Association Between Surrounding Greenness and Schizophrenia: A Taiwanese Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
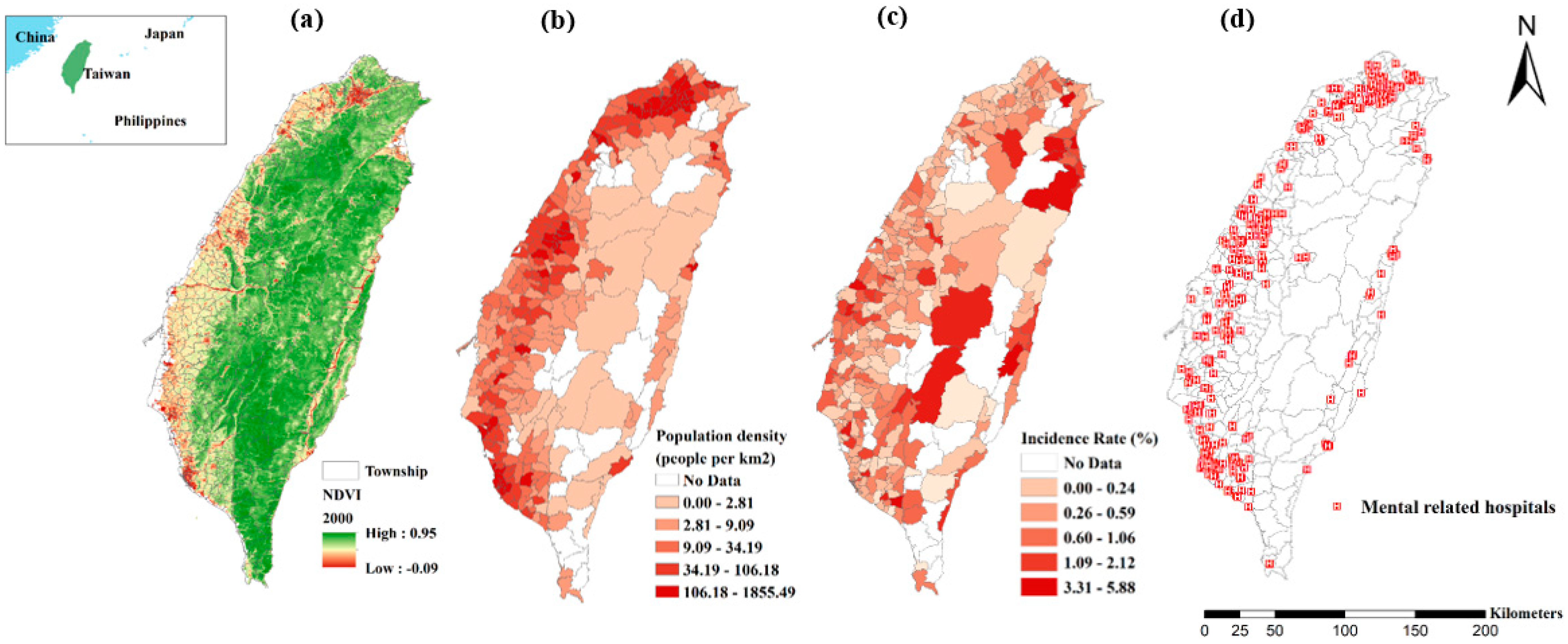
2.1. Study Area
2.2. Databases
2.2.1. Remotely Sensing Greenness Data
2.2.2. LHID
2.2.3. Meteorological Information
2.2.4. Mental-Related Information
2.3. Statistical Analysis
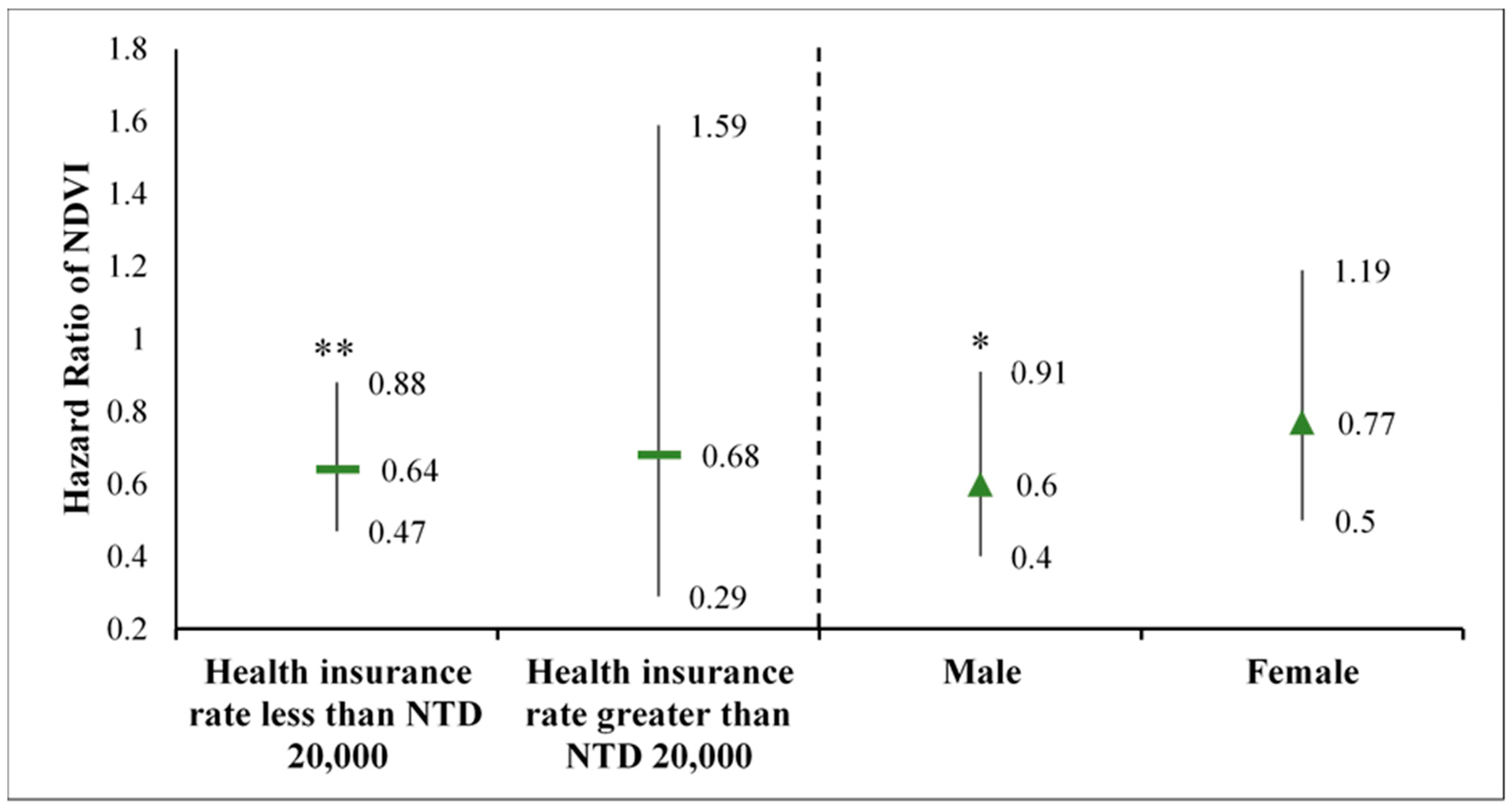
2.4. Sensitivity Test and Stratified Analysis
3. Results
3.1. Descriptive Statistics
3.2. Model Analysis and Sensitivity Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mental Disorders. Available online: http://www.who.int/mental_health/management/en/ (accessed on 9 March 2018).
- National Institue of Mental Health. Mental Illness. Available online: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml (accessed on 1 November 2017).
