1. Introduction
Ovarian cancer is the second and third most common gynecologic malignancy in developed and developing countries, respectively [
1]. The most common histological type is epithelial [
2]. Because of its non-specific symptoms and non-useful screening methods, approximately 70–75% cases are at advanced stages at the time of diagnosis. Advanced epithelial ovarian, fallopian tubal, and peritoneal cancer (EOC) is characterized by a high recurrence rate within two years after primary management and a low five-year survival rate [
1].
Currently, the Federation of Gynecology and Obstetrics (FIGO) revised the staging system of EOC since 2014 [
3]. In early stage, stage IC was separated into three sub-categories and stage IIC was removed. In advanced disease, solitary retroperitoneal lympho nodes (LN) metastases without peritoneal disease was re-staged as IIIA1. Retroperitoneal spread of EOC seems to have a better prognosis than intraperitoneal tumor dissemination. Occasionally, retroperitoneal LN dissection would not be performed if peritoneal carcinomatosis is encountered during a primary or interval debulking operation, which are cases with major medical problems or unstable hemodynamic condition during surgery.
Primary debulking surgery followed by systemic chemotherapy is the preferred treatment for advanced EOC. Advancements in systemic therapies, including chemotherapy and anti-vascular target therapy, have considerably improved the outcomes of patients with advanced EOC. The most promising results have come from the Gynecologic Oncology Group (GOG) trials in the United States, which led to increased progression-free survival (PFS) and overall survival (OS) since 1996. Addition of paclitaxel in platinum-based regimens was found to lead to improved outcomes compared with the traditional regimen of cyclophosphamide plus cisplatin [
4]. A 3-h infusion of paclitaxel plus carboplatin had equal PFS but less comorbidity than a 24-h infusion of paclitaxel plus cisplatin in GOG-158 in 2003 [
5]. Intraperitoneal chemotherapy with paclitaxel and cisplatin in optimally debulked patients with EOC had promising PFS in a phase-3 trial of GOG-175 in 2006 [
6]. Schedule modification of weekly infusion of paclitaxel plus three-week carboplatin was studied in Japan’s GOG (JGOG-3016), which revealed substantial improvement in PFS and OS when compared with other trials [
7]. Adding anti-vascular bevacizumab (Genentech, South San Francisco, CA, USA) in the traditional three-weekly paclitaxel–carboplatin chemotherapy plus maintenance also led to better PFS in GOG-218 and ICON-7 [
8,
9]. Nevertheless, determination of the most effective chemotherapy regimen is challenging because of a lack of more substantial randomized trials and the unfeasibility of a direct cross-trial comparison.
In this study, with an aim to provide useful data for selecting the best treatment approach in real-world practice, we, retrospectively, evaluated the factors that could interfere with outcomes of patients with stage III and IV EOC.
4. Discussion
In 2016, 1507 newly diagnosed EOC cases in Taiwan based on the cancer registry from Health Promotion Administration, the Ministry of Health and Welfare [
13]. In general, approximately 70–75% of cases with EOC present at an advanced stage (≥IIIA). However, in our institute, only half of the cases with EOC had an advanced stage at the time of diagnosis. A high recurrence rate within two years after primary management and low five-year survival rate in advanced EOC are the same as those in Western countries [
14].
