The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Design and Task
2.3. Measures
2.3.1. Dynamic Lung Function
2.3.2. Maximal Inspiratory Pressure
2.3.3. Aerobic Endurance Measurement
2.3.4. Inspiratory Muscle Training
2.3.5. Incremental Endurance Training
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Effects of Inspiratory Muscle Training on Inspiratory Muscle Function and PImax
4.2. Mechanisms of Improvement in Aerobic Endurance Performance
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Barros, R.; Misuta, M.; Menezes, R.; Figueroa, P.; Moura, F.; Cunda, S.; Leite, H. Analysis of the distances covered by first division Brazilian soccer players obtained with an automatic tracking method. J. Sport Sci. Med. 2006, 6, 233–244. [Google Scholar]
- Di Salvo, V.; Baron, R.; Tschan, H.; Calderon, Montero, F.J.; Bachl, H.; Pigozzi, F. Performance characteristic according to playing position in elite soccer. Int, J. Sports Med. 2007, 3, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Novack, L.F.; de Souza, G.C.; Szymczak Conde, J.H.; de Souza, R.O.; Osiecki, R. Quantification of match internal load and its relationship with physical fitness and recovery state of professional soccer athletes during the competitive period. Hum. Mov. 2018, 19, 30–37. [Google Scholar] [CrossRef]
- Reilly, T.; Ball, D. The net physiological cost of dribbling a soccer ball. Res. Q Exerc. Sport. 1984, 55, 67–71. [Google Scholar] [CrossRef]
- Bangsbo, J.; Nørregaard, L.; Thorsøe, F. Activity profile of competition soccer. Can. J. Sport Sci. 1991, 16, 110–116. [Google Scholar]
- Bangsbo, J. Energy demands in competitive soccer. J. Sports Sci. 1994, 12, 5–12. [Google Scholar] [CrossRef]
- Pate, R.R.; Kriska, A. Physiological basis of the sex difference in cardiorespiratory endurance. Sports Med. 1984, 1, 87–98. [Google Scholar] [CrossRef]
- Hoff, J.; Wisløff, U.; Engen, L.C.; Kemi, O.J.; Helgerud, J. Soccer specific aerobic endurance training. Br. J. Sports Med. 2002, 36, 218–221. [Google Scholar] [CrossRef]
- Mohr, M.; Krustrup, P.; Bangsbo, J. Match performance of high-standard soccer players with special reference to development of fatigue. J. Sports Sci. 2003, 21, 519–528. [Google Scholar] [CrossRef]
- Rebelo, A.; Brito, J.; Seabra, A.; Oliveira, J.; Krustrup, P. Physical match performance of youth football players in relation to physical capacity. Eur. J. Sport Sci. 2014, 1, 148–156. [Google Scholar] [CrossRef]