- World Health Organization. Depression and other Common Mental Disorders: Global Health Estimates; WHO/MSD/MER/2017.2; World Health Organization: Geneva, Switzerland, 2017; p. 24. [Google Scholar]
- National Institue of Mental Health. Schizophrenia. Available online: https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml (accessed on 1 May 2018).
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Robertson, L. Lastest questions & answers on schizophrenia. In Mental Health Matters; Health Service: Gauteng, South Africa, 2017; Volume 4, pp. 41–44. [Google Scholar]
- National Institute of Mental Health. Schizophrenia. Available online: https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml (accessed on 1 February 2016).
- Morozov, P.V. Mental health and urbanization: A Russian perspective. Curr. Opin. Psychiatry 2018, 31, 272–275. [Google Scholar] [CrossRef]
- Okkels, N.; Kristiansen, C.B.; Munk-Jørgensen, P.; Sartorius, N. Urban mental health: Challenges and perspectives. Curr. Opin. Psychiatry 2018, 31, 258–264. [Google Scholar] [CrossRef]
- United Nations Department of Economic and Social Affairs. 2018 Revision of World Urbanization Prospects. Available online: https://www.un.org/development/desa/publications/2018-revision-of-world-urbanization-prospects.html (accessed on 16 May 2018).
- James, P.; Banay, R.F.; Hart, J.E.; Laden, F. A review of the health benefits of greenness. Curr. Epidemiol. Rep. 2015, 2, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Fong, K.C.; Hart, J.E.; James, P. A review of epidemiologic studies on greenness and health: Updated literature through 2017. Curr. Environ. Health Rep. 2018, 5, 77–87. [Google Scholar] [CrossRef] [PubMed]
- United States Environmental Protection Agency. Using Trees and Vegetation to Reduce Heat Islands. Available online: https://www.epa.gov/heat-islands/using-trees-and-vegetation-reduce-heat-islands (accessed on 12 August 2016).
- Jacobs, S.J.; Gallant, A.J.E.; Tapper, N.J.; Li, D. Use of cool roofs and vegetation to mitigate urban heat and improve human thermal stress in Melbourne, Australia. J. Appl. Meteorol. Clim. 2018, 57, 1747–1764. [Google Scholar] [CrossRef]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Forns, J.; Plasència, A.; Nieuwenhuijsen, M.J. Mental health benefits of long-term exposure to residential green and blue spaces: A systematic review. Int. J. Environ. Res. Public Health 2015, 12, 4354–4379. [Google Scholar] [CrossRef] [PubMed]
- Ministry Of the Interior. Monthly Bulletin of Interior Statistics. Available online: https://www.moi.gov.tw/files/site_stuff/321/1/month/month_en.html#4%20Land%20Adm. (accessed on 1 July 2018).
- Clough, R. Taiwan under Nationalist rule, 1949–1982. The Cambridge History of China 1991, 15, 813–874. [Google Scholar]
- Fu, T.S.-T.; Lee, C.-S.; Gunnell, D.; Lee, W.-C.; Cheng, A.T.-A. Changing trends in the prevalence of common mental disorders in Taiwan: A 20-year repeated cross-sectional survey. Lancet 2013, 381, 235–241. [Google Scholar] [CrossRef]
- National Health Insurance Administration Ministry of Health and Welfare. National Health Insurance Annual Report 2017–2018. Available online: https://www.nhi.gov.tw/Resource/webdata/13767_1_National%20Health%20Insurance%20in%20Taiwan%202016-2017(bilingual).pdf (accessed on 1 February 2019).
- National Health Research Institutes. National Health Insurance Research Database. Available online: http://nhird.nhri.org.tw/en/index.htm (accessed on 30 June 2016).
- National Health Insurance Administration Ministry of Health and Welfare. How Premiums Are Calculated. Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=B9C9C690524F2543&topn=46FA76EB55BC2CB8 (accessed on 1 January 2018).
