Long-Acting Reversible Contraception Uptake and Associated Factors among Women of Reproductive Age in Rural Kenya
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Design
2.3. Study Population
2.4. Sampling Procedure and Sample Size
2.5. Ethical Clearance
2.6. Data Collection Procedures
2.7. Statistical Analysis
2.7.1. Quantitative Data
2.7.2. Qualitative Data
3. Results
3.1. Quantitative Data
3.1.1. Socio-Demographic and Reproductive Characteristics of Study Participants
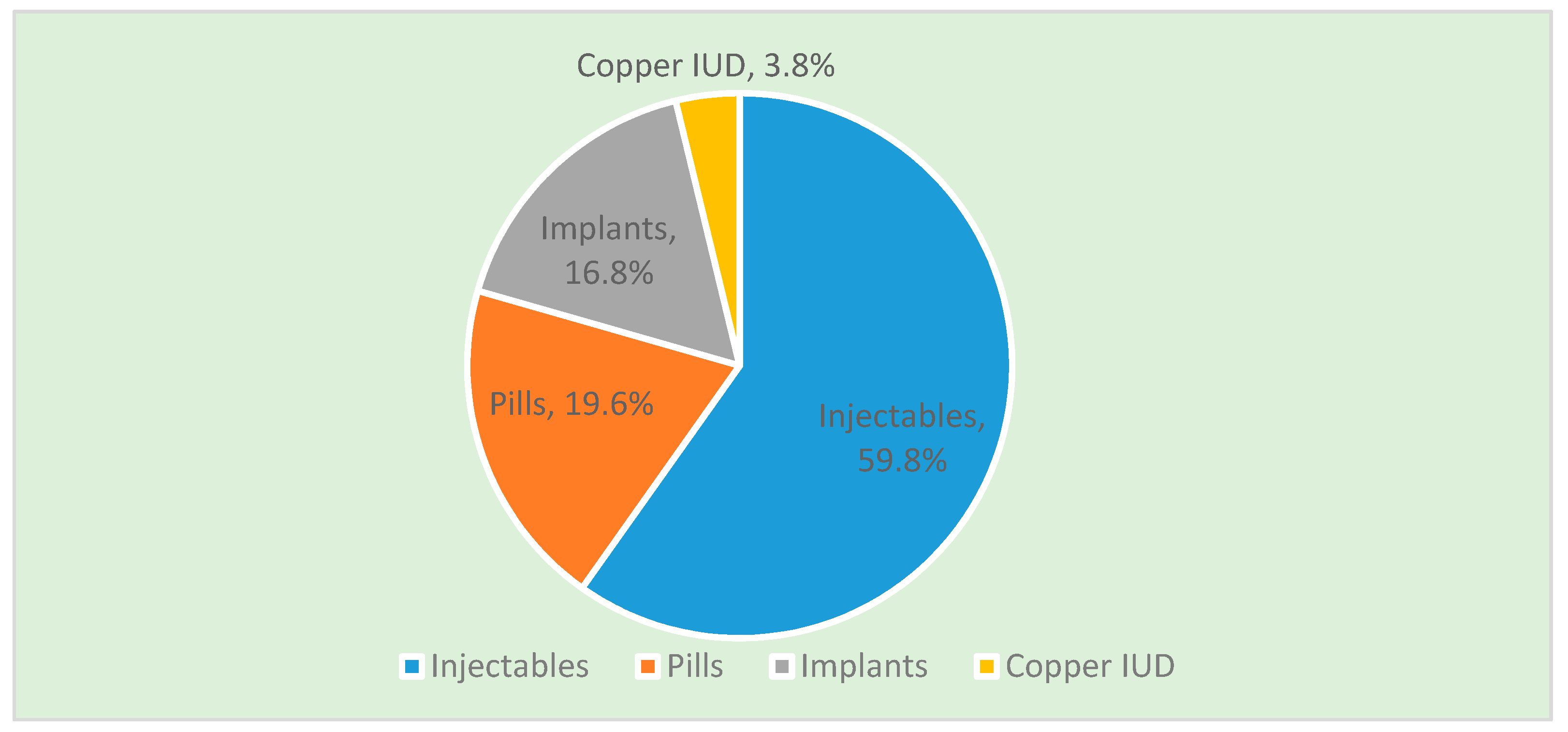
3.1.2. Contraceptive Method Mix among Women Initiating Use
3.1.3. Factors Associated with Uptake of LARC among Women of Reproductive Age
3.2. Qualitative Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Blumenthal, P.; Voedisch, A.; Gemzell-Danielsson, K. Strategies to prevent unintended pregnancy: Increasing use of long-acting reversible contraception. Hum. Reprod. Update 2011, 17, 121–137. [Google Scholar] [CrossRef] [PubMed]
- Trussell, J.; Guthrie, K. Choosing a contraceptive: Efficacy, safety, and personal considerations. In Contraceptive Technology, 19th revised ed.; Hatcher, R.A., Trussell, J., Nelson, A.L., Cates, W., Stewart, F.H., Kowal, D., Eds.; Ardent Media, Inc.: New York, NY, USA, 2007; pp. 19–47. [Google Scholar]
- Jacobstein, R.; Stanley, H. Contraceptive implants: Providing better choice to meet growing family planning demand. Glob. Health Sci. Pract. 2013, 1, 11–17. [Google Scholar] [CrossRef]
- Frost, J.J.; Darroch, J.E. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect. Sex. Reprod. Health 2008, 40, 94–104. [Google Scholar] [CrossRef]
- Kenya National Bureau of Statistics; Ministry of Health/Kenya; National AIDS Control Council/Kenya; Kenya Medical Research Institute; National Council for Population Development/Kenya. Kenya Demographic and Health Survey 2014; ICF Macro: Rockville, MD, USA, 2015. [Google Scholar]
- Performance Monitoring and Accountability 2020 (PMA2020) Project, International Centre for Reproductive Health—Kenya. 2017. PMA2017/Kenya-Round 5 & 6: Family Planning Key indicator Brief—Kakamega County. Baltimore MD: PMA2020, Bill and Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins Bloomberg School of Public Health. 2017. Available online: https://www.pma2020.org/sites/default/files/KER6_SOI_2017.11.27.pdf (accessed on 11 March 2019).
