Characteristics of the Family Support Network of Pregnant Adolescents and Its Association with Gestational Weight Gain and Birth Weight of Newborns
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Measurement of the Family Support Network (FSN)
2.4. Evaluation of the FSN Size
2.5. Anthropometric Evaluation
2.6. Neonatal Characteristics
2.7. Sociodemographic Data
2.8. Dietary Evaluation
2.9. Ethical Considerations
2.10. Statistical Analysis
2.11. Ethics Approval and Consent to Participate
3. Results
3.1. Sociodemographic Data
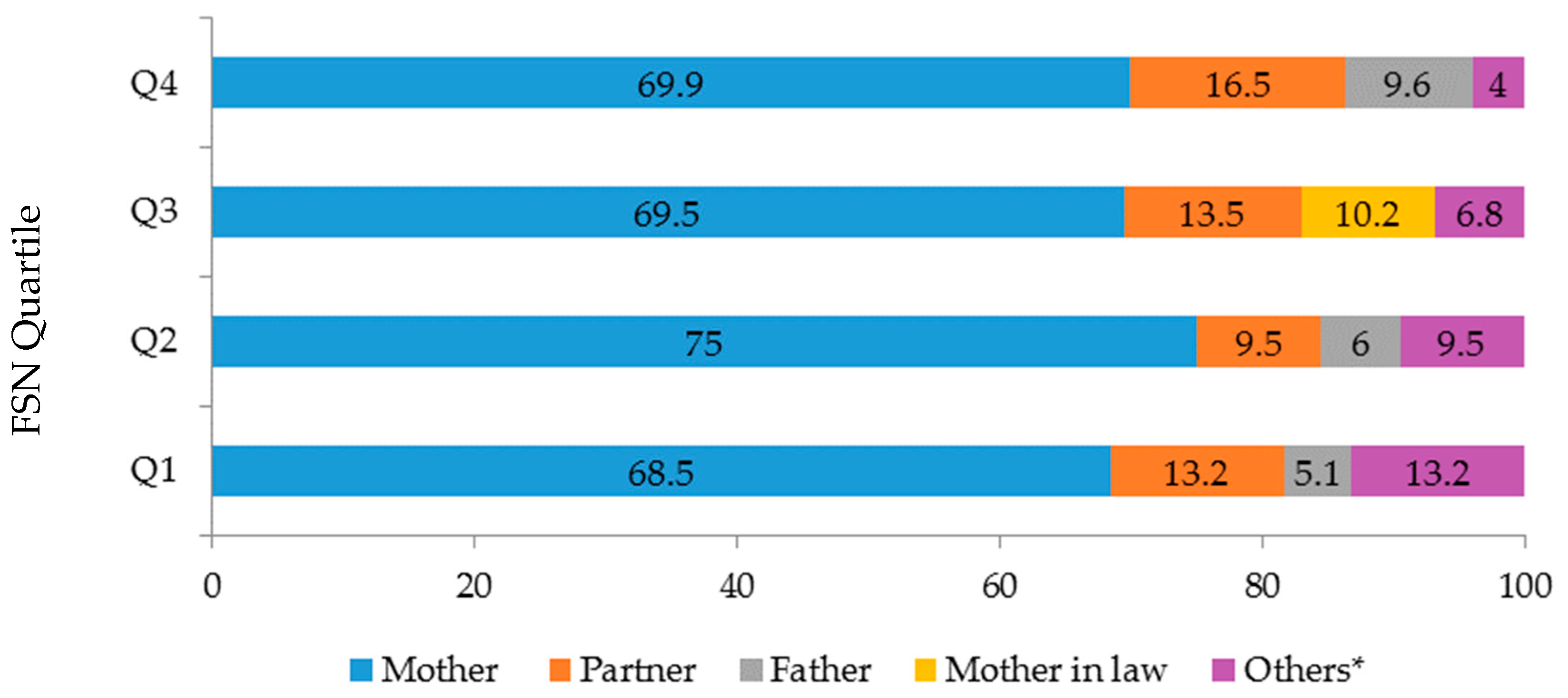
3.2. Family Support Network
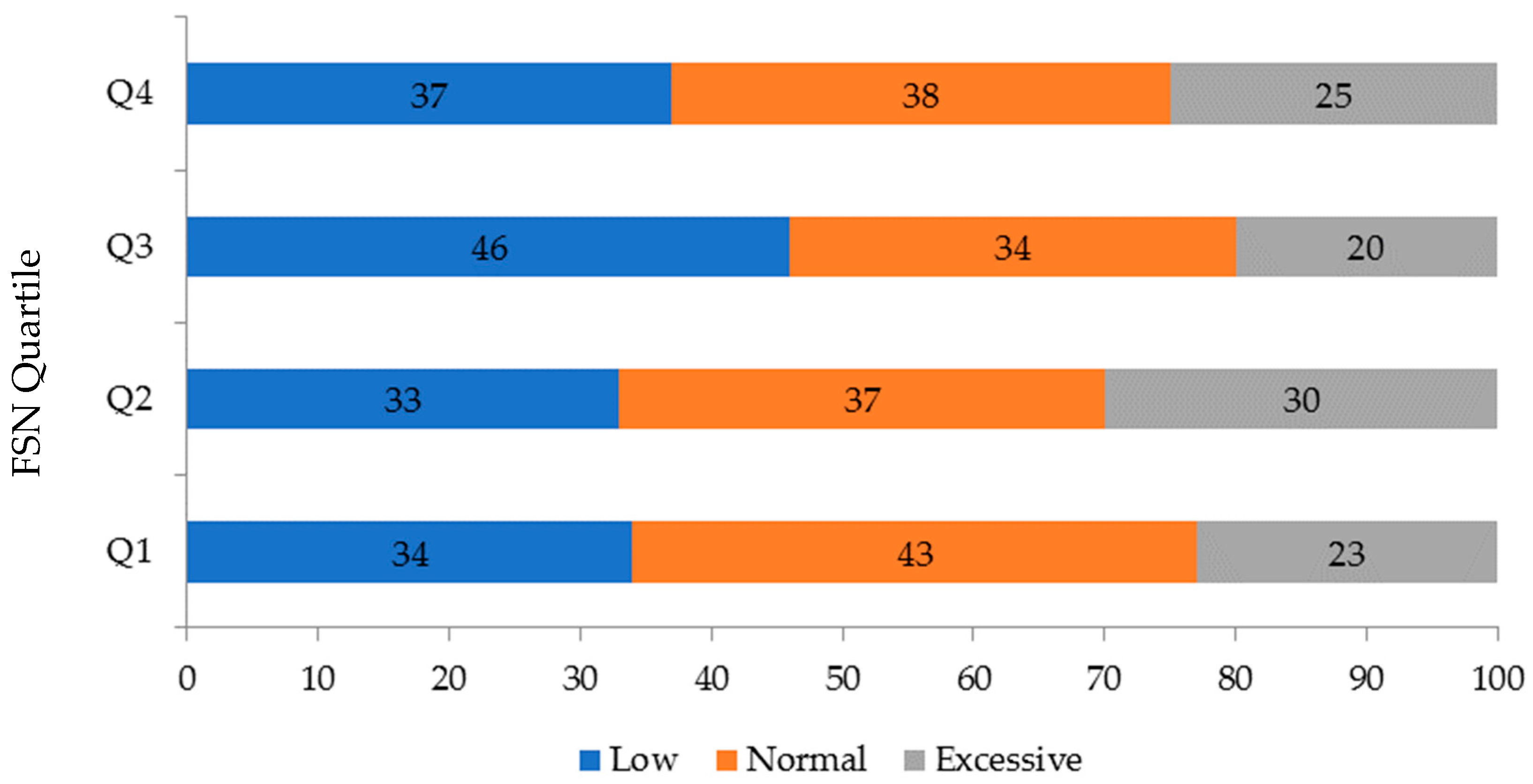
3.3. Dietary Evaluation
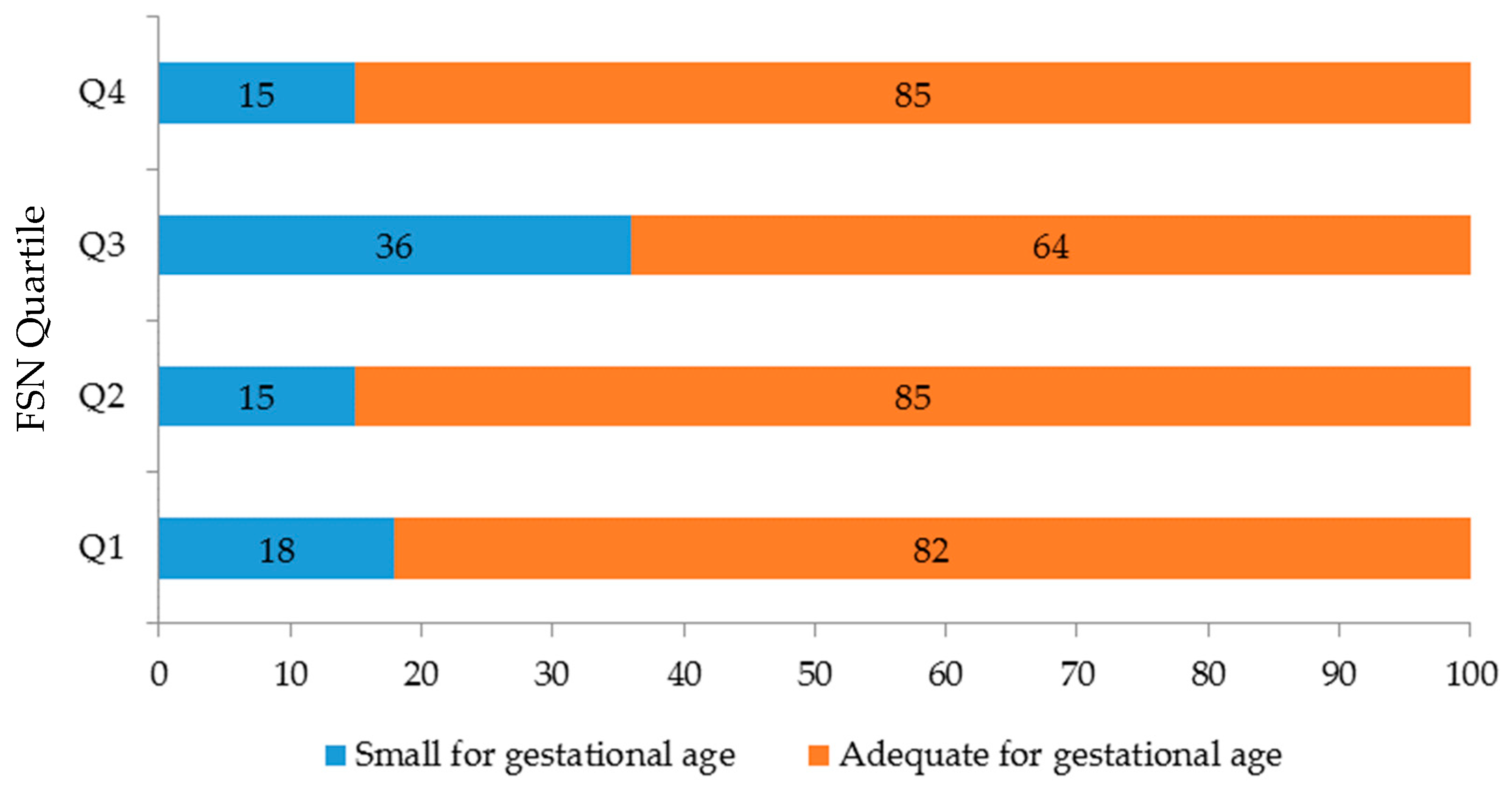
3.4. Evaluation of the Newborn
4. Discussion
4.1. Family Support Network Members
4.2. Family Support Network Size
4.3. Gestational Weigh Gain and Birth Weight
4.4. Implications of the Study
4.5. Limitations and Strengths of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CI | Confidence interval |
| FSN | Family support network |
| OR | Odds ratio |
| WHO | World Health Organization |
References
- Bourdieu, P. Forms of capital. In Handbook of Theory for the Sociology of Education; Richardson, J.G., Ed.; Greenwood Press: Westport, CT, USA, 1986; pp. e241–e258. [Google Scholar]
- Pearson, J.E. The definition and measurement of social support. J. Couns. Dev. 1986, 64, 390–395. [Google Scholar] [CrossRef]
