Can We Predict the Evolution of Depressive Symptoms, Adjustment, and Perceived Social Support of Pregnant Women from Their Personality Characteristics? a Technology-Supported Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
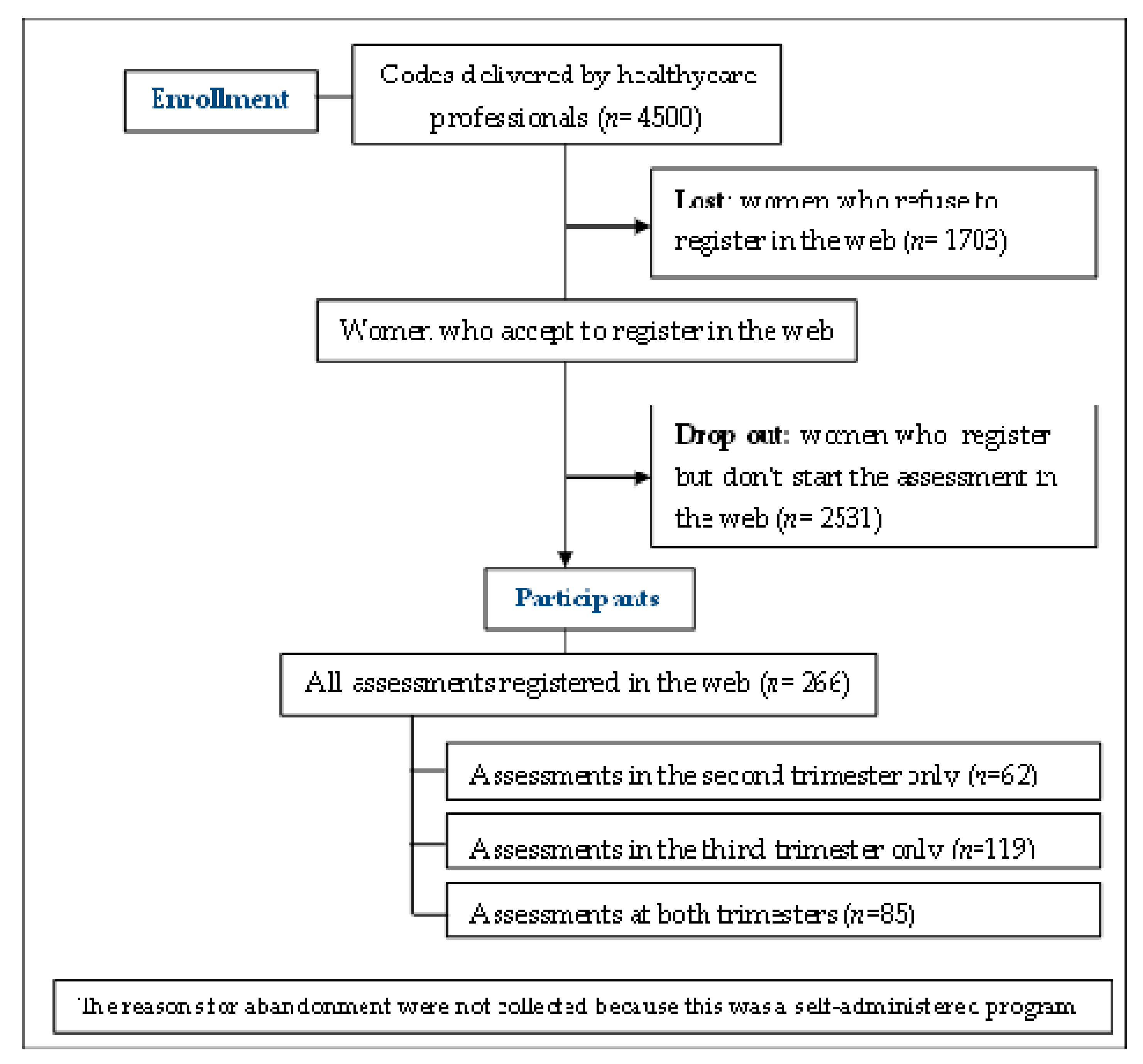
2.1. Participants
2.2. Method
2.3. Instruments
2.4. Data Analysis
3. Results
3.1. Retention of the Participants Into the Online Assessment Program MMF
3.2. Descriptive Results of the Study Variables
3.3. Evolution of Outcomes (Depressive Symptoms, Adjustment, and Perceived Social Support) During Pregnancy
3.4. Bivariate Associations Between Personality Variables, Depressive Symptoms, Adjustment, and Perceived Social Support
3.5. Personality Factors as Predictors of Depressive Symptoms, Maladjustment, and Perceived Social Support Evolution During Pregnancy: Multivariate Analysis)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Glazier, R.H.; Elgar, F.J.; Goel, V.; Holzapfel, S. Stress, social support, and emotional distress in a community sample of pregnant women. J. Psychosom. Obstet. Gynecol. 2005, 25, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Rubertsson, C.; Hellström, J.; Cross, M.; Sydsjö, G. Anxiety in early pregnancy: Prevalence and contributing factors. Arch. Women’s Ment. Heal. 2014, 17, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Rallis, S.; Skouteris, H.; McCabe, M.P.; Milgrom, J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth 2014, 27, e36–e42. [Google Scholar] [CrossRef] [PubMed]
- Accortt, E.E.; Cheadle, A.C.D.; Schetter, C.D. Prenatal depression and adverse birth outcomes: An updated systematic review. Matern. Child Heal. J. 2015, 19, 1306–1337. [Google Scholar] [CrossRef]
- Rodriguez, M.D.L.F.; Le, H.-N.; La Cruz, I.V.-D.; Crespo, M.E.O.; Méndez, N.I. Feasibility of screening and prevalence of prenatal depression in an obstetric setting in Spain. Eur. J. Obstet. Gynecol. Reprod. Boil. 2017, 215, 101–105. [Google Scholar] [CrossRef]
- Clinical Practice Guideline for Care in Pregnancy and Puerperium. Available online: https://portal.guiasalud.es/wp-content/uploads/2018/12/GPC_533_Embarazo_AETSA_compl_en.pdf (accessed on 6 May 2020).
- The American College os Obstetricians and Gynecologist. ACOG Screening for perinatal depression. Obstet. Gynecol. 2018, 132, e208–e212. [Google Scholar] [CrossRef]
- Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance. Available online: https://www.nice.org.uk/guidance/cg192 (accessed on 6 May 2020).
- Guia De Practica Clinica de atención en el embarazo y puerperio. Available online: https://portal.guiasalud.es/wp-content/uploads/2018/12/GPC_533_Embarazo_AETSA_compl.pdf (accessed on 6 May 2020).