- Stølen, T.; Chamari, K.; Castagna, C.; Wisløff, U. Physiology of soccer: An update. Sports Med. 2005, 35, 01–536. [Google Scholar]
- Da Silva, C.D.; Bloomfield, J.; Marins, J.C. A review of stature, body mass and maximal oxygen uptake profiles of U17, U20 and first division players in Brazilian soccer. J. Sports Sci. Med. 2008, 7, 309–319. [Google Scholar] [PubMed]
- Nikolaidis, P.T. Cardiorespiratory power across adolescence in male soccer players. Hum. Physiol. 2011, 37, 636–641. [Google Scholar] [CrossRef]
- McMillan, K.; Helgerud, J.; Macdonald, R.; Hoff, J. Physiological adaptations to soccer specific endurance training in professional youth soccer players. Br. J. Sports Med. 2005, 39, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Hoff, J.; Helgerud, J. Endurance and strength training for soccer players. Physiological considerations. Sports Med. 2004, 34, 165–180. [Google Scholar]
- Castagna, C.; Impellizzeri, F.M.; Belardinelli, R.; Abt, G.; Coutts, A.; Chamari, K.; D’Ottavio, S. Cardiorespiratory responses to Yo-Yo intermittent endurance test in nonelite youth soccer players. J. Strength Cond. Res. 2006, 20, 326–330. [Google Scholar]
- Tønnessen, E.; Hem, E.; Leirstein, S.; Haugen, T.; Seiler, S. Maximal Aerobic Power Characteristics of Male Professional Soccer Players, 1989–2012. Int. J. Sports Physiol. Perform. 2013, 8, 323–329. [Google Scholar] [CrossRef]
- Wisloff, U.; Helgerud, J.; Hoff, J. Strength and endurance of elite soccer players. Med. Sci. Sports Exerc. 1998, 30, 462–467. [Google Scholar] [CrossRef]
- Wagner, P.D. Determinants of maximal oxygen transport and and utilization. Annu. Rev. Physiol. 1996, 58, 21–50. [Google Scholar] [CrossRef]
- Higino, W.P.; de Souza Sorroche, A.; de Mattos Falqueiro, P.G.; Lima, Y.C.S.; Higa, C.L. Determination of Aerobic Performance in Youth Soccer Players: Effect of Direct and Indirect Methods. J. Hum. Kinet. 2017, 56, 109–118. [Google Scholar] [CrossRef]
- Silva, J.F.; Guglielmo, L.G.A.; Carminatti, L.J.; Oliveira, F.R.; Dittrich, N.; Paton, C.D. Validity and reliability of a new field test (Carminatti’s test) for soccer players compared with laboratory-based measures. J. Sports Sci. 2011, 29, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