- Bassett, E.; Moore, S. Social capital and depressive symptoms: The association of psychosocial and network dimensions of social capital with depressive symptoms in Montreal, Canada. Soc. Sci. Med. 2013, 6, 96–102. [Google Scholar] [CrossRef]
- Vaux, A. Social Support: Theory, Research, and Intervention; Praeger Publishers: New York, NY, USA, 1988. [Google Scholar]
- Xie, R.-H.; He, G.; Koszycki, D.; Walker, M.; Wen, S.W. Prenatal social support, postnatal social support, and postpartum depression. Ann. Epidemiol. 2009, 19, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Appleton, A.A.; Kiley, K.; Holdsworth, E.A.; Schell, L.M. Social Support during Pregnancy Modifies the Association between Maternal Adverse Childhood Experiences and Infant Birth Size. Matern. Child Health J. 2019, 23, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.B.; Leal, L.P.; Coriolano-Marinus, M.W.; Santos, A.H.; Horta, B.L.; Pontes, C.M. Meta-analysis of the effectiveness of educational interventions for breastfeeding promotion directed to the woman and her social network. J. Adv. Nurs. 2017, 73, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Katzow, M.; Messito, M.J.; Mendelsohn, A.L.; Scott, M.A.; Gross, R.S. The Protective Effect of Prenatal Social Support on Infant Adiposity in the First 18 Months of Life. J. Pediatr. 2019. [Google Scholar] [CrossRef]
