Injury Severity and Psychological Distress Sustained in the Aftermath of the Attacks of 11 September 2001 Predict Somatic Symptoms in World Trade Center Health Registry Enrollees Sixteen Years Later
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Design
2.2. Analytic Sample
2.3. Study Variables
2.3.1. Outcome Measure
2.3.2. Covariates
2.4. Statistical Analysis
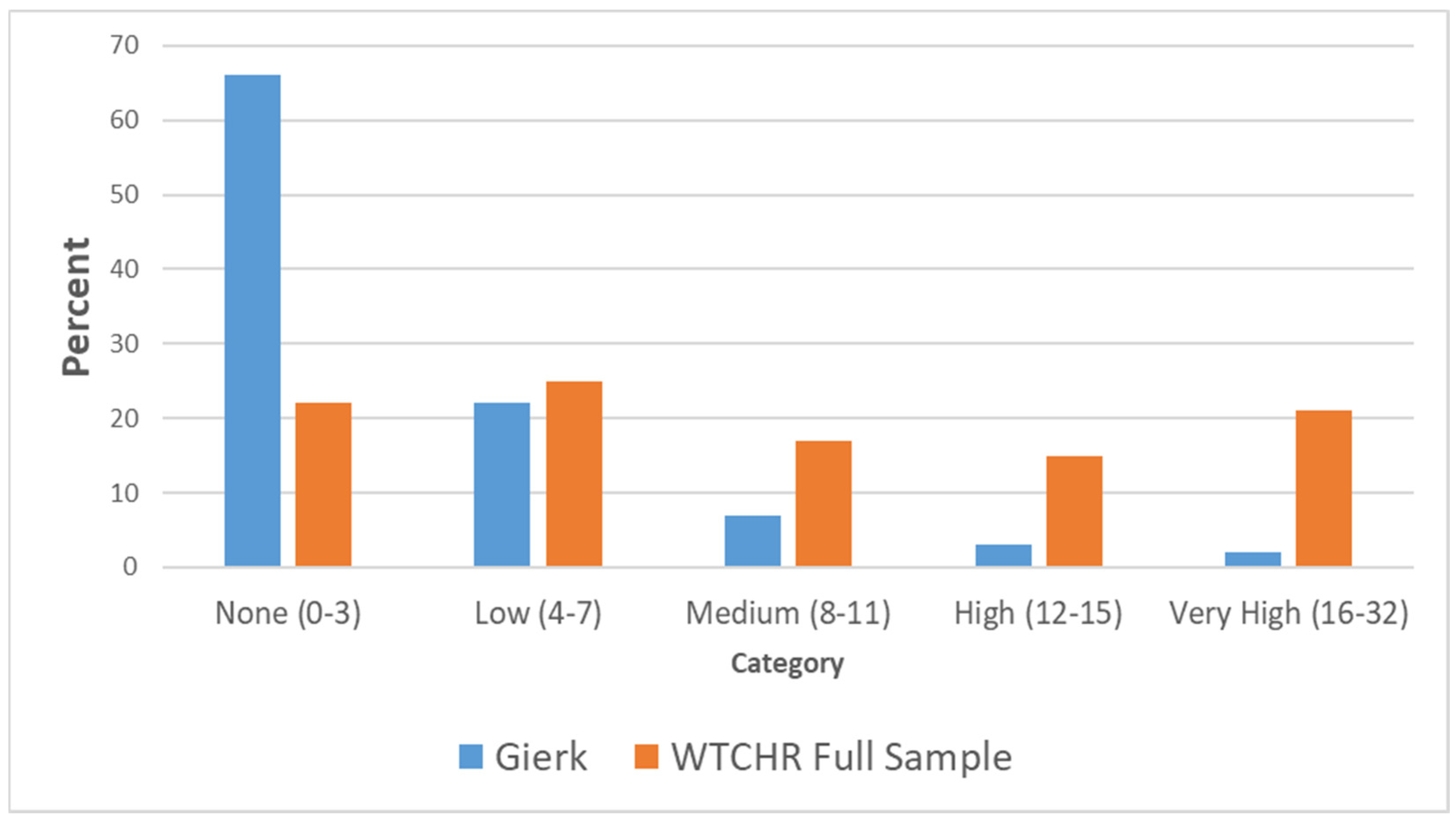
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| WTCHR | World Trade Center Health Registry |
| PTSD | Post-traumatic Stress Disorder |
| CI | Confidence Interval |
| DSM-IV | Diagnostic Statistical Manual-IV |
| PCL-S | Posttraumatic Stress Disorder Check List–Specific |
| PHQ | Patient Health Questionnaire -8 |
| K6 | KesslerK6 Scale |
| SSS-8 | Somatic Symptom Scale–8 |
References
- Banauch, G.I.; Hall, C.; Weiden, M.; Cohen, H.W.; Aldrich, T.K.; Christodoulou, V.; Arcentales, N.; Kelly, K.J.; Prezant, D.J. Pulmonary function after exposure to the World Trade Center collapse in the New York City Fire Department. Am. J. Respir. Crit. Care Med. 2006, 174, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Brackbill, R.M.; Thorpe, L.E.; DiGrande, L.; Perrin, M.; Sapp, J.H., II; Wu, D.; Campolucci, S.; Walker, D.J.; Cone, J.; Pulliam, P.; et al. Surveillance for World Trade Center disaster health effects among survivors of collapsed and damaged buildings. MMWR Surveill. Summ. 2006, 55, 1–18. [Google Scholar] [PubMed]
- Brackbill, R.M.; Hadler, J.L.; DiGrande, L.; Ekenga, C.C.; Farfel, M.R.; Friedman, S.; Perlman, S.E.; Stellman, S.D.; Walker, D.J.; Wu, D.; et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA 2009, 302, 502–516. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.M.; Farfel, M.R.; Maslow, C.; Jordan, H.T.; Li, J.; Alper, H.; Cone, J.E.; Stellman, S.D.; Brackbill, R.M. Risk factors for and consequences of persistent lower respiratory symptoms among World Trade Center Health Registrants 10 years after the disaster. Occup. Environ. Med. 2016, 73, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Herbert, R.; Landrigan, P.; Markowitz, S.B.; Moline, J.M.; Savitz, D.A.; Todd, A.C.; Udasin, I.G.; Wisnivesky, J.P. Increased rates of asthma among World Trade Center disaster responders. Am. J. Ind. Med. 2012, 55, 44–53. [Google Scholar] [CrossRef]
- Alper, H.E.; Yu, S.; Stellman, S.D.; Brackbill, R.M. Injury, intense dust exposure, and chronic disease among survivors of the World Trade Center terrorist attacks of September 11, 2001. Inj. Epidemiol. 2017, 4, 17. [Google Scholar] [CrossRef]
- Li, J.; Alper, H.E.; Gargano, L.M.; Maslow, C.B.; Brackbill, R.M. Re-experiencing 9/11-Related PTSD symptoms following exposure to hurricane sandy. Int. J. Emerg. Ment. Health 2018, 20. [Google Scholar] [CrossRef]
