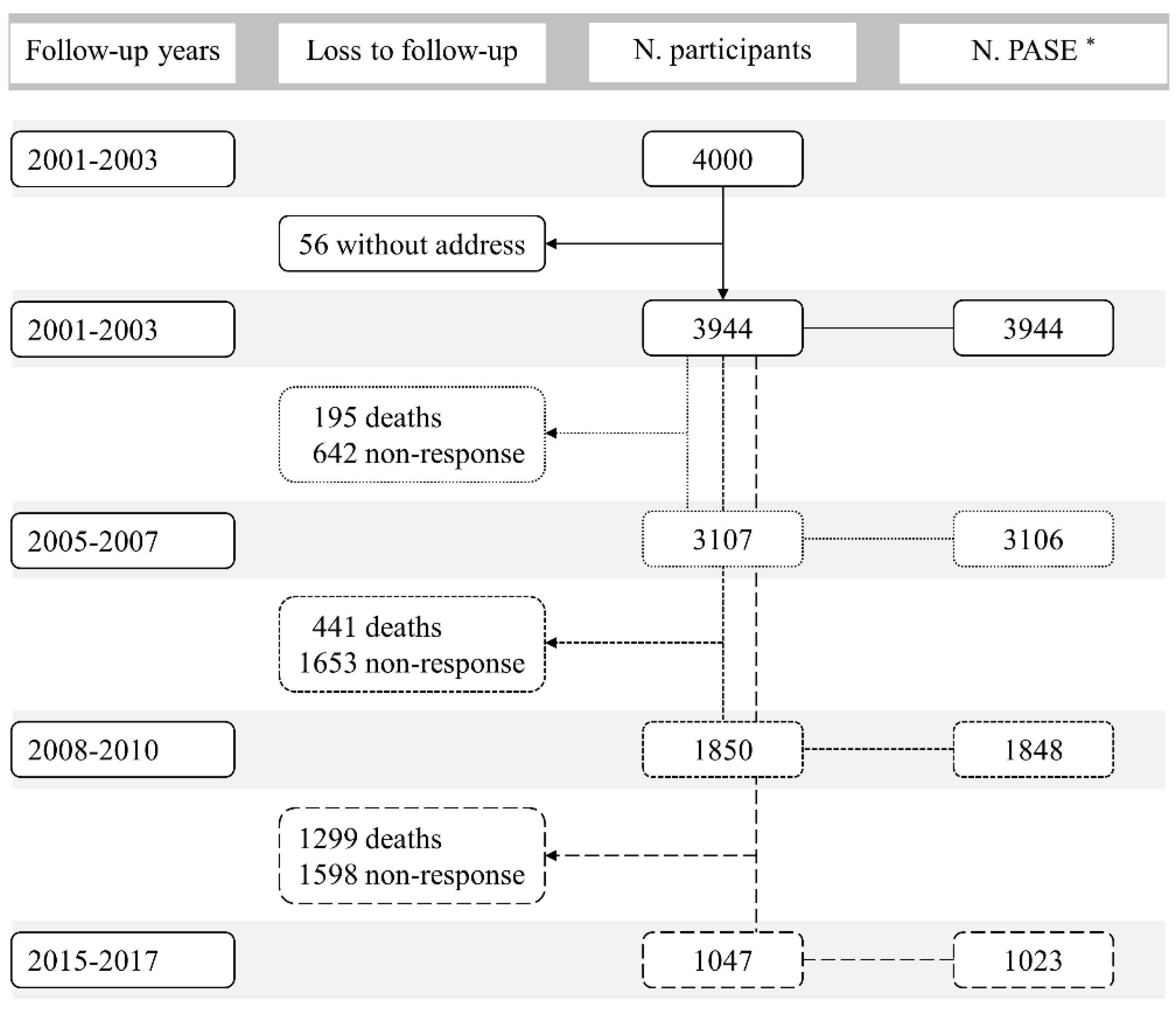
2.1. Study Design and Population
2.2. Measurement of Built Environment
2.3. Self-Reported Physical Activity
2.4. Covariates
2.5. Statistical Analyses
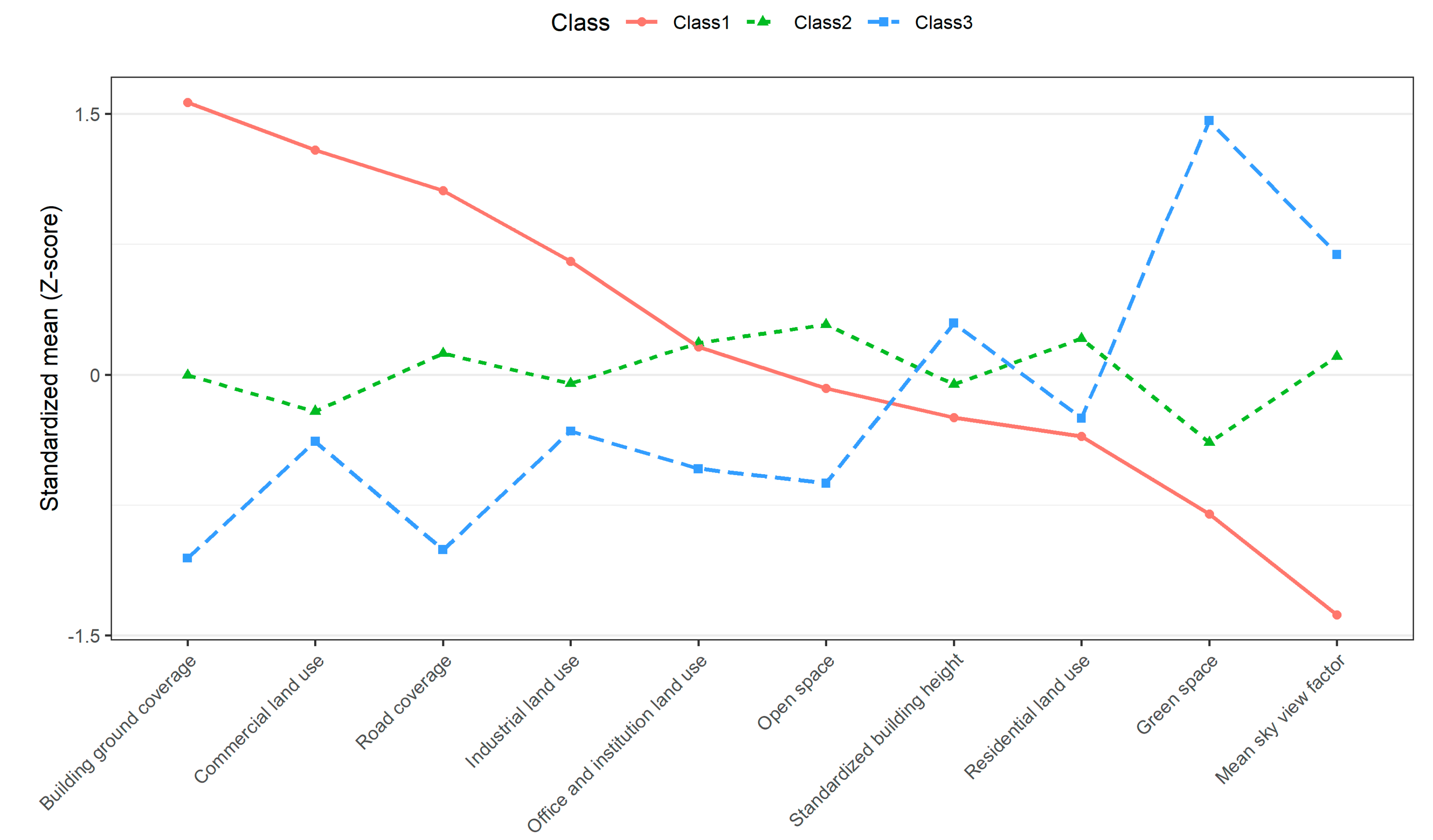