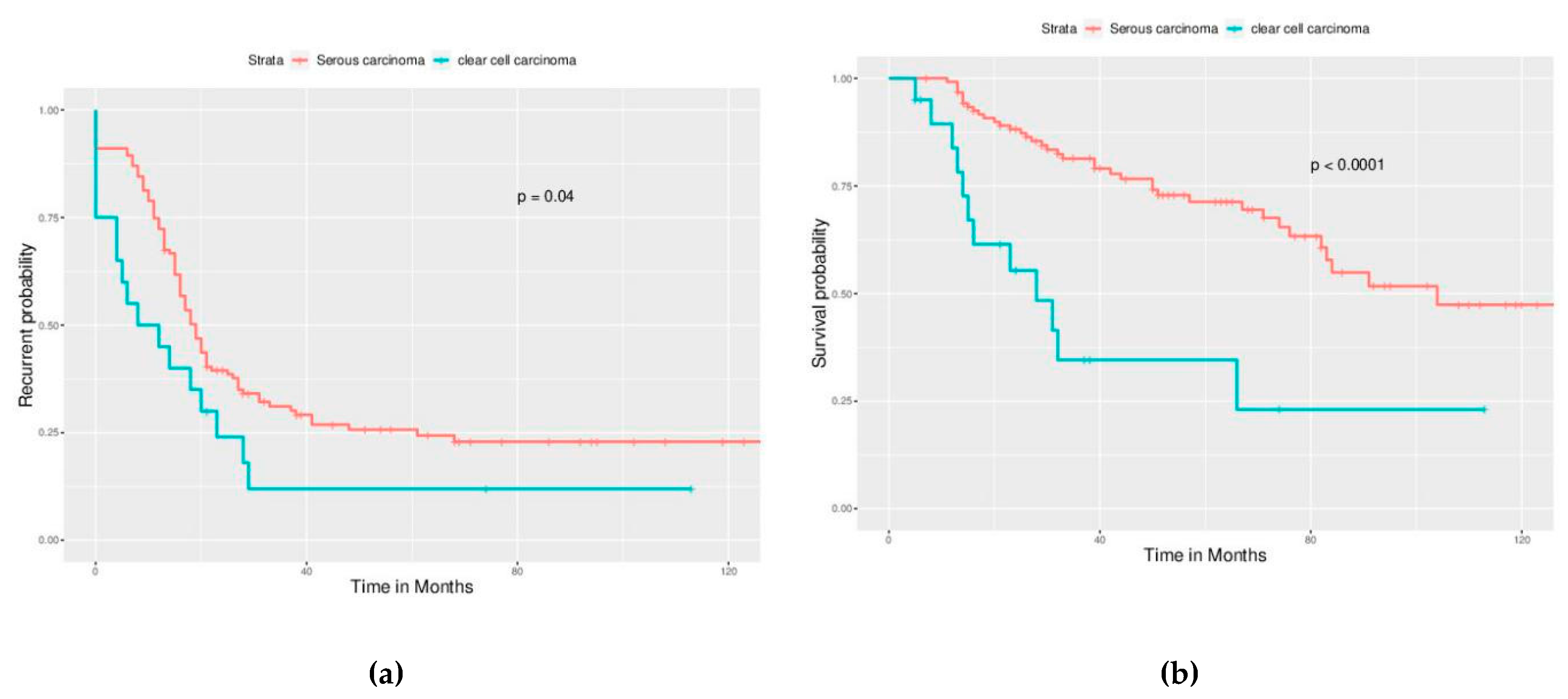
Serous carcinoma is the most common histological type in EOC worldwide. A higher incidence of clear cell carcinoma is observed in East and South Asian countries than in Western countries [
15,
16]. Ovarian clear cell carcinoma is often diagnosed at an early stage. In our cases with advanced EOC, the clear cell type was the second most common cell type (10.4%). Shu et al. reported that the median OS for stage III/IV ovarian clear cell carcinoma was 37.0 and 28.7 months, respectively [
17]. Chan et al. reported a worsened five-year survival rate for clear cell carcinoma than for serous carcinoma for patients with stage III (31.5% vs. 35.0%,
p < 0.001) and stage IV (17.5% vs. 22.2%,
p < 0.001) disease [
18]. We observed similar results in our analysis. Clear cell carcinoma had a worse outcome than serous carcinoma, including a higher risk of recurrence/persistence, higher risk in mortality, and shorter PFS and OS even in cases with optimal debulking. The number of cases with other histological types were too few in our study for statistical analysis.
