Distribution of the Indicator of the Appropriate Admission of Patients with Circulatory System Diseases to County Hospitals in Rural China: A Cross-Sectional Study
Abstract
1. Background
2. Methods
2.1. Setting and Participants
2.2. Sampling and Data Collection
2.3. Measurement
2.4. Medical Record Evaluation
2.5. Statistics Analysis
2.6. Research Ethics
3. Result
3.1. Characteristics of Patients Who were Appropriately Admitted to County Hospitals
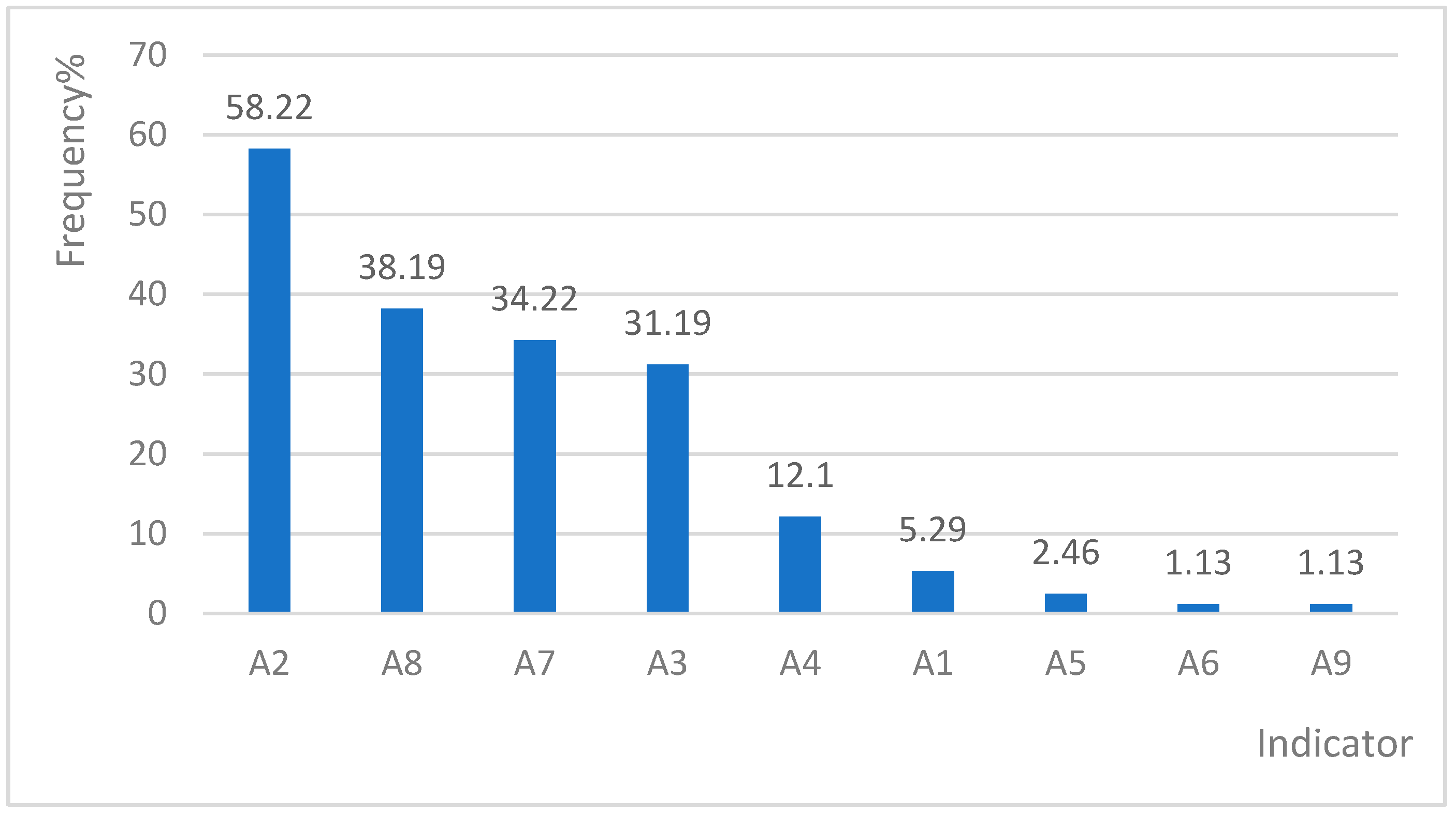
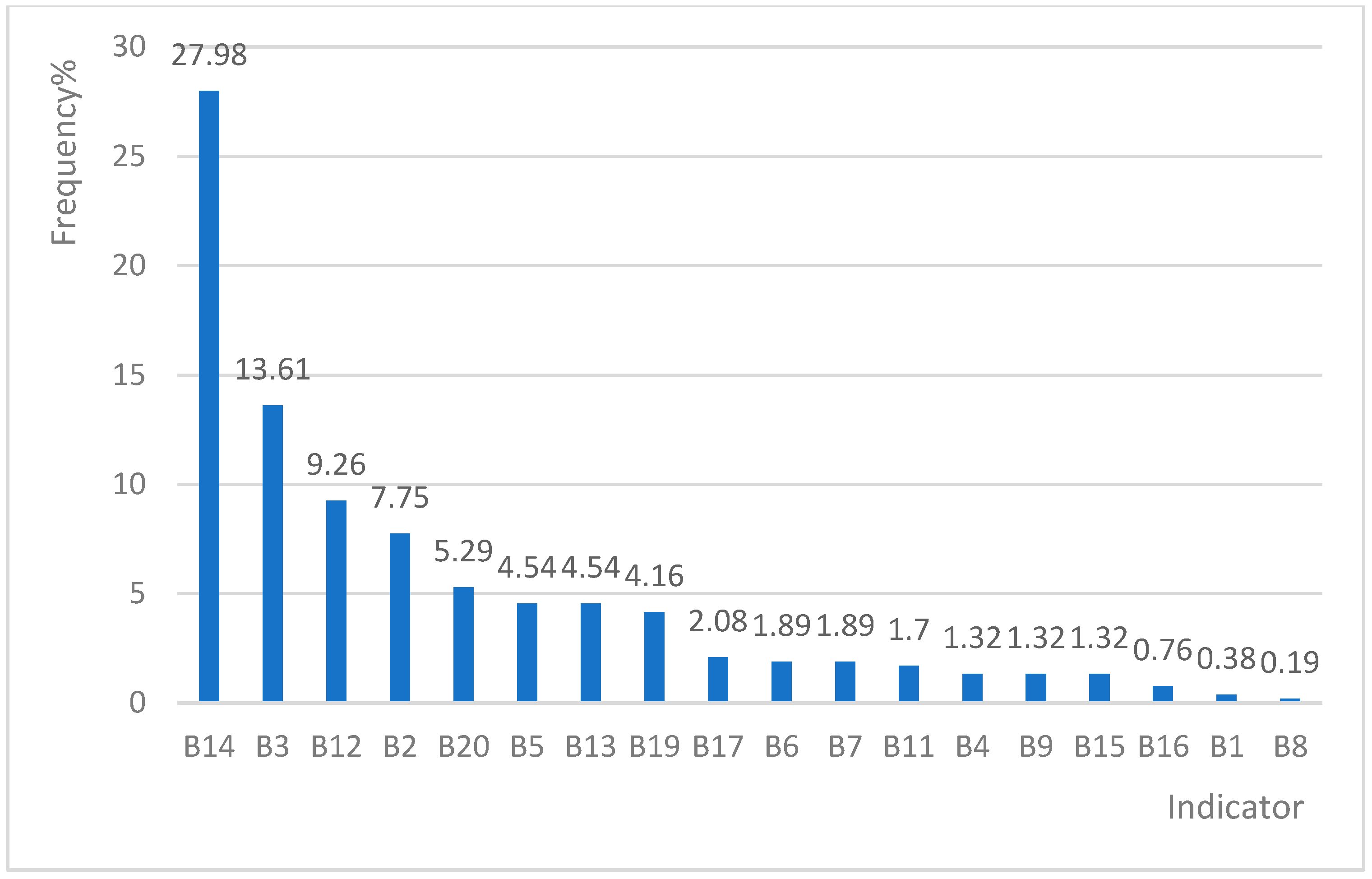
3.2. Total Positive Frequency of Each Indicator
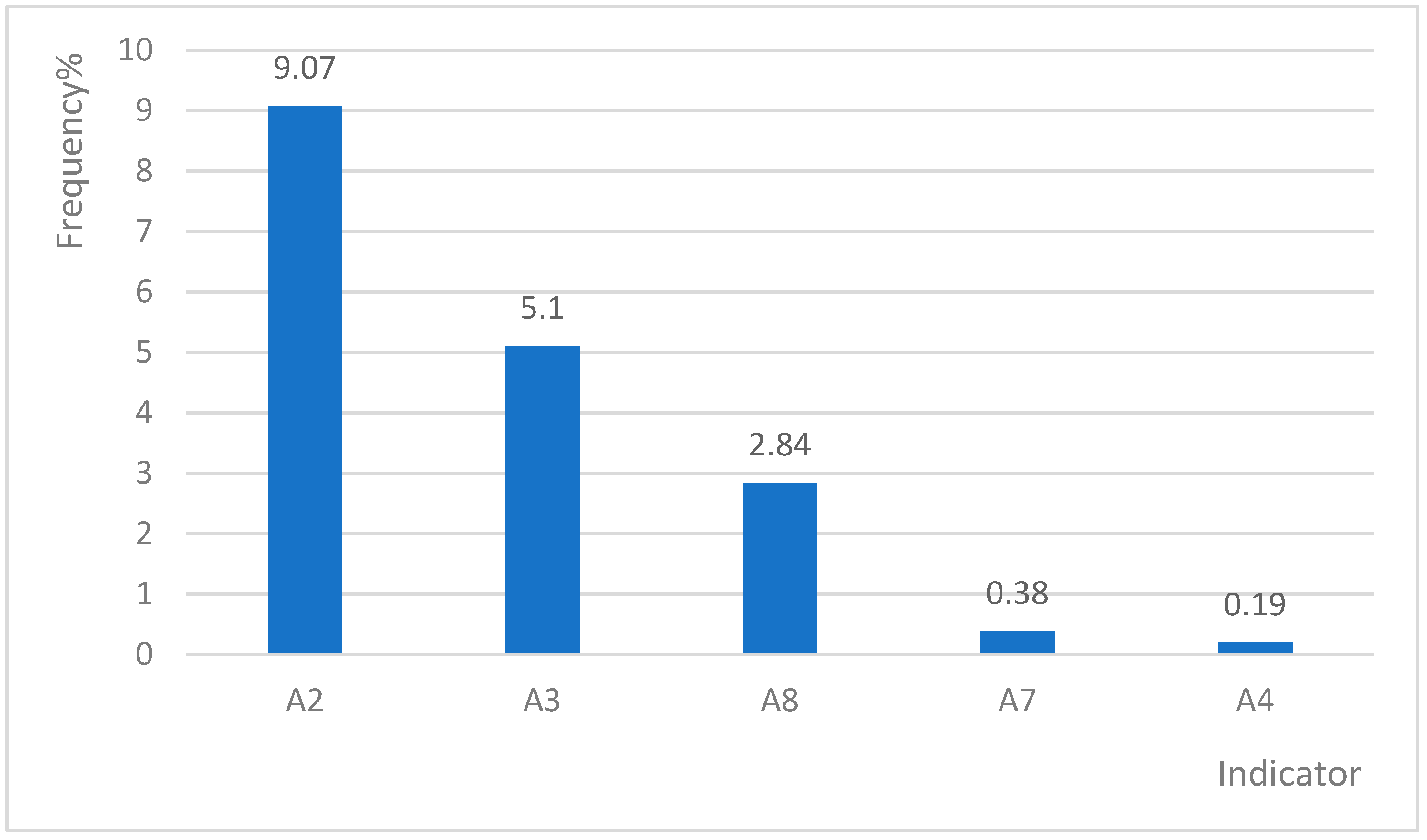
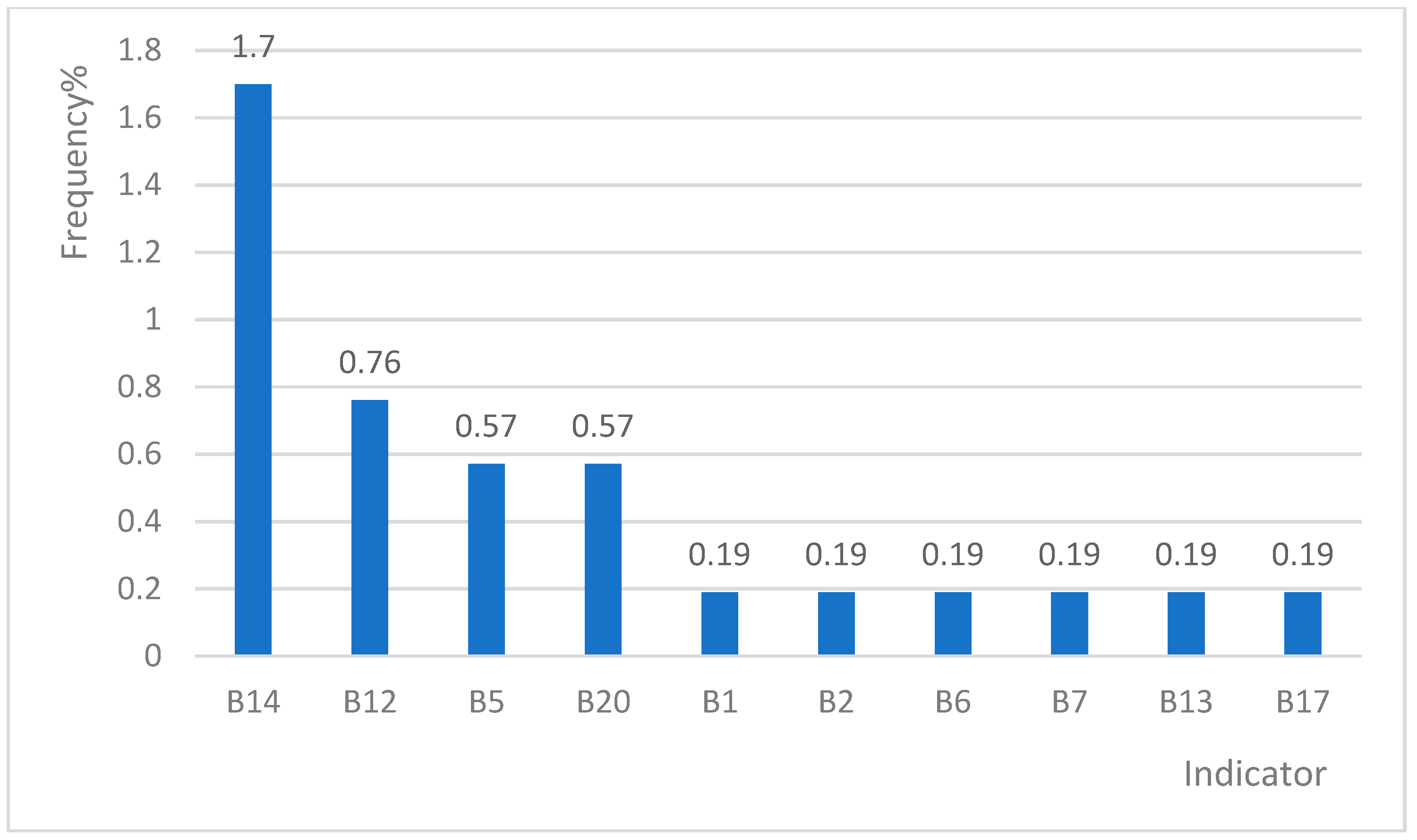
3.3. Positive Frequencies of Single or Multiple Indicators
3.4. Comparison of the Frequencies of Indicators A and B
3.5. Analysis of the Influencing Factors of Positive Indicators
4. Discussion
4.1. Inappropriate Admission Rates of Circulatory System Disease (CSD) Cases Vary Across Different Regions
4.2. Indicators with High-Positive Rates in CSD Cases
4.3. Difference between the High Rural Appropriateness Evaluation Protocol (RAEP) Positive Rate Index in this Study and the International AEP of CSDs
4.4. Indicator Characteristics of Patients Who Were Appropriately Hospitalised for CSDs
5. Conclusions
6. Limitation
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CSDs | Circulatory System Diseases; |
| NRCMS | New rural cooperative medical system; |
| AEP | Appropriateness Evaluation Protocol; |
| RAEP | Rural Appropriateness Evaluation Protocol. |
References
- National Health and Family Planning Commission. 2017 China Health and Family Planning Statistical Yearbook; China’s Health and Family Planning Statistical Yearbook; Peking Union Medical College Press: Bejing, China, 2017; ISBN 978-7-5679-0888-8.
