Association between Chronic Pain and Physical Frailty in Community-Dwelling Older Adults
Abstract
1. Introduction
2. Materials and Methods
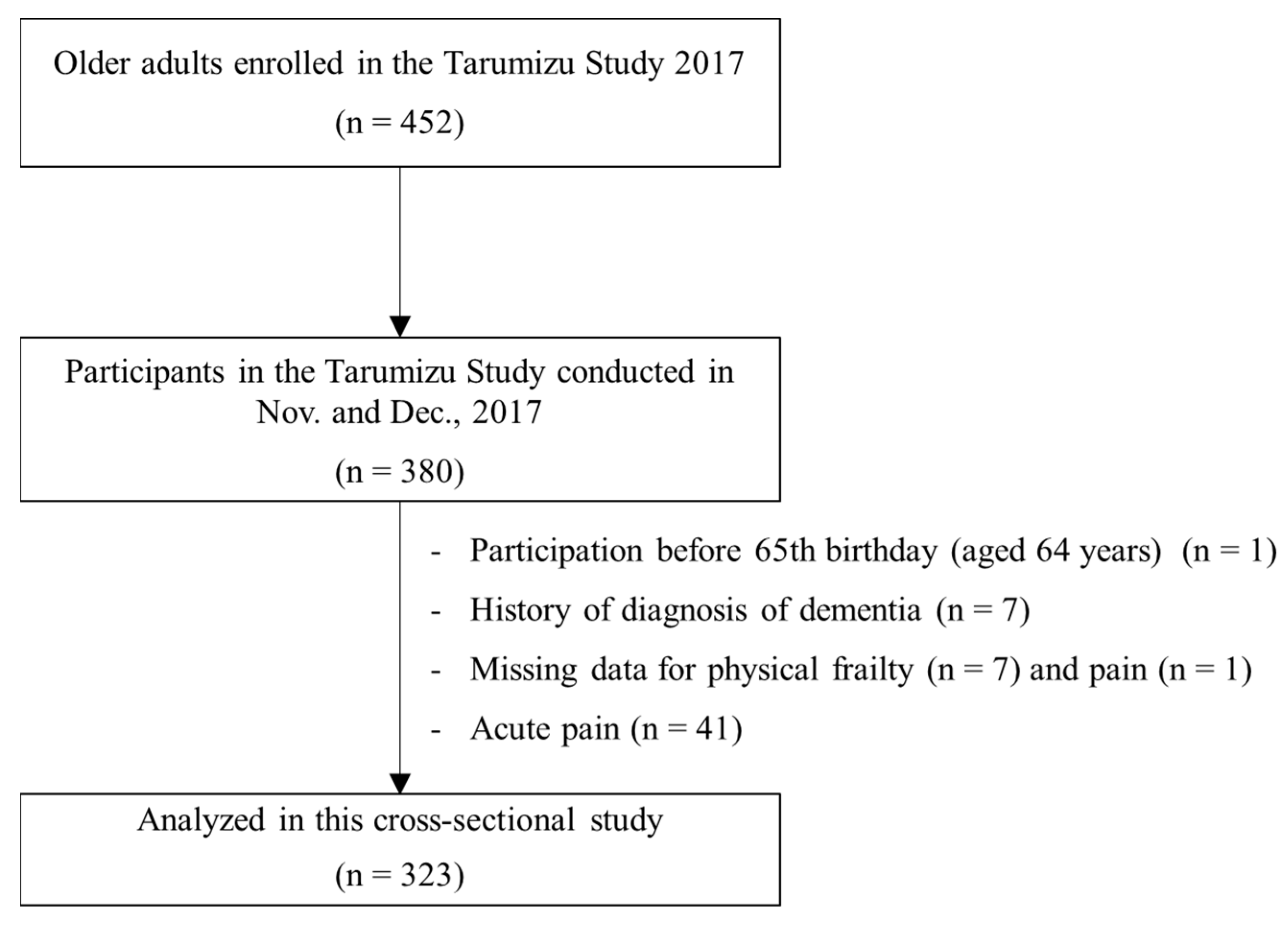
2.1. Participants
2.2. Physical Frailty
2.3. Chronic Pain
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Subsection Characteristics of Participants
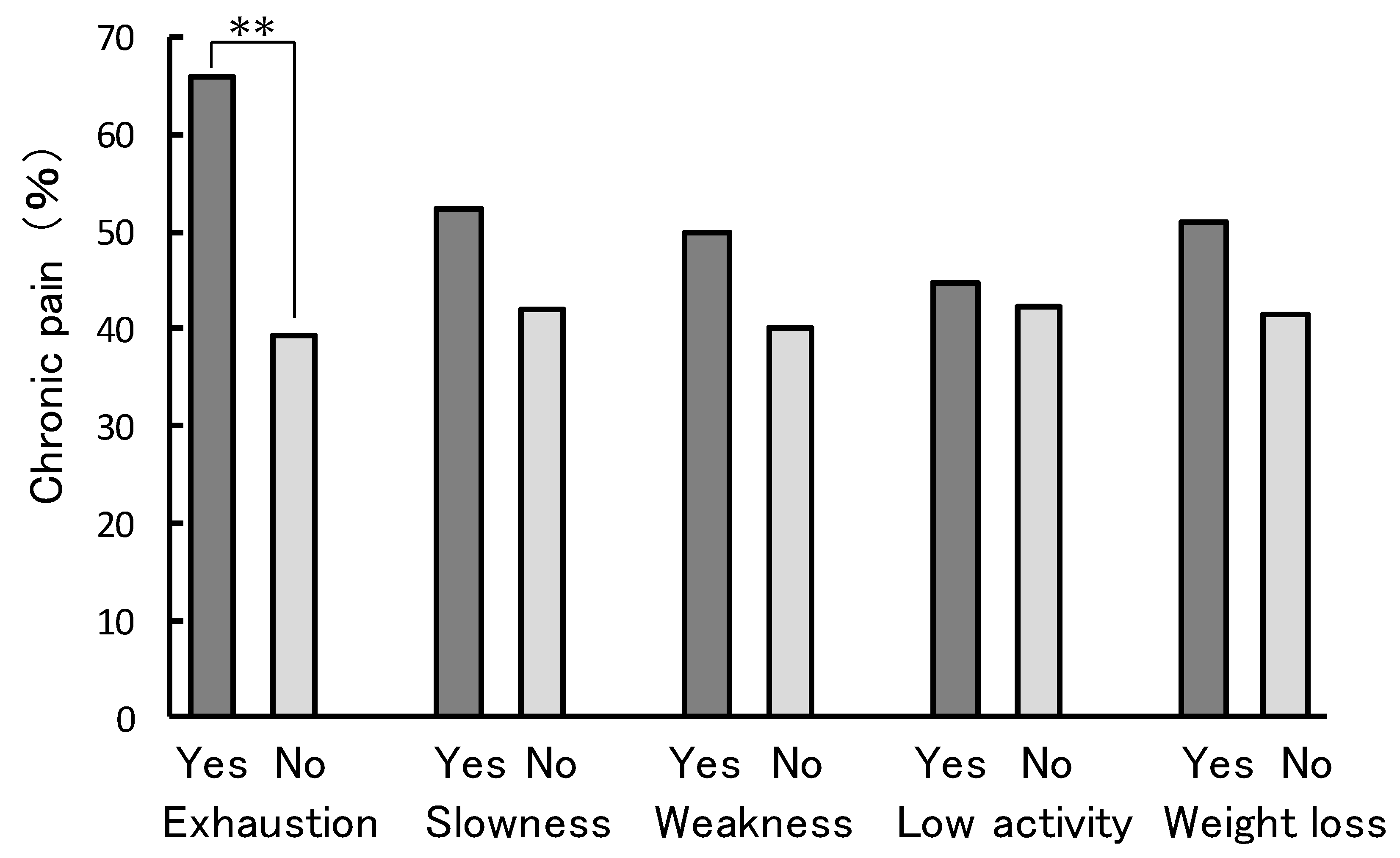
3.2. Associations of Prevalence of Chronic Pain and Physical Frailty
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fried, L.P. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Biol. Sci. Med. Sci. 2001, 56, 146–156. [Google Scholar] [CrossRef]
- Mitnitski, A.; Collerton, J.; Martin-Ruiz, C.; Jagger, C.; von Zglinicki, T.; Rockwood, K.; Kirkwood, T.B.L. Age-related frailty and its association with biological markers of ageing. BMC Med. 2015, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Schols, J.M.G.A.; Gobbens, R.J.J.; van Assen, M.A.L.M.; Luijkx, K.G.; Wijnen-Sponselee, M.T. Determinants of Frailty. J. Am. Med. Dir. Assoc. 2010, 11, 356–364. [Google Scholar]
- Bernabei, R.; Marzetti, E.; Albaina, O.; Junius-Walker, U.; Wiese, B.; Soleymani, D.; Onder, G. The essence of frailty: A systematic review and qualitative synthesis on frailty concepts and definitions. Eur. J. Intern. Med. 2018, 56, 3–10. [Google Scholar]
- Tom, S.E.; Adachi, J.D.; Anderson, F.A.; Boonen, S.; Chapurlat, R.D.; Compston, J.E.; Cooper, C.; Gehlbach, S.H.; Greenspan, S.L.; Hooven, F.H.; et al. Frailty and fracture, disability, and falls: A multiple country study from the global longitudinal study of osteoporosis in women. J. Am. Geriatr. Soc. 2013, 61, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Garre-Olmo, J.; Calvó-Perxas, L.; López-Pousa, S.; De Gracia Blanco, M.; Vilalta-Franch, J. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age Ageing 2013, 42, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G.; Iliffe, S.; Jivraj, S.; Walters, K. Association between frailty and quality of life among community-dwelling older people: A systematic review and meta-analysis. J. Epidemiol. Community Health 2016, 70, 716–721. [Google Scholar] [CrossRef]
- Vermeiren, S.; Vella-Azzopardi, R.; Beckwée, D.; Habbig, A.K.; Scafoglieri, A.; Jansen, B.; Bautmans, I.; Bautmans, I.; Verté, D.; Beyer, I.; et al. Frailty and the Prediction of Negative Health Outcomes: A Meta-Analysis. J. Am. Med. Dir. Assoc. 2016, 17, 1163.e1–1163.e17. [Google Scholar] [CrossRef] [PubMed]