- McConnell, K. Respiratory muscle training as an ergogenic aid. J. Exerc. Sci. Fit. 2008, 7, 18–27. [Google Scholar] [CrossRef]
- Enright, S.J.; Unnithan, V.B. Effect of inspiratory muscle training intensities on pulmonary function and work capacity in subjects who are healthy. Phys. Ther. 2006, 86, 245–354. [Google Scholar]
- Silva, R.L.C.; Hall, E.; Maior, A.S. Inspiratory muscle training improves performance of a repeated sprints ability test in professional soccer players. J. Bodyw. Mov. Ther. 2019, 23, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, M.; Kurosawa, H.; Kohzuki, M. Effects of inspiratory and expiratory muscle training in normal subjects. J. Jpn. Phys. Ther. Assoc. 2005, 8, 29–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guy, J.H.; Edwards, A.M.; Deakin, G.B. Inspiratory muscle training improves exercise tolerance in recreational soccer players without concomitant gain in soccer-specific fitness. J. Strength Cond. Res. 2014, 28, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Ozmen, T.; Gunes, G.Y.; Ucar, I. Effect of respiratory muscle training on pulmonary function and aerobic endurance in soccer players. J. Sports Med. Phys. Fit. 2017, 57, 507–513. [Google Scholar]
- Archiza, B.; Andaku, D.K.; Caruso, F.C.R.; Bonjorno, J.C., Jr.; Oliveira, C.R.; Ricci, P.A.; Amaral, A.C.D.; Mattiello, S.M.; Libardi, C.A.; Phillips, S.A.; et al. Effects of inspiratory muscle training in professional women football players: A randomized sham-controlled trial. J. Sports Sci. 2018, 36, 771–780. [Google Scholar] [CrossRef]
- Ross, E.Z.; Nowieky, A.V.; McConnell, A.K. Influence of acute inspiratory loading upon diaphragm motor-evoked potentials in healthy humans. J. Appl. Physiol. 2007, 102, 1883–1890. [Google Scholar] [CrossRef]
- Brown, P.I.; Sharpe, G.R.; Johnson, M.A. Inspiratory muscle training reduces blood lactate concentration during volitional hyperpnoea. Eur. J. Appl. Physil. 2008, 104, 111–117. [Google Scholar] [CrossRef]
- Downey, A.E.; Chenoweth, L.M.; Townsend, D.K.; Ramum, J.D.; Ferguson, C.S.; Harms, C.A. Effects of inspiratory muscle training on exercise responses in normoxia and hypoxia. Respir. Physiol. Neurobiol. 2007, 156, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Mickleborough, T.D.; Stager, J.M.; Chatham, K.; Lindley, M.R.; Ionescu, A.A. Pulmonary adaptations to swim and inspiratory muscle training. Eur. J. Appl. Physiol. 2008, 103, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Majewska-Pulsakowska, M.; Wytrychowski, K.; Rożek-Piechura, K. The Role of Inspiratory Muscle Training in the Process of Rehabilitation of Patients with Chronic Obstructive Pulmonary Disease. Adv. Exp. Med. Biol. 2016, 885, 47–51. [Google Scholar] [PubMed]