- Statistics and Information Centre of the Ministry of Health. China Health Service Survey and Research: The Third National Health Service Survey and Analysis Report; Peking Union Medical College Press: Bejing, China, 2004.
- National Health and Family Planning Commission Statistical Information Centre. 2013 Fifth National Health Service Survey and Analysis Report; Peking Union Medical College Press: Bejing, China, 2015.
- Restuccia, J.; Shwartz, M.; Ash, A.; Payne, S. High Hospital Admission Rates And Inappropriate Care. Heal. Aff. 1996, 15, 156–163. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Y.; Zhang, X.; Zhang, L. Current level and determinants of inappropriate admissions to township hospitals under the new rural cooperative medical system in China: a cross-sectional study. BMC Heal. Serv. 2014, 14, 855. [Google Scholar] [CrossRef] [PubMed]
- Lavis, J.N.; Anderson, G.M. Appropriateness in health care delivery: definitions, measurement and policy implications. Can. Med Assoc. J. 1996, 154, 321–328. [Google Scholar]
- Payne, S.M. Identifying and managing inappropriate hospital utilization: a policy synthesis. Heal. Serv. 1987, 22, 709–769. [Google Scholar]
- Zhang, Y.; Zhang, L.; Li, H.; Chen, Y. Determinants of inappropriate admissions in county hospitals in rural china: a cross-sectional study. Int. J. Environ. Res. Public Health 2018, 15, 1050. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J. Inappropriate admissions: thoughts of patients and referring doctors. J. Soc. Med. 2001, 94, 628–631. [Google Scholar] [CrossRef]
- Peiró, S.; Meneu, R. Revisión de la utilización. Definición, concepto, métodos. Rev. Calidad. Asistencial. 1997, 12, 122–136. [Google Scholar]
- Kaplan, R.S.; Lave, L.B. Patient incentives and hospital insurance. Health Serv. Res. 1971, 6, 288–300. [Google Scholar]
- Price, S.D.; Holman, C.D.J.; Sanfilippo, F.M.; Emery, J.D. Are high-care nursing home residents at greater risk of unplanned hospital admission than other elderly patients when exposed to Beers potentially inappropriate medications? Geriatr. Gerontol. Int. 2014, 14, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Alarcon, R.D.; Walter-Ryan, W.G.; Shaw, L. Inappropriate Admissions to Psychiatric Wards. South. Med J. 1985, 78, 827–832. [Google Scholar] [CrossRef]
- Pozen, M.W.; D’Agostino, R.B.; Mitchell, J.B.; Rosenfeld, D.M.; Guglielmino, J.T.; Schwartz, M.L.; Teebagy, N.; Valentine, J.M.; Hood, W.B. Jr. The usefulness of a predictive instrument to reduce inappropriate admissions to the coronary care unit. Ann. Intern. Med. 1980, 92, 238–242. [Google Scholar] [CrossRef]
- Su, L.; Jiang, Q.; Zhou, H.; Zhang, Z. Study on the status of unreasonable hospitalisation of chronic non-communicable diseases in China. China Health Econ. 2016, 35, 70–73. [Google Scholar]
- Gertman, P.M.; Restuccia, J.D. The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med. Care 1981, 19, 855–871. [Google Scholar] [CrossRef] [PubMed]
- Ishoy, T.; Qvist, P.; Rasmussen, L.; Gjorup, T.; Rasmussen, J.H.; Christau, B.; Wiemann, O. Inappropriate admissions to medical departments. Appropriateness Evaluation Protocol. Ugeskr Laeger 2005, 167, 2057–2060. [Google Scholar]