- Peleg, R.; Press, Y.; Freud, T.; Liberman, O.; Keren, A. Chronic pain and geriatric syndromes in community-dwelling patients aged ≥65 years. J. Pain Res. 2018, 11, 1171–1180. [Google Scholar]
- Nakamura, M.; Nishiwaki, Y.; Ushida, T.; Toyama, Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan. J. Orthop. Sci. 2011, 16, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, M.; Yamazaki, S.; Kimura, M.; Nakano, K.; Yasumura, S. Community-based exercise program reduces chronic knee pain in elderly Japanese women at high risk of requiring long-term care: A non-randomized controlled trial. Geriatr. Gerontol. Int. 2013, 13, 167–174. [Google Scholar] [CrossRef]
- Eggermont, L.H.P.; Penninx, B.W.J.H.; Jones, R.N.; Leveille, S.G. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: The mobilize Boston study. J. Am. Geriatr. Soc. 2012, 60, 230–237. [Google Scholar] [CrossRef]
- Buchman, A.S.; Shah, R.C.; Leurgans, S.E.; Boyle, P.A.; Wilson, R.S.; Bennett, D.A. Musculoskeletal pain and incident disability in community-dwelling older adults. Arthritis Care Res. 2010, 62, 1287–1293. [Google Scholar] [CrossRef]
- Park, J.; Hughes, A.K. Nonpharmacological approaches to the management of chronic pain in community-dwelling older adults: A review of empirical evidence. J. Am. Geriatr. Soc. 2012, 60, 555–568. [Google Scholar] [CrossRef]
- Lihavainen, K.; Sipilä, S.; Rantanen, T.; Sihvonen, S.; Sulkava, R.; Hartikainen, S. Contribution of musculoskeletal pain to postural balance in community-dwelling people aged 75 years and older. J. Gerontol. Ser. Biol. Sci. Med. Sci. 2010, 65A, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Landi, F.; Gambassi, G.; Liperoti, R.; Soldato, M.; Catananti, C.; Finne-Soveri, H.; Katona, C.; Carpenter, I.; Bernabei, R. Association between pain and depression among older adults in Europe: Results from the Aged in Home Care (AdHOC) project: A cross-sectional Study. J. Clin. Psych. 2005, 66, 982–988. [Google Scholar] [CrossRef]
- Eggermont, L.H.P.; Leveille, S.G.; Shi, L.; Kiely, D.K.; Shmerling, R.H.; Jones, R.N.; Guralnik, J.M.; Bean, J.F. Pain characteristics associated with the onset of disability in older adults: The maintenance of balance, independent living, intellect, and zest in the elderly boston study. J. Am. Geriatr. Soc. 2014, 62, 1007–1016. [Google Scholar] [CrossRef]