- Bach, J.R.; Gonçalves, M.R.; Páez, S.; Winck, J.C.; Leitão, S.; Abreu, P. Expiratory flow maneuvers in patients with neuromuscular diseases. Am. J. Phys. Med. Rehabil. 2006, 85, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Bach, J.R. Maximum insufflation capacity: The relationships with vital capacity and cough flows for patients with neuromuscular disease. Am. J. Phys. Med. Rehabil. 2000, 79, 222–227. [Google Scholar] [CrossRef]
- Nunn, A.J.; Gregg, I. New regression equations for predicting peak expiratory flow in adults. BMJ 1989, 298, 1068–1070. [Google Scholar] [CrossRef]
- Black, L.F.; Hyatt, R.E. Maximal respiratory pressures: Normal values and relationship to age and sex. Am. Rev. Resp. Dis. 1969, 99, 696–702. [Google Scholar]
- Tudorache, V.; Oancea, C.; Mlădinescu, O. Clinical relevance of maximal inspiratory pressure: Determination in COPD exacerbation. Int. J. Chron. Obstruct. Pulmon. Dis. 2010, 5, 119–123. [Google Scholar]
- Baker, D.; Coleman, D.A.; Wiles, J. The reliability of responses to repeated laboratory assessment: The evaluation of a preload-performance protocol in runners. In Proceedings of the BASES (The British Association of Sport and Exercise Sciences) Student Conference, University of Chester, Chester, UK, 12–13 April 2011. [Google Scholar]
- Ronan, J.T.; Shafer, A.B. Concurrent validity of the five-minute pyramid test for VO2max estimation in healthy young adults. Hum. Mov. 2019, 20, 41–45. [Google Scholar] [CrossRef]
- Zwiren, L.D.; Freedson, P.S.; Ward, A.; Wilke, S.; Rippe, J.M. Estimation of VO2max: A comparative analysis of five exercise tests. Res. Q Exerc. Sport 1991, 62, 73–78. [Google Scholar] [CrossRef]
- Grant, S.; Corbett, K.; Amjad, A.M.; Wilson, J.; Aitchison, T. A comparison of methods of predicting maximum oxygen uptake. Br. J. Sports Med. 1995, 29, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Reilly, T.; Bangsbo, J.; Franks, A. Anthropometric and physiological predispositions for elite soccer. J. Sports Sci. 2000, 18, 669–683. [Google Scholar] [CrossRef] [PubMed]
