School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review
Abstract
1. Introduction
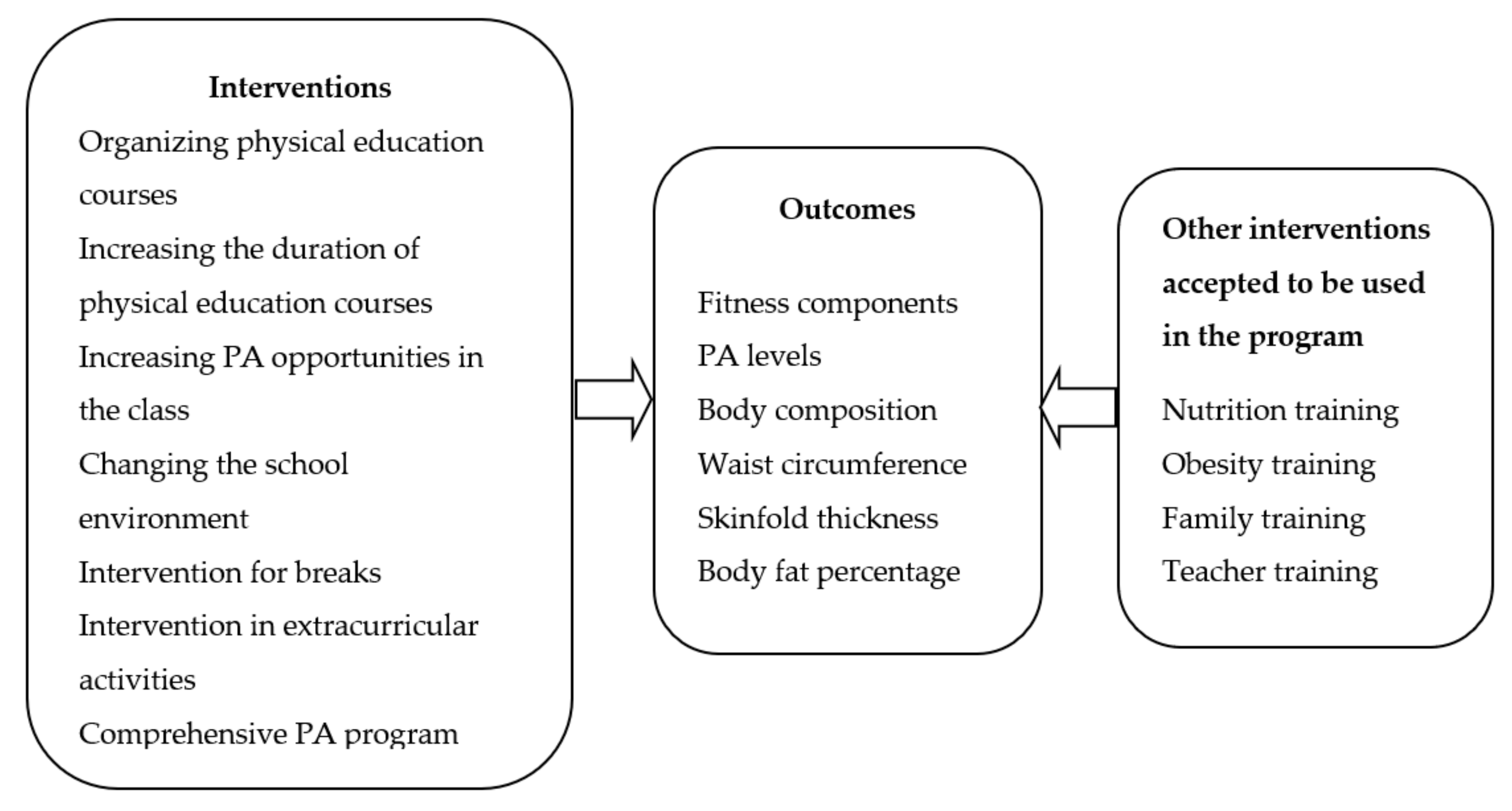
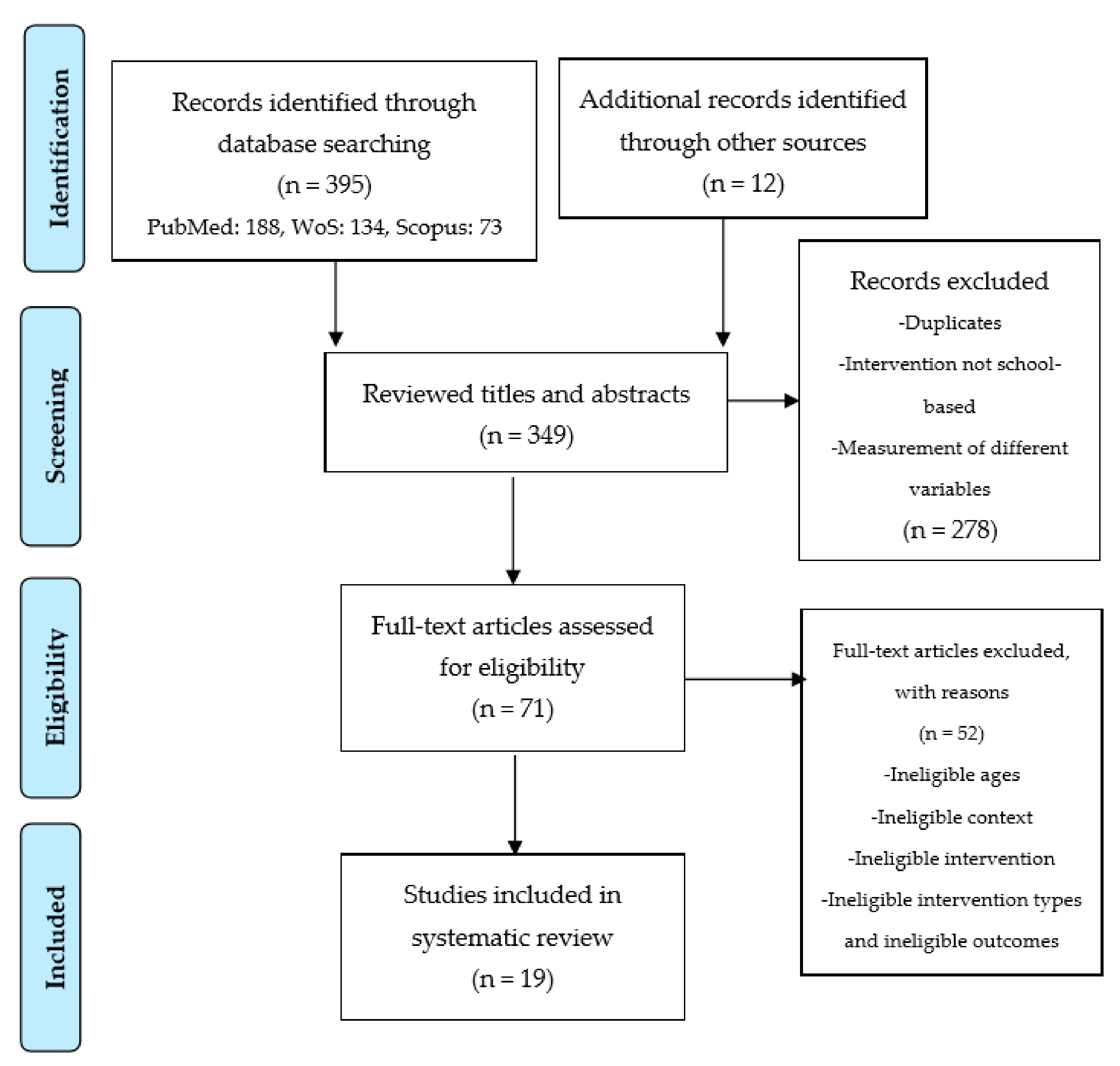
2. Materials and Methods
2.1. Literature Search and Study Selection
2.2. Eligibility Criteria
2.3. Data Extraction and Risk of Bias
3. Results
3.1. Description of Intervention and Study Quality
3.2. Main Outcomes Regarding Obesity Parameters, Physical Activity and Physical Fitness
3.2.1. Obesity
3.2.2. Physical Activity
3.2.3. Physical Fitness
4. Discussion
- (1)
- In this research, publications other than articles (theses, papers, books, etc.) and studies published in languages other than English were not included.
- (2)
- Although many variables are measured in school-based PA programs, it was focused only on measurements related to obesity, PA, and PF in this study.
- (3)
- Since the contents and the type of implementation of PA programs are generally multi-component, it is difficult to understand what the most effective way is in such studies.
- (4)
- Evaluation of the focus of school-based intervention programs was determined according to the details given in the articles.
- (5)
- Besides, some variables were measured by questionnaire and some studies did not provide enough details.
- (6)
- In this study, variables such as curriculum, teaching models and teacher competencies related to the learning process in PA, and PF developmental processes were excluded.
Practical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chaddha, A.; Jackson, E.A.; Richardson, C.R.; Franklin, B.A. Technology to Help Promote Physical Activity. Am. J. Cardiol. 2017, 119, 149–152. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Curtin, L.R.; McDowell, M.A.; Tabak, C.J.; Flegal, K.M. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006, 295, 1549–1555. [Google Scholar] [CrossRef]
- Janssen, I.; Leblanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef]
- Lonsdale, C.; Rosenkranz, R.R.; Peralta, L.R.; Bennie, A.; Fahey, P.; Lubans, D.R. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev. Med. 2013, 56, 152–161. [Google Scholar] [CrossRef]