- Branje, S. Development of Parent–Adolescent Relationships: Conflict Interactions as a Mechanism of Change. Child Dev. Perspect. 2018, 12, 171–176. [Google Scholar]
- bin Yaacob, M.J. Parent-adolescent relationships and its association to adolescents’ self-esteem. Malays. J. Med. Sci. 2006, 13, 21–24. [Google Scholar]
- Wall-Wieler, E.; Roos, L.L.; Nickel, N.C. Adolescent Pregnancy Outcomes among Sisters and Mothers: A Population-Based Retrospective Cohort Study Using Linkable Administrative Data. Public Health Rep. 2018, 133, 100–108. [Google Scholar] [CrossRef]
- Kumar, N.A.; Danilack, V.A.; Ware, C.F.; Phipps, M.G. Adolescent Mothers’ Relationships with their Mothers and their Babies’ Fathers during Pregnancy and Postpartum. J. Child Fam. Stud. 2018, 27, 2862–2870. [Google Scholar] [CrossRef]
- Lamarca, G.A.; DoCLeal, M.; Sheiham, A.; Vettore, M.V. The association of neighborhood and individual social capital with consistent self-rated health: A longitudinal study in Brazilian pregnant and postpartum women. BMC Pregnancy Childbirth 2013, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Nava-Aguilar, S.; Terán-Trillo, M.; Morena-Aguilera, F.; Bazán-Castro, M. Temas de salud y redes de apoyo en un grupo de adolescentes de la clínica de medicina familiar “Oriente” del ISSSTE. Revista de Especialidades Médico-Quirúrgicas 2007, 12, 46–52. [Google Scholar]