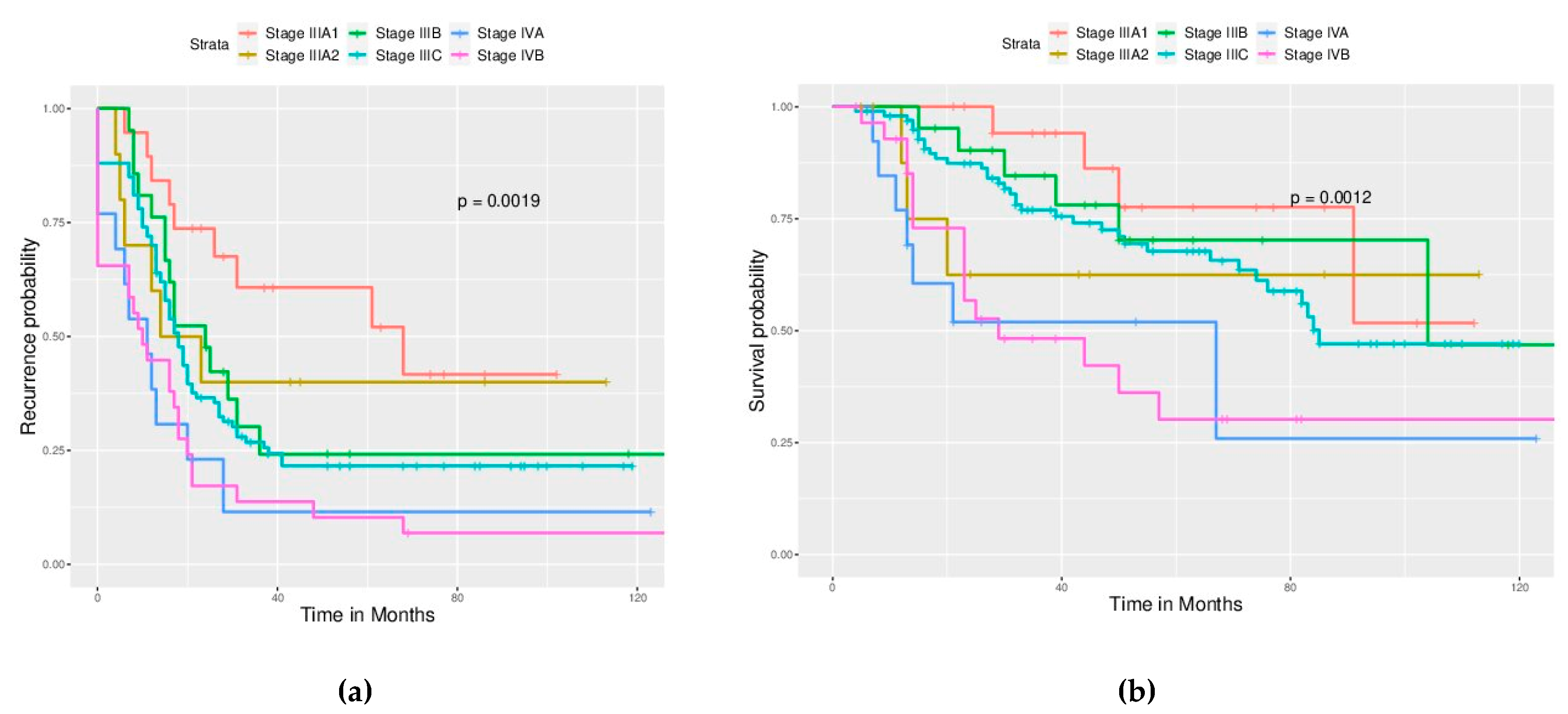
On the basis of the revised FIGO staging system (2014), LN metastasis is newly re-classified as stage IIIA1 instead of IIIC [
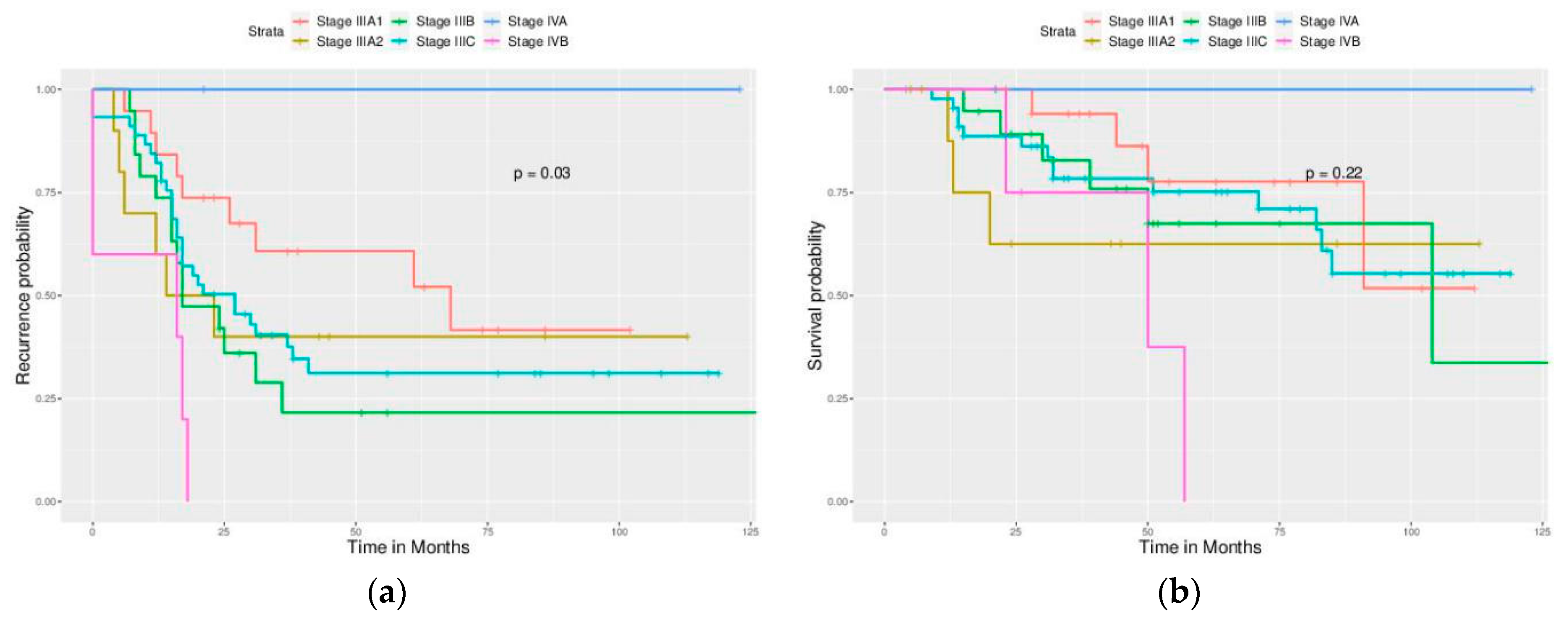
3]. We, therefore, re-classified cases with LN metastases according to the new FIGO staging system. Stage IIIC was “macroscopic peritoneal metastases beyond the pelvis >2 cm in the greatest dimension regardless of the LN status.” We found that most our patients were stage IIIC (50%) and that patients with only retroperitoneal LN metastases without intraperitoneal lesions (re-classified stage IIIA1) had better PFS and OS than the re-classified IIIC cases. This finding supports the downstaging of the LN status to stage IIIA1 by FIGO.