- Varghese, T.; Schultz, W.M.; McCue, A.A.; Lambert, C.T.; Sandesara, P.B.; Eapen, D.J.; Gordon, N.F.; Franklin, B.A.; Sperling, L.S. Physical activity in the prevention of coronary heart disease: Implications for the clinician. Heart 2016, 102, 904–909. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Recommendations on Physical Activity for Health; WHO Press: Geneva, Switzerland, 2010. [Google Scholar]
- Knuth, A.G.; Hallal, P.C. Temporal trends in physical activity: A systematic review. J. Phys. Act. Health 2009, 6, 548–559. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.; Ruiz, J.; Castillo, M.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1. [Google Scholar] [CrossRef] [PubMed]
- Green, K. Understanding Physical Education; Sage: London, UK, 2008. [Google Scholar]
- To, Q.G.; Wharton, L.; Gallegos, D.; Stylianou, M.; Do, D.V.; To, K.G.; Tran, H.T.M.; Trost, S.G. School-based physical education: Physical activity and implementation barriers in Vietnamese elementary schools. Eur. Phys. Educ. Rev. 2019. [Google Scholar] [CrossRef]
- Morgan, P.; Bourke, S. Non-specialist teachers’ confidence to teach PE: The nature and influence of personal school experiences in PE. Phys. Educ. Sport Pedagog. 2008, 13, 1–29. [Google Scholar] [CrossRef]
- Slusser, W. Family physicians and the childhood obesity epidemic. Am. Fam. Physician 2008, 78, 34–37. [Google Scholar]
- WHO. Global Strategy on Diet, Physical Activity and Health. Available online: https://www.who.int/dietphysicalactivity/childhood/en/ (accessed on 15 September 2019).
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 September 2019).
- Hardy, L.L.; King, L.; Espinel, P.; Okely, A.D.; Bauman, A. Methods of the NSW Schools Physical Activity and Nutrition Survey 2010 (SPANS 2010). J. Sci. Med. Sport 2011, 14, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- WHO. What Is Overweight and Obesity? Available online: https://www.who.int/dietphysicalactivity/childhood_what/en/ (accessed on 23 September 2019).