- Force, U.P.S.T.; Curry, S.J.; Krist, A.H.; Owens, U.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Grossman, D.C.; et al. Interventions to Prevent Perinatal Depression: US Preventive Services Task Force Recommendation Statement. JAMA 2019, 321, 580–587. [Google Scholar] [CrossRef] [Green Version]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2015, 191, 62–77. [Google Scholar] [CrossRef] [Green Version]
- Lancaster, C.A.; Gold, K.J.; Flynn, H.A.; Yoo, H.; Marcus, S.M.; Davis, M.M. Risk factors for depressive symptoms during pregnancy: A systematic review. Am. J. Obstet. Gynecol. 2010, 202, 5–14. [Google Scholar] [CrossRef] [Green Version]
- Dennis, C.-L.; Boyce, P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. J. Psychosom. Obstet. Gynecol. 2005, 25, 305–311. [Google Scholar] [CrossRef]
- Barlow, D.H.; Sauer-Zavala, S.; Carl, J.R.; Bullis, J.R.; Ellard, K.K. The Nature, Diagnosis, and Treatment of Neuroticism. Clin. Psychol. Sci. 2013, 2, 344–365. [Google Scholar] [CrossRef]
- Barlow, D.; Ellard, K.K.; Sauer-Zavala, S.; Bullis, J.R.; Carl, J.R. The Origins of Neuroticism. Perspect. Psychol. Sci. 2014, 9, 481–496. [Google Scholar] [CrossRef] [PubMed]
- Bunevicius, R.; Kusminskas, L.; Bunevicius, A.; Nadisauskiene, R.J.; Jureniene, K.; Pop, V.J. Psychosocial risk factors for depression during pregnancy. Acta Obstet. et Gynecol. Scand. 2009, 88, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Podolska, M.Z.; Bidzan, M.; Majkowicz, M.; Podolski, J.; Sipak-Szmigiel, O.; Ronin-Walknowska, E. Personality traits assessed by the NEO Five-Factor Inventory (NEO-FFI) as part of the perinatal depression screening program. Med Sci. Monit. 2010, 16, 77–81. [Google Scholar]
- Swickert, R. Personality and social support processes. In The Cambridge Handbook of Personality Psychology; Cambridge University Press: New York, NY, USA, 2012; pp. 524–540. [Google Scholar]
- Johnston, R.; Brown, A. Maternal trait personality and childbirth: The role of extraversion and neuroticism. Midwifery 2013, 29, 1244–1250. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A. Extraversion and Its Positive Emotional Core. In Handbook of Personality Psychology, 1st ed.; Hogan, R., Johnson, J., Briggs, S., Eds.; Academic Press: Amsterdam, The Netherlands, 1997; pp. 767–793. [Google Scholar]
- Yang, S.K.; Ha, Y. Predicting Posttraumatic Growth among Firefighters: The Role of Deliberate Rumination and Problem-Focused Coping. Int. J. Environ. Res. Public Heal. 2019, 16, 3879. [Google Scholar] [CrossRef] [Green Version]
- Kotov, R.; Gamez, W.; Schmidt, F.; Watson, D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol. Bull. 2010, 136, 768–821. [Google Scholar] [CrossRef]