- Aznar-Lain, S.; Webster, A.L.; Cañete, S.; San Juan, A.F.; López Mojares, L.M.; Pérez, M.; Lucia, A.; Chicharro, J.L. Effects of inspiratory muscle training on exercise capacity and spontaneous physical activity in elderly subjects: A randomized controlled pilot trial. Int. J. Sports Med. 2007, 28, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- Lemaitre, F.; Coquart, J.; Chavallard, F.; Castres, I.; Mucci, P.; Costalat, G.; Chollet, D. Effect of additional respiratory muscle endurance training in young well-trained swimmers. J. Sports Sci. Med. 2013, 12, 630–638. [Google Scholar]
- Wells, G.D.; Plyley, M.; Thomas, S.; Goodman, L.; Duffin, J. Effects of concurrent inspiratory and expiratory muscle training on respiratory and exercise performance in competitive swimmers. Eur. J. Appl. Physiol. 2005, 94, 527–540. [Google Scholar] [CrossRef]
- Romer, L.M.; McConnell, A.K.; Jones, D.A. Effects of inspiratory muscle training on time-trial performance in trained cyclists. J. Sport Sci. 2002, 20, 547–562. [Google Scholar] [CrossRef]
- McMahon, M.E.; Boutellier, U.; Smith, R.M.; Spengler, C.M. Hyperpnea training attenuates peripheral chemo-sensitivity and improves cycling endurance. J. Exp. Biol. 2002, 205, 3937–3943. [Google Scholar]
- Volianitis, S.; McConnell, A.K.; Koutedakis, Y.; McNaughton, L.; Backx, K.; Jones, D.A. Inspiratory muscle training improves rowing performance. Med. Sci. Sports Exerc. 2001, 33, 803–809. [Google Scholar] [CrossRef]
- Wohlgemuth, M.; van der Kooi, E.L.; Hendriks, J.C.; Padberg, G.W.; Folgering, H.T. Face mask spirometry and respiratory pressures in normal subjects. Eur. Respir. J. 2003, 22, 1001–1006. [Google Scholar] [CrossRef]
- El-Deen, H.A.B.; Alanazi, F.S.; Ahmed, K.T. Effects of inspiratory muscle training on pulmonary functions and muscle strength in sedentary hemodialysis patients. J. Phys. Ther. Sci. 2018, 30, 424–427. [Google Scholar] [CrossRef][Green Version]
- Kovelis, D.; Pitta, F.; Probst, V.S.; Peres, C.P.; Delfino, V.D.; Mocelin, A.J.; Brunetto, A.F. Pulmonary function and respiratory muscle strength in chronic renal failure patients on hemodialysis. J. Bras. Pneumol. 2008, 34, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Wells, C.M.; Edwards, A.M.; Winter, E.M.; Fysh, M.L.; Drust, B. Sport-specific fitness testing differentiates professional from amateur soccer players where VO2max and VO2 kinetics do not. J. Sport Med. Phys. Fit. 2012, 52, 245–254. [Google Scholar]