- Terán-Trillo, M. Test Para la Identificación de la Red Social Egocéntrica de Apoyo Social. Cuaderno 3. Serie. Cuadernos e Instrumentos de Apoyo Para la Atención Social en Cuidados Paliativos y Tanatología; Universidad Nacional Autónoma de México/Escuela Nacional de Trabajo Social, Terán-Trillo INDA-RPDA No. 03200506141111270001; En México registro ante el Instituto Nacional del Autor: México City, México, 2014. [Google Scholar]
- Roth, L.W.; Allshouse, A.A.; Lesh, J.; Polotsky, A.J.; Santoro, N. The correlation between self-reported and measured height, weight, and BMI in reproductive age women. Maturitas 2013, 76, 185–188. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of the WHO Consultation, WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Rasmussen, K.M.; Yaktine, A.L. (Eds.) Weight Gain during Pregnancy: Reexamining the Guidelines Institute of Medicine and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Lohman, T.G.; Roche, E.F.; Martorell, R. Anthropometric Standardization Reference Manual Champaign; Human Kinetics Books: Champaign, IL, USA, 1998; Volume Ill. [Google Scholar]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Mexican Association of Market Agencies and Public Opinion. Socioeconomic Levels. Mexico. 2015. Available online: http://nse.amai.org/ (accessed on 11 October 2015).