- WHO. Report of the Commission on Ending Childhood Obesity. Available online: https://apps.who.int/iris/bitstream/handle/10665/204176/9789241510066_eng.pdf (accessed on 13 September 2019).
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar]
- Jongenelis, M.I.; Scully, M.; Morley, B.; Pratt, I.S.; Slevin, T. Physical activity and screen-based recreation: Prevalences and trends over time among adolescents and barriers to recommended engagement. Prev. Med. 2018, 106, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.; Reilly, J.J.; Huang, W.Y. Longitudinal changes in objectively measured sedentary behaviour and their relationship with adiposity in children and adolescents: Systematic review and evidence appraisal. Obes. Rev. 2014, 15, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.C.; Kuramoto, L.K.; Schulzer, M.; Retallack, J.E. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. Cmaj 2009, 180, 719–726. [Google Scholar] [CrossRef]
- Griffiths, L.J.; Sera, F.; Cortina-Borja, M.; Law, C.; Ness, A.; Dezateux, C. Objectively measured physical activity and sedentary time: Cross-sectional and prospective associations with adiposity in the Millennium Cohort Study. BMJ Open 2016, 6, e010366. [Google Scholar] [CrossRef]
- Ekelund, U.; Luan, J.; Sherar, L.B.; Esliger, D.W.; Griew, P.; Cooper, A.; International Children’s Accelerometry Database, C. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012, 307, 704–712. [Google Scholar] [CrossRef]
- Ahn, S.; Fedewa, A.L. A meta-analysis of the relationship between children’s physical activity and mental health. J. Pediatr. Psychol. 2011, 36, 385–397. [Google Scholar] [CrossRef]
- Lubans, D.R.; Smith, J.J.; Plotnikoff, R.C.; Dally, K.A.; Okely, A.D.; Salmon, J.; Morgan, P.J. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: The ATLAS cluster randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 92. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T. Exergaming: Hope for future physical activity? or blight on mankind? J. Sport Health Sci. 2017, 6, 44–46. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Meyer, U.; Martin, E.; van Sluijs, E.M.; Andersen, L.B.; Martin, B.W. Effect of school-based interventions on physical activity and fitness in children and adolescents: A review of reviews and systematic update. Br. J. Sports Med. 2011, 45, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Demetriou, Y.; Honer, O. Physical activity interventions in the school setting: A systematic review. Psychol. Sport Exerc. 2012, 13, 186–196. [Google Scholar] [CrossRef]
- Van de Kop, J.H.; van Kernebeek, W.G.; Otten, R.H.J.; Toussaint, H.M.; Verhoeff, A.P. School-Based Physical Activity Interventions in Prevocational Adolescents: A Systematic Review and Meta-Analyses. J. Adolesc. Health 2019, 65, 185–194. [Google Scholar] [CrossRef]
- Hynynen, S.T.; van Stralen, M.M.; Sniehotta, F.F.; Araújo-Soares, V.; Hardeman, W.; Chinapaw, M.J.M.; Vasankari, T.; Hankonen, N. A systematic review of school-based interventions targeting physical activity and sedentary behaviour among older adolescents. Int. Rev. Sport Exerc. Psychol. 2016, 9, 22–44. [Google Scholar] [CrossRef]
- Hung, L.-S.; Tidwell, D.K.; Hall, M.E.; Lee, M.L.; Briley, C.A.; Hunt, B.P. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr. Res. 2015, 35, 229–240. [Google Scholar] [CrossRef]
- Sigmund, E.; Sigmundová, D. Longitudinal 2-year follow-up on the effect of a non-randomised school-based physical activity intervention on reducing overweight and obesity of Czech children aged 10–12 years. Int. J. Environ. Res. Public Health 2013, 10, 3667–3683. [Google Scholar] [CrossRef]
- Sacchetti, R.; Ceciliani, A.; Garulli, A.; Dallolio, L.; Beltrami, P.; Leoni, E. Effects of a 2-year school-based intervention of enhanced physical education in the primary school. J. Sch. Health 2013, 83, 639–646. [Google Scholar] [CrossRef]
- Pbert, L.; Druker, S.; Barton, B.; Schneider, K.L.; Olendzki, B.; Gapinski, M.A.; Kurtz, S.; Osganian, S. A school-based program for overweight and obese adolescents: A randomized controlled trial. J. Sch. Health 2016, 86, 699–708. [Google Scholar] [CrossRef]
- Kahn, E.B.; Ramsey, L.T.; Brownson, R.C.; Heath, G.W.; Howze, E.H.; Powell, K.E.; Stone, E.J.; Rajab, M.W.; Corso, P. The effectiveness of interventions to increase physical activity. A systematic review. Am. J. Prev. Med. 2002, 22, 73–107. [Google Scholar] [CrossRef]
- Thomas, B.H.; Ciliska, D.; Dobbins, M.; Micucci, S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004, 1, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Almas, A.; Islam, M.; Jafar, T.H. School-based physical activity programme in preadolescent girls (9–11 years): A feasibility trial in Karachi, Pakistan. Arch. Dis. Child. 2013, 98, 515–519. [Google Scholar] [CrossRef]
- Aperman-Itzhak, T.; Yom-Tov, A.; Vered, Z.; Waysberg, R.; Livne, I.; Eilat-Adar, S. School-Based Intervention to Promote a Healthy Lifestyle and Obesity Prevention Among Fifth- and Sixth-Grade Children. Am. J. Health Educ. 2018, 49, 289–295. [Google Scholar] [CrossRef]
- Bhave, S.; Pandit, A.; Yeravdekar, R.; Madkaikar, V.; Chinchwade, T.; Shaikh, N.; Shaikh, T.; Naik, S.; Marley-Zagar, E.; Fall, C.H.D. Effectiveness of a 5-year school-based intervention programme to reduce adiposity and improve fitness and lifestyle in Indian children; the SYM-KEM study. Arch. Dis. Child. 2016, 101, 33–40. [Google Scholar] [CrossRef]