- Yu, S.; Alper, H.E.; Nguyen, A.-M.; Brackbill, R.M. Risk of stroke among survivors of the september 11, 2001, world trade center disaster. J. Occup. Environ. Med. 2018, 60, e371–e376. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Feder, A.; Singh, R.; Schechter, C.B.; Bromet, E.J.; Katz, C.L.; Reissman, D.B.; Ozbay, F.; Sharma, V.; Crane, M.; et al. Trajectories of PTSD risk and resilience in World Trade Center responders: An 8-year prospective cohort study. Psychol. Med. 2014, 44, 205–219. [Google Scholar] [CrossRef]
- Remch, M.; Laskaris, Z.; Flory, J.; Mora-McLaughlin, C.; Morabia, A. Post-traumatic stress disorder and cardiovascular diseases: A cohort study of men and women involved in cleaning the debris of the world trade center complex. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e004572. [Google Scholar] [CrossRef]
- Li, J.; Brackbill, R.M.; Liao, T.S.; Qiao, B.; Cone, J.E.; Farfel, M.R.; Hadler, J.L.; Kahn, A.R.; Konty, K.J.; Stayner, L.T.; et al. Ten-year cancer incidence in rescue/recovery workers and civilians exposed to the September 11, 2001 terrorist attacks on the World Trade Center. Am. J. Ind. Med. 2016, 59, 709–721. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, E.J.; Christos, P.J.; Gerber, L.M.; Reilly, J.P.; Moran, W.F.; Einstein, A.J.; Neugut, A.I. NYPD cancer incidence rates 1995–2014 encompassing the entire world trade center cohort. J. Occup. Environ. Med. 2015, 57, e101–e113. [Google Scholar] [CrossRef] [PubMed]
- Dyster-Aas, J.; Arnberg, F.K.; Lindam, A.; Johannesson, K.B.; Lundin, T.; Michel, P.-O. Impact of physical injury on mental health after the 2004 Southeast Asia tsunami. Nord. J. Psychiatry 2012, 66, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Brackbill, R.M.; Cone, J.E.; Farfel, M.R.; Stellman, S.D. Chronic physical health consequences of being injured during the terrorist attacks on World Trade Center on September 11, 2001. Am. J. Epidemiol. 2014, 179, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Gargano, L.M.; Gershon, R.R.; Brackbill, R.M. Quality of life of persons injured on 9/11: Qualitative analysis from the world trade center health registry. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Brackbill, R.M.; Alper, H.E.; Frazier, P.; Gargano, L.M.; Jacobson, M.H.; Solomon, A. An assessment of long-term physical and emotional quality of life of persons injured on 9/11/2001. Int. J. Environ. Res. Public Health 2019, 16, 1054. [Google Scholar] [CrossRef]
- Kohlmann, S.; Gierk, B.; Hümmelgen, M.; Blankenberg, S.; Löwe, B. Somatic symptoms in patients with coronary heart disease: Prevalence, risk factors, and quality of life. JAMA Intern. Med. 2013, 173, 1469–1471. [Google Scholar] [CrossRef]
- Kroenke, K.; Zhong, X.; Theobald, D.; Wu, J.; Tu, W.; Carpenter, J.S. Somatic symptoms in patients with cancer experiencing pain or depression: Prevalence, disability, and health care use. Arch. Intern. Med. 2010, 170, 1686–1694. [Google Scholar] [CrossRef]
- Kroenke, K.; Jackson, J.L.; Chamberlin, J. Depressive and anxiety disorders in patients presenting with physical complaints: Clinical predictors and outcome. Am. J. Med. 1997, 103, 339–347. [Google Scholar] [CrossRef]