- Peñacoba-Puente, C.; Marín-Morales, D.; Carmona-Monge, F.J.; Furlong, L.V. Post-Partum Depression, Personality, and Cognitive-Emotional Factors: A Longitudinal Study on Spanish Pregnant Women. Heal. Care Women Int. 2015, 37, 1–21. [Google Scholar] [CrossRef]
- Eysenck, H. The definition and measurement of psychoticism. Pers. Individ. Differ. 1992, 13, 757–785. [Google Scholar] [CrossRef]
- Zeng, Y.; Cui, Y.; Li, J. Prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester: A cross-sectional survey. BMC Psychiatry 2015, 15, 66. [Google Scholar] [CrossRef] [Green Version]
- McCrae, R.R.; Costa, P.T., Jr. Comparison of EPI and psychoticism scales with measures of the five-factor model of personality. Pers. Individ. Differ. 1985, 6, 587–597. [Google Scholar] [CrossRef]
- Peñacoba, C.; Rodriguez, L.; Carmona, J.; Marin, D. Agreeableness and pregnancy: Relations with coping and psychiatric symptoms, a longitudinal study on Spanish pregnant women. Women Heal. 2017, 58, 204–220. [Google Scholar] [CrossRef] [PubMed]
- Martini, J.; Petzoldt, J.; Einsle, F.; Beesdo-Baum, K.; Höfler, M.; Wittchen, H.-U. Risk factors and course patterns of anxiety and depressive disorders during pregnancy and after delivery: A prospective-longitudinal study. J. Affect. Disord. 2015, 175, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, J.; Hirshler, Y.; Reece, J.; Holt, C.; Gemmill, A.W. Social Support-A Protective Factor for Depressed Perinatal Women? Int. J. Environ. Res. Public Heal. 2019, 16, 1426. [Google Scholar] [CrossRef] [Green Version]
- Bouvette-Turcot, A.-A.; Bernier, A.; Leblanc, E. Maternal Psychosocial Maladjustment and Child Internalizing Symptoms: Investigating the Modulating Role of Maternal Sensitivity. J. Abnorm. Child Psychol. 2016, 45, 157–170. [Google Scholar] [CrossRef] [Green Version]
- Field, T. Prenatal depression effects on early development: A review. Infant Behav. Dev. 2011, 34, 1–14. [Google Scholar] [CrossRef]
- Outomuro, D.; Actis, A. Estimación del tiempo de consulta ambulatoria en clínica médica. Revista médica de Chile 2013, 141, 361–366. [Google Scholar] [CrossRef] [Green Version]
- McLoughlin, J. Stigma associated with postnatal depression: A literature review. Br. J. Midwifery 2013, 21, 784–791. [Google Scholar] [CrossRef]
- Kingston, D.; Austin, M.-P.; Heaman, M.; McDonald, S.; Lasiuk, G.; Sword, W.A.; Giallo, R.; Hegadoren, K.; Vermeyden, L.; Van Zanten, S.V.; et al. Barriers and facilitators of mental health screening in pregnancy. J. Affect. Disord. 2015, 186, 350–357. [Google Scholar] [CrossRef]
- Internet Use by Individuals. Available online: https://ec.europa.eu/eurostat/databrowser/view/tin00028/default/table?lang=en (accessed on 15 April 2020).