- Mickleborough, T.D.; Nichols, T.; Lindley, M.R.; Chatham, K. Inspiratory flow resistive loading improves respiratory muscle function and endurance capacity in recreational runners. Scand. J. Med. Sci. Sports 2010, 20, 458–468. [Google Scholar] [CrossRef] [PubMed]
- Nicks, C.R.; Morgan, D.W.; Fuller, D.K.; Caputo, J.L. The influence of respiratory muscle training upon intermittent exercise performance. Int. J. Sports Med. 2009, 30, 16–21. [Google Scholar] [CrossRef]
- Boutellier, U.; Buchel, R.; Kundert, A.; Spengler, C. The respiratory system as an exercise limiting factor in normal trained subjects. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 347–353. [Google Scholar] [CrossRef]
- Pine, M.; Murphy, A.; Watsford, M.; Coutts, A. Specific respiratory muscle training: The effects of various training strategies upon repeat sprint performance. J. Sci. Med. Sport 2005, 8, 64. [Google Scholar] [CrossRef]
- Morgan, D.W.; Kohrt, W.M.; Bates, B.J.; Skinner, J.S. Effects of respiratory muscle endurance training on ventilatory and endurance performance of moderately trained cyclists. Int. J. Sports Med. 1987, 8, 88–93. [Google Scholar] [CrossRef]
- Kilding, E.A.; Brown, S.; McConnell, K. Inspiratory muscle training improves 100 and 200 m swimming performance. Eur. J. Appl. Physiol. 2010, 108, 505–511. [Google Scholar] [CrossRef]
- Sperlich, B.; Fricke, H.; de Marees, M.; Linville, J.W.; Mester, J. Does respiratory muscle training increase physical performance? Mil. Med. 2009, 174, 977–982. [Google Scholar] [CrossRef]
- Azizimasouleh, M.; Razmjoo, S.; Hasan, H.S.; Pezhman, A. Effect of respiratory muscles training on swimming performance of elite female swimmers. Ann. Biol. Res. 2012, 3, 196–203. [Google Scholar]
- McConnell, A.K.; Romer, L.M. Dyspnoea in health and obstructive pulmonary disease: The role of respiratory muscle function and training. Sports Med. 2004, 34, 117–132. [Google Scholar] [CrossRef]
- Coast, J.R.; Clifford, P.S.; Henrich, T.W.; Stray-Gundersen, J.; Johnson, R.L., Jr. Maximal inspiratory pressure following maximal exercise in trained and untrained subjects. Med. Sci. Sports Exerc. 1990, 22, 811–815. [Google Scholar] [CrossRef]