- Brown, E.C.; Buchan, D.S.; Cavana, J.; Baker, J.S.; Wyatt, F.B.; Kilgore, J.L. Fit for school: Results of a 10-week school-based child healthy weight pilot intervention for primary school students. Int. J. Health Promot. Educ. 2016, 54, 229–244. [Google Scholar] [CrossRef]
- Carlson, J.A.; Engelberg, J.K.; Cain, K.L.; Conway, T.L.; Mignano, A.M.; Bonilla, E.A.; Geremia, C.; Sallis, J.F. Implementing classroom physical activity breaks: Associations with student physical activity and classroom behavior. Prev. Med. 2015, 81, 67–72. [Google Scholar] [CrossRef]
- Eather, N.; Morgan, P.J.; Lubans, D.R. Improving the fitness and physical activity levels of primary school children: Results of the Fit-4-Fun group randomized controlled trial. Prev. Med. 2013, 56, 12–19. [Google Scholar] [CrossRef]
- Grydeland, M.; Bjelland, M.; Anderssen, S.A.; Klepp, K.I.; Bergh, I.H.; Andersen, L.F.; Ommundsen, Y.; Lien, N. Effects of a 20-month cluster randomised controlled school-based intervention trial on BMI of school-aged boys and girls: The HEIA study. Br. J. Sports Med. 2014, 48, 768–773. [Google Scholar] [CrossRef]
- Hollis, J.L.; Sutherland, R.; Campbell, L.; Morgan, P.J.; Lubans, D.R.; Nathan, N.; Wolfenden, L.; Okely, A.D.; Davies, L.; Williams, A.; et al. Effects of a ‘school-based’ physical activity intervention on adiposity in adolescents from economically disadvantaged communities: Secondary outcomes of the ‘Physical Activity 4 Everyone’ RCT. Int. J. Obes. 2016, 40, 1486–1493. [Google Scholar] [CrossRef] [PubMed]
- Kipping, R.R.; Howe, L.D.; Jago, R.; Campbell, R.; Wells, S.; Chittleborough, C.R.; Mytton, J.; Noble, S.M.; Peters, T.J.; Lawlor, D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014, 348, g3256. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Zahner, L.; Schindler, C.; Meyer, U.; Hartmann, T.; Hebestreit, H.; Brunner-La Rocca, H.P.; van Mechelen, W.; Puder, J.J. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: Cluster randomised controlled trial. BMJ 2010, 340, c785. [Google Scholar] [CrossRef] [PubMed]
- Li, X.H.; Lin, S.T.; Guo, H.X.; Huang, Y.L.; Wu, L.J.; Zhang, Z.L.; Ma, J.; Wang, H.J. Effectiveness of a school-based physical activity intervention on obesity in school children: A nonrandomized controlled trial. BMC Public Health 2014, 14. [Google Scholar] [CrossRef]
- Lynch, B.A.; Gentile, N.; Maxson, J.; Quigg, S.; Swenson, L.; Kaufman, T. Elementary School-Based Obesity Intervention Using an Educational Curriculum. J. Prim. Care Community Health 2016, 7, 265–271. [Google Scholar] [CrossRef]
- Madsen, K.; Linchey, J.; Gerstein, D.; Ross, M.; Myers, E.; Brown, K.; Crawford, P. Energy Balance 4 Kids with Play: Results from a Two-Year Cluster-Randomized Trial. Child. Obes. 2015, 11, 375–383. [Google Scholar] [CrossRef]
- Magnusson, K.T.; Hrafnkelsson, H.; Sigurgeirsson, I.; Johannsson, E.; Sveinsson, T. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ. Res. 2012, 27, 484–494. [Google Scholar] [CrossRef]
- Shore, S.M.; Sachs, M.L.; DuCette, J.P.; Libonati, J.R. Step-Count Promotion through a School-Based Intervention. Clin. Nurs. Res. 2014, 23, 402–420. [Google Scholar] [CrossRef]
- Sigmund, E.; El Ansari, W.; Sigmundova, D. Does school-based physical activity decrease overweight and obesity in children aged 6–9 years? A two-year non-randomized longitudinal intervention study in the Czech Republic. BMC Public Health 2012, 12, 570. [Google Scholar] [CrossRef]
- Thivel, D.; Isacco, L.; Lazaar, N.; Aucouturier, J.; Ratel, S.; Dore, E.; Meyer, M.; Duche, P. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur. J. Pediatrics 2011, 170, 1435–1443. [Google Scholar] [CrossRef]
- Tian, H.L.; du Toit, D.; Toriola, A.L. The effects of an enhanced quality Physical Education programme on the physical activity levels of Grade 7 learners in Potchefstroom, South Africa. Phys. Educ. Sport Pedagog. 2017, 22, 35–50. [Google Scholar] [CrossRef]
- Vander Ploeg, K.A.; McGavock, J.; Maximova, K.; Veugelers, P.J. School-based health promotion and physical activity during and after school hours. Pediatrics 2014, 133, e371–e378. [Google Scholar] [CrossRef] [PubMed]
- Haerens, L.; Kirk, D.; Cardon, G.; De Bourdeaudhuij, I. Toward the development of a pedagogical model for health-based physical education. Quest 2011, 63, 321–338. [Google Scholar] [CrossRef]
- O’Sullivan, M. New Directions, New Questions: Relationships between Curriculum, Pedagogy, and Assessment in Physical Education. Sport Edu. Soc. 2013, 18, 1–5. [Google Scholar] [CrossRef]
- Castelli, D.M.; Barcelona, J.M.; Bryant, L. Contextualizing physical literacy in the school environment: The challenges. J. Sport Health Sci. 2015, 4, 156–163. [Google Scholar] [CrossRef]
- Rowling, L.; Samdal, O. Filling the black box of implementation for health-promoting schools. Health Educ. 2011, 111, 347–362. [Google Scholar] [CrossRef]
- Naylor, P.J.; Nettlefold, L.; Race, D.; Hoy, C.; Ashe, M.C.; Wharf Higgins, J.; McKay, H.A. Implementation of school based physical activity interventions: A systematic review. Prev. Med. 2015, 72, 95–115. [Google Scholar] [CrossRef]