- Osma, J.; Barrera, A.Z.; Ramphos, E. Are Pregnant and Postpartum Women Interested in Health-Related Apps? Implications for the Prevention of Perinatal Depression. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 412–415. [Google Scholar] [CrossRef]
- Lewis, B.A.; Gjerdingen, D.K.; Avery, M.D.; Guo, H.; Sirard, J.R.; Bonikowske, A.R.; Marcus, B.H. Examination of a telephone-based exercise intervention for the prevention of postpartum depression: Design, methodology, and baseline data from The Healthy Mom study. Contemp. Clin. Trials 2012, 33, 1150–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belisario, J.M.; Gupta, A.K.; O’Donoghue, J.; Ramchandani, P.; Morrison, C.; Car, J. Implementation of depression screening in antenatal clinics through tablet computers: Results of a feasibility study. BMC Med Inform. Decis. Mak. 2017, 17, 59. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Borba, V.; Suso-Ribera, C.; Osma, J. The Use of Information and Communication Technologies in Perinatal Depression Screening: A Systematic Review. Cyberpsychol. Behav. Soc. Netw. 2018, 21, 741–752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozer, D.; Benet-Martinez, V. Personality and the Prediction of Consequential Outcomes. Annu. Rev. Psychol. 2006, 57, 401–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eysenck, S.; Eysenck, H.; Barrett, P. A revised version of the psychoticism scale. Pers. Individ. Differ. 1985, 6, 21–29. [Google Scholar] [CrossRef] [Green Version]
- Eysenck, H.J.; Eysenck, S.B.G. EPQ-R: Cuestionario Revisado de Personalidad de Eysenck: Versiones Completa (EPQ-R) y Abreviada (EPQ-RS): Manual, 2nd ed.; Hodder & Stoughton: London, UK, 2001. [Google Scholar]
- Vázquez, M.B.; Míguez, M.D.C. Validation of the Edinburgh postnatal depression scale as a screening tool for depression in Spanish pregnant women. J. Affect. Disord. 2019, 246, 515–521. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Echeburúa, E.; de Corral, P.; Fernandez-Montalvo, J. Escala de inadaptación (EI): Propiedades psicométricas en contextos clínicos. Análisis y Modificación de Conducta 2000, 26, 325–340. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Landeta, O.; Calvete, E. Adaptación y validación de la escala multidimensional de apoyo social percibido. Ansiedad y estrés 2002, 8, 173–182. [Google Scholar]
- Guedes, M.; Canavarro, M.C. Personal competencies, social resources, and psychosocial adjustment of primiparous women of advanced maternal age and their partners. Child Adolesc. Soc. Work. J. 2015, 36, 506–521. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, A.; Bohlin, G.; Lindmark, G. Symptoms across pregnancy in relation to psychosocial and biomedical factors. Acta Obstet. et Gynecol. Scand. 2001, 80, 213–223. [Google Scholar] [CrossRef] [PubMed]
- O’Mahen, H.; A Richards, D.; Woodford, J.; Wilkinson, E.; McGinley, J.; Taylor, R.S.; Warren, F.C. Netmums: A phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychol. Med. 2013, 44, 1675–1689. [Google Scholar] [CrossRef] [PubMed]