- Plooij, B.; Scherder, E.J.A.; Eggermont, L.H.P. Physical inactivity in aging and dementia: A review of its relationship to pain. J. Clin. Nurs. 2012, 21, 3002–3008. [Google Scholar] [CrossRef]
- McGreevy, K.; Bottros, M.M.; Raja, S.N. Preventing chronic pain following acute pain: Risk factors, preventive strategies, and their efficacy. Eur. J. Pain Suppl. 2011, 5, 365–376. [Google Scholar] [CrossRef]
- Makizako, H.; Kubozono, T.; Kiyama, R.; Takenaka, T.; Kuwahata, S.; Tabira, T.; Kanoya, T.; Horinouchi, K.; Shimada, H.; Ohishi, M. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr. Gerontol. Int. 2019, 19, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Fukutomi, E.; Okumiya, K.; Wada, T.; Sakamoto, R.; Ishimoto, Y.; Kimura, Y.; Chen, W.L.; Imai, H.; Kasahara, Y.; Fujisawa, M.; et al. Relationships between each category of 25-item frailty risk assessment (Kihon Checklist) and newly certified older adults under Long-Term Care Insurance: A 24-month follow-up study in a rural community in Japan. Geriatr. Gerontol. Int. 2015, 15, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Salpakoski, A.; Portegijs, E.; Kallinen, M.; Sihvonen, S.; Kiviranta, I.; Alen, M.; Rantanen, T.; Sipil, S. Physical inactivity and pain in older men and women with hip fracture history. Gerontology 2010, 57, 19–27. [Google Scholar] [CrossRef]
- Wade, K.F.; Lee, D.M.; Mcbeth, J.; Ravindrarajah, R.; Gielen, E.; Pye, S.R.; Vanderschueren, D.; Pendleton, N.; Finn, J.D.; Bartfai, G.; et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing 2016, 45, 268–274. [Google Scholar] [CrossRef]
- Shimada, H.; Makizako, H.; Doi, T.; Yoshida, D.; Tsutsumimoto, K.; Anan, Y.; Uemura, K.; Ito, T.; Lee, S.; Park, H.; et al. Combined Prevalence of Frailty and Mild Cognitive Impairment in a Population ofElderly Japanese People. J. Am. Med. Dir. Assoc. 2013, 14, 518–524. [Google Scholar] [CrossRef]
- Makizako, H.; Tsutsumimoto, K.; Nakakubo, S.; Hotta, R.; Makino, K.; Shimada, H.; Doi, T.; Lee, S. Social Frailty Leads to the Development of Physical Frailty among Physically Non-Frail Adults: A Four-Year Follow-Up Longitudinal Cohort Study. Int. J. Environ. Res. Pub. Health 2018, 15, 490. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Suzuki, T. Impact of physical frailty on disability in community-dwelling older adults: A prospective cohort study. BMJ Open 2015, 5, 1–9. [Google Scholar] [CrossRef]
- Hirase, T.; Kataoka, H.; Inokuchi, S.; Nakano, J.; Sakamoto, J.; Okita, M. Factors associated with chronic musculoskeletal pain in Japanese community-dwelling older adults. Medicine 2017, 96, e7069. [Google Scholar] [CrossRef]