- Panis, L.J.; Verheggen, F.W.; Pop, P. To stay or not to stay. The assessment of appropriate hospital stay: A Dutch report. Int. J. Qual. Health Care 2002, 14, 55–67. [Google Scholar] [CrossRef] [PubMed]
- Neumann, A.; Schultz-Coulon, H.J. Use of the appropriateness evaluation protocol in inpatient ENT practice. HNO 2001, 49, 12–20. [Google Scholar] [CrossRef]
- Tao, W.; Luo, C.; Ma, J. Consistency study of applicability evaluation methods for admission and hospitalisation in gynecology and neurology applications. J. Shanghai Jiaotong U. 2013, 33, 751. [Google Scholar]
- Pan, Q. Research on Mathematical Model of Multi-Scale Circulation System. Ph.D. Thesis, Zhejiang University, Hangzhou, China, 2013. [Google Scholar]
- Jurkovičová, J.; Štefániková, Z.; Sobotová, L.A.; Ševčíková, L.; Ághová, L. Cardiovascular disease risk factors in a sample group of 65+ year-old people in the Slovak Republic. Kardiologia 2009, 18, 47–62. [Google Scholar]
- Lin, B.S.; Wong, A.M.; Tseng, K.C. Community-based ECG monitoring system for patients with cardiovascular diseases. J. Med. Syst. 2016, 40, 80. [Google Scholar] [CrossRef]
- Gao, X.; Chen, Y.; Chu, Z.; Zhang, L. Characteristics and causes of excessive demand for inpatient services in new rural cooperatives. Chin. J. Hosp. Manag. 2015, 279–282. [Google Scholar]
- Qiu, J. Clinical medication experience of cardiovascular and cerebrovascular diseases. Chin. Community Dr. 2016, 32, 113–115. [Google Scholar]
- Guo, S.; Zhang, Y. Calculation error and correction method of patient fluid intake and withdrawal. Heilongjiang Nurs. J. 1998, 1, 5. [Google Scholar]
- Tavakoli, N.; Hosseini Kasnavieh, S.M.; Yasinzadeh, M.; Amini, M.; Mahmoudi Nejad, M. Evaluation of appropriate and inappropriate admission and hospitalisation days according to appropriateness evaluation protocol (AEP). Arch. Iran. Med. 2015, 18, 430–434. [Google Scholar]
- Zhu, Y. Common cardiovascular and cerebrovascular diseases and hypoxia. Family Med. 2013, 67. [Google Scholar]
- Johansen, H.; Thillaiampalam, S.; Nguyen, D.; Sambell, C. Diseases of the circulatory system—hospitalisation and mortality. Health Rep. 2005, 17, 49–53. [Google Scholar] [PubMed]
- Bosone, D.; Fogari, R.; Ramusino, M.C.; Ghiotto, N.; Guaschino, E.; Zoppi, A.; D’Angelo, A.; Costa, A. Ambulatory 24-h ECG monitoring and cardiovascular autonomic assessment for the screening of silent myocardial ischemia in elderly type 2 diabetic hypertensive patients. Heart Vessels 2017, 32, 507–513. [Google Scholar] [CrossRef]
- Du, Z.Q.; Wang, H.Y.; Wang, P. Application of Mannitol in Patients with Cerebrovascular Diseases. Chin. J. Cerebrovasc. Dis. 2008, 2, 475–480, 525. [Google Scholar]
- Chizyński, K. Coronary risk factors and mode of ischemic heart disease treatment in patients over 65 years of age. Przegl Lek 2003, 60, 451–455. [Google Scholar] [PubMed]
- Varon, J. Treatment of acute severe hypertension: current and newer agents. Drugs 2008, 68, 283–297. [Google Scholar] [CrossRef]
| Variable | All (Column %) | Appropriateness of Admission | p-Value | |