- Cox, D.R. Regression models and life-tables. In Breakthroughs in Statistics; Kotz, S., Johnson, N.L., Eds.; Springer: New York, NY, USA, 1992; pp. 527–541. [Google Scholar]
- Cox, D.R. Analysis of Survival Data; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Sung, T.-I.; Chen, M.-J.; Su, H.-J. A positive relationship between ambient temperature and bipolar disorder identified using a national cohort of psychiatric inpatients. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Chien, I.C.; Chou, Y.J.; Lin, C.H.; Bih, S.H.; Chou, P.; Chang, H.J. Prevalence and incidence of schizophrenia among national health insurance enrollees in Taiwan, 1996–2001. Psychiatry Clin. Neurosci. 2004, 58, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Brandl, E.J.; Lett, T.A.; Bakanidze, G.; Heinz, A.; Bermpohl, F.; Schouler-Ocak, M. Weather conditions influence the number of psychiatric emergency room patients. Int. J. Biometeorol. 2018, 62, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Padhy, S.K.; Sarkar, S.; Panigrahi, M.; Paul, S. Mental health effects of climate change. Indian J. Occup. Environ. Med. 2015, 19, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Browning, M.; Lee, K. Within what distance does “greenness” best predict physical health? A systematic review of articles with GIS buffer analyses across the lifespan. Int. J. Environ. Res. Public Health 2017, 14, 675. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, H. Demographic and environmental factors associated with mental health: A cross-sectional study. Int. J. Environ. Res. Public Health 2017, 14, 431. [Google Scholar] [CrossRef]
- Agerbo, E.; Sullivan, P.F.; Vilhjalmsson, B.J.; Pedersen, C.B.; Mors, O.; Børglum, A.D.; Hougaard, D.M.; Hollegaard, M.V.; Meier, S.; Mattheisen, M. Polygenic risk score, parental socioeconomic status, family history of psychiatric disorders, and the risk for schizophrenia: A Danish population-based study and meta-analysis. JAMA Psychiatry 2015, 72, 635–641. [Google Scholar] [CrossRef]
- Engemann, K.; Pedersen, C.B.; Arge, L.; Tsirogiannis, C.; Mortensen, P.B.; Svenning, J.-C. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proc. Natl. Acad. Sci. USA 2019, 116, 5188–5193. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; Van Dillen, S.M.; Verheij, R.A.; Groenewegen, P.P. Social contacts as a possible mechanism behind the relation between green space and health. Health Place 2009, 15, 586–595. [Google Scholar]
- National Statistics, R.O.C. Family Income Expenditure-Annual. Available online: https://web.archive.org/web/20151024182701/http://statdb.dgbas.gov.tw/pxweb/Dialog/varval.asp?ma=FF0001A1A&ti=Major%20Figures%20of%20Family%20Income%20and%20Expenditure-Annual&path=../PXfileE/HouseholdFinances/&lang=1&strList=L (accessed on 5 September 2017).
- Ministry of Health and Welfare. Statistics of Medical Care Institution’s Status & Hospital’s Utilization 2017. Available online: https://www.mohw.gov.tw/cp-4113-43597-2.html (accessed on 27 August 2018).
- Brown, S.; Perrino, T.; Lombard, J.; Wang, K.; Toro, M.; Rundek, T.; Gutierrez, C.; Dong, C.; Plater-Zyberk, E.; Nardi, M. Health disparities in the relationship of neighborhood greenness to mental health outcomes in 249,405 US Medicare beneficiaries. Int. J. Environ. Res. Public Health 2018, 15, 430. [Google Scholar] [CrossRef] [PubMed]
- Piccininni, C.; Michaelson, V.; Janssen, I.; Pickett, W. Outdoor play and nature connectedness as potential correlates of internalized mental health symptoms among Canadian adolescents. Prev Med. 2018, 112, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9–17. [Google Scholar] [CrossRef]
- Cho, K.S.; Lim, Y.-R.; Lee, K.; Lee, J.; Lee, J.H.; Lee, I.-S. Terpenes from forests and human health. Toxicol. Res. 2017, 33, 97–106. [Google Scholar] [CrossRef]
- College of the Environment, U.o.W. Mental Health & Function. Available online: https://depts.washington.edu/hhwb/Thm_Mental.html (accessed on 17 August 2018).