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef] [PubMed]
- Knutson, G.A. Incidence of foot rotation, pelvic crest unleveling, and supine leg length alignment asymmetry and their relationship to self-reported back pain. J. Manipul. Physiol. Ther. 2002, 25, 110E. [Google Scholar] [CrossRef]
- Hirase, T.; Kataoka, H.; Inokuchi, S.; Nakano, J.; Sakamoto, J.; Okita, M. Effects of exercise training combined with increased physical activity to prevent chronic pain in community-dwelling older adults: A preliminary randomized controlled trial. Pain Res. Manag. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hunt, I.M.; Silman, A.J.; Benjamin, S.; McBeth, J.; Macfarlane, G.J. The prevalence and associated features of chronic widespread pain in the community using the “Manchester” definition of chronic widespread pain. Rheumatology 1999, 38, 275–279. [Google Scholar] [CrossRef]
- Yesavage, J.A. Geriatric Depression Scale. Psychopharmacol. Bull. 1988, 24, 709–711. [Google Scholar]
- Inoue, S.; Kobayashi, F.; Nishihara, M.; Arai, Y.-C.P.; Ikemoto, T.; Kawai, T.; Inoue, M.; Hasegawa, T.; Ushida, T. Chronic Pain in the Japanese Community—Prevalence, Characteristics and Impact on Quality of Life. PLoS ONE 2015, 10, e0129262. [Google Scholar] [CrossRef]
- Zhu, K.; Devine, A.; Dick, I.M.; Prince, R.L. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine 2007, 32, 2012–2018. [Google Scholar] [CrossRef]
- Isanejad, M.; Mursu, J.; Sirola, J.; Kröger, H.; Rikkonen, T.; Tuppurainen, M.; Erkkilä, A.T. Dietary protein intake is associated with better physical function and muscle strength among elderly women. Br. J. Nutr. 2016, 115, 1281–1291. [Google Scholar] [CrossRef]
- Oliveira, M.R.; Fogaça, K.C.; Leandro-Merhi, V.A. Nutritional status and functional capacity of hospitalized elderly. Nutr. J. 2009, 8, 54. [Google Scholar] [CrossRef]
- Frontera, W.R.; Ochala, J. Skeletal Muscle: A Brief Review of Structure and Function. Calcif. Tiss. Int. 2015, 96, 183–195. [Google Scholar] [CrossRef]
| Variable | Total | Non-Frailty | Pre-Frailty | Frailty | p * |
|---|---|---|---|---|---|
| (n = 323) | (n = 152) | (n = 152) | (n = 19) | ||
| Chronic pain, n (%) | 138 (42.7) | 52 (34.2) | 76 (50.0) | 10 (52.6) | 0.014 |
| Age, mean ± SD (years) | 75.2 ± 6.5 | 74.1 ± 5.8 | 75.4 ± 6.7 | 81.9 ± 7.1 | <0.001 |