2.5.1. Latent Profile Analysis
2.5.2. Inverse Probability Weighting
2.5.3. Main Analyses
2.5.4. Sensitivity Analyses
3. Results
3.1. Latent Profile Analysis
3.2. Inverse Probability Weighting
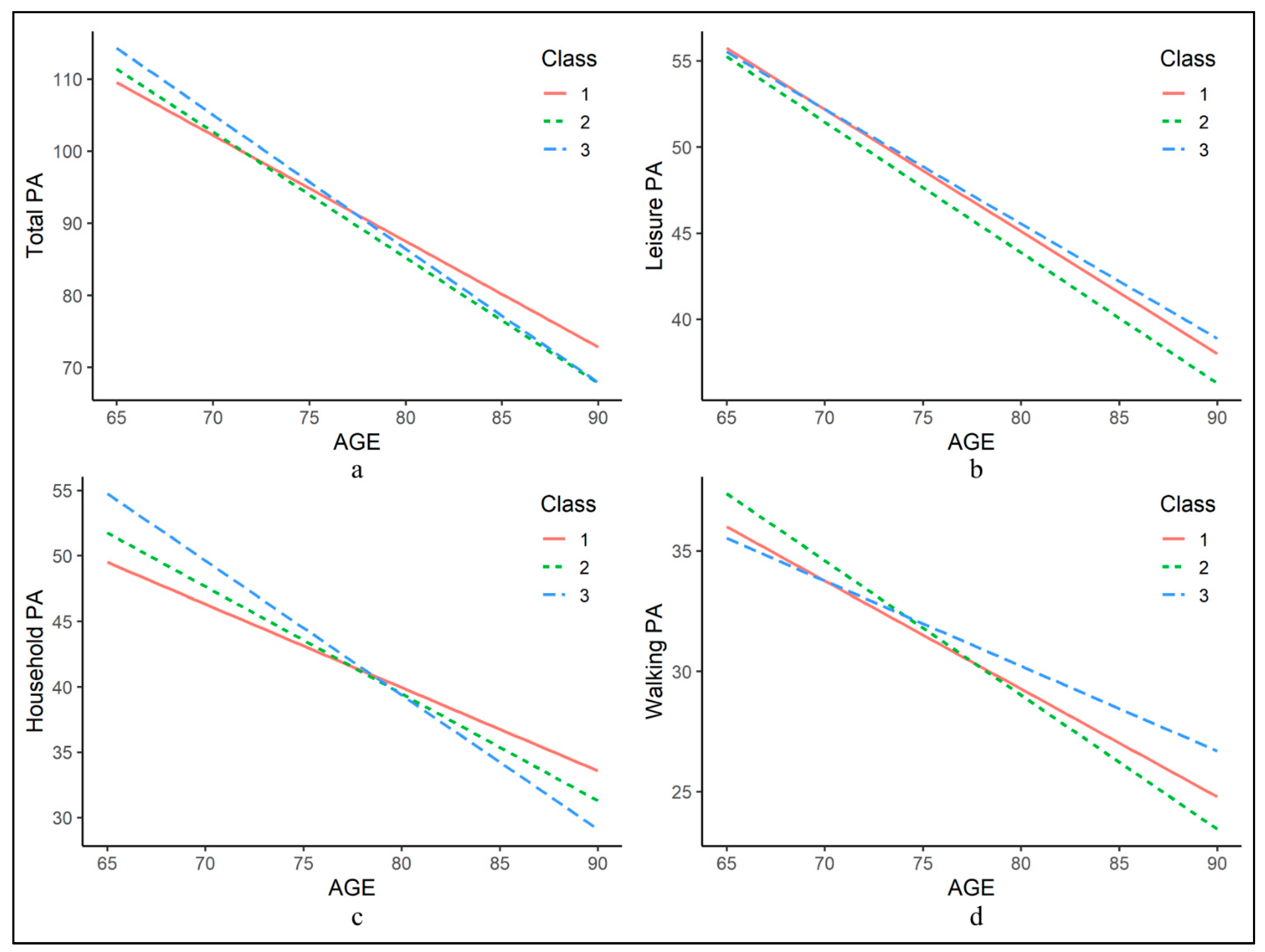
3.3. Main Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Health Observatory (GHO) Data: Prevalence of Insufficient Physical Activity. Available online: https://www.who.int/gho/ncd/risk_factors/physical_activity_text/en/ (accessed on 29 April 2020).