- Wu, C.-D.; McNeely, E.; Cedeño-Laurent, J.G.; Pan, W.-C.; Adamkiewicz, G.; Dominici, F.; Lung, S.-C.C.; Su, H.-J.; Spengler, J.D. Linking student performance in Massachusetts elementary schools with the “greenness” of school surroundings using remote sensing. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- Li, Q.; Kobayashi, M.; Wakayama, Y.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Shimizu, T.; Kawada, T.; Park, B. Effect of phytoncide from trees on human natural killer cell function. Int. J. Immunopathol Pharmacol. 2009, 22, 951–959. [Google Scholar] [CrossRef]
- Zhou, C.; Yan, L.; Yu, L.; Wei, H.; Guan, H.; Shang, C.; Chen, F.; Bao, J. Effect of Short-term Forest Bathing in Urban Parks on Perceived Anxiety of Young-adults: A Pilot Study in Guiyang, Southwest China. Chin. Geogr. Sci. 2019, 29, 139–150. [Google Scholar] [CrossRef]
- Hansen, M.M.; Jones, R.; Tocchini, K. Shinrin-yoku (forest bathing) and nature therapy: A state-of-the-art review. Int. J. Environ. Res. Public Health 2017, 14, 851. [Google Scholar] [CrossRef]
- Erbino, C.; Toccolini, A.; Vagge, I.; Ferrario, P.S. Guidelines for the design of a healing garden for the rehabilitation of psychiatric patients. J. Agric. Eng. 2015, 46, 43–51. [Google Scholar] [CrossRef]
- Cascio, M.T.; Cella, M.; Preti, A.; Meneghelli, A.; Cocchi, A. Gender and duration of untreated psychosis: A systematic review and meta-analysis. Early Interv. Psychiatry 2012, 6, 115–127. [Google Scholar] [CrossRef]
- Directorate-General of Budget, A.a.S., Executive Yuan, R.O.C. (Taiwan). Unemployment Ratio. Available online: http://www.dgbas.gov.tw/point.asp?index=3 (accessed on November 2018).
- Wang, D.; Ma, J.; Tan, L.; Chen, Y.; Li, X.; Tian, X.; Zhou, X.; Liu, X. Epidemiology of severe mental illness in Hunan province in central China during 2014–2015: A multistage cross-sectional study. PLoS ONE 2017, 12, e0188312. [Google Scholar] [CrossRef]
- Thompson, R.; Hornigold, R.; Page, L.; Waite, T. Associations between high ambient temperatures and heat waves with mental health outcomes: A systematic review. Public Health 2018, 161, 171–191. [Google Scholar] [CrossRef]
- Miller, C.L. Evidence for phenotypic plasticity in response to photic cues and the connection with genes of risk in schizophrenia. Front. Behav. Neurosci. 2013, 7, 82. [Google Scholar] [CrossRef]
- Lencz, T.; Guha, S.; Liu, C.; Rosenfeld, J.; Mukherjee, S.; DeRosse, P.; John, M.; Cheng, L.; Zhang, C.; Badner, J.A. Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat. Commun. 2013, 4, 273. [Google Scholar] [CrossRef]
| Greenness Exposure | <1st (N = 4006) | 1st–4th (N = 34,627) | 5th–9th (N = 41,591) | 10th–24th (N = 144,006) | 25th–49th (N = 210,814) | 50th–74th (N = 212,808) | 75th–89th (N = 135,532) | 90th–94th (N = 42,666) | 95th–99th (N = 34,789) | >99th (N = 8645) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p * | |