| Women, n (%) | 241 (74.6) | 115 (75.7) | 109 (71.7) | 17 (89.5) | 0.226 |
| BMI, mean ± SD (kg/m2) | 23.5 ± 3.4 | 23.4 ± 3.2 | 23.5 ± 3.5 | 23.6 ± 4.2 | 0.924 |
| GDS-15 score mean ± SD (points) | 2.5 ± 2.5 | 2.0 ± 2.0 | 2.8 ± 2.5 | 5.2 ± 3.5 | <0.001 |
| Medications mean ± SD (number) | 3.7 ± 3.9 | 3.0 ± 3.4 | 4.1 ± 4.0 | 6.0 ± 5.3 | 0.001 |
| Independent Variable | Dependent Value: Classification of Two Patterns of Physical Frailty Prevalence Rates | |||||||
|---|---|---|---|---|---|---|---|---|
| Non-Frailty & Pre-Frailty vs Frailty | Non-Frailty vs Pre-Frailty & Frailty | |||||||
| Crude | Adjusted | Crude | Adjusted | |||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Chronic pain | 1.53 (0.60–3.87) | 0.371 | 2.83 (0.79–10.21) | 0.112 | 1.95 (1.24–3.05) | 0.004 ** | 1.68 (1.03–2.76) | 0.040 * |
| Age | 1.22 (1.09–1.36) | 0.001 ** | 1.03 (0.99–1.07) | 0.176 | ||||
| Women | 2.15 (0.42–10.90) | 0.358 | 0.80 (0.47–1.38) | 0.428 | ||||
| BMI | 1.21 (1.00–1.46) | 0.058 | 1.00 (0.94–1.08) | 0.938 | ||||
| GDS-15 | 1.50 (1.20–1.87) | <0.001 ** | 1.17 (1.06–1.30) | 0.003 ** | ||||
| Medications | 1.15 (1.00–1.32) | 0.047 * | 1.06 (1.00–1.14) | 0.069 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakai, Y.; Makizako, H.; Kiyama, R.; Tomioka, K.; Taniguchi, Y.; Kubozono, T.; Takenaka, T.; Ohishi, M. Association between Chronic Pain and Physical Frailty in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 1330. https://doi.org/10.3390/ijerph16081330
Nakai Y, Makizako H, Kiyama R, Tomioka K, Taniguchi Y, Kubozono T, Takenaka T, Ohishi M. Association between Chronic Pain and Physical Frailty in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health. 2019; 16(8):1330. https://doi.org/10.3390/ijerph16081330
Chicago/Turabian StyleNakai, Yuki, Hyuma Makizako, Ryoji Kiyama, Kazutoshi Tomioka, Yoshiaki Taniguchi, Takuro Kubozono, Toshihiro Takenaka, and Mitsuru Ohishi. 2019. "Association between Chronic Pain and Physical Frailty in Community-Dwelling Older Adults" International Journal of Environmental Research and Public Health 16, no. 8: 1330. https://doi.org/10.3390/ijerph16081330
APA StyleNakai, Y., Makizako, H., Kiyama, R., Tomioka, K., Taniguchi, Y., Kubozono, T., Takenaka, T., & Ohishi, M. (2019). Association between Chronic Pain and Physical Frailty in Community-Dwelling Older Adults. International Journal of Environmental Research and Public Health, 16(8), 1330. https://doi.org/10.3390/ijerph16081330