- Barsky, A.J.; Orav, E.J.; Bates, D.W. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch. Gen. Psychiatry 2005, 62, 903–910. [Google Scholar] [CrossRef]
- North, C.S.; Kawasaki, A.; Spitznagel, E.L.; Hong, B.A. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J. Nerv. Ment. Dis. 2004, 192, 823–829. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, B.; Grievink, L.; Yzermans, J.; Lebret, E. Medically unexplained physical symptoms in the aftermath of disasters. Epidemiol. Rev. 2005, 27, 92–106. [Google Scholar] [CrossRef] [PubMed]
- Andreski, P.; Chilcoat, H.; Breslau, N. Post-traumatic stress disorder and somatization symptoms: A prospective study. Psychiatry Res. 1998, 79, 131–138. [Google Scholar] [CrossRef]
- Myrtveit, S.M.; Skogen, J.C.; Wenzel, H.G.; Mykletun, A. Somatic symptoms beyond those generally associated with a whiplash injury are increased in self-reported chronic whiplash. A population-based cross sectional study: The Hordaland Health Study (HUSK). BMC Psychiatry 2012, 12, 129. [Google Scholar] [CrossRef]
- Farfel, M.; DiGrande, L.; Brackbill, R.; Prann, A.; Cone, J.; Friedman, S.; Walker, D.J.; Pezeshki, G.; Thomas, P.; Galea, S.; et al. An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees. J. Urban Health 2008, 85, 880–909. [Google Scholar] [CrossRef]
- Jacobson, M.H.; Brackbill, R.M.; Frazier, P.; Gargano, L.M. Conducting a study to assess the long-term impacts of injury after 9/11: Participation, recall, and description. Inj. Epidemiol. 2019, 6, 8. [Google Scholar] [CrossRef]
- Gierk, B.; Kohlmann, S.; Kroenke, K.; Spangenberg, L.; Zenger, M.; Brähler, E.; Löwe, B. The somatic symptom scale-8 (SSS-8): A brief measure of somatic symptom burden. JAMA Intern. Med. 2014, 174, 399–407. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Stolk, R.P.; Lowe, B.; Rief, W.; BioSHaRE; White, P.D.; Rosmalen, J.G.M. How to assess common somatic symptoms in large-scale studies: A systematic review of questionnaires. J. Psychosom. Res. 2013, 74, 459–468. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Caramanica, K.; Brackbill, R.M.; Stellman, S.D.; Farfel, M.R. Posttraumatic stress disorder after hurricane sandy among persons exposed to the 9/11 disaster. Int. J. Emerg. Ment. Health 2015, 17, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Ginzburg, K.; Solomon, Z. Trajectories of stress reactions and somatization symptoms among war veterans: A 20-year longitudinal study. Psychol. Med. 2011, 41, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Welch, A.E.; Caramanica, K.; Maslow, C.B.; Brackbill, R.M.; Stellman, S.D.; Farfel, M.R. Trajectories of PTSD Among Lower Manhattan Residents and Area Workers Following the 2001 World Trade Center Disaster, 2003–2012. J. Trauma. Stress 2016, 29, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Maslow, C.B.; Caramanica, K.; Welch, A.E.; Stellman, S.D.; Brackbill, R.M.; Farfel, M.R. Trajectories of scores on a screening instrument for PTSD among world trade center rescue, recovery, and clean-up workers. J. Trauma. Stress 2015, 28, 198–205. [Google Scholar] [CrossRef]