| NDVI | 0.22 (0.05) | 0.27 (0.01) | 0.30 (0.01) | 0.33 (0.02) | 0.39 (0.02) | 0.47 (0.02) | 0.53 (0.02) | 0.58 (0.01) | 0.64 (0.02) | 0.74 (0.02) | <0.001 |
| Health insurance rate | 12,812.28 (15,286.60) | 13,153.26 (15,363.66) | 13,128.03 (15,929.97) | 13,912.55 (16,607.39) | 12,400.93 (15,081.04) | 12,836.53 (14,831.04) | 12,728.42 (14,284.15) | 12,348.53 (13,373.57) | 12,686.02 (12,681.59) | 12,535.24 (12,000.73) | <0.001 |
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | p * | |
| Sex | |||||||||||
| Male | 2127 (53.1) | 16,964 (48.99) | 20,767 (49.93) | 69,309 (48.13) | 104,891 (49.76) | 108,603 (51.03) | 69,190 (51.05) | 22,138 (51.89) | 18,376 (52.82) | 4649 (53.78) | <0.001 |
| Female | 1879 (46.9) | 17,663 (51.01) | 20,824 (50.07) | 74,697 (51.87) | 105,923 (50.24) | 104,205 (48.97) | 66,342 (48.95) | 20,528 (48.11) | 16,413 (47.18) | 3996 (46.22) | -- |
| Age (years) | |||||||||||
| 0–15 | 160 (3.99) | 1895 (5.47) | 2389 (5.74) | 8993 (6.24) | 16,054 (7.62) | 15,825 (7.44) | 10,000 (7.38) | 3099 (7.26) | 2073 (5.96) | 471 (5.45) | <0.001 |
| 15–30 | 637 (15.90) | 7629 (22.03) | 8085 (19.44) | 32,601 (22.64) | 50,691 (24.05) | 50,386 (23.68) | 30,907 (22.80) | 9702 (22.74) | 7351 (21.13) | 1770 (20.47) | -- |
| 30 + | 3209 (80.1) | 25,103 (72.50) | 31,117 (74.82) | 102,412 (71.12) | 144,069 (68.34) | 146,597 (68.89) | 94,625 (69.82) | 29,865 (70.00) | 25,365 (72.91) | 6404 (74.08) | -- |
| Health insurance rate | |||||||||||
| NTD 0–20,000 | 2102 (52.47) | 17,716 (51.16) | 22,103 (53.14) | 74,952 (52.05) | 113,003 (53.60) | 107,866 (50.69) | 66,872 (49.34) | 20,587 (48.25) | 15,524 (44.62) | 3724 (43.08) | <0.001 |
| NTD 20,000 + | 1904 (47.53) | 16,911 (48.84) | 19,488 (46.86) | 69,054 (47.95) | 97,811 (46.40) | 104,942 (49.31) | 68,660 (50.66) | 22,079 (51.75) | 19,265 (55.38) | 4921 (56.92) | -- |
| Psychological status | |||||||||||
| Incidence cases of schizophrenia | 50 (1.25) | 174 (0.50) | 337 (0.81) | 721 (0.50) | 1211 (0.57) | 1209 (0.57) | 858 (0.63) | 236 (0.55) | 218 (0.63) | 55 (0.64) | <0.001 |
| Variable | HR (95% C.I.) | p-Value |
|---|---|---|
| NDVI | ||
| <1st (0.26) | 1.00 | |
| 1st (0.26)–4th | 0.44 (0.32, 0.61) | <0.001 |
| 5th (0.29)–9th | 0.69 (0.51, 0.93) | 0.01 |
| 10th (0.31)–24th | 0.45 (0.34, 0.60) | <0.001 |
| 25th (0.35)–49th | 0.47 (0.35, 0.62) | <0.001 |
| 50th (0.43)–74th | 0.49 (0.37, 0.65) | <0.001 |
| 75th (0.50)–89th | 0.49 (0.37, 0.65) | <0.001 |
| 90th (0.56)–94th | 0.41 (0.30, 0.56) | <0.001 |
| 95th (0.60)–99th | 0.41 (0.30, 0.55) | <0.001 |
| ≥99th (0.69) | 0.37 (0.25, 0.55) | <0.001 |
| Age (years) | ||
| 0–15 | 1 | |
| 15–30 | 3.90 (3.25, 4.67) | <0.001 |
| >30 | 2.71 (2.27, 3.24) | <0.001 |
