Abstract
The purpose of this study was to analyze the relationship between elevated cardiovascular disease (CVD) risk and type of anesthesia by using the National Health Insurance Research Database (NHIRD) of Taiwan in a one-year follow-up period. We assessed whether general anesthesia (GA) or neuraxial anesthesia (NA) increased CVD occurrence in lower-limb fracture patients. Approximately 1 million patients were randomly sampled from the NHIRD registry. We identified and enrolled 3437 lower-limb fracture patients who had received anesthesia during operations conducted in the period from 2010 to 2012. Next, patients were divided into two groups, namely GA (n = 1504) and NA (n = 1933), based on the anesthetic technique received during surgery. Our results revealed that those receiving GA did not differ in their risk of CVD relative to those receiving NA, adjusted HR = 1.24 (95% CI: 0.80–1.92). Patients who received GA for more than 2 h also did not differ in their risk of CVD relative to those receiving NA for less than 2 h, adjusted HR = 1.43 (95% CI: 0.81–2.50). Moreover, in the GA group (i.e., patients aged ≥65 years and women), no significant difference for the risk of CVD events was observed. In conclusion, in our study, the difference in the risk of CVD between lower-limb fracture patients receiving NA and GA was not statistically significant. The incidence rate of CVD seemed to be more correlated with patients’ underlying characteristics such as old age, comorbidities, or admission to the intensive care unit. Due to the limited sample size in this study, a database which reviews a whole national population will be required to verify our results in the future.
1. Introduction
Anesthetic techniques can be classified as general anesthesia (GA), regional (caudal and neuraxial (spinal and epidural)) anesthesia, and peripheral nerve block. Choosing a suitable anesthetic technique can have benefits for patients. For some patients, physicians need to determine whether GA or neuraxial anesthesia (NA) is more suitable for a particular surgical procedure. GA has been reported to be a risk factor for dementia. In a mouse experiment, anesthetizing mice with ether vapors or sodium pentobarbital for short periods (30 s to 5 min) induced tau phosphorylation. In humans, this might increase the risk of postoperative cognitive impairment and the risk for Alzheimer’s disease. [1]. Isoflurane-treated AbetaPP mice had increased beta-amyloid protein aggregates in the brain [2]. Studies on the relationship between GA and AD have yielded inconsistent results. Another example includes a primiparous female who underwent cesarean delivery with epidural anesthesia, but not with spinal anesthesia, who was suggested to have an increased risk of subsequent chronic low back pain [3].
Cardiovascular disease (CVD) is one of the most common causes of morbidity and mortality worldwide. To date, CVD is the second leading cause of death in Taiwan. According to the definition of the World Health Organization, CVD is a group of disorders of the heart and blood vessels including coronary heart disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, and pulmonary embolism. Risk factors for CVD have been divided into invariable and variable risk factors. Invariable risk factors include age, sex, and genetic status [4]. However, known variable risk factors include improper lifestyle habits, such as smoking tobacco and poor exercise and eating habits. Other risk factors associated with CVD include the presence of underlying diseases such as arterial hypertension, diabetes mellitus, dyslipidemia, cholesterol, and obesity. In addition, myocardial injury after noncardiac surgery (MINS) might be important factor in cardiovascular events during perioperative complications [5]. Hip fracture was found to be one of the risk factors for MINS during the pre-operative period [6].
Anesthesia types are unique to each individual patients with ASA (American Society of Anesthesiologists) physical status or multiple comorbidities and types of surgery, even in different hospital [7]. As such, the purpose of physicians and anesthesiologists in deciding the method of anesthesia (GA or NA) is to reduce the risk of complications, promote faster recovery, minimize surgical stress response, and improve post anesthesia outcome [8]. In previous literature reviews, the advantages and risks of GA and NA have been compared. For cesarean section, NA was linked with a shorter duration of hospitalization than GA [9]. The opioid-sparing effects of NA were associated with a better quality of recovery in patients after the surgical procedure [10]. A meta-analysis indicated that the use of NA for hip joint replacement may have better outcomes, including a lower blood transfusion requirement and a decrease in deep venous thrombosis or pulmonary embolism and serious complications [11]. In addition, the long-term effects of anesthesia remain unknown. Although NA may be associated with a relatively lower risk on several aspects and a better outcome when compared with GA, more studies are required for verification. Therefore, to determine whether GA or NA have shown benefits and better outcome for patient with lower limbs fracture surgery, we compared the association of GA and NA with CVD risk in lower-limb fracture patients at the one-year follow-up period. The purpose of this study was to investigate the risk of CVD in patients with GA and NA. The hypothesis was that GA and NA have significant differences in CVD risk.