- Nader, A. Relationship between somatic symptoms, peripheral inflammation, and clinical outcomes after traumatic injury. Brain Behav. Immun. 2017, 66, e26. [Google Scholar] [CrossRef]
- Irwin, M.R. Inflammation at the intersection of behavior and somatic symptoms. Psychiatr. Clin. N. Am. 2011, 34, 605–620. [Google Scholar] [CrossRef]
- Kurlansik, S.L.; Maffei, M.S. Somatic symptom disorder. Am. Fam. Physician 2016, 93, 49–54. [Google Scholar]
- Mahaffey, B.L.; Gonzalez, A.; Farris, S.G.; Zvolensky, M.J.; Bromet, E.J.; Luft, B.J.; Kotov, R. Understanding the connection between posttraumatic stress symptoms and respiratory problems: Contributions of anxiety sensitivity. J. Trauma. Stress 2017, 30, 71–79. [Google Scholar] [CrossRef][Green Version]
- Bermingham, S.L.; Cohen, A.; Hague, J.; Parsonage, M. The cost of somatisation among the working-age population in England for the year 2008–2009. Ment. Health Fam. Med. 2010, 7, 71–84. [Google Scholar]
- Bauer, A.M.; Chen, C.N.; Alegria, M. Prevalence of physical symptoms and their association with race/ethnicity and acculturation in the United States. Gen. Hosp. Psychiatry 2012, 34, 323–331. [Google Scholar] [CrossRef]
- Yu, S.; Brackbill, R.M.; Stellman, S.D.; Ghuman, S.; Farfel, M.R. Evaluation of non-response bias in a cohort study of World Trade Center terrorist attack survivors. BMC Res. Notes 2015, 8, 42. [Google Scholar] [CrossRef] [PubMed]
- Roennenberg, C.; Sattel, H.; Schaefert, R.; Henningsen, P.; Hausteiner-Wiehle, C. Functional somatic symptoms—Clinical practice guideline. Dtsch. Arztebl. Int. 2019, 116, 553–560. [Google Scholar]
| Characteristic | Total | SSS-8 Total Sore | ||
|---|---|---|---|---|
| n | % | Mean | SD | |
| Total Sample | 2322 | 100 | 9.72 | 7.17 |
| Injury Severity | ||||
| None | 1547 | 65.62 | 7.76 | 6.02 |
| Low | 100 | 4.31 | 11.06 | 6.91 |
| Medium | 369 | 15.89 | 13.74 | 7.26 |
| High | 306 | 13.18 | 14.29 | 7.54 |
| K6 Trajectory | ||||
| Resilient | 556 | 23.94 | 5.00 | 4.88 |
| Low-stable | 1339 | 57.67 | 9.75 | 6.31 |
| Moderate increasing | 226 | 9.73 | 16.20 | 7.16 |
| High Decreasing | 201 | 8.66 | 15.17 | 7.08 |
| Gender | ||||
| Male | 1315 | 56.63 | 8.99 | 6.86 |
| Female | 1007 | 43.37 | 10.60 | 7.22 |
| Age at 9/11 | ||||
| 0–17 | 7 | 0.30 | 7.33 | 6.12 |
| 18–24 | 105 | 4.52 | 8.26 | 6.42 |
| 25–44 | 1194 | 51.42 | 10.06 | 7.37 |
| 45–64 | 998 | 42.98 | 9.39 | 6.76 |
| 65+ | 18 | 0.78 | 10.41 | 4.87 |
| Race | ||||
| White | 1779 | 76.61 | 9.13 | 6.79 |
| Black | 215 | 9.26 | 11.32 | 7.76 |
| Hispanic | 224 | 9.65 | 13.00 | 7.37 |
| Asian | 86 | 3.70 | 9.20 | 7.09 |
| Other | 18 | 0.78 | 7.11 | 6.88 |
| Education | ||||
| Less Than or High School | 330 | 14.21 | 12.37 | 7.60 |
| Some College | 470 | 20.24 | 11.64 | 7.42 |
| College or Post-Grad | 1522 | 65.55 | 8.52 | 6.53 |
| Income | ||||
| 0 ≤ 25 K | 135 | 5.81 | 12.08 | 8.45 |