- Kavanaugh, M.L.; Jerman, J.; Hubacher, D.; Kost, K.; Finer, L.B. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet. Gynecol. 2011, 117, 1349–1357. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.; Bobak, M. Women’s autonomy, education and contraception use in Pakistan: A national study. Reprod. Health 2005, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Curtis, S.L.; Neitzel, K. Contraceptive Knowledge Use and Sources; Macro International: Calverton, MD, USA, 1996. [Google Scholar]
- Yeatman, S.E.; Trinitapoli, J. Beyond denomination: The relationship between religion and family planning in rural Malawi. Demographic Res. 2008, 19, 1851. [Google Scholar] [CrossRef]
- Melka, A.S.; Tekelab, T.; Wirtu, D. Determinants of long acting and permanent contraceptive methods utilization among married women of reproductive age groups in western Ethiopia: A cross-sectional study. Pan Afr. Med. J. 2015, 21, 246. [Google Scholar] [CrossRef]
- Anguzu, R.; Sempeera, H.; Sekandi, J.N. High parity predicts use of long-acting reversible contraceptives in the extended postpartum period among women in rural Uganda. Contracept. Reprod. Med. 2018, 3, 6. [Google Scholar] [CrossRef]
- Dempsey, A.R.; Billingsley, C.C.; Savage, A.H.; Korte, J.E. Predictors of long-acting reversible contraception use among unmarried young adults. Am. J. Obstet. Gynecol. 2012, 206, 526.e1–526.e5. [Google Scholar] [CrossRef]
- Eeckhaut, M.C.; Sweeney, M.M.; Gipson, J.D. Who Is Using Long-Acting Reversible Contraceptive Methods? Findings from Nine Low-Fertility Countries. Perspect. Sex. Reprod. Health 2014, 46, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, P.; Akintomide, H.; Brima, N.; Copas, A.; D’Souza, R. Determinants of long-acting reversible contraceptive (LARC) use by adolescent girls and young women. Eur. J. Contracept. Reprod. Health Care 2012, 17, 298–306. [Google Scholar] [CrossRef]
- Track20: The S-Curve: Putting mCPR Growth into Context October 2017. Available online: http://www.track20.org/pages/data_analysis/in_depth/mCPR_growth/s_curve.php (accessed on 20 February 2019).