2. Experimental Section
2.1. Data Sources
The Longitudinal Health Insurance Database (LHID) is managed by the Taiwan National Health Research Institutes. One million randomly sampled beneficiaries were recruited with all outpatient and inpatient medical claims including drug medications, medical operations, procedures, and fees. The study was approved by the Ethical Review Board of Chung Shan Medical University Hospital (CS18096).
2.2. Study Groups
This study used a retrospective cohort study design. All recruited patients were aged 18 years or older, had lower-limb fractures (ICD-9-CM codes 820–827), and underwent an operation with anesthesia between 1 January 2010, and 31 December 2012. The index date was defined as the first date of lower-limb fracture. To eliminate confounding from a past disease or re-anesthesia surgery, we excluded patients with a CVD diagnosis before the index date or the requirement of anesthesia surgery again during the study period. The study population was divided into GA and NA groups by surgical codes (96005C, 96006C, 96007C, 96008C, 96017C, 96018C, 96019C, 96020C, 96021C, and 96022C). NA included spinal and epidural anesthesia.
2.3. Outcome and Covariate Measurement
The study endpoint was the diagnosis of new-onset CVD, including ischemic heart disease (ICD-9-CM codes 410, 411, 413, 414), heart failure (ICD-9-CM codes 428), and cerebrovascular disease (ICD-9-CM codes 430–437) during emergency or hospitalization. All patients were followed until one year until the occurrence of CVD, withdrawal from the social insurance system, or the end of follow-up, whichever came first. Covariates were age, sex, hypertension (ICD-9-CM codes 401–405), hyperlipidemia (ICD-9-CM codes 272.0–272.4), diabetes (ICD-9-CM code 250), renal disease (ICD-9-CM codes 582, 583.0–583.7, 585, 586, and 588), liver disease (ICD-9-CM codes 456.0, 456.1, 456.2, 571.2, 571.4, 571.5, 571.6, 572.2, 572.3, 572.4, and 572.8), chronic pulmonary disease (ICD-9-CM codes 490–496, 500–505, and 506.4), and usage of anticoagulants (aspirin/clopidogrel/warfarin). From the LHID, we were unable to obtain personal behavioral information such as smoking, alcohol consumption, and laboratory data. In this study, we used chronic pulmonary disease and liver disease as substitutes for the indirect control of smoking and alcohol consumption interference. Other comorbidity choices, such as hypertension, hyperlipidemia, diabetes, and renal disease are all potential CVD risk factors. These covariates were defined before the index date. Furthermore, admission into the intensive care unit (ICU) was considered to control the severity of lower-limb fractures in both groups.
2.4. Statistical Analysis
To compare GA and NA, the chi-squared test or independent t test was used, as appropriate. The cumulative incidence of CVD cases was analyzed using Kaplan–Meier analysis, and the significance was calculated using the log-rank test. The Cox proportional hazard model was used to estimate the hazard ratios of CVDs. A sensitivity analysis of risk of CVD events was also conducted for different follow-up periods. Statistical analyses were performed using SPSS V.18.0 (SPSS, Chicago, Il, USA). A p-value less than 0.05 was considered statistically significant.
3. Results
3.1. Characteristics of Study Subjects
A total of 6319 patients with lower-limb fractures who received anesthesia during an operation were identified from 2010 to 2012. After excluding patients with CVD diagnosis and repeated anesthesia surgery during the study period, 3437 patients were enrolled in the study. Furthermore, patients were divided into two groups. One group received GA (n = 1504) and the other group received NA (n = 1933) during the surgery for lower-limb fractures (Figure 1). The distributions of age, sex, comorbidities, ICU admission, anticoagulants, anesthesia time, and hospital levels among patients receiving GA and NA are presented in Table 1. The mean age and standard deviation of patients receiving GA and NA were 50.7 ± 20.8 and 57.6 ± 20.8 years, respectively. The proportions of male patients receiving GA and NA were 52.1% and 50.7%, respectively.