- Hernández-Ávila, J.E.; González-Avilés, L.; Rosales-Mendoza, E. Manual de Usuario. SNUT Sistema de Evaluación de Hábitos Nutricionales y Consumo de Nutrimentos; Instituto Nacional de Salud Pública: Cuernavaca, México, 2003. [Google Scholar]
- World Medical Association Inc. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects; World Medical Association, Inc.: Ferney-Voltaire, France, 2014. [Google Scholar]
- Quinn, D.A.; Mitchell, S.J.; Lewin, A. The role of teen mother’s support relationships in maintenance of contraceptive use. J. Pediatr. Adolesc. Gynecol. 2017, 30, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Long, Z.; Cao, D.; Cao, F. Social support and depression across the perinatal period: A longitudinal study. J. Clin. Nurs. 2017, 26, 2776–2783. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.M.; Bogat, G.A.; Davidson, W.S.; von Eye, A.; Levendosky, A. Family support and mental health in pregnant women experiencing interpersonal partner violence: An analysis of ethnic differences. Am. J. Community Psychol. 2005, 36, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.A.; Rhodes, J.E.; Hamilton-leaks, J. When both parents may be a source of support and problems: An analysis of pregnant and parenting female African American adolescents’ relationships with their mothers and fathers. J. Res. Adolesc. 1997, 7, 331–348. [Google Scholar] [CrossRef] [PubMed]
- Elsenbruch, S.; Benson, S.; Rücke, M.; Rose, M.; Dudenhausen, J.; Pincus-Knackstedt, M.K.; Klapp, B.F.; Arck, P.C. Social support during pregnancy: Effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum. Reprod. 2007, 22, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, L.E.; Newby, A. Family support and pregnancy behavior among women in two border Mexican cities. Frontera Norte 2010, 22, 7–34. [Google Scholar]
- Killoren, S.E.; Zeiders, K.H.; Updegraff, K.A.; Umaña-Taylor, A.J. The sociocultural context of Mexican-origin pregnant adolescents’ attitudes toward teen pregnancy and links to future outcomes. J. Youth Adolesc. 2016, 45, 887–899. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Kestens, Y.; Dahhou, M.; Daniel, M.; Kramer, M.S. Neighbourhood deprivation and maternal psychological distress during pregnancy: A multilevel analysis. Matern. Child Health J. 2015, 19, 1142–1151. [Google Scholar] [CrossRef] [PubMed]
- Ashaman, A.M.; Collins, C.E.; Hure aj Jensen, M.; Oldmeandow, C. Maternal diet during early childhood, but not pregnancy, predicts diet quality, fruit, and vegetable acceptance in Offspring. Matern. Child Nutr. 2016, 12, 579–590. [Google Scholar] [CrossRef]