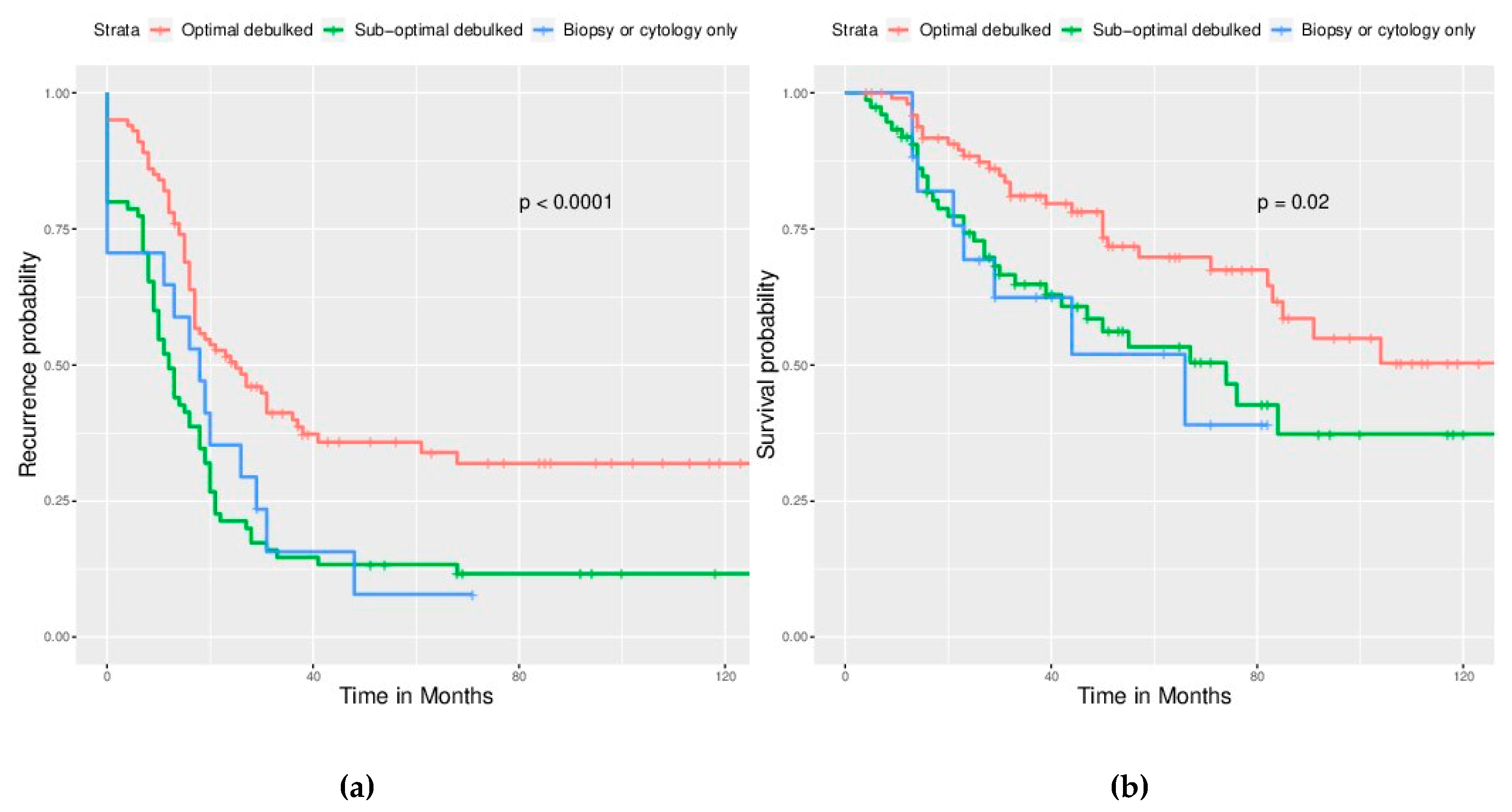
The completeness of surgical debulking plays a critical role in treating advanced EOC. Optimally debulked cases in our study had significantly longer PFS and OS than those cases with suboptimal or no debulking. This finding is compatible with the current knowledge of treating EOC. Moreover, we found that the outcome between patients with suboptimal debulking and no debulking was similar. Thus, surgeons should do their best to achieve optimal debulking or abort debulking surgery if this goal cannot be achieved. Neoadjuvant chemotherapy and optimal interval debulking surgery could be considered to improve the outcome of such difficult cases [
19]. In our study, cases with an optimal interval debulked surgery after neoadjuvant chemotherapy (data not shown) were classified into our optimally debulked group, and they also had better PFS and OS than the primary sub-optimally debulked group or no debulking group.