|---|---|---|---|---|
| Yes Number (Line %) | No Number (Line %) | |||
| All | 794 | 529 (66.6) | 265 (33.4) | |
| County | ||||
| Weiyuan | 215 (27.1) | 121 (56.3) | 94 (43.7) | 0.001 |
| Dingyuan | 193 (24.3) | 132 (68.4) | 61 (31.6) | |
| Huining | 219 (27.6) | 150 (68.5) | 69 (31.5) | |
| Yilong | 167 (21.0) | 126 (75.4) | 41 (24.6) | |
| Gender | ||||
| Male | 384 (48.4) | 257 (66.9) | 127 (33.1) | 0.764 |
| Female | 399 (50.3) | 263 (65.9) | 136 (34.1) | |
| Age, years | ||||
| Less than 25 | 9 (1.1) | 9 (100.0) | 0 (0.0) | 0.008 |
| 26–45 | 44 (5.5) | 28 (63.6) | 16 (36.4) | |
| 46–65 | 309 (38.9) | 186 (60.2) | 123 (39.8) | |
| More than 65 | 426 (53.7) | 302 (70.9) | 124 (29.1) | |
| Mean (SD) | 65.32 (12.867) | |||
| Disease category | ||||
| Cerebral infarction | 137 (17.3) | 85 (62.0) | 52 (38.0) | 0.255 |
| Coronary heart disease | 117 (14.7) | 79 (67.5) | 38 (32.5) | |
| hypertension | 50 (6.3) | 32 (64.0) | 18 (36.0) | |
| hypertension III | 53 (6.7) | 30 (56.6) | 23 (43.4) | |
| Other | 437 (55.0) | 303 (69.3) | 134 (30.7) | |
| Indicator | Total Positive | Single Positive | Multi Positive of 2 Indicators | Multi Positive of 3 Indicators | Multi Positive of 4 Indicators |
|---|---|---|---|---|---|
| A2 | 308 (58.22%) | 48 (9.07%) | 107 (20.23%) | 69 (13.04%) | 39 (7.37%) |
| A8 | 202 (38.19%) | 15 (2.84%) | 39 (7.37%) | 54 (10.21%) | 40 (7.56%) |
| A7 | 181 (34.22%) | 2 (0.38%) | 41 (7.75%) | 59 (11.15%) | 33 (6.24%) |
| A3 | 165 (31.19%) | 27 (5.10%) | 46 (8.70%) | 37 (6.99%) | 26 (4.91%) |
| B14 | 148 (27.98%) | 9 (1.70%) | 45 (8.51%) | 29 (5.48%) | 29 (5.48%) |
| Multi-positive of 2 Indicators | Multi-positive of 3 Indicators | Multi-positive of 4 Indicators | ||||||
|---|---|---|---|---|---|---|---|---|
| Indicator | Number of Case (n) | Proportion (%) | Indicator | Number of Case (n) | Proportion (%) | Indicator | Number of Case (n) | Proportion (%) |
| A2 + A7 | 33 | 6.24 | A2 + A7 + A8 | 18 | 3.40 | A2 + A7 + A8 + B14 | 9 | 1.70 |
| A2 + B14 | 28 | 5.29 | A3 + A4 + A8 | 8 | 1.51 | A3 + A4 + A8 + B3 | 6 | 1.13 |
| A2 + A8 | 16 | 3.02 | A2 + A8 + B14 | 6 | 1.13 | A2 + A7 + A8 + B13 | 3 | 0.57 |
| A8 + B14 | 9 | 1.70 | A2 + A3 + A7 | 5 | 0.95 | A3 + B2 + B3 + B14 | 3 | 0.57 |
| A3 + B3 | 8 | 1.51 | A2 + B3 + B14 | 5 | 0.95 | A1 + A2 + A3 + A7 | 2 | 0.38 |
| A2 + B12 | 7 | 1.32 | A7 + A8 + B14 | 5 | 0.95 | A2 + A3 + A7 + B14 | 2 | 0.38 |
| A7 + A8 | 7 | 1.32 | A3 + A4 + B3 | 4 | 0.76 | A3 + A7 + A8 + B14 | 2 | 0.38 |
| A2 + A3 | 6 | 1.13 | A2 + A7 + B12 | 3 | 0.57 | -- | -- | -- |
| A3 + A8 | 6 | 1.13 | A2 + A7 + B14 | 3 | 0.57 | -- | -- | -- |
| A3 + B14 | 6 | 1.13 | A2 + A7 + B20 | 3 | 0.57 | -- | -- | -- |
| A3 + A4 | 5 | 0.95 | A2 + B12 + B14 | 3 | 0.57 | -- | -- | -- |
| Others | 38 | 7.18 | Others | 54 | 10.21 | -- | -- | -- |
| Total | 169 | 31.95 | Total | 117 | 22.12 | Total | 63 | 11.91 |
| Indicator | B vs A | C vs A | C vs B | |||
|---|---|---|---|---|---|---|
| COR(95%CI) | AOR(95%CI) | COR(95%CI) | AOR(95%CI) | COR(95%CI) | AOR(95%CI) | |
| Age | 0.993(0.966 to 1.020) | 1.002(0.973 to 1.033) | 0.998(0.984 to 1.011) | 0.999(0.985 to 1.013) | 1.005(0.979 to 1.032) | 0.997(0.967 to 1.027) |