- De Bourdeaudhuij, I.; Van Cauwenberghe, E.; Spittaels, H.; Oppert, J.M.; Rostami, C.; Brug, J.; Van Lenthe, F.; Lobstein, T.; Maes, L. School-based interventions promoting both physical activity and healthy eating in Europe: A systematic review within the HOPE project. Obes. Rev. 2011, 12, 205–216. [Google Scholar] [CrossRef]
- Whitehead, J.; Fox, K. Student-centred physical education. Bull. Phys. Educ. 1983, 19, 21–30. [Google Scholar]
- McKenzie, T.L.; Sallis, J.F.; Rosengard, P. Beyond the stucco tower: Design, development, and dissemination of the SPARK physical education programs. Quest 2009, 61, 114–127. [Google Scholar] [CrossRef]
- Guerra, P.H.; Nobre, M.R.; Silveira, J.A.; Taddei, J.A. The effect of school-based physical activity interventions on body mass index: A meta-analysis of randomized trials. Clinics 2013, 68, 1263–1273. [Google Scholar] [CrossRef]
- Sharma, M. School-based interventions for childhood and adolescent obesity. Obes. Rev. 2006, 7, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Summerbell, C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes. Rev. 2009, 10, 110–141. [Google Scholar] [CrossRef] [PubMed]
- Yuksel, H.S. Experiences of Prospective Physical Education Teachers on Active Gaming within the Context of School-Based Physical Activity. Eur. J. Educ. Res. 2019, 8, 199–211. [Google Scholar]
- Grasten, A. School-based physical activity interventions for children and youth: Keys for success. J. Sport Health Sci. 2017, 6, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.; Stratton, G. Physical activity levels in middle and high school physical education: A review. Pediatric Exerc. Sci. 2005, 17, 217–236. [Google Scholar] [CrossRef]
- Wallhead, T.L.; Buckworth, J. The Role of Physical Educationin the Promotionof Youth Physical Activity. Quest 2004, 56, 285–301. [Google Scholar] [CrossRef]
- Dobbins, M.; De Corby, K.; Robeson, P.; Husson, H.; Tirilis, D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef]
- Gorely, T.; Nevill, M.E.; Morris, J.G.; Stensel, D.J.; Nevill, A. Effect of a school-based intervention to promote healthy lifestyles in 7–11 year old children. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 5. [Google Scholar] [CrossRef]
- Minatto, G.; Petroski, E.L.; Silva, K.S.d.; Duncan, M.J. School-Based Intervention on Cardiorespiratory Fitness in Brazilian Students: A Nonrandomized Controlled Trial. J. Funct. Morphol. Kinesiol. 2019, 4, 10. [Google Scholar] [CrossRef]
- McKenzie, T.L.; Lounsbery, M.A. School physical education: The pill not taken. Am. J. Lifestyle Med. 2009, 3, 219–225. [Google Scholar] [CrossRef]
- Greco, G.; Cataldi, S.; Fischetti, F. Effectiveness of a Short After-School Intervention on Physical Fitness in School-Aged Children. J. Theor. Res. Edu. 2019, 14, 143–164. [Google Scholar]
| Quality Assessment Tool for Quantitative Studies | |
|---|---|
| (A) Selection bias | Do the individuals selected for the study represent the target population? Number of individuals participating in the study. |
| (B) Study design | Is the study defined as randomized? If yes, is the randomization method specified? If yes, is the method appropriate? |
| (C) Confounders | Are there significant differences between pre-intervention groups? If yes, is the proportion of situations that cause confusion about the design or analysis indicated? |
| (D) Blinding | Are the assessors aware of the intervention or the exposure of the participants? Are the study participants aware of the research questions? |
| (E) Data collection methods | Is the validity of the data collection tools shown? Has the reliability of data collection tools been demonstrated? |
| (F) Withdrawals and dropouts | Were those who quit or were unable to complete reported? Is the proportion of those completing the study indicated? |
| Study | Design | Setting and Participants | Aim | Intervention Duration | Quality |
|---|---|---|---|---|---|
| Almas et al. [40] | Parallel cluster intervention trial |
| To examine the feasibility of the school-based program and its effect on blood pressure and body mass index among pre-adolescent girls. | Over 20 months | Strong |
| Aperman-Itzhak et al. [41] | A non-randomized controlled trial |
| To evaluate the effectiveness of a healthy lifestyle intervention on health knowledge, behavior, and anthropometric measurements. | 2011–2012 school year | Moderate |
| Bhave et al. [42] | A non-randomized controlled trial |
| To examine the 5-year impact of the program on preventing fat and improving PF and lifestyle. | 5 years | Moderate |
| Brown et al. [43] | A one-group, repeated measures design |
| To examine body mass index standard deviation score changes following a Child Healthy Weight pilot intervention. | 10 weeks | Moderate |
| Carlson et al. [44] | Mixed-effects model |
| To examine the relationship between PA breaks and PA and class behaviors. | 2013–2014 school year | Moderate |
| Eather et al. [45] | Randomized controlled trial |
| To evaluate the impact of a school-based PA intervention (Fit-4-Fun) on health-related fitness. | 8 weeks | Moderate |
| Grydeland et al. [46] | Cluster randomized, controlled study |
| To examine the effects of a multicomponent school-based intervention on anthropometric outcomes. | 20 months | Moderate |
| Hollis et al. [47] | Cluster randomized controlled trial |