- Gutiérrez, J.P.; García-Saisó, S.; Espinosa-de la Peña, R.; Balandrán, D.A. Health inequalities on adolescents’ risk behavior indicators in Mexico: Analysis of two national health surveys. Salud Publica Mex. 2016, 58, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Almeida Mda, C.; Aquino, E.M. Adolescent pregnancy and completion of basic education: A study of young people in three state capital cities in Brazil. Cad. Saude Publica 2011, 27, 2386–2400. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.M.; Teich, J.L.; Mutter, R. The impact of single mothers’ health insurance coverage on behavioral health services utilization by their adolescent children. J. Behav. Health Serv. Res. 2018, 45, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-González, A.; Granados-Cosme, J.A.; Rosales-Flores, R.A. Adolescense pregnancy in a marginalized rural community in Mexico. Salud Publica Mex. 2017, 59, 11–18. [Google Scholar] [CrossRef]
- Rodríguez, M.A.; Jiménez, M.A. Epidemiological assessment of the influence of socio-family factors in adolescent pregnancy. Eur. J. Epidemiol. 2001, 17, 653–659. [Google Scholar] [CrossRef]
- Wamoyi, J.; Wight, D. ‘Mum never loved me.’ How structural factors influence adolescent sexual and reproductive health through parent-child connectedness: A qualitative study in rural Tanzania. Afr. J. AIDS Res. 2014, 13, 169–178. [Google Scholar] [CrossRef]
- Jonas, K.; Crutzen, R.; van den Borne, B.; Sewpaul, R.; Reddy, P. Teenage pregnancy rates and associations with other health risk behaviours: A three-wave cross-sectional study among South African school-going adolescents. Reprod. Health 2016, 13, 50. [Google Scholar] [CrossRef]
| Characteristics | Q1 (n = 136) | Q2 (n = 84) | Q3 (n = 59) | Q4 (n = 73) | p-Value |
|---|---|---|---|---|---|
| Age (years) * | 15.3 ± 1 | 15.6 ± 1 | 15.7 ± 1 | 15.4 ± 1 | 0.360 |
| Age of menarche (years) * | 11.7 ± 1 | 11.7 ± 1 | 11.5 ± 1 | 11.9 ± 2 | 0.450 |
| Gynaecological age (years) * | 3.6 ± 1.4 | 3.9 ± 1.5 | 4.2 ± 1.5 | 3.5 ± 1 | 0.900 |
| Level of education ** | 0.320 | ||||
| <9 years | 117 (86) | 65 (77) | 44 (79) | 60 (85) | |
| ≥9 years | 19 (14) | 19 (23) | 12 (21) | 11 (15) | |
| Partner’s occupation ** | 0.650 | ||||
| Student | 38 (29) | 21 (27) | 12 (23) | 13 (20) | |
| Working | 69 (52) | 46 (60) | 32 (62) | 43 (66) | |
| Other | 24 (18) | 10 (13) | 8 (15) | 9 (14) | |
| Marital status (n = 341) ** | 0.016 | ||||
| Single | 88 (66) | 47 (57) | 23 (42) | 35 (51) | |
| Married/cohabiting | 46 (34) | 36 (43) | 32 (58) | 34 (49) | |
| Number of persons living in the household ** | <0.001 | ||||
| 0–2 | 59 (43) | 17 (21) | 13 (23) | 13 (18) | |
| 3–4 | 51 (38) | 44 (52) | 26 (46) | 33 (46) | |
| 5–24 | 26 (19) | 23 (27) | 17 (30) | 25 (35) | |
| Prenatal care initiation (weeks) * | 19 ± 6 | 19 ± 6 | 19 ± 5 | 18 ± 6 | |
| Prenatal care initiation (by trimester) ** | |||||
| First | 23 (17) | 16 (19) | 11 (20) | 15 (21) | 0.790 |
| Second | 107 (79) | 65 (77) | 40 (71) | 53 (75) | |
| Third | 6 (4) | 3 (4) | 5 (9) | 3 (4) |
| Characteristics | Q1 (n = 136) | Q2 (n = 84) | Q3 (n = 59) | Q4 (n = 73) | p-value |
|---|---|---|---|---|---|
| Mother | |||||
| Pre-gestational weight (kg) | 51.2 ± 7.9 | 52.2 ± 8.8 | 52.5 ± 7.5 | 52.0 ± 7.6 | 0.670 |