- Li, F. Physical activity and health in the presence of china’s economic growth: Meeting the public health challenges of the aging population. J. Sport Health Sci. 2016, 5, 258–269. [Google Scholar] [CrossRef]
- Keadle, S.K.; McKinnon, R.; Graubard, B.I.; Troiano, R.P. Prevalence and trends in physical activity among older adults in the united states: A comparison across three national surveys. Prev. Med. 2016, 89, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Sallis, J.E.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Publ. Health 2006, 27, 297–322. [Google Scholar] [CrossRef]
- Travert, A.S.; Sidney Annerstedt, K.; Daivadanam, M. Built environment and health behaviors: Deconstructing the black box of interactions-a review of reviews. Int. J. Environ. Res. Public Health 2019, 16, 1454. [Google Scholar] [CrossRef] [PubMed]
- Kondo, M.C.; Fluehr, J.M.; McKeon, T.; Branas, C.C. Urban green space and its impact on human health. Int. J. Environ. Res. Public Health 2018, 15, 445. [Google Scholar] [CrossRef]
- Fong, K.C.; Hart, J.E.; James, P. A review of epidemiologic studies on greenness and health: Updated literature through 2017. Curr. Environ. Health Rep. 2018, 5, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Dalton, A.M.; Wareham, N.; Griffin, S.; Jones, A.P. Neighbourhood greenspace is associated with a slower decline in physical activity in older adults: A prospective cohort study. SSM Popul. Health 2016, 2, 683–691. [Google Scholar] [CrossRef]
- Miralles-Guasch, C.; Dopico, J.; Delclos-Alio, X.; Knobel, P.; Marquet, O.; Maneja-Zaragoza, R.; Schipperijn, J.; Vich, G. Natural landscape, infrastructure, and health: The physical activity implications of urban green space composition among the elderly. Int. J. Environ. Res. Public Health 2019, 16, 3986. [Google Scholar] [CrossRef]
- Josey, M.J.; Moore, S. The influence of social networks and the built environment on physical inactivity: A longitudinal study of urban-dwelling adults. Health Place 2018, 54, 62–68. [Google Scholar] [CrossRef]
- Kim, J.; Lee, H.Y.; Lee, E.Y. Association between built environment and moderate to vigorous physical activity in korean adults: A multilevel analysis. J. Public Health UK 2017, 39, 227–240. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cerin, E.; Conway, T.L.; Adams, M.A.; Frank, L.D.; Pratt, M.; Salvo, D.; Schipperijn, J.; Smith, G.; Cain, K.L.; et al. Physical activity in relation to urban environments in 14 cities worldwide: A cross-sectional study. Lancet 2016, 387, 2207–2217. [Google Scholar] [CrossRef]
- Cerin, E.; Sit, C.H.; Barnett, A.; Johnston, J.M.; Cheung, M.C.; Chan, W.M. Ageing in an ultra-dense metropolis: Perceived neighbourhood characteristics and utilitarian walking in hong kong elders. Public Health Nutr. 2014, 17, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Pelclova, J.; Fromel, K.; Blaha, L.; Zajac-Gawlak, I.; Tlucakova, L. Neighborhood environment and walking for transport and recreation in central european older adults. Acta Gymnica 2012, 42, 49–56. [Google Scholar] [CrossRef]
- Cerin, E.; Lee, K.Y.; Barnett, A.; Sit, C.H.; Cheung, M.C.; Chan, W.M. Objectively-measured neighborhood environments and leisure-time physical activity in chinese urban elders. Prev. Med. 2013, 56, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Cleland, C.; Reis, R.S.; Ferreira Hino, A.A.; Hunter, R.; Fermino, R.C.; Koller de Paiva, H.; Czestschuk, B.; Ellis, G. Built environment correlates of physical activity and sedentary behaviour in older adults: A comparative review between high and low-middle income countries. Health Place 2019, 57, 277–304. [Google Scholar] [CrossRef]
- Frank, L.D.; Sallis, J.F.; Saelens, B.E.; Leary, L.; Cain, K.; Conway, T.L.; Hess, P.M. The development of a walkability index: Application to the neighborhood quality of life study. Br. J. Sports Med. 2010, 44, 924–933. [Google Scholar] [CrossRef]
- Todd, M.; Adams, M.A.; Kurka, J.; Conway, T.L.; Cain, K.L.; Buman, M.P.; Frank, L.D.; Sallis, J.F.; King, A.C. Gis-measured walkability, transit, and recreation environments in relation to older adults‘ physical activity: A latent profile analysis. Prev. Med. 2016, 93, 57–63. [Google Scholar] [CrossRef]