| Training Period | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 | Week 7 | Week 8 |
|---|---|---|---|---|---|---|---|---|
| Inspiratory Muscle Training | ||||||||
| Training load (cmH2O) | 40% PImax | 45% PImax | 50% PImax | 55% PImax | 60% PImax | 70% PImax | 75% PImax | 80% PImax |
| Time/session (min.) | 5 | 7 | 9 | 10 | 12 | 13 | 14 | 15 |
| Periodized endurance running training | ||||||||
| 6 km | 5.30 min/km | 5.20 min/km | 5.10 min/km | 5.05 min/km | - | - | - | - |
| 3 × (5 × 200 m) | - | - | - | - | 42 s | 42 s | 40 s | 38 s |
| Parameters | IMT Group | Control Group | p |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (year) | 17.63 ± 0.48 | 17.71 ± 0.45 | 0.7365 |
| Height, cm | 182 ± 0.05 | 180 ± 0.05 | 0.7881 |
| Mass, kg | 68.88 ± 4.48 | 69 ± 3.34 | 0.950 |
| BMI | 20.89 ± 0.56 | 21.20 ± 0.84 | 0.45 |
| Variables | Experimental Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre- | Post- | % Differ | d | Pre- | Post- | % Differ | d | |
| VC(l) | 5.49 ± 0.56 | 5.42 ± 0.76 | 1.18 | 0.11 | 4.9 ± 0.83 | 5.15 ± 1. 05 | 5.10 | 0.28 |
| VC (%) | 111.13 ± 7.39 | 107. 08 ± 7.5 | 3.65 | 0.56 | 96.97 ± 15.74 | 102.14 ± 13.02 | 5.33 | 0.38 |
| FVC (l) | 5.65 ± 0.75 | 6.04 ± 0.78 | 6.90 | 0.55 | 5.63 ± 0.69 | 5.7 ± 0.67 | 1.24 | 0.11 |
| FVC (%) | 112.98 ± 9.24 | 121 ± 7.57 | 7.09 | 1.01 | 107.47 ± 13.27 | 106.13 ± 13.3 | 1.25 | 0.10 |
| FEV1(l) | 4.8 ± 0.57 | 5.31 ± 0.67 | 10.62 | 0.88 | 4.55 ± 0.81 | 4.7 ± 0.77 | 3.29 | 0.20 |
| FEV1 (%) | 113.15 ± 10.79 | 125.11 ± 10.83 | 10.57 | 1.18 | 98.03 ± 12.7 | 104.71 ± 14.97 | 1.57 | 0.51 |
| PEF (l/s) | 6.77 ± 1.44 | 7.7 ± 1.48 | 13.73 | 0.73 | 5.97 ± 1.95 | 6.36 ± 1.61 | 6.53 | 0.23 |
| PEF (%) | 82.57 ± 18.31 | 93 ± 16.9 | 12.64 | 0.63 | 83.56 ± 16.33 | 91.76 ± 8.08 | 9.81 | 0.68 |
| PImax (kPa) | 6.85 ± 0.39 | 11.15 ± 1.07 | 12.63 | 5.73 | 6.39 ± 0.60 | 7.49 ± 0.86 | 17.21 | 1.59 |
| PImax (%) | 85.75 ± 5.02 | 138.08 ± 16.21 | 61.02 | 4.66 | 82.75 ± 3,46 | 97.08 ± 4,53 | 17.31 | 3.80 |
| PEmax(kPa) | 4.02 ± 2.52 | 8.04 ± 2.26 | 100 | 1.79 | 3.51 ± 1.54 | 3.93 ± 1.99 | 3.42 | 0.25 |
| PEmax (%) | 84.62 ± 4.7 | 128.4 ± 14.3 | 51.73 | 4.39 | 83.2 ± 4.5 | 96.4 ± 3.9 | 15.86 | 3.35 |
| Variables | IMT-Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre- | Post- | p | d | Pre- | Post- | p | d | |
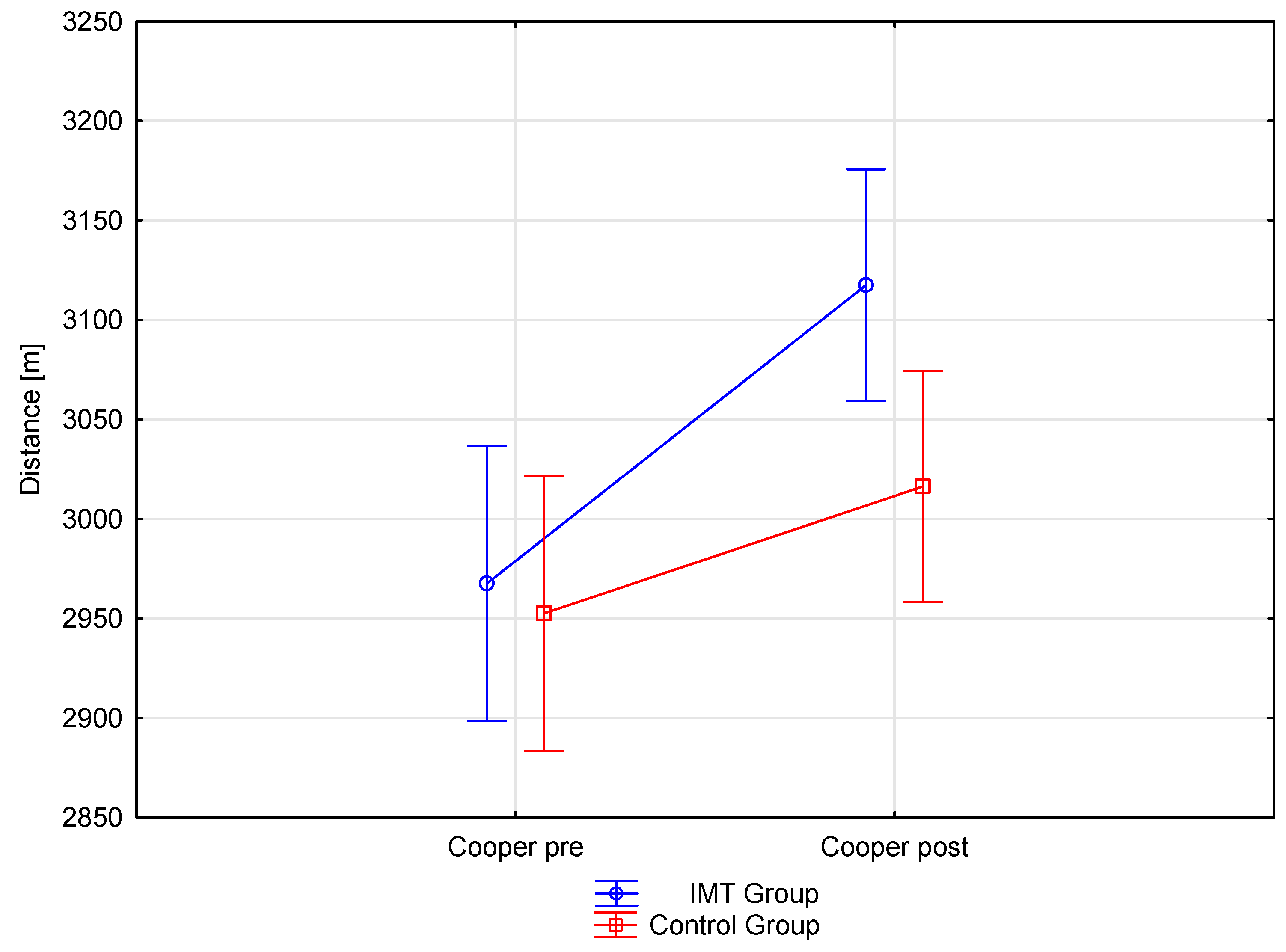