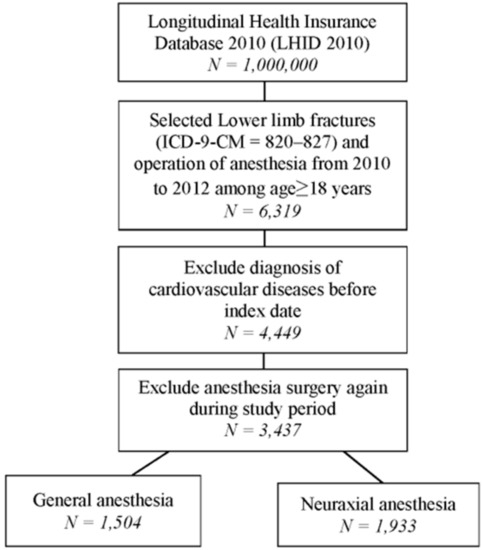
Figure 1.
Flow chart for patient selection.

Table 1.
Demographic characteristics of general anesthesia (GA) and neuraxial anesthesia (NA) groups.
3.2. Risk of CVD with General Anesthesia, Neuraxial Anesthesia, Age, Gender, Different Comorbidities, and Other Conditions
We estimated the cumulative incidence of CVD cases in patients who received GA and NA. The Kaplan–Meier curve of the cumulative probability of CVDs indicated that the GA group did not have a higher risk of CVDs within 1 year (log-rank test, p = 0.933; Figure 2). The Cox proportional hazard model revealed that the incidence of CVD did not differ in patients receiving GA than in patients receiving NA, HR = 1.24 (95% CI: 0.80–1.92). After adjustment for age, sex, comorbidities, ICU admission, and anticoagulants, patients aged 65 years or older (adjusted hazard ratio (HR): 5.77; 95% confidence interval [CI]: 3.21–10.38), male patients (adjusted HR: 1.89; 95% CI: 1.21–2.95), and patients with comorbidities, such as diabetes (adjusted HR: 2.09; 95% CI: 1.29–3.37), had a higher risk of developing a CVD. Patients who had been admitted to the ICU due to lower-limb fractures also had a higher risk of a CVD event occurring (adjusted HR: 2.59; 95% CI: 1.35–4.96; Table 2).
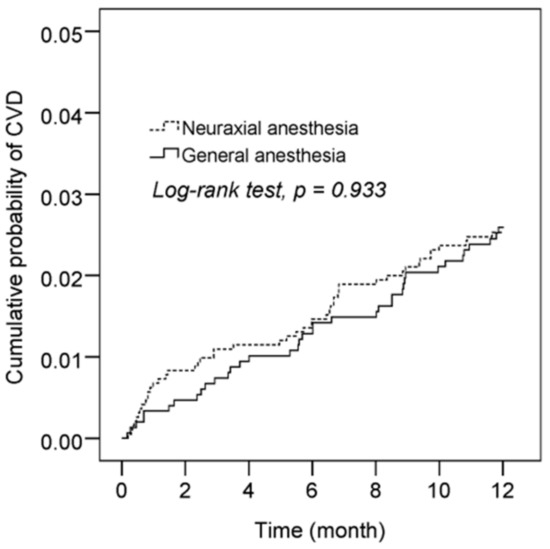
Figure 2.
Kaplan–Meier curves with a cumulative probability of cardiovascular disease (CVD) following GA and NA in lower-limb fracture patients.

Table 2.
Cox proportional hazard model of risk of CVD events among GA and NA groups.