| Pre-gestational BMI (kg/m2) | 21.2 ± 3.3 | 21.8 ± 3.9 | 21.7 ± 3.3 | 21.5 ± 3.3 | 0.640 |
| Energy intake (Kcal) | 2035 ± 572 | 2127 ± 573 | 2124 ± 513 | 2300 ± 592 | 0.020 |
| Gestational age (weeks) | 39 ± 1 | 39 ± 1 | 38 ± 2 | 39 ± 1 | 0.540 |
| Total gestational weight gain (kg) | 12.8 ± 4.9 | 13.1 ± 6.0 | 11.8 ± 4.6 | 13.0 ± 4.9 | 0.054 |
| Newborns | |||||
| Gender * | |||||
| Girl | 74 (54) | 47 (56) | 32 (57) | 34 (48) | 0.690 |
| Boy | 62 (46) | 37 (44) | 24 (43) | 37 (52) | |
| Birth weight (g) | 2897 ± 456 | 2964 ± 396 | 2790 ± 483 | 2914 ± 440 | 0.150 |
| Birth weight for gestational age (z-score) | −0.62 ± 0.9 | −0.46 ± 1.0 | −0.83 ± 0.8 | −0.59 ± 0.84 | 0.120 |
| Birth length for gestational age (z-score) † | −0.35 ± 0.8 | −0.2 ± 1.0 | −0.55 ± 0.9 | −0.39 ± 0.88 | 0.140 |
| Head circumference (cm) | 33.2 ± 1.4 | 33.1 ± 1.7 | 33.0 ± 1.3 | 33.9 ± 2.0 | 0.700 |
| Odds ratio | p-value | 95% CI | |
|---|---|---|---|
| Model 1 * | |||
| Quartile 1 | 1.23 | 0.60 | 0.57–2.67 |
| Quartile 2 | 0.99 | 0.99 | 0.42–2.39 |
| Quartile 3 | 3.03 | 0.01 | 1.30–7.0 |
| Quartile 4 | Reference | ||
| Model 2 ** | |||
| Quartile 1 | 1.1 | 0.81 | 0.49–2.44 |
| Quartile 2 | 0.89 | 0.80 | 0.36–2.20 |
| Quartile 3 | 2.99 | 0.01 | 1.25–7.15 |
| Quartile 4 | Reference | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sámano, R.; Martínez-Rojano, H.; Chico-Barba, G.; Sánchez-Jiménez, B.; Illescas-Zarate, D.; Rodríguez-Ventura, A.L. Characteristics of the Family Support Network of Pregnant Adolescents and Its Association with Gestational Weight Gain and Birth Weight of Newborns. Int. J. Environ. Res. Public Health 2019, 16, 1222. https://doi.org/10.3390/ijerph16071222
Sámano R, Martínez-Rojano H, Chico-Barba G, Sánchez-Jiménez B, Illescas-Zarate D, Rodríguez-Ventura AL. Characteristics of the Family Support Network of Pregnant Adolescents and Its Association with Gestational Weight Gain and Birth Weight of Newborns. International Journal of Environmental Research and Public Health. 2019; 16(7):1222. https://doi.org/10.3390/ijerph16071222
Chicago/Turabian StyleSámano, Reyna, Hugo Martínez-Rojano, Gabriela Chico-Barba, Bernarda Sánchez-Jiménez, Daniel Illescas-Zarate, and Ana Lilia Rodríguez-Ventura. 2019. "Characteristics of the Family Support Network of Pregnant Adolescents and Its Association with Gestational Weight Gain and Birth Weight of Newborns" International Journal of Environmental Research and Public Health 16, no. 7: 1222. https://doi.org/10.3390/ijerph16071222
APA StyleSámano, R., Martínez-Rojano, H., Chico-Barba, G., Sánchez-Jiménez, B., Illescas-Zarate, D., & Rodríguez-Ventura, A. L. (2019). Characteristics of the Family Support Network of Pregnant Adolescents and Its Association with Gestational Weight Gain and Birth Weight of Newborns. International Journal of Environmental Research and Public Health, 16(7), 1222. https://doi.org/10.3390/ijerph16071222