| To report the secondary outcomes of the study; to determine whether the intervention impacted on adiposity outcomes (weight, body mass index (BMI), BMI z-score. | 12 months | Strong |
| Kipping et al. [48] | Cluster randomized controlled trial |
| To investigate the effectiveness of a school-based intervention to increase PA, reduce sedentary behaviour, and increase fruit and vegetable consumption in children. | 5 years | Moderate |
| Kriemler et al. [49] | A cluster randomized controlled trial. |
| To assess the effectiveness of a school-based PA program during one school year on physical and psychological health in children. | 9 months | Strong |
| Li et al. [50] | Non-randomized controlled trial |
| To assess the effectiveness of a school-based PA intervention during 12 weeks on obesity and related health outcomes in school children. | 12 weeks | Strong |
| Lynch et al. [51] | A cluster randomized controlled trial |
| To evaluate the impact of the Let’s Go! 5-2-1-0 program in an elementary school. | 8 weeks | Moderate |
| Madsen et al. [52] | A cluster randomized controlled study |
| To examine the impact of Energy Balance for Kids with Play (EB4K with Play), on students’ PA, dietary habits and knowledge, and weight status over 2 years. | Over 2 years | Strong |
| Magnusson et al. [53] | A cluster randomized controlled trial. |
| To assess the effects of a 2-year intervention program on body composition and objectively measured cardiorespiratory fitness. | 2 years | Moderate |
| Shore et al. [54] | A quasi-experimental design |
| To determine the effects of a school-based pedometer intervention (SBPI) on daily accrued steps, academic performance, attendance, tardiness, and fitness performance in middle school students. | 6 weeks | Strong |
| Sigmund et al. [55] | Non-randomized controlled trial |
| To investigate the effect of increased PA on increasing daily PA and decreasing obesity in 6–9-year children. | 2006–2008 | Strong |
| Thivel et al. [56] | Randomized intervention study |
| To assess the effect of a PA program on body composition and PF. | 6 months | Strong |
| Tian et al. [57] | A pre-test and post-test control-group design |
| To evaluate the effects of a once-a-week enhanced quality PE program on the PA levels. | Over 12 weeks | Strong |
| Vander Ploeg et al. [58] | Quasi-experimental, pre-post-trial with a parallel, non-equivalent control group |
| To examine the 2-year change in PA during and after school among students participating in a comprehensive school health (CSH) intervention. | 2008–2011 | Strong |
| Study | BMI (kg/m2) | Body Composition | Physical Activity Levels | Physical Fitness |
|---|---|---|---|---|
| Almas et al. [40] | + | NA | NA | NA |
| Aperman-Itzhak et al. [41] | + | + | NA | NA |
| Bhave et al. [42] | − | + | NA | + |
| Brown et al. [43] | + | NA | NA | NA |
| Carlson et al. [44] | NA | NA | + | NA |
| Eather et al. [45] | + | + | + | + |
| Grydeland et al. [46] | + (Only girls) | − | NA | NA |
| Hollis et al. [47] | + | NA | − | NA |
| Kipping et al. [48] | NA | NA | − | NA |
| Kriemler et al. [49] | + | + | − | + |
| Li et al. [50] | + | + | + | NA |
| Lynch et al. [51] | − | NA | − | NA |
| Madsen et al. [52] | + | NA | − | NA |
| Magnusson et al. [53] | − | − | NA | + |
| Shore et al. [54] | NA | NA | + | − |
| Sigmund et al. [55] | NA | NA | + | NA |
| Thivel et al. [56] | − | − | NA | + |
| Tian et al. [57] | − | − | − | NA |
| Vander Ploeg et al. [58] | NA | NA | + | NA |
| Study | Types and Intensities of School-Based Programs | Outcomes Measured | Results | Multiple Components | |||
|---|---|---|---|---|---|---|---|
| Almas et al. [40] | Type: PA program
| PA: Questionnaire (Last 7 days) BP: Omron M5 BP monitors Height: Community-setting aluminum scale Weight: Tanita Solar Powered Digital Scale 1631 BMI = kg/m2 | BMIz Intervention | BMIz Control | |||
| Baseline Mean (SD): −1.35 (1.39) Follow-up Mean (SD): −1.02 (1.41) | Baseline Mean (SD): −1.92 (1.82) Follow-up Mean (SD): −1.04 (1.23) | ||||||
| The difference between systolic blood pressure (SBP), diastolic blood pressure (DBP) and BMI z scores (BMIz) of the experimental group and control group was found to be significant (1.9 mm Hg, 0.7 mm hg and 0.55 kg/m2). | |||||||
| Aperman-Itzhak et al. [41] | Type: A healthy lifestyle intervention
| Healthy Lifestyle: A self-administered non-quantitative FFQ BMI (kg/m2): Height, weight, and fat percentiles were measured using a Tanita BC 418MA Segmental Body Composition Analyzer | Overweight and obesity decreased significantly within the intervention group (from 25% to 17.9%, p = 0.040), without a significant change in the control group (from 20.5% to 17.6%, p = 0.12). No significant difference was found between the beginning (p = 0.59) and the end of the year (p = 0.036) in health behaviors of the participants. |
| |||
| Bhave et al. [42] | School-Based Intervention
| Anthropometry: Height, weight and waist circumference was recorded according to standard protocols Physical fitness: 1 min of sit-ups, 1 min of push-ups, a measured vertical jump, a measured long jump, a stand-and-reach test, a timed 30-m sprint Diet and activity: self-completed questionnaires | BMI (kg/m2): Pre and post, Boys: Mean, 17.1–22.3 Girls: Mean, 17.7—22.8) Children were fitter than controls in running, long jump, sit-up and push-up tests (p < 0.05 for all). The intervention did not reduce BMI (kg/m2) or the prevalence of overweight/obesity, but waist circumference was lower than the control group (p = 0.004). |