3.3. Risk of CVD Between General Anesthesia and Neuraxial Anesthesia Patients and Specific Subgroup Characteristics
To determine whether the duration of both GA and NA affects the risk of CVD, both anesthesia groups were divided into less than 2 h and more than 2 h groups. Compared with patients who received NA for less than 2 h, patients who received GA for more than 2 h did not differ in their risk of developing a CVD (adjusted HR: 1.43; 95% CI: 0.81–2.50; Table 3). We also conducted a subgroup analysis between GA and NA patients. In stratification of age and gender, those receiving GA did not differ in their risk of CVD relative to those receiving NA (Table 4). A sensitivity analysis was conducted, which showed that the GA and NA groups did not have statistically significant differences in different follow-up periods (Table 5).

Table 3.
Subgroup analysis of the Cox proportional hazard model at anesthesia time.

Table 4.
Subgroup analysis of Cox proportional hazard model using age and sex.

Table 5.
Sensitivity analysis of risk of CVD events in different follow-up periods.
4. Discussion
In this study, a total of 3437 lower-limb fracture patients who received GA (n = 1504) or NA (n = 1933) were enrolled. The risk of CVD events did not differ in general anesthesia when compared with neuraxial anesthesia in the Cox proportional hazard model. To date, no studies have reported either GA or NA as a risk factor for the development of CVD. In contrast, CVDs have been described as postoperative outcomes of any type of anesthesia [12,13,14]. Generally, the postoperative time frame can range from 24 h to 30 days [13]. In our study, the average onset of CVDs in patients who received NA and GA was 4.8 and 6.0 months, respectively (Appendix A Table A1).
Risk factors for CVDs have accumulated rapidly. Underlying diseases, such as hypertension, atrial fibrillation, kidney failure, diabetes, aging, and sex are also risk factors for CVDs that have been reported for more than 20 years [4,15]. In our study, patients aged ≥65 years, male patients, and patients with diabetes were shown to have a higher risk of developing a CVD.
In this study, we found that lower-limb fracture patients admitted to the ICU had a higher risk of developing CVD relative to those lower-limb fracture patients that underwent surgery but through direct hospital admission. In fact, several studies have indicated that VTE might be a predisposing factor of CVDs [16,17,18]. In fact, patients with particularly serious diseases staying in the ICU could also have an increased risk of CVD. A cohort study indicated that intensive care patients with acute kidney injury (AKI) had an increased risk of heart failure or myocardial infarction up to three years after hospital discharge [19].
Recently, two meta-analyses indicated an association between intra-operative hypotension (IOH) and MINS. Gu’s group reviewed 14 cohort studies of IOH and MINS. They found that IOH was associated with increased risks of 30-day mortality and major adverse cardiac events (MACEs), especially myocardial injury and AKI after non-cardiac surgery [20]. Similarly, An’s group reviewed 15 observational studies of IOH and MINS. They found that IOH was associated with an increased risk of postoperative AKI and myocardial injury. In more detail, the duration of IOH lasting only more than 5 min was associated with an increased risk of 30-day mortality [21]. In particular, patients suffering from pre-existing CVDs may have increased risks of perioperative cardiovascular morbidity and mortality following noncardiac surgery. Therefore, physicians and anesthesiologists need to consider cardioprotective medication, anesthetic regimen choice, blood pressure management, and transfusion regimens carefully in order to decrease such CVD risk [22]. The development of intraoperative hypotension is known to be associated with MINS, intraoperative vasopressor use, postoperative sepsis, number of ventilator days, and the types and quantities of ICU sedative and narcotic use, just to name a few contributors.
The current study has some limitations. First, we did not have access to potentially relevant personal behavioral information such as smoking habits, alcohol consumption, body mass index, and the severity of lower-limb fracture. This is significant because smoking, drinking, and BMI (obesity) are risk factors for CVD, and these factors may be diversifying the type of anesthesia. Second, the dataset did not provide information regarding the types of anesthetic technique used in patients, clinical presentations, or laboratory data. Patients’ individual statuses, presence of severity of lower limbs fracture and bleeding profile laboratory data may determine the type of anesthesia method selected by anesthesiologist. Third, the study subjects were not selected from the national population. Therefore, in consequence of limiting by the sample sizes that the study results may exist a wide confidence interval and corresponding lower power.