| Gender | ||||||
| Male | 0.442(0.207 to 0.944)* | 0.514(0.229 to 1.153) | 0.642(0.448 to 0.919)* | 0.612 (0.422 to 0.887)** | 1.450(0.686 to 3.068) | 1.190(0.536 to 2.645) |
| Female (Ref) | ||||||
| Year | 0.565(0.411 to 0.777)* | 0.642 (0.457 to 0.903)* | 0.904(0.769 to 1.062) | 0.904(0.758 to 1.079) | 1.600(1.171 to 2.186)** | 1.408 (1.009 to 1.965)* |
| Region | ||||||
| Weiyuan | 3.375(1.020 to 11.166)* | 2.646(0.768 to 9.122) | 1.009(0.600 to 1.698) | 0.979(0.566 to 1.695) | 0.299(0.0902 to 0.976)* | 0.370(0.109 to 1.253) |
| Dingyuan | 0.233(0.025 to 2.148) | 0.323(0.034 to 3.119) | 0.999(0.608 to 1.642) | 1.127(0.650 to 1.956) | 4.294(0.468 to 39.382) | 3.486(0.365 to 33.255) |
| Huining | 3.375(1.064 to 10.701)* | 3.455 (1.044 to 11.437)* | 0.869(0.531 to 1.421) | 1.027(0.610 to 1.730) | 0.257(0.082 to 0.809)* | 0.297 (0.091 to 0.968)* |
| Yilong (Ref) | ||||||
| Disease type | ||||||
| Cerebral infarction | 1.131(0.352 to 3.638) | 1.646 (0.479 to 5.656) | 1.642(0.975 to 2.767) | 1.601(0.922 to 2.779) | 1.452(0.468 to 4.501) | 0.973(0.296 to 3.193) |
| Coronary heart disease | 0.501(0.140 to 1.793) | 0.707 (0.185 to 2.696) | 0.565(0.338 to 0.942)* | 0.563 (0.327 to 0.968) * | 1.126(0.312 to 4.070) | 0.796(0.207 to 3.057) |
| hypertension | 1.379(0.363 to 5.229) | 0.823 (0.204 to 3.327) | 0.631(0.293 to 1.360) | 0.563(0.256 to 1.237) | 0.458(0.118 to 1.767) | 0.684(0.169 to 2.778) |
| hypertension III | 3.394(1.139 to 10.114)* | 2.260 (0.649 to 7.869) | 0.657(0.285 to 1.516) | 0.628(0.262 to 1.508) | 0.194(0.064 to 0.589)** | 0.278 (0.080 to 0.966)* |
| Other diseases (Ref) | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ye, Q.; Zhang, Y.; Gao, H.-x.; Chen, Y.-c.; Li, H.-m.; Zhang, H.; Hu, X.-m.; Lei, S.-h.; Jiang, D. Distribution of the Indicator of the Appropriate Admission of Patients with Circulatory System Diseases to County Hospitals in Rural China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 1621. https://doi.org/10.3390/ijerph16091621
Ye Q, Zhang Y, Gao H-x, Chen Y-c, Li H-m, Zhang H, Hu X-m, Lei S-h, Jiang D. Distribution of the Indicator of the Appropriate Admission of Patients with Circulatory System Diseases to County Hospitals in Rural China: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2019; 16(9):1621. https://doi.org/10.3390/ijerph16091621
Chicago/Turabian StyleYe, Qing, Yan Zhang, Hong-xia Gao, Ying-chun Chen, Hao-miao Li, Hui Zhang, Xiao-mei Hu, Shi-han Lei, and Di Jiang. 2019. "Distribution of the Indicator of the Appropriate Admission of Patients with Circulatory System Diseases to County Hospitals in Rural China: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 16, no. 9: 1621. https://doi.org/10.3390/ijerph16091621
APA StyleYe, Q., Zhang, Y., Gao, H.-x., Chen, Y.-c., Li, H.-m., Zhang, H., Hu, X.-m., Lei, S.-h., & Jiang, D. (2019). Distribution of the Indicator of the Appropriate Admission of Patients with Circulatory System Diseases to County Hospitals in Rural China: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 16(9), 1621. https://doi.org/10.3390/ijerph16091621