| |||
| Brown et al. [43] | A school-based pilot intervention
| Weight: SecaTM 899 digital scales Height: Seca Leicester Height Measure stadiometer BMI = kg/m2 | Effects of program on BMI-SDS from pre to post | p |
| ||
| Pre, mean (SD): 0.49 (1.16) | p < 0.001 | ||||||
| Post, mean (SD): 0.47 (1.17) | |||||||
| BMI-SDS: −0.03 (0.29) | |||||||
| Standardised BMI (BMI-SDS) scores were significantly decreased in the whole (p < 0.001). | |||||||
| Carlson et al. [44] | Type: Classroom PA breaks
| PA: Actigraph GT3X+ accelerometers Students’ behaviors: Teacher survey | Physical activity breaks min/day: Fall 2013, mean, 5.2; Spring 2014, mean, 6.4 Class activity breaks were positively associated with MVPA of children (βs = 0.07–0.14; p = 0.012–0.016). Class-based PA practices can increase students’ level of PA throughout the day. βs = Standardized regression coefficient score |
| |||
| Eather et al. [45] | Fit-4-Fun Program
| Cardio-respiratory fitness (CRF): 20 m shuttle run Other tests: BMI (kg/m2), Y stage sit-up test, push-up test, basketball throw test, standing jump, sit and reach and pedometer | CRF: Mean, 1.14 levels, p < 0.001 BMI: Mean, −0.96 kg/m2, p < 0.001 BMI z-score (BMIz): Mean, −0.47, p < 0.001 Flexibility: Mean, 1.52 cm, p = 0.0013 Muscular fitness: Mean, 0.62 stages, p = 0.003 Physical activity: Mean, 3253 steps/day, p < 0.001 A school-based intervention focusing on fitness education significantly improved health-related fitness and PA levels in children. |
| |||
| Grydeland et al. [46] | Multiple interventions
| Height: Wall-mounted measurement tape Weight: Digital body composition analyzer BMI = kg/m2 Waist circumference (WC): A measuring tape between the lower rib and the iliac-crest | Beneficial effects were found for BMI (p = 0.02) and BMIz (p = 0.003) in girls, but not in boys. There were no intervention effects for WC and weight status (p > 0.05). |
| |||
| Hollis et al. [47] | ‘PA 4 Everyone’ intervention
| Socio-demographic characteristics: Survey Weight: A portable digital scale (Model no. UC-321PC, A&D Company Ltd., Tokyo, Japan). Height: A portable stadiometer (Model no. PE087, Mentone Educational Centre, Springvale, VIC, Australia). BMI = kg/m2 PA: Accelerometer (Actigraph GT3X+ and GT3X models, Pensacola, FL, USA43). | Difference in change between groups | p |
| ||
| BMI (Baseline to 12 month): −0.28 | 0.012 | ||||||
| BMIz (Baseline to 12 month): −0.05 | 0.130 | ||||||
| There were group-by-time effects for weight and BMI (kg/m2) (p < 0.01) in favor of the intervention group, but not for BMIz (p = 0.13). School-based intervention achieved moderate reductions in adiposity among adolescents. | |||||||
| Kipping et al. [48] | The Active for Life Year 5 (AFLY5) intervention
| MVPA, sedentary behavior: Accelerometer Weight: Digital scale Height: A portable Harpenden stadiometer Waist Circumference: Flexible tape Daily fruit and vegetable consumptions: A Day in the Life Questionnaire | Mean differences | p |
| ||
| The differences in mean: −1.35 min/day | 0.050 | ||||||
| BMIz Scores: −0.02 | 0.41 | ||||||
| Waist circumference: −0.12 | 0.03 | ||||||
| School-based intervention is not effective at increasing levels of PA, but it is effective at BMI and waist circumference. | |||||||
| Kriemler et al. [49] | A multi-component PA program
| Primary outcomes: Skinfolds (mm): Harpenden calipers (HSK BI, British Indicators). Aerobic fitness: 20 m shuttle run PA: Accelerometer (MTI/CSA 7164, Actigraph, Shalimar, FL, USA). Quality of life: health questionnaire Body mass index A cardiovascular risk score: An automated oscillograph | Intervention and control group comparison | p | |||
| The z score of the sum of four skinfolds: −0.12 | 0.009 | ||||||
| Z scores for aerobic fitness: 0.17 | 0.04 | ||||||
| MDVA physical activity: 0.92 | 0.003 | ||||||
| A school-based PA intervention improved PA and fitness and reduced adiposity in children. | |||||||
| Li et al. [50] | A multi-component PA intervention
| Weight: A lever scale Height: A stadiometer BMI = kg/m2 Duration of MVPA: Self-administered questionnaires | The reduction of BMI was statistically significant in the intervention group (−0.02 ± 0.06 kg/m2), compared with the increase of BMI in the control group (0.41 ± 0.08 kg/m2) (p < 0.001). The change in duration of MVPA in the intervention group (8.9 ± 4.3 min/day) was significantly different from that in the control group (−13.8 ± 3.3 min/day). |
| |||
| Lynch et al. [51] | Let’s Go! 5-2-1-0 Curriculum
| Healthy Habits: Survey BMI = kg/m2, median (Q1, Q3) PA: Pedometer (The Omron HJ-321 pedometer). | Intervention Group | Control Group | p |
| |
| BMI (kg/m2, median change: 0.2 | BMI (kg/m2, median change: 0.1 | 0.469 | |||||
| Number of pedometer steps per day (median): 2293.5 | Number of pedometer steps per day (median): 2651.3 | 0.929 | |||||
| There was no statistical difference in the improvement of healthy habits, BMI, or PA in the intervention group compared with the control group (p > 0.05). | |||||||
| Madsen et al. [52] | Energy Balance for Kids with Play (EB4K with Play)