- Berlin, K.S.; Williams, N.A.; Parra, G.R. An introduction to latent variable mixture modeling (part 1): Overview and cross-sectional latent class and latent profile analyses. J. Pediatr. Psychol. 2014, 39, 174–187. [Google Scholar] [CrossRef]
- Green, M.J. Latent class analysis was accurate but sensitive in data simulations. J. Clin. Epidemiol. 2014, 67, 1157–1162. [Google Scholar] [CrossRef]
- Kurka, J.M.; Adams, M.A.; Todd, M.; Colburn, T.; Sallis, J.F.; Cain, K.L.; Glanz, K.; Frank, L.D.; Saelens, B.E. Patterns of neighborhood environment attributes in relation to children‘s physical activity. Health Place 2015, 34, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Todd, M.; Kurka, J.; Conway, T.L.; Cain, K.L.; Frank, L.D.; Sallis, J.F. Patterns of walkability, transit, and recreation environment for physical activity. Am. J. Prev. Med. 2015, 49, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Sallis, J.F.; Kerr, J.; Conway, T.L.; Saelens, B.E.; Frank, L.D.; Norman, G.J.; Cain, K.L. Neighborhood environment profiles related to physical activity and weight status: A latent profile analysis. Prev. Med. 2011, 52, 326–331. [Google Scholar] [CrossRef]
- Norman, G.J.; Adams, M.A.; Kerr, J.; Ryan, S.; Frank, L.D.; Roesch, S.C. A latent profile analysis of neighborhood recreation environments in relation to adolescent physical activity, sedentary time, and obesity. J. Public Health Manag. Pract. 2010, 16, 411–419. [Google Scholar] [CrossRef] [PubMed]
- McDonald, K.; Hearst, M.; Farbakhsh, K.; Patnode, C.; Forsyth, A.; Sirard, J.; Lytle, L. Adolescent physical activity and the built environment: A latent class analysis approach. Health Place 2012, 18, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Ding, D.; Sallis, J.F.; Bowles, H.R.; Ainsworth, B.E.; Bergman, P.; Bull, F.C.; Carr, H.; Craig, C.L.; De Bourdeaudhuij, I.; et al. Patterns of neighborhood environment attributes related to physical activity across 11 countries: A latent class analysis. Int. J. Behavi. Nutr. Phy. 2013, 10, 34. [Google Scholar] [CrossRef]
- Hawkesworth, S.; Silverwood, R.J.; Armstrong, B.; Pliakas, T.; Nanchalal, K.; Jefferis, B.J.; Sartini, C.; Amuzu, A.A.; Wannamethee, S.G.; Ramsay, S.E.; et al. Investigating associations between the built environment and physical activity among older people in 20 uk towns. J. Epidemiol. Commun. 2018, 72, 121–131. [Google Scholar] [CrossRef]
- Adams, M.A.; Sallis, J.F.; Conway, T.L.; Frank, L.D.; Saelens, B.E.; Kerr, J.; Cain, K.L.; King, A.C. Neighborhood environment profiles for physical activity among older adults. Am. J. Health Behav. 2012, 36, 757–769. [Google Scholar] [CrossRef]
- Kwok, T.C.Y.; Su, Y.; Khoo, C.C.; Leung, J.; Kwok, A.; Orwoll, E.; Woo, J.; Leung, P.C. Predictors of non-vertebral fracture in older chinese males and females: Mr. Os and ms. Os (hong kong). J. Bone Miner. Metab. 2017, 35, 330–337. [Google Scholar] [CrossRef]
- Chan, R.; Leung, J.; Woo, J.; Kwok, T. Associations of dietary protein intake on subsequent decline in muscle mass and physical functions over four years in ambulant older chinese people. J. Nutr. Health Aging 2014, 18, 171–177. [Google Scholar] [CrossRef]
- Kwok, A.W.L.; Gong, J.S.; Wang, Y.X.J.; Leung, J.C.S.; Kwok, T.; Griffith, J.F.; Leung, P.C. Prevalence and risk factors of radiographic vertebral fractures in elderly chinese men and women: Results of mr. Os (hong kong) and ms. Os (hong kong) studies. Osteoporos. Int. 2013, 24, 877–885. [Google Scholar] [CrossRef]
- Yu, R.; Wang, D.; Leung, J.; Lau, K.; Kwok, T.; Woo, J. Is neighborhood green space associated with less frailty? Evidence from the mr. And ms. Os (hong kong) study. J. Am. Med. Dir. Assoc. 2018, 19, 528–534. [Google Scholar] [CrossRef]
- Wang, D.; Lau, K.K.L.; Yu, R.; Wong, S.Y.S.; Kwok, T.T.Y.; Woo, J. Neighbouring green space and mortality in community-dwelling elderly hong kong chinese: A cohort study. BMJ Open 2017, 7, e015794. [Google Scholar] [CrossRef]
- Census and Statistics Department. 2006 Population by Census: Thematic Report–Older Persons; Hong Kong Special Administrative Region: Government Logistics Department: Hongkong, China, 2008.