| Sex | ||
| Female | 1 | |
| Male | 1.03 (0.98, 1.09) | 0.29 |
| Health insurance rate (NTD) | ||
| ≤20,000 | 1 | |
| >20,000 | 0.77 (0.70, 0.85) | <0.001 |
| Classification of the insured | ||
| Category 1 | 1 | |
| Category 2 | 1.14 (1.05, 1.24) | <0.01 |
| Category 3 | 1.10 (1.00, 1.21) | 0.05 |
| Category 4 | 1.28 (0.78, 2.10) | 0.32 |
| Category 5 | 6.40 (5.47, 7.49) | <0.001 |
| Category 6 | 2.42 (2.24, 2.61) | <0.001 |
| Temperature (°C) | 0.90 (0.88, 0.92) | <0.001 |
| Relative humidity (%) | 0.24 (0.18, 0.31) | <0.001 |
| Precipitation (mm) | 1.08 (1.06, 1.09) | <0.001 |
| Model | No. of Participant (Case) | HR (95% C.I.) | p-Value |
|---|---|---|---|
| NDVI as a continuous variable | |||
| NDVI from 1000 m buffers | 869,249 (5065) | 0.96 (0.70, 1.31) | 0.79 |
| NDVI from 1250 m buffers | 869,484 (5069) | 0.81 (0.60, 1.11) | 0.19 |
| NDVI from 1500 m buffers | 869,484 (5069) | 0.73 (0.54, 0.99) | 0.04 |
| NDVI from 1750 m buffers | 869,484 (5069) | 0.69 (0.51, 0.93) | 0.02 |
| NDVI from 2000 m buffers | 869,484 (5069) | 0.67 (0.50, 0.91) | 0.01 |
| NDVI from 2000 m buffers with addition of PM10 | 869,484 (5069) | 0.68 (0.51, 0.92) | 0.01 |
| Subgroup analysis | |||
| Taipei City | 111,642 (690) | 0.24 (0.04, 1.35) | 0.11 |
| Kaohsiung City | 60,989 (365) | 0.21 (0.03, 1.64) | 0.14 |
| Taipei and Kaohsiung City | 172,631 (1055) | 0.22 (0.06, 0.81) | 0.02 |
| Restricted to participants in Taipei metropolitan 1 area | 257,302 (1389) | 0.15 (0.06, 0.37) | <0.001 |
| Restricted to participants in Taipei metropolitan 1 and Kaohsiung metropolitan 2 area | 363,575 (2020) | 0.46 (0.25, 0.85) | 0.01 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, H.-T.; Wu, C.-D.; Pan, W.-C.; Lung, S.-C.C.; Su, H.-J. Association Between Surrounding Greenness and Schizophrenia: A Taiwanese Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 1415. https://doi.org/10.3390/ijerph16081415
Chang H-T, Wu C-D, Pan W-C, Lung S-CC, Su H-J. Association Between Surrounding Greenness and Schizophrenia: A Taiwanese Cohort Study. International Journal of Environmental Research and Public Health. 2019; 16(8):1415. https://doi.org/10.3390/ijerph16081415
Chicago/Turabian StyleChang, Hao-Ting, Chih-Da Wu, Wen-Chi Pan, Shih-Chun Candice Lung, and Huey-Jen Su. 2019. "Association Between Surrounding Greenness and Schizophrenia: A Taiwanese Cohort Study" International Journal of Environmental Research and Public Health 16, no. 8: 1415. https://doi.org/10.3390/ijerph16081415
APA StyleChang, H.-T., Wu, C.-D., Pan, W.-C., Lung, S.-C. C., & Su, H.-J. (2019). Association Between Surrounding Greenness and Schizophrenia: A Taiwanese Cohort Study. International Journal of Environmental Research and Public Health, 16(8), 1415. https://doi.org/10.3390/ijerph16081415