| 25 ≤ 50 K | 334 | 14.38 | 12.14 | 7.70 |
| 50 ≤ 75 K | 497 | 21.40 | 10.30 | 6.92 |
| 75 ≤ 150 K | 933 | 40.18 | 9.09 | 6.76 |
| ≥150 K | 423 | 18.22 | 7.69 | 6.03 |
| Eligibility Group | ||||
| Rescue/Recovery | 535 | 23.04 | 11.03 | 7.52 |
| Resident | 264 | 11.37 | 8.66 | 6.60 |
| Area Worker | 1330 | 57.28 | 9.33 | 6.89 |
| Passerby | 193 | 8.31 | 9.79 | 7.09 |
| Marital Status at Wave 4 | ||||
| Married/Living | 1592 | 69.10 | 9.24 | 6.98 |
| Divorced/Separated/Widowed | 712 | 30.90 | 10.69 | 7.15 |
| Social Support at Wave 4 | ||||
| Low | 1280 | 56.16 | 11.83 | 7.30 |
| High | 999 | 43.84 | 8.03 | 6.39 |
| Stressful Events | ||||
| None | 1514 | 65.23 | 8.49 | 6.59 |
| Low | 696 | 29.99 | 11.53 | 7.11 |
| High | 111 | 4.78 | 14.59 | 8.34 |
| Chronic Physical Diseases–Pre/Post-9/11 | ||||
| 0 | 689 | 29.67 | 7.41 | 6.07 |
| 1 | 747 | 32.17 | 8.74 | 6.56 |
| 2 or more | 886 | 38.16 | 12.28 | 7.38 |
| Chronic Mental Diseases–Pre-9/11 | ||||
| No | 2131 | 91.77 | 9.61 | 7.11 |
| Yes | 191 | 8.23 | 10.55 | 6.50 |
| Characteristic * | Somatic Symptoms | ||
|---|---|---|---|
| b | CI (L) | CI (U) | |
| Injury Severity | |||
| None | Ref | ||
| Low | 1.5 | 0.3 | 2.7 |
| Medium | 3.1 | 2.4 | 3.8 |
| High | 3.7 | 2.9 | 4.5 |
| K6 Trajectory | |||
| Resilient | Ref | ||
| Low-stable | 3.3 | 2.7 | 3.9 |
| Moderate increasing | 8.2 | 7.2 | 9.2 |
| High decreasing | 6.4 | 5.4 | 7.4 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alper, H.E.; Gargano, L.M.; Cone, J.E.; Brackbill, R.M. Injury Severity and Psychological Distress Sustained in the Aftermath of the Attacks of 11 September 2001 Predict Somatic Symptoms in World Trade Center Health Registry Enrollees Sixteen Years Later. Int. J. Environ. Res. Public Health 2020, 17, 4232. https://doi.org/10.3390/ijerph17124232
Alper HE, Gargano LM, Cone JE, Brackbill RM. Injury Severity and Psychological Distress Sustained in the Aftermath of the Attacks of 11 September 2001 Predict Somatic Symptoms in World Trade Center Health Registry Enrollees Sixteen Years Later. International Journal of Environmental Research and Public Health. 2020; 17(12):4232. https://doi.org/10.3390/ijerph17124232
Chicago/Turabian StyleAlper, Howard E., Lisa M. Gargano, James E. Cone, and Robert M. Brackbill. 2020. "Injury Severity and Psychological Distress Sustained in the Aftermath of the Attacks of 11 September 2001 Predict Somatic Symptoms in World Trade Center Health Registry Enrollees Sixteen Years Later" International Journal of Environmental Research and Public Health 17, no. 12: 4232. https://doi.org/10.3390/ijerph17124232
APA StyleAlper, H. E., Gargano, L. M., Cone, J. E., & Brackbill, R. M. (2020). Injury Severity and Psychological Distress Sustained in the Aftermath of the Attacks of 11 September 2001 Predict Somatic Symptoms in World Trade Center Health Registry Enrollees Sixteen Years Later. International Journal of Environmental Research and Public Health, 17(12), 4232. https://doi.org/10.3390/ijerph17124232