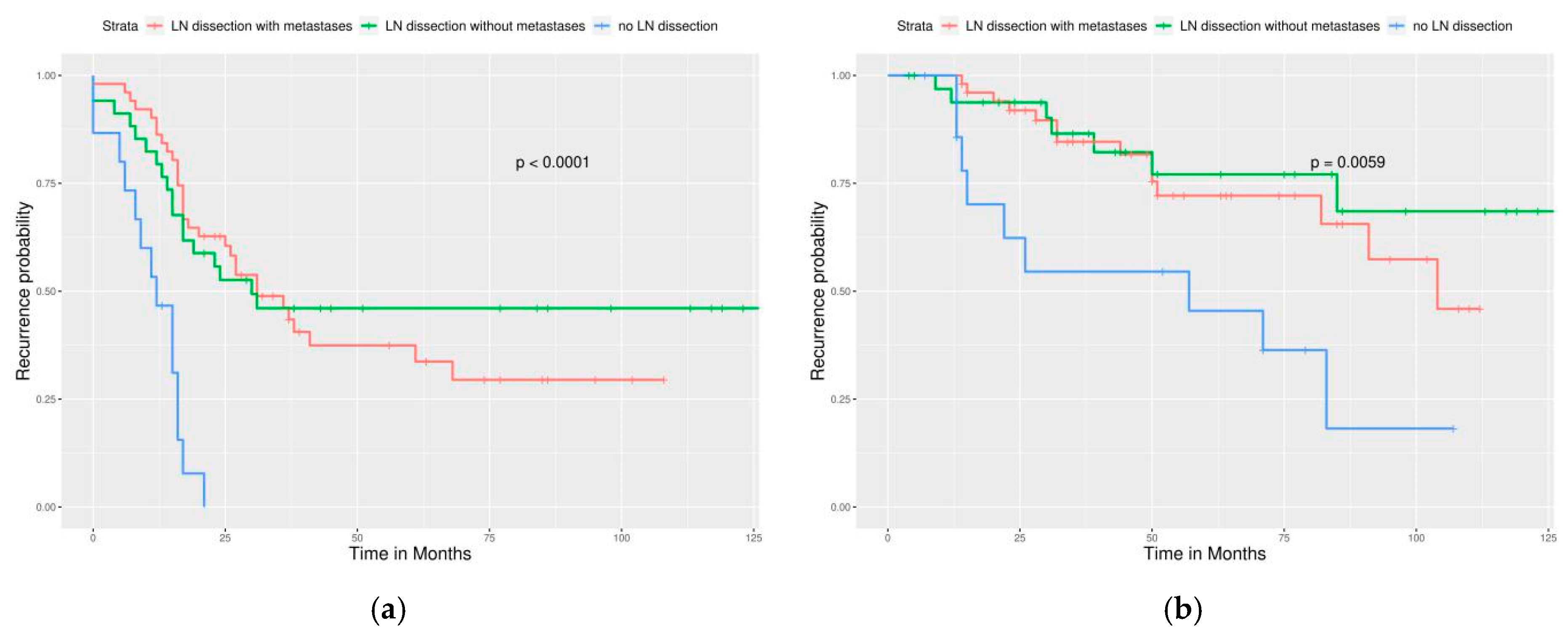
Retroperitoneal LN dissection is included in the debulking and staging procedure and improves the completeness of debulking surgery, but its benefits to patients’ outcomes is debatable. Benedetti et al. reported that systematic lymphadenectomy in optimally debulked EOC improves PFS, but not OS in their randomized trial [
20]. However, the trial by Harter et al. in 2019 reported no improvement of PFS and OS if systematic retroperitoneal lymphadenectomy was performed in advanced EOC without residual intraperitoneal macroscopic lesions [
21]. This study excluded cases with evident lymphadenopathy before preoperative imaging and demonstrated that additional LN dissection for non-bulky LNs was associated with frequent surgical complications.
Many gynecological oncologists choose to omit retroperitoneal LN dissection when peritoneal carcinomatosis is identified during surgery (stage ≥ IIIA2) if preoperative imaging does not reveal lymphadenopathy. This is because LN metastasis does not up-stage the disease. Furthermore, omitting LN dissection shortens the surgical time, and, thus, decreases morbidity. They think that microscopic LN metastases could likely be treated by adjuvant target chemotherapy [
21]. On the basis of our findings, we recommend LN dissection in all cases undergoing optimal debulking surgery, even with no evidence of LN metastases in order to achieve better PFS and OS and a lower risk of recurrence/persistence and mortality. However, LN dissection was not found to improve survival in our sub-optimally debulked cases. Therefore, it could be omitted in such a scenario.