- Israel, G.D. Determining Sample Size; University of Florida IFAS extension: Gainesville, FL, USA, 2009. [Google Scholar]
- Jacobstein, R.; Curtis, C.; Spieler, J.; Radloff, S. Meeting the need for modern contraception: Effective solutions to a pressing global challenge. Int. J. Gynecol. Obstet. 2013, 121 (Suppl. 1), S9–S15. [Google Scholar] [CrossRef] [PubMed]
- Varney, S.J.; Guest, J.F. Relative cost effectiveness of Depo-Provera®, Implanon®, and Mirena® in reversible long-term hormonal contraception in the UK. Pharmacoeconomics 2004, 22, 1141–1151. [Google Scholar] [CrossRef] [PubMed]
- Jacobstein, R. Liftoff: The blossoming of contraceptive implant use in Africa. Glob. Health Sci. Pract. 2018, 6, 17–39. [Google Scholar] [CrossRef]
- Zenebe, C.B.; Adefris, M.; Yenit, M.K.; Gelaw, Y.A. Factors associated with utilization of long-acting and permanent contraceptive methods among women who have decided not to have more children in Gondar city. BMC Women‘s Health 2017, 17, 75. [Google Scholar] [CrossRef]
- Tibaijuka, L.; Odongo, R.; Welikhe, E.; Mukisa, W.; Kugonza, L.; Busingye, I.; Nabukalu, P.; Ngonzi, J.; Asiimwe, S.B.; Bajunirwe, F. Factors influencing use of long-acting versus short-acting contraceptive methods among reproductive-age women in a resource-limited setting. BMC Women‘s Health 2017, 17, 25. [Google Scholar] [CrossRef]
- Finer, L.B.; Jerman, J.; Kavanaugh, M.L. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fert. Steril. 2012, 98, 893–897. [Google Scholar] [CrossRef]
- Dassah, E.T.; Odoi, A.T.; Owusu-Asubonteng, G. Prevalence and factors predictive of long-acting reversible contraceptive use in a tertiary hospital in urban Ghana. Eur. J. Contracept. Reprod. Health Care 2013, 18, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.J.; Siwatu, M.; Robinson, A.K. “My religion picked my birth control”: The influence of religion on contraceptive use. J. Relig. Health 2014, 53, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Bulto, G.A.; Zewdie, T.A.; Beyen, T.K. Demand for long acting and permanent contraceptive methods and associated factors among married women of reproductive age group in Debre Markos Town, North West Ethiopia. BMC Women‘s Health 2014, 14, 1. [Google Scholar] [CrossRef]
- Agha, S. Intentions to use contraceptives in Pakistan: Implications for behavior change campaigns. BMC Public Health 2010, 10, 1. [Google Scholar] [CrossRef]
- WHO. Facts on Induced Abortion Worldwide; Department of Reproductive Health and Research WHO Document Production Services: Geneva, Switzerland, 2011. [Google Scholar]
- Luchowski, A.T.; Anderson, B.L.; Power, M.L.; Raglan, G.B.; Espey, E.; Schulkin, J. Obstetrician-Gynecologists and contraception: Long-acting reversible contraception practices and education. Contraception 2014, 89, 578–583. [Google Scholar] [CrossRef]