- Dozier, J.; Frew, J. Rapid calculation of terrain parameters for radiation modeling from digital elevation data. IEEE Trans. Geosci. Remote Sens. 1990, 28, 963–969. [Google Scholar] [CrossRef]
- Nichol, J.; Wong, M.S.; Fung, C.; Leung, K.K.M. Assessment of urban environmental quality in a subtropical city using multispectral satellite images. Environ. Plan. B Plan. Des. 2006, 33, 39–58. [Google Scholar] [CrossRef]
- Yu, R.; Leung, J.; Woo, J. Incremental predictive value of sarcopenia for incident fracture in an elderly chinese cohort: Results from the osteoporotic fractures in men (mros) study. J. Am. Med. Dir. Assoc. 2014, 15, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; Smith, K.W.; Jette, A.M.; Janney, C.A. The physical-activity scale for the elderly (pase)—Development and evaluation. J. Clin. Epidemiol. 1993, 46, 153–162. [Google Scholar] [CrossRef]
- Washburn, R.A.; McAuley, E.; Katula, J.; Mihalko, S.L.; Boileau, R.A. The physical activity scale for the elderly (pase): Evidence for validity. J. Clin. Epidemiol. 1999, 52, 643–651. [Google Scholar] [CrossRef]
- Washburn, R.A.; Ficker, J.L. Physical activity scale for the elderly (pase): The relationship with activity measured by a portable accelerometer. J. Sport Med. Phys. Fit. 1999, 39, 336–340. [Google Scholar]
- Vaughan, K.; Miller, W.C. Validity and reliability of the chinese translation of the physical activity scale for the elderly (pase). Disabil. Rehabil. 2013, 35, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Ngai, S.P.; Cheung, R.T.; Lam, P.L.; Chiu, J.K.; Fung, E.Y. Validation and reliability of the physical activity scale for the elderly in chinese population. J. Rehabil. Med. 2012, 44, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Weuve, J.; Tchetgen, E.J.T.; Glymour, M.M.; Beck, T.L.; Aggarwal, N.T.; Wilson, R.S.; Evans, D.A.; de Leon, C.F.M. Accounting for bias due to selective attrition the example of smoking and cognitive decline. Epidemiology 2012, 23, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Conway, T.L.; Cain, K.L.; Carlson, J.A.; Frank, L.D.; Kerr, J.; Glanz, K.; Chapman, J.E.; Saelens, B.E. Neighborhood built environment and socioeconomic status in relation to physical activity, sedentary behavior, and weight status of adolescents. Prev. Med. 2018, 110, 47–54. [Google Scholar] [CrossRef] [PubMed]
- van Heeswijck, T.; Paquet, C.; Kestens, Y.; Thierry, B.; Morency, C.; Daniel, M. Differences in associations between active transportation and built environmental exposures when expressed using different components of individual activity spaces. Health Place 2015, 33, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Qian, F.; Lau, S.S.Y. Urban form and density as indicators for summertime outdoor ventilation potential: A case study on high-rise housing in shanghai. Build. Environ. 2013, 70, 122–137. [Google Scholar] [CrossRef]
- Jamei, E.; Rajagopalan, P.; Seyedmahmoudian, M.; Jamei, Y. Review on the impact of urban geometry and pedestrian level greening on outdoor thermal comfort. Renew. Sust. Energ. Rev. 2016, 54, 1002–1017. [Google Scholar] [CrossRef]