5. Conclusions
In summary, our study indicates that the difference in the risk of CVD between lower-limb fracture patients receiving NA and GA was not statistically significant. Owing to the limited sample size, further experiments are required to identify whether different anesthetic procedures are associated with differential risks of CVD in the future. For the application of anesthesia in different diseases, further study is needed for verification. Therefore, physicians themselves might decide to use GA or NA under different conditions.
Author Contributions
Conceptualization, H.-W.Y., L.-T.Y., C.-H.C. and C.-B.Y.; Validation, S.-F.Y. and S.-W.H.; Formal analysis, H.-W.Y., Y.-H.C., Y.-T.Y. (Ying-Tung Yeh) and Y.-T.Y. (Ying-Ting Yeh); Writing—original draft preparation, H.-W.Y., L.-T.Y., C.-H.C. and C.-B.Y.; Writing—review & editing, S.-W.H., S.-F.Y., Y.-T.Y. (Ying-Tung~Yeh), C.-H.C. and C.-B.Y. All authors have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
This study was partly based on data from the NHIRD provided by the NHI Administration, Ministry of Health and Welfare and managed by the National Health Research Institutes (registration number: NHIRD-104-148). The interpretation and conclusions contained herein do not represent those of the NHI Administration, Ministry of Health and Welfare, or National Health Research Institutes.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Track time of CVD following general anesthesia and neuraxial anesthesia.
Table A1.
Track time of CVD following general anesthesia and neuraxial anesthesia.
| Neuraxial Anesthesia | General Anesthesia | |
|---|---|---|
| Follow-up duration (month, mean ± SD) | 11.6 ± 2 | 11.5 ± 2.0 |
| Time to CVD (month, mean ± SD), N = 86 | 4.8 ± 3.6 | 6.0 ± 3.8 |
CVD: cardiovascular diseases.
References
- Run, X.; Liang, Z.; Zhang, L.; Iqbal, K.; Grundke-Iqbal, I.; Gong, C.X. Anesthesia induces phosphorylation of tau. J. Alzheimer′s Dis. JAD 2009, 16, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Perucho, J.; Rubio, I.; Casarejos, M.J.; Gomez, A.; Rodriguez-Navarro, J.A.; Solano, R.M.; De Yebenes, J.G.; Mena, M.A. Anesthesia with isoflurane increases amyloid pathology in mice models of alzheimer′s disease. J. Alzheimer′s Dis. JAD 2010, 19, 1245–1257. [Google Scholar] [CrossRef] [PubMed]
- Chia, Y.Y.; Lo, Y.; Chen, Y.B.; Liu, C.P.; Huang, W.C.; Wen, C.H. Risk of chronic low back pain among parturients who undergo cesarean delivery with neuraxial anesthesia: A nationwide population-based retrospective cohort study. Medicine 2016, 95, e3468. [Google Scholar] [CrossRef] [PubMed]
- Francula-Zaninovic, S.; Nola, I.A. Management of measurable variable cardiovascular disease′ risk factors. Curr. Cardiol. Rev. 2018, 14, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Recommendations for use of an isoniazid-rifapentine regimen with direct observation to treat latent mycobacterium tuberculosis infection. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 1650–1653. [Google Scholar]
- Devereaux, P.J.; Sessler, D.I. Cardiac complications in patients undergoing major noncardiac surgery. N. Engl. J. Med. 2015, 373, 2258–2269. [Google Scholar] [CrossRef]
- Fitz-Henry, J. The asa classification and peri-operative risk. Ann. R. Coll. Surg. Engl. 2011, 93, 185–187. [Google Scholar] [CrossRef]
- Gelb, A.W.; Morriss, W.W.; Johnson, W.; Merry, A.F.; Abayadeera, A.; Belii, N.; Brull, S.J.; Chibana, A.; Evans, F.; Goddia, C.; et al. World health organization-world federation of societies of anaesthesiologists (who-wfsa) international standards for a safe practice of anesthesia. Anesth. Analg. 2018, 126, 2047–2055. [Google Scholar] [CrossRef]