- Harper, C.C.; Henderson, J.T.; Raine, T.R.; Goodman, S.; Darney, P.D.; Thompson, K.M.; Dehlendorf, C.; Speidel, J.J. Evidence-based IUD practice: Family physicians and obstetrician-gynecologists. Fam. Med. 2012, 44, 637. [Google Scholar]
- Harper, C.C.; Blum, M.; De Bocanegra, H.T.; Darney, P.D.; Speidel, J.J.; Policar, M.; Drey, E.A. Challenges in translating evidence to practice: The provision of intrauterine contraception. Obstet. Gynecol. 2008, 111, 1359–1369. [Google Scholar] [CrossRef]
- World Health Organization. WHO Recommendations: Optimizing Health Worker Roles to Improve Access to Key Maternal and Newborn Health Interventions Through Task Shifting; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Jacobstein, R. Lessons from the recent rise in use of female sterilization in Malawi. Stud. Fam. Plan. 2013, 44, 85–95. [Google Scholar] [CrossRef]
- Anguzu, R.; Tweheyo, R.; Sekandi, J.N.; Zalwango, V.; Muhumuza, C.; Tusiime, S.; Serwadda, D. Knowledge and attitudes towards use of long acting reversible contraceptives among women of reproductive age in Lubaga division, Kampala district, Uganda. BMC Res. Notes 2014, 7, 153. [Google Scholar] [CrossRef]
- Belohlav, K.; Karra, M. Household Decisionmaking and Contraceptive Use in Zambia; Population Reference Bureau: Washington, DC, USA, 2013. [Google Scholar]
| Variable (n = 423) | Category | n | % |
|---|---|---|---|
| Age (years) | 15–24 | 143 | 34 |
| 25–34 | 187 | 44 | |
| 35+ | 93 | 22 | |
| Marital Status | Married | 306 | 72 |
| Not Married | 117 | 28 | |
| Education Level | None | 11 | 3 |
| Primary | 179 | 42 | |
| Secondary | 170 | 40 | |
| Tertiary | 63 | 15 | |
| Religion | None | 5 | 1 |
| Muslim | 40 | 9 | |
| Catholic | 121 | 29 | |
| Protestant | 257 | 61 | |
| Residence | Urban | 92 | 22 |
| Rural | 331 | 78 | |
| Occupation | Not Working | 168 | 40 |
| Casual/Business | 100 | 24 | |
| Farming | 126 | 30 | |
| Paid Employment | 29 | 7 | |
| Distance to facility M (SD) | 2.5 (±2.3) km | ||
| Ever given birth | Yes | 392 | 93 |
| No | 31 | 7 | |
| Sexual debut age (years) | ≤19 | 292 | 69 |
| ≥20 | 131 | 31 | |
| Parity | 0 | 32 | 8 |
| 1 | 109 | 26 | |
| 2–3 | 179 | 42 | |
| 4+ | 103 | 24 | |
| Desired Number of Children | 1–2 | 118 | 28 |
| 3–4 | 220 | 52 | |
| 5+ | 85 | 20 | |
| Fertility Intention | No more children | 113 | 27 |
| Wants in 2 years | 56 | 13 | |
| Wants after 2 years | 116 | 27 | |
| Wants but unsure of timing | 41 | 10 | |
| Undecided | 97 | 23 | |
| Age at first birth M (SD) | 19.8 (±3) | ||
| Variable | Category | LARC Uptake (n = 87) | Crude Odds Ratio (95% CI) | p Value | Adjusted Odds Ratio (95% CI) | p Value | |
|---|---|---|---|---|---|---|---|
| n | % | ||||||
| Age (years) | 15–24 | 17 | 11.9 | Ref | |||