- Salonen, A.; Pridham, K.F.; Brown, R.L.; Kaunonen, M. Impact of an internet-based intervention on Finnish mothers’ perceptions of parenting satisfaction, infant centrality and depressive symptoms during the postpartum year. Midwifery 2014, 30, 112–122. [Google Scholar] [CrossRef]
- Bjelland, I.; Krokstad, S.; Mykletun, A.; Dahl, A.A.; Tell, G.S.; Tambs, K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc. Sci. Med. 2008, 66, 1334–1345. [Google Scholar] [CrossRef]
- Warren, P.L. First-time mothers: Social support and confidence in infant care. J. Adv. Nurs. 2005, 50, 479–488. [Google Scholar] [CrossRef]
- Gavin, N.I.; Gaynes, B.; Lohr, K.; Meltzer-Brody, S.; Gartlehner, G.; Swinson, T. Perinatal Depression: A Systematic Review of Prevalence and Incidence. Obstet. Gynecol. 2005, 106, 1071–1083. [Google Scholar] [CrossRef]
- Caramlau, I.; Barlow, J.; Sembi, S.; McKenzie-McHarg, K.; McCabe, C. Mums 4 Mums: Structured telephone peer-support for women experiencing postnatal depression. Pilot and exploratory RCT of its clinical and cost effectiveness. Trials 2011, 12, 88. [Google Scholar] [CrossRef] [Green Version]
- Siegel, R.S.; Brandon, A.R. Adolescents, Pregnancy, and Mental Health. J. Pediatr. Adolesc. Gynecol. 2014, 27, 138–150. [Google Scholar] [CrossRef]
- Fellenzer, J.L.; Cibula, D.A. Intendedness of Pregnancy and Other Predictive Factors for Symptoms of Prenatal Depression in a Population-Based Study. Matern. Child Heal. J. 2014, 18, 2426–2436. [Google Scholar] [CrossRef]
- Goodman, J.H. Women’s Attitudes, Preferences, and Perceived Barriers to Treatment for Perinatal Depression. Birth 2009, 36, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Danaher, B.G.; Milgrom, J.; Seeley, J.R.; Stuart, S.; Schembri, C.; Tyler, M.S.; Ericksen, J.; Lester, W.; Gemmill, A.W.; Lewinsohn, P.; et al. Web-based Intervention for Postpartum Depression: Formative Research and Design of the MomMoodBooster Program. JMIR Res. Protoc. 2012, 1, e18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suso-Ribera, C.; Castilla, D.; Zaragozá, I.; Ribera-Canudas, M.V.; Arbona, C.B.; Palacios, A.G. Validity, Reliability, Feasibility, and Usefulness of Pain Monitor, a Multidimensional Smartphone App for Daily Monitoring of Adults with Heterogeneous Chronic Pain. Clin. J. Pain 2018, 34, 900–908. [Google Scholar] [CrossRef] [PubMed]
- Sardi, L.; Idri, A.; Fernández-Alemán, J.L. A systematic review of gamification in e-Health. J. Biomed. Inform. 2017, 71, 31–48. [Google Scholar] [CrossRef]
- Barrera, A.Z.; Kelman, A.R.; Muñoz, R.F.; Donker, T.; Danaher, B. Keywords to Recruit Spanish- and English-Speaking Participants: Evidence From an Online Postpartum Depression Randomized Controlled Trial. J. Med Internet Res. 2014, 16, e6. [Google Scholar] [CrossRef]
- Kingston, D.; Biringer, A.; Toosi, A.; Heaman, M.; Lasiuk, G.C.; McDonald, S.; Kingston, J.; Sword, W.A.; Jarema, K.; Austin, M.-P. Disclosure during prenatal mental health screening. J. Affect. Disord. 2015, 186, 90–94. [Google Scholar] [CrossRef]
- Commissioning Stepped Care for People with Common Mental Health Disorders. Available online: http://www.swscn.org.uk/wp/wp-content/uploads/2015/03/non-guidance-commissioning-stepped-care-for-people-with-common-mental-health-disorders-pdf.pdf (accessed on 6 May 2020).