EOC is the most chemo-sensitive solid tumor. Therefore, adjuvant chemotherapy plays a critical role in its treatment [
14]. Various regimens have been studied for decades, and the platinum-based combination has been the regimen of choice since 1990. The three-weekly regimen of intravenous paclitaxel and carboplatin/cisplatin after surgical debulking is the current standard of care since the consensus meeting of International Gynecological Cancer Intergroup Ovarian Cancer (GCIS) since 2005 [
14]. Many clinical trials have tried various modifications for this regimen to improve patient outcomes [
6,
7,
8,
9] such as changing the route of administration (from intravenous to intraperitoneal), schedule of regimen (dose-dense weekly infusion), and adding newly developed target therapeutic agents (such as a tyrosine-kinase inhibitor or a monoclonal antibody against vascular epithelial growth factor). The milestones of these trials are summarized in
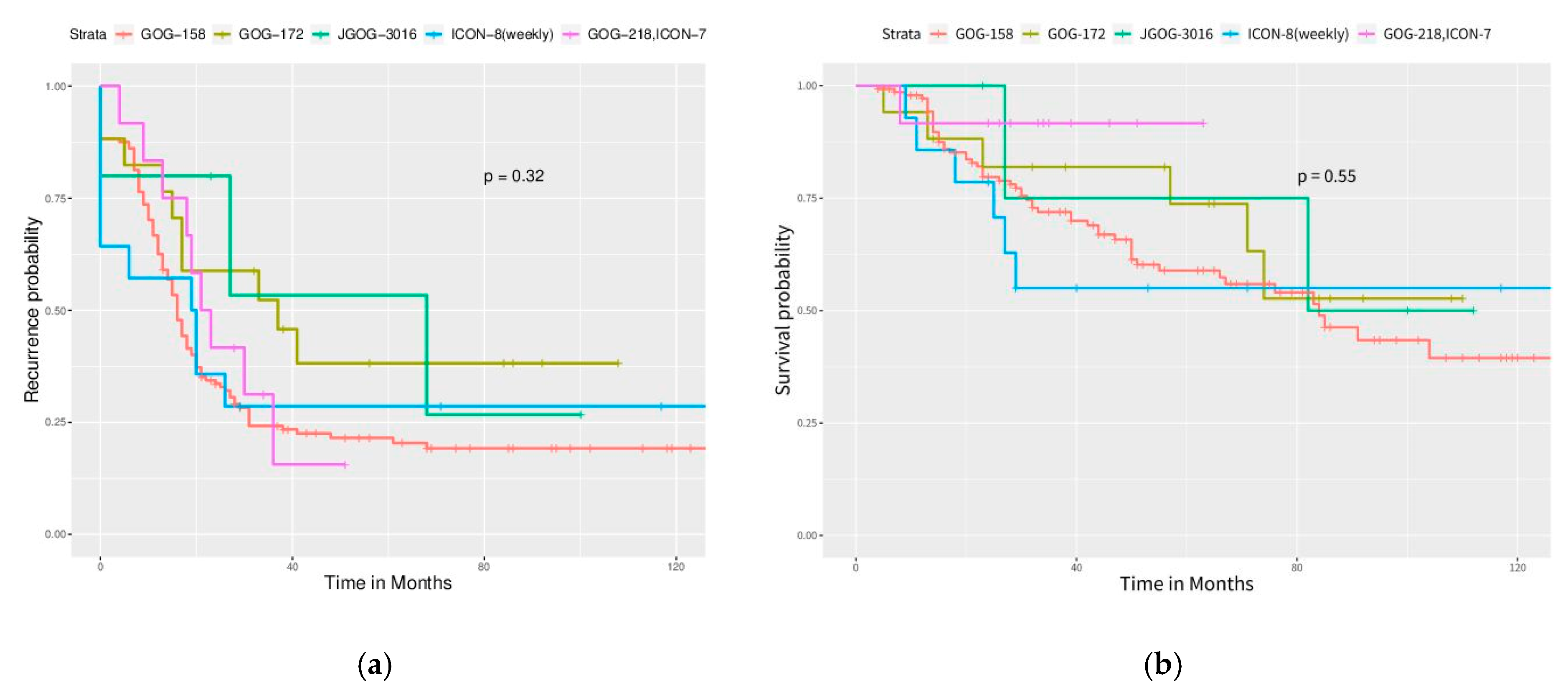
Table 2. Although they revealed more promising results than the traditional regimen, a direct cross-trial comparison is unacceptable and unreasonable, which precludes the determination of the best new regimen. Many pros and cons are discussed in these published trials. For example, intraperitoneal chemotherapy (GOG-172) has a higher treatment-related toxicity and morbidity than a traditional intravenous regimen, and the completion rate of the total six courses is only 44%. Dose dense, weekly schedule of paclitaxel infusion (JGOG-3016 [
7]) is the only prospective trial with such a promising result, but it was not reproduced by other identical schedule trials (GOG-262, MITO-7, and ICON-8) in Western countries [
22]. ICON-8, which included one arm of weekly paclitaxel, three-weekly carboplatin, and one arm of weekly paclitaxel–carboplatin did not show improvement from dose-dense chemotherapy [
10]. Adding bevacizumab (GOG-218/ICON-7) improved PFS but not OS in a recent long-term, follow-up trial [
8].
The selection of the adjuvant chemotherapy regimen depends on many factors, such as surgical completeness, clinicians’ preference and experience, cases’ performance status, and economic status. In the present retrospective study, we tried to find the regimen with the best outcome in our daily practice. We found that no new or modified adjuvant chemotherapies led to a lower risk of recurrence/persistence or death or better PFS and OS than the traditional regimen from GOG-158, even when a sub-analysis of cases with optimal debulking was