| PA: Actigraph GT1M or GT3X accelerometer Cardiorespiratory fitness: 1-mile run Anthropometric measures: Standardised height and weight measurement Other variables: Fruit and vegetable consumption, dietary behaviors, dietary knowledge | Intervention and control group comparison adjusted difference | p |
| ||
| School-day PA: −0.1 | p > 0.05 | ||||||
| BMIz scores total: −0.07 | p > 0.05 | ||||||
| There were no group differences in change in PA or dietary behaviors, although BMIz decreased overall by −0.07 (p = 0.05). | |||||||
| Magnusson et al. [53] | School-Based PA Program
| Body fat percentage: A dual-energy x-ray scan (DEXA). Cardiorespiratory fitness (W/kg): A Monark ergometer bike | Intervention and control group comparison z scores | p |
| ||
| Cardiorespiratory fitness (W/kg: 0.37 | p = 0.18 | ||||||
| Waist circumference (cm): 0.15 | p = 0.53 | ||||||
| Skinfolds (mm): 0.10 | p = 0.52 | ||||||
| Body composition was not statistically significant (p > 0.05). Children in the intervention group increased their fitness by an average of 0.37 z score units more than the controls (p = 0.18). There was no significant difference in waist circumference and skinfold results (p > 0.05). | |||||||
| Shore et al. [54] | Step-Count Promotion
| PA: SW-401 DIGI-walker pedometer. Fitness Performance: Curl ups, shuttle run, endurance 1-mile run/walk, pull-ups, and sit and reach | Step-count (steps/d) Intervention Group | Step-count (steps/d) Control Group |
| ||
| Pre-test Mean (SD): 9692 (476) Post-test Mean (SD): −12,307 (679) | Pre-test Mean (SD): 9420 (446) Post-test Mean (SD): −10,608 (702) | ||||||
| Step-count promotion program significantly increased daily accrued step counts versus control (p < 0.05). Shuttle and mile run performance decreased from pre- to post-intervention in both groups. | |||||||
| Sigmund et al. [55] | PA Intervention program
| PA: Caltrac accelerometer and Yamax Digiwalker SW-200 pedometer | There was a significant increase in daily activity levels compared to the control group (from 1718 to 3247 steps per day; and from 2.1 to 3.6 Kcal/Kg per day). The school-based intervention allows children to take more than 10,500 steps and reduces the risk of declined PA. | ||||
| Thivel et al. [56] | PA program:
| BMI (kg/m2): A portable digital scale Height: A standing stadiometer (Seca model 720, Germany). Waist circumference: A level midway between the last rib and superior iliac crest. Cardiorespiratory fitness: The 20-m shuttle run test Peak power: A calibrated friction loaded ergometer. | PA levels at pre and post-test (Intervention) | PA levels at pre and post-test (Control) | |||
| Aerobic (stage) pre-test mean (SD): 3.10 (0.9) Aerobic (stage) pre-test mean (SD): 3.68 (1.1) | Aerobic (stage) pre-test mean (SD): 3.15 (1.14) Aerobic (stage) pre-test mean (SD): 3.31 (1.4) | ||||||
| Anaerobic and aerobic fitness levels were significantly improved in both lean and obese children (p < 0.05), but there was no significant change in anthropometric variables (p > 0.05). | |||||||
| Tian et al. [57] | PE intervention program
| PA Levels: The Children’s Leisure Activities Study Survey (CLASS) questionnaire Bodyweight: A portable electronic scale Height: Stadiometer Percentage of body fat was calculated from triceps and subscapular skinfolds measurements | PA levels at pre and post-test (Intervention) | PA levels at pre and post-test (Control) |
| ||
| Total PA (min/week) pretest mean (SD): 91.0 (43.9) Total PA (min/week) post-test mean (SD): 112.1 (66.4) | Total PA (min/week) pretest mean (SD): 93.7 (52.2) Total PA (min/week) post-test mean (SD): 92.4 (55.4) | ||||||
| No significant difference between intervention and control groups at pre and post-test measurements (p > 0.05). Moderate PA, vigorous PA and total PA significantly increased in the experimental group after the 12-week intervention program. | |||||||
| Vander Ploeg et al. [58] | APPLE School
| PA Levels: The Omron HJ-720 ITC time-stamped pedometer | Step-count (steps/d) APPLE Schools (2009) | Step-count (steps/d) APPLE Schools (2011) |
| ||
| School days, mean (SD): 11,371 (3306) School hours, mean (SD): 850 (233) | School days, mean (SD): 13,375 (3653) School hours, mean (SD): 933 (222) | ||||||
| Children were significantly more active in 2011 in comparison with 2009 (p < 0.001). Comprehensive school programs affect the levels of children’s PA during school. | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuksel, H.S.; Şahin, F.N.; Maksimovic, N.; Drid, P.; Bianco, A. School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 347. https://doi.org/10.3390/ijerph17010347
Yuksel HS, Şahin FN, Maksimovic N, Drid P, Bianco A. School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(1):347. https://doi.org/10.3390/ijerph17010347
Chicago/Turabian StyleYuksel, Hidayet Suha, Fatma Neşe Şahin, Nebojsa Maksimovic, Patrik Drid, and Antonino Bianco. 2020. "School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 1: 347. https://doi.org/10.3390/ijerph17010347
APA StyleYuksel, H. S., Şahin, F. N., Maksimovic, N., Drid, P., & Bianco, A. (2020). School-Based Intervention Programs for Preventing Obesity and Promoting Physical Activity and Fitness: A Systematic Review. International Journal of Environmental Research and Public Health, 17(1), 347. https://doi.org/10.3390/ijerph17010347