| Distance (m) | 2967.50 ± 79.24 | 3117.50 ± 72.85 * | 0.00 * | 2.06 | 2952.50 ± 101.38 | 3016.25 ± 80.34 * | 0.00 * | 0.74 |
| VO2max (mL/kg/min) | 55.11 ± 1.88 | 58.41 ± 1.63 | 0.00 * | 3.32 | 54.75 ± 2.22 | 55.95 ± 1.80 | 0.00 * | 0.63 |
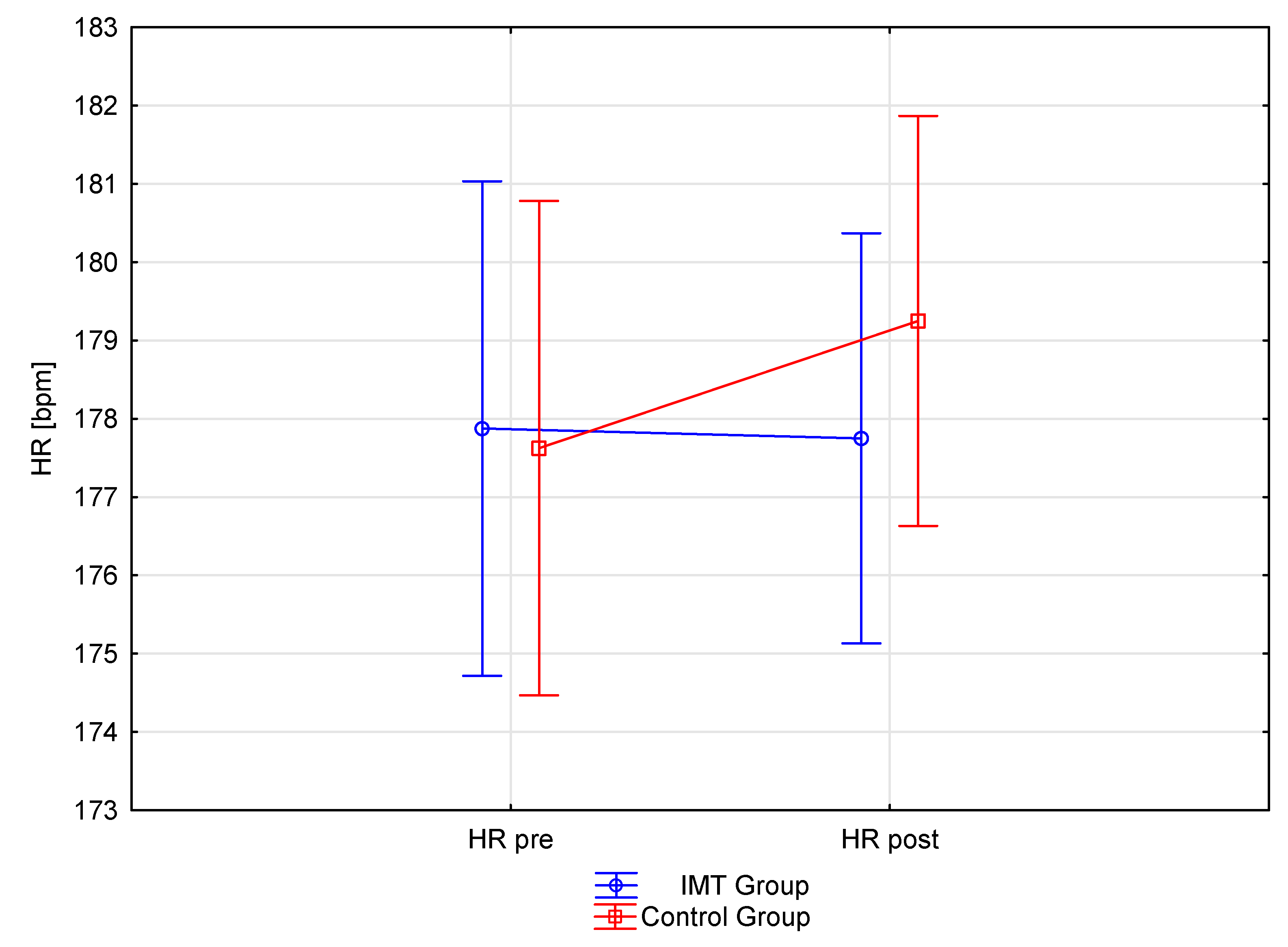
| HR max (bpm) | 177.87 ± 4.73 | 177.75 ± 3.53 | 0.87 | 0.03 | 177.62 ± 3.50 | 179.25 ± 3.3 | 0.07 | 0.50 |
| Variable | IMT Group | Control Group | IMT Group-Control Group | IMT Group-Control Group |
|---|---|---|---|---|
| Pre-Post | Pre-Post | Pre-Pre | Post-Post | |
| Distance (m) | 0.0001 | 0.0000 | 0.7266 | 0.0297 |
| VO2 max (l/min) | 0.0001 | 0.0002 | 0.7077 | 0.0310 |
| HRmax | 0.8774 | 0.0790 | 0.9037 | 0.4686 |
| VC (l) | 0.7071 | 0.2179 | 0.2438 | 0.5572 |
| FVC (l) | 0.0104 | 0.4078 | 0.9627 | 0.4080 |
| FVC (%) | 0.0022 | 0.1560 | 0.3172 | 0.0321 |
| FEV1 (%) | 0.0457 | 0.0147 | 0.3296 | 0.5938 |
| PEF (1/s) | 0.1206 | 0.5021 | 0.4158 | 0.1748 |
| PImax (kPa) | 0.0000 | 0.1738 | 0.7761 | 0.0026 |
| PImax (%) | 0.0001 | 0.0848 | 0.4897 | 0.0006 |
| PEmax (kPa) | 0.0001 | 0.3616 | 0.6923 | 0.0046 |
| PEmax (%) | 0.0001 | 0.4123 | 0.5976 | 0.0049 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mackała, K.; Kurzaj, M.; Okrzymowska, P.; Stodółka, J.; Coh, M.; Rożek-Piechura, K. The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players. Int. J. Environ. Res. Public Health 2020, 17, 234. https://doi.org/10.3390/ijerph17010234
Mackała K, Kurzaj M, Okrzymowska P, Stodółka J, Coh M, Rożek-Piechura K. The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players. International Journal of Environmental Research and Public Health. 2020; 17(1):234. https://doi.org/10.3390/ijerph17010234
Chicago/Turabian StyleMackała, Krzysztof, Monika Kurzaj, Paulina Okrzymowska, Jacek Stodółka, Milan Coh, and Krystyna Rożek-Piechura. 2020. "The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players" International Journal of Environmental Research and Public Health 17, no. 1: 234. https://doi.org/10.3390/ijerph17010234
APA StyleMackała, K., Kurzaj, M., Okrzymowska, P., Stodółka, J., Coh, M., & Rożek-Piechura, K. (2020). The Effect of Respiratory Muscle Training on the Pulmonary Function, Lung Ventilation, and Endurance Performance of Young Soccer Players. International Journal of Environmental Research and Public Health, 17(1), 234. https://doi.org/10.3390/ijerph17010234