performed. Intraperitoneal chemotherapy (from GOG-172) in the optimally debulked group was the only regimen that showed a change including lower risk of mortality than the traditional regiment. However, no PFS or OS benefit was noted. Too few cases were administered using this regimen in our study, which likely contributed to this result. In addition, a high withdrawal rate was observed, which was the same as GOG-172, because of the intolerable side effects of this regimen. Grade 3–4 hematologic toxicities are frequently encountered on Day 8 with infusion of intraperitoneal paclitaxel. Currently, the application of cisplatin in first-line chemotherapy is lower than carboplatin. Carboplatin has lower renal toxicity, and it can be timesaving in paclitaxel infusion (from 24 h infusion to 3 h infusion) [
5]. Therefore, this intraperitoneal regimen is not chosen as the first-line treatment by many clinicians, even if it demonstrated excellent improvement of PFS and OS in a clinical trial. It is possible that a higher number of cases in that arm in our study could have demonstrated a survival difference.
In the arm of chemotherapy plus bevacizumab, we did not have sufficient cases to analyze because we considered enrollment of cases until only December 2017. This was because we wanted to evaluate the actual recurrence rate because most cases with advanced EOC experience recurrence within 24 months [
5,
6,
7,
8,
9,
10]. In our institute, adding bevacizumab in chemotherapy became more frequent after 2017. Thus, there should be more cases from 2018, and they could be enrolled in a future study. For economic consideration, the dose of bevacizumab is 7.5 mg/kg in our daily practice, which is the same as ICON-7 [
9].
Our study has some limitations. Its retrospective design results in a lower strength of evidence than prospective studies. Non-balanced case numbers in different groups of adjuvant chemotherapies (75% of cases received the traditional regimen of GOG-158) likely resulted in a statistical bias. Lack of precise surgical records in ancient cases undergoing optimal debulking surgery (no macro-residual, <1 or <2 cm residual) increased the heterogenicity of the optimally debulked group. The scale of LN dissection (biopsy only, regional sampling, or systemic lymphadenectomy) was sometimes difficult to determine from ancient surgical records. A larger multi-center retrospective study might be considered and conducted in the future by the Taiwanese Gynecological Oncology Study Group to collect more experience from the real world.