- Woo, J.; Ho, S.C.; Yu, A.L. Lifestyle factors and health outcomes in elderly hong kong chinese aged 70 years and over. Gerontology 2002, 48, 234–240. [Google Scholar] [CrossRef]
- Barnett, A.; Cerin, E.; Cheung, M.C.; Chan, W.M. An in-depth pilot study on patterns, destinations, and purposes of walking in hong kong older adults. J. Aging Phys. Activ. 2015, 23, 144–152. [Google Scholar] [CrossRef]
- Lu, Z.; Harris, T.B.; Shiroma, E.J.; Leung, J.; Kwok, T. Patterns of physical activity and sedentary behavior for older adults with alzheimer’s disease, mild cognitive impairment, and cognitively normal in hong kong. J. Alzheimers Dis. 2018, 66, 1453–1462. [Google Scholar] [CrossRef]
- Hirsch, J.A.; Grengs, J.; Schulz, A.; Adar, S.D.; Rodriguez, D.A.; Brines, S.J.; Roux, A.V.D. How much are built environments changing, and where? Patterns of change by neighborhood sociodemographic characteristics across seven us metropolitan areas. Soc. Sci. Med. 2016, 169, 97–105. [Google Scholar] [CrossRef]
| Median | Interquartile Range | Min | Max | |
|---|---|---|---|---|
| Standardized building height, m | 31.8 | 14.1 | 0.00 | 74.8 |
| Mean sky view factor | 0.62 | 0.15 | 0.25 | 1.00 |
| Building ground coverage, % | 21.0 | 14.0 | 0.00 | 52.0 |
| Green space, % | 13.1 | 29.5 | 0.00 | 100 |
| Open space, % | 5.06 | 8.14 | 0.00 | 47.9 |
| Road coverage, % | 17.2 | 8.56 | 0.00 | 37.9 |
| Industrial land use, % | 0.00 | 1.03 | 0.00 | 38.3 |
| Residential land use, % | 36.9 | 17.0 | 0.00 | 99.5 |
| Commercial land use, % | 0.07 | 1.45 | 0.00 | 32.4 |
| Government, institution and community land use, % | 6.54 | 7.43 | 0.00 | 51.7 |
| Class 1 (N = 665) | Class 2 (N = 2300) | Class 3 (N = 979) | p-Value 1 | |
|---|---|---|---|---|
| Mean (SD) or Number (%) | ||||
| Age, years | 71.9 (4.84) | 72.6 (5.25) | 72.7 (5.26) | 0.004 |
| Sex, female, N (%) | 273 (41.1) | 1182 (51.4) | 517 (52.8) | <0.001 |
| Marital status, N (%) | <0.001 | |||
| Married | 525 (78.9) | 1596 (69.4) | 674 (68.8) | |
| Widowed | 117 (17.6) | 603 (26.2) | 251 (25.6) | |
| Separated or divorced | 10 (1.5) | 51 (2.2) | 27 (2.8) | |
| Single (never married) | 13 (2.0) | 50 (2.2) | 27 (2.8) | |
| Education level, N (%) | <0.001 | |||
| No education | 90 (13.5) | 525 (22.8) | 228 (23.3) | |
| Primary school or below | 308 (46.3) | 1137 (49.4) | 532 (54.3) | |
| Secondary school or above | 267 (40.2) | 638 (27.8) | 219 (22.4) | |
| Years lived in Hong Kong | 53.0 (14.7) | 53.0 (14.7) | 52.1 (15.5) | 0.216 |
| Alcohol drinking, N (%) | 102 (15.3) | 295 (12.8) | 118 (12.1) | 0.137 |
| Smoking, N (%) | 43 (6.5) | 157 (6.8) | 73 (7.5) | 0.711 |
| Number of chronic diseases, N (%) | 0.030 | |||
| 0 | 117 (17.6) | 390 (17.0) | 141 (14.4) | |
| 1 or 2 | 376 (56.5) | 1230 (53.5) | 576 (58.8) | |
| ≥3 | 172 (25.9) | 680 (29.5) | 262 (26.8) | |
| Self-rated health, N (%) | 0.151 | |||
| Very poor, poor or fair | 329 (49.5) | 1223 (53.2) | 530 (54.1) | |
| Good or very good | 336 (50.5) | 1077 (46.8) | 449 (45.9) | |
| Live alone, N (%) | 61 (9.2) | 270 (11.7) | 92 (9.4) | 0.054 |
| Depression, N (%) | 45 (6.8) | 224 (9.7) | 96 (9.8) | 0.052 |