- Barlow, D.; Farchione, T.J.; Bullis, J.R.; Gallagher, M.W.; Murray-Latin, H.; Sauer-Zavala, S.; Bentley, K.H.; Thompson-Hollands, J.; Conklin, L.R.; Boswell, J.F.; et al. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA Psychiatry 2017, 74, 875–884. [Google Scholar] [CrossRef]
| Total | |
|---|---|
| Nationality | |
| Spanish | 94.1% |
| Latin American | 2.4% |
| Western Europe | 3.5% |
| Marital Status | |
| With a living partner | 81.2% |
| Without a living partner | 18.8% |
| Educational level | |
| ≤12 years of education | 5.9% |
| >12 years of education | 94.1% |
| Employment situation | |
| Working | 67.1% |
| Unemployment | 20% |
| Sick leave | 12.9% |
| Variables | N | Pregnant Women M (SD) | N | Reference Female Population M (SD) | t | p | d |
|---|---|---|---|---|---|---|---|
| Personality | 85 | 583 | |||||
| EPQ-RS (N) | 3.8 (3.1) | 6.6 (3.4) | 7.169 | <0.001 | 0.86 | ||
| EPQ-RS (E) | 8.7 (2.7) | 8.2 (2.9) | 1.498 | 0.135 | 0.18 | ||
| EPQ-RS (P) | 2.1 (1.8) | 3.8 (2.5) | 6.043 | <0.001 | 0.78 | ||
| Depressive symptoms | 85 | 569 | |||||
| EPDS (2nd T) | 5.2 (4.6) | 5.7 (3.9) | 1.076 | 0.282 | 0.12 | ||
| EPDS (3rd T) | 4.7 (4.3) | 5.7 (4.3) | 1.999 | 0.046 | 0.23 | ||
| Maladjustment | 85 | ||||||
| MS | 6.2 (5.3) | - | - | - | - | ||
| Social support | 85 | 265 | |||||
| MSPSS (Family) | 6.5 (0.8) | 6.0 (1.2) | 3.592 | <0.001 | 0.49 | ||
| MSPSS (Friends) | 6.3 (1.0) | 5.6 (1.3) | 4.549 | <0.001 | 0.60 |
| Time 1 | Time 2 | t | 95% CI | r | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| EPDS | 5.2 | 4.6 | 4.7 | 4.3 | −1.024 | −1.42,0.46 | 0.53 ** |
| MS | 6.2 | 5.3 | 8.9 | 5.4 | 4.832 ** | 1.59, 3.80 | 0.54 ** |
| MSPSS (F) | 6.5 | 0.8 | 6.4 | 1.0 | −0.744 | −0.15, 0.07 | 0.85 ** |
| MSPSS (Fr) | 6.3 | 1.0 | 6.1 | 1.0 | −1.493 | −0.29, 0.04 | 0.71 ** |
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Second trimester | |||||||||||
| 1. Neuroticism | −0.36 ** | 0.19 | −0.31 * | −0.34 * | 0.61 ** | 0.29 * | 0.10 | −0.29 * | −0.48 ** | 0.54 ** | 0.46 ** |
| 2. Extraversion | −0.09 | 0.34 ** | 0.34 * | −0.43 ** | −0.30 * | −0.12 | 0.28 * | 0.38 ** | −0.29 * | −0.36 ** | |
| 3. Psychoticism | −0.34 * | −0.19 | 0.11 | 0.03 | −0.09 | −0.29 * | −0.34 * | 0.33 * | 0.08 | ||
| 4. Family support | 0.65 ** | −0.23 | −0.20 | −0.05 | 0.85 ** | 0.67 ** | −0.33 * | −0.29 * | |||
| 5. Friends support | −0.27 | −0.18 | 0.04 | 0.60 ** | 0.71 ** | −0.31 * | −0.16 | ||||
| 6. Depression | 0.67 ** | 0.13 | −0.18 | −0.28 * | 0.53 ** | 0.48 ** | |||||
| 7. Maladjustment | 0.11 | −0.13 | −0.22 | 0.27 | 0.54 ** | ||||||
| 8. Age (third trimester) | −0.10 | −0.04 | 0.18 | 0.15 | |||||||
| 9. Family support | 0.71 ** | −0.38 ** | −0.27 | ||||||||
| 10. Friends support | −0.47 ** | −0.34 * | |||||||||
| 11. Depression | 0.44 ** | ||||||||||
| 12. Maladjustment |
| DV | Beta | t | 95% CI | R2 Change | F Change | |
|---|---|---|---|---|---|---|
| Depression (T2) | ||||||
| Block 1: depression (T1) | 0.28 | 2.70 ** | 0.07, 0.50 | 0 .279 | 32.15 ** | |