- Fassoulaki, A.; Petropoulos, G.; Staikou, C.; Siafaka, I.; Sarantopoulos, C. General versus neuraxial anaesthesia for caesarean section: Impact on the duration of hospital stay. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2009, 29, 25–30. [Google Scholar] [CrossRef]
- Catro-Alves, L.J.; De Azevedo, V.L.; De Freitas Braga, T.F.; Goncalves, A.C.; De Oliveira, G.S., Jr. The effect of neuraxial versus general anesthesia techniques on postoperative quality of recovery and analgesia after abdominal hysterectomy: A prospective, randomized, controlled trial. Anesth. Analg. 2011, 113, 1480–1486. [Google Scholar] [CrossRef]
- Mauermann, W.J.; Shilling, A.M.; Zuo, Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: A meta-analysis. Anesth. Analg. 2006, 103, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Pang, Q.Y.; Chen, B.; Liu, H.L. Effect of anesthesia methods on postoperative major adverse cardiac events and mortality after non-cardiac surgeries: A systematic review and meta-analysis. Minerva Anestesiol. 2017, 83, 749–761. [Google Scholar] [PubMed]
- Belmont, P.J., Jr.; Goodman, G.P.; Kusnezov, N.A.; Magee, C.; Bader, J.O.; Waterman, B.R.; Schoenfeld, A.J. Postoperative myocardial infarction and cardiac arrest following primary total knee and hip arthroplasty: Rates, risk factors, and time of occurrence. J. Bone Jt. Surg. Am. 2014, 96, 2025–2031. [Google Scholar] [CrossRef] [PubMed]
- You, A.H.; Han, D.W.; Ham, S.Y.; Lim, W.; Song, Y. Serum alkaline phosphatase as a predictor of cardiac and cerebrovascular complications after lumbar spinal fusion surgery in elderly: A retrospective study. J. Clin. Med. 2019, 8, 1111. [Google Scholar] [CrossRef] [PubMed]
- Costantino, S.; Paneni, F.; Cosentino, F. Ageing, metabolism and cardiovascular disease. J. Physiol. 2016, 594, 2061–2073. [Google Scholar] [CrossRef] [PubMed]
- Ageno, W.; Becattini, C.; Brighton, T.; Selby, R.; Kamphuisen, P.W. Cardiovascular risk factors and venous thromboembolism: A meta-analysis. Circulation 2008, 117, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ljungqvist, M.; Holmstrom, M.; Kieler, H.; Odeberg, J.; Larfars, G. Cardiovascular disease and mortality after a first episode of venous thromboembolism in young and middle-aged women. Thromb. Res. 2016, 138, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Roshani, S.; Lijfering, W.M.; Coppens, M.; Hamulyak, K.; Prins, M.H.; Buller, H.R.; Middeldorp, S. Risk factors of arterial cardiovascular complications in patients with prior venous thromboembolism. Neth. J. Med. 2011, 69, 27–30. [Google Scholar]
- Gammelager, H.; Christiansen, C.F.; Johansen, M.B.; Tonnesen, E.; Jespersen, B.; Sorensen, H.T. Three-year risk of cardiovascular disease among intensive care patients with acute kidney injury: A population-based cohort study. Crit. Care (Lond. Engl.) 2014, 18, 492. [Google Scholar] [CrossRef]
- Gu, W.J.; Hou, B.L.; Kwong, J.S.W.; Tian, X.; Qian, Y.; Cui, Y.; Hao, J.; Li, J.C.; Ma, Z.L.; Gu, X.P. Association between intraoperative hypotension and 30-day mortality, major adverse cardiac events, and acute kidney injury after non-cardiac surgery: A meta-analysis of cohort studies. Int. J. Cardiol. 2018, 258, 68–73. [Google Scholar] [CrossRef]
- An, R.; Pang, Q.Y.; Liu, H.L. Association of intra-operative hypotension with acute kidney injury, myocardial injury and mortality in non-cardiac surgery: A meta-analysis. Int. J. Clin. Pract. 2019, 73, e13394. [Google Scholar] [CrossRef] [PubMed]
- Janssen, H.; Dehne, S.; Giannitsis, E.; Weigand, M.A.; Larmann, J. [Perioperative cardiovasular morbidity and mortality in noncardiac surgical interventions: Measures for optimal anesthesiological care]. Der Anaesthesist 2019, 68, 653–664. [Google Scholar] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).