| MMSE | 26.3 (3.19) | 25.5 (3.78) | 25.5 (3.71) | <0.001 |
| CSI-D | 30.6 (1.65) | 30.1 (2.08) | 30.0 (2.13) | <0.001 |
| Model 1 2 | Model 2 3 | Model 3 4 | |||
|---|---|---|---|---|---|
| Baseline | 5-Year Change | Baseline | 5-Year Change | 5-Year Change | |
| Total PA | |||||
| Class 2 vs. 1 | 0.07 (−3.05, 3.18) | −0.83 (−2.89, 1.22) | 0.22 (−2.85, 3.29) | −0.87 (−2.85, 1.12) | 0.16 (−1.66, 1.99) |
| Class 3 vs. 1 | 2.25 (−1.34, 5.83) | −1.76 (−4.13, 0.60) | 2.37 (−1.18, 5.91) | −1.23 (−3.51, 1.05) | −0.17 (−2.27, 1.92) |
| Class 3 vs. 2 | 2.18 (−0.59, 4.95) | −0.93 (−2.73, 0.87) | 2.14 (−0.58, 4.87) | −0.36 (−2.10, 1.37) | −0.34 (−1.93, 1.25) |
| Leisure PA | |||||
| Class 2 vs. 1 | −0.33 (−2.23, 1.57) | −0.41 (−1.69, 0.87) | −0.34 (−2.21, 1.54) | −0.39 (−1.65, 0.86) | −0.26 (−1.43, 0.91) |
| Class 3 vs. 1 | 0.64 (−1.54, 2.83) | 0.02 (−1.45, 1.49) | 0.60 (−1.57, 2.76) | 0.30 (−1.13, 1.74) | 0.68 (−0.66, 2.03) |
| Class 3 vs. 2 | 0.97 (−0.72, 2.66) | 0.43 (−0.69, 1.55) | 0.93 (−0.73, 2.60) | 0.70 (−0.40, 1.79) | 0.94 (−0.08, 1.97) |
| Household PA | |||||
| Class 2 vs. 1 | 0.54 (−1.29, 2.36) | −0.20 (−1.41, 1.00) | 0.69 (−1.12, 2.51) | −0.22 (−1.39, 0.95) | 0.44 (−0.64, 1.51) |
| Class 3 vs. 1 | 2.05 (−0.05, 4.15) | −1.69 (−3.08, −0.31) * | 2.20 (0.10, 4.29) * | −1.39 (−2.74, −0.04) * | −0.83 (−2.06, 0.40) |
| Class 3 vs. 2 | 1.52 (−0.10, 3.14) | −1.49 (−2.55, −0.44) ** | 1.50 (−0.10, 3.11) | −1.17 (−2.20, −0.14) * | −1.26 (−2.20, −0.33) ** |
| Walking PA | |||||
| Class 2 vs. 1 | 1.05 (−0.32, 2.41) | −0.60 (−1.54, 0.35) | 0.91 (−0.44, 2.27) | −0.58 (−1.51, 0.36) | −0.46 (−1.33, 0.42) |
| Class 3 vs. 1 | 0.77 (−0.80, 2.34) | 0.41 (−0.67, 1.50) | 0.58 (−0.98, 2.15) | 0.56 (−0.52, 1.63) | 0.73 (−0.27, 1.73) |
| Class 3 vs. 2 | −0.28 (−1.49, 0.93) | 1.01 (0.18, 1.83) * | −0.33 (−1.54, 0.87) | 1.13 (0.31, 1.95) ** | 1.19 (0.42, 1.95) ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, J.-S.; Chan, F.Y.-F.; Leung, J.; Yu, B.; Lu, Z.-H.; Woo, J.; Kwok, T.; Lau, K.K.-L. Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis. Int. J. Environ. Res. Public Health 2020, 17, 4275. https://doi.org/10.3390/ijerph17124275
Lin J-S, Chan FY-F, Leung J, Yu B, Lu Z-H, Woo J, Kwok T, Lau KK-L. Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis. International Journal of Environmental Research and Public Health. 2020; 17(12):4275. https://doi.org/10.3390/ijerph17124275
Chicago/Turabian StyleLin, Jie-Sheng, Faye Ya-Fen Chan, Jason Leung, Blanche Yu, Zhi-Hui Lu, Jean Woo, Timothy Kwok, and Kevin Ka-Lun Lau. 2020. "Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis" International Journal of Environmental Research and Public Health 17, no. 12: 4275. https://doi.org/10.3390/ijerph17124275
APA StyleLin, J.-S., Chan, F. Y.-F., Leung, J., Yu, B., Lu, Z.-H., Woo, J., Kwok, T., & Lau, K. K.-L. (2020). Longitudinal Association of Built Environment Pattern with Physical Activity in a Community-Based Cohort of Elderly Hong Kong Chinese: A Latent Profile Analysis. International Journal of Environmental Research and Public Health, 17(12), 4275. https://doi.org/10.3390/ijerph17124275