| Block 2: age (T1) | 0.14 | 1.56 | −0.04, 0.33 | 0.013 | 1.55 | |
| Block 3: personality (T1) | 0.133 | 6.08 ** | ||||
| Neuroticism | 0.40 | 2.62 ** | 0.10, 0.71 | |||
| Extraversion | −0.02 | −0.16 | −0.33, 0.28 | |||
| Psychoticism | 0.58 | 2.84 ** | 0.17, 0.99 | |||
| Maladjustment (T2) | ||||||
| Block 1: maladjustment (T1) | 0.42 | 4.44 ** | 0.23, 0.60 | 0.291 | 34.09 ** | |
| Block 2: age (T1) | 0.09 | 0.74 | −0.15, 0.32 | 0.009 | 1.09 | |
| Block 3: personality (T1) | 0.112 | 5.04 * | ||||
| Neuroticism | 0.50 | 2.99 * | 0.17, 0.84 | |||
| Extraversion | −0.26 | −1.35 | −0.64, 0.12 | |||
| Psychoticism | 0.03 | 0.12 | −0.48, 0.55 | |||
| Family support (T2) | ||||||
| Block 1: family support (T1) | 0.95 | 12.48 ** | 0.80, 1.10 | 0.719 | 212.81 ** | |
| Block 2: age (T1) | −0.02 | −1.03 | −0.04, 0.01 | 0.004 | 1.08 | |
| Block 3: personality (T1) | 0.001 | 0.06 | ||||
| Neuroticism | −0.06 | −0.31 | −0.05, 0.03 | |||
| Extraversion | −0.07 | −0.31 | −0.05, 0.04 | |||
| Psychoticism | −0.04 | −0.12 | −0.07, 0.06 | |||
| Social support friends (T2) | ||||||
| Block 1: friends support (T1) | 0.56 | 7.39 ** | 0.41, 0.71 | 0.506 | 84.95 ** | |
| Block 2 : age (T1) | −0.01 | −0.68 | −0.05, 0.02 | 0.005 | 0.82 | |
| Block 3: personality (T1) | 0.100 | 6.73 ** | ||||
| Neuroticism | −0.07 | −2.65 * | −0.12, −0.02 | |||
| Extraversion | 0.03 | 1.15 | −0.03, 0.09 | |||
| Psychoticism | −0.10 | −2.58 * | −0.18, 0.02 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreu-Pejó, L.; Martínez-Borba, V.; Suso-Ribera, C.; Osma, J. Can We Predict the Evolution of Depressive Symptoms, Adjustment, and Perceived Social Support of Pregnant Women from Their Personality Characteristics? a Technology-Supported Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 3439. https://doi.org/10.3390/ijerph17103439
Andreu-Pejó L, Martínez-Borba V, Suso-Ribera C, Osma J. Can We Predict the Evolution of Depressive Symptoms, Adjustment, and Perceived Social Support of Pregnant Women from Their Personality Characteristics? a Technology-Supported Longitudinal Study. International Journal of Environmental Research and Public Health. 2020; 17(10):3439. https://doi.org/10.3390/ijerph17103439
Chicago/Turabian StyleAndreu-Pejó, Laura, Verónica Martínez-Borba, Carlos Suso-Ribera, and Jorge Osma. 2020. "Can We Predict the Evolution of Depressive Symptoms, Adjustment, and Perceived Social Support of Pregnant Women from Their Personality Characteristics? a Technology-Supported Longitudinal Study" International Journal of Environmental Research and Public Health 17, no. 10: 3439. https://doi.org/10.3390/ijerph17103439
APA StyleAndreu-Pejó, L., Martínez-Borba, V., Suso-Ribera, C., & Osma, J. (2020). Can We Predict the Evolution of Depressive Symptoms, Adjustment, and Perceived Social Support of Pregnant Women from Their Personality Characteristics? a Technology-Supported Longitudinal Study. International Journal of Environmental Research and Public Health, 17(10), 3439. https://doi.org/10.3390/ijerph17103439