| 25–34 | 43 | 23 | 2.21 (1.20–4.07) | 0.011 | 0.84–3.15 | 0.148 | |
| 35+ | 27 | 29.1 | 3.03 (1.54–5.96) | 0.001 | 0.88–4.20 | 0.103 | |
| Education Level | None/Primary | 27 | 14.2 | Ref | |||
| Secondary | 41 | 24.1 | 1.92 (1.12–3.29) | 0.018 | 0.98–3.16 | 0.061 | |
| Tertiary | 19 | 30.2 | 2.61 (1.33–5.12) | 0.005 | 2.58 (1.10–6.03) | 0.029 | |
| Religion | Catholic | 34 | 28.1 | Ref | Ref | ||
| None | 1 | 20 | 0.64 (0.07–5.93) | 0.694 | 0.52 (0.04–6.29) | 0.605 | |
| Muslim | 10 | 25 | 0.85 (0.38–1.93) | 0.703 | 0.73 (0.29–1.79) | 0.489 | |
| Protestant | 42 | 16.3 | 0.51 (0.3–0.84) | 0.008 | 0.42 (0.24–0.73) | 0.002 | |
| Occupation | Not Working | 24 | 14.3 | Ref | Ref | ||
| Casual/Business | 20 | 20 | 1.53 (0.78–2.88) | 0.224 | 0.96 (0.45–2.05) | 0.917 | |
| Farming | 34 | 27 | 2.22 (1.24–3.98) | 0.008 | 1.62 (0.84–3.16) | 0.152 | |
| Paid Employment | 9 | 31 | 2.71 (1.10–6.62) | 0.032 | 1.29 (0.43–3.89) | 0.651 | |
| Fertility Intention | Wants in 2 years | 6 | 11.1 | Ref | Ref | ||
| No more children | 35 | 31.8 | 3.73 (1.46–9.55) | 0.006 | 3.77 (1.37–10.42) | 0.001 | |
| Wants after 2 years | 26 | 22.4 | 2.31 (0.89–6.00) | 0.085 | 2.94 (1.07–8.08) | 0.037 | |
| Wants but unsure of timing | 6 | 14.6 | 1.37 (0.41–4.61) | 0.614 | 1.81 (0.51–6.37) | 0.357 | |
| Undecided | 12 | 12.4 | 1.13 (0.40–3.20) | 0.231 | 1.12 (0.37–3.25) | 0.864 | |
| Age at first birth | ≤19 | 24 | 14.0 | Ref | |||
| ≥20 | 63 | 25.1 | 2.07 (1.23–3.47) | 0.006 | 1.66 (0.91–3.02) | 0.098 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ontiri, S.; Ndirangu, G.; Kabue, M.; Biesma, R.; Stekelenburg, J.; Ouma, C. Long-Acting Reversible Contraception Uptake and Associated Factors among Women of Reproductive Age in Rural Kenya. Int. J. Environ. Res. Public Health 2019, 16, 1543. https://doi.org/10.3390/ijerph16091543
Ontiri S, Ndirangu G, Kabue M, Biesma R, Stekelenburg J, Ouma C. Long-Acting Reversible Contraception Uptake and Associated Factors among Women of Reproductive Age in Rural Kenya. International Journal of Environmental Research and Public Health. 2019; 16(9):1543. https://doi.org/10.3390/ijerph16091543
Chicago/Turabian StyleOntiri, Susan, Gathari Ndirangu, Mark Kabue, Regien Biesma, Jelle Stekelenburg, and Collins Ouma. 2019. "Long-Acting Reversible Contraception Uptake and Associated Factors among Women of Reproductive Age in Rural Kenya" International Journal of Environmental Research and Public Health 16, no. 9: 1543. https://doi.org/10.3390/ijerph16091543
APA StyleOntiri, S., Ndirangu, G., Kabue, M., Biesma, R., Stekelenburg, J., & Ouma, C. (2019). Long-Acting Reversible Contraception Uptake and Associated Factors among Women of Reproductive Age in Rural Kenya. International Journal of Environmental Research and Public Health, 16(9), 1543. https://doi.org/10.3390/ijerph16091543





