Implications of Cardioprotective Assumptions for National Drinking Guidelines and Alcohol Harm Monitoring Systems
Abstract
:1. Introduction
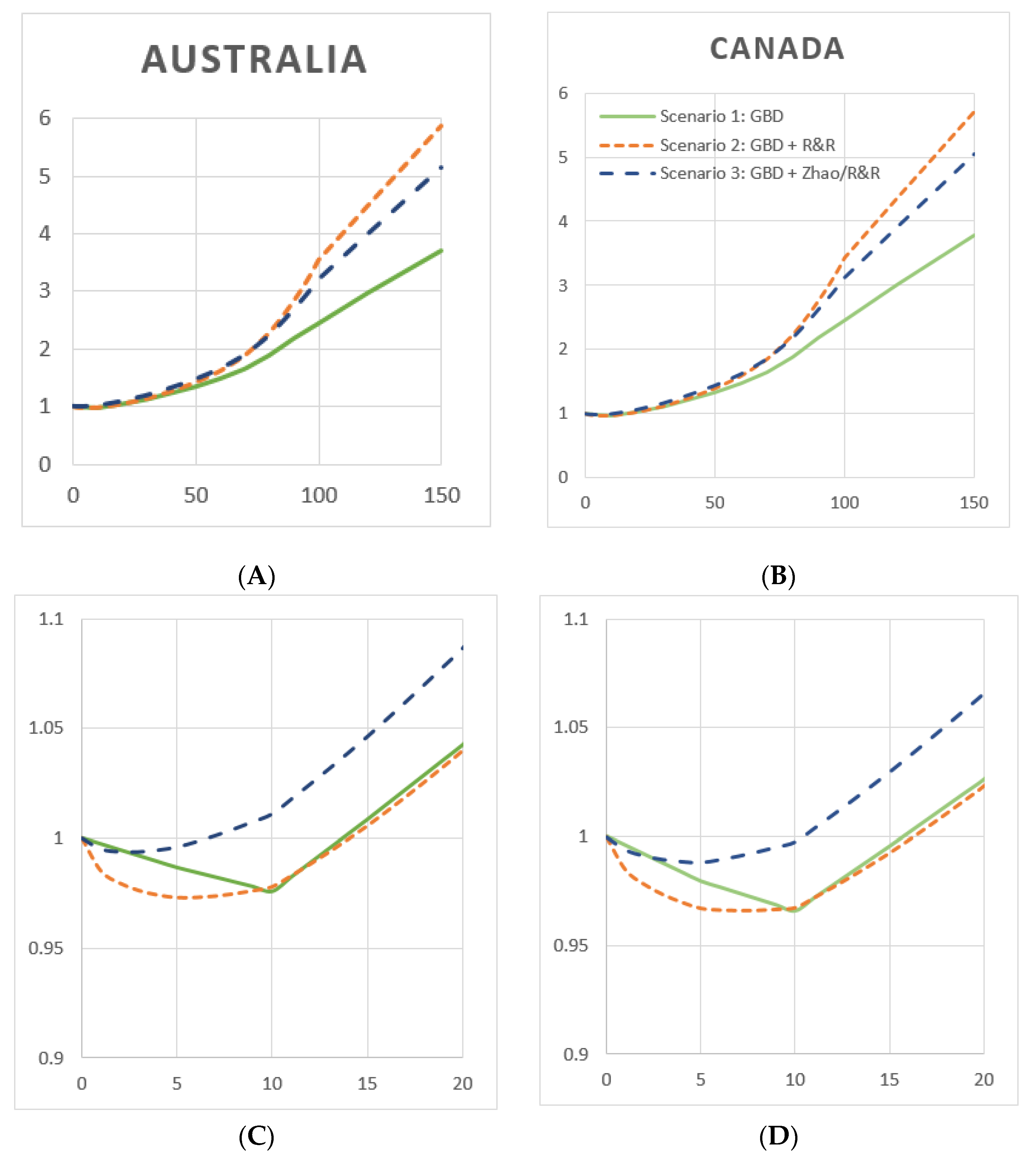
- (A)
- (B)
- In Scenario 1, IHD RR functions for men and women were from the 2016 GBD study [2] (p. 97);
- In Scenario 2, IHD RR functions for men and women were sourced from Roerecke & Rehm [19] (p. 1252), and;
- In Scenario 3, the IHD RR function for men was sourced from Zhao et al. [20]. The functional form, requested from the author, is a component of a further study [22] (p. 72). The IHD RR function for women was sourced from Roerecke & Rehm [19] (p. 1252); this was chosen as there were too few women-specific studies in the Zhao et al. analysis to complete a gender-specific meta-analysis.
- Estimates of alcohol-caused mortality in Australia and Canada in 2015, the most recent year for which data was available for both countries, and
- Country-specific mortality-weighted RR functions, by gender and total.
2. Materials and Methods
2.1. Conceptual Framework and Terminology
2.2. Alcohol-Attributable Fraction Methodology
2.3. Data Sources
2.3.1. Mortality Data
2.3.2. Alcohol Exposure Data
2.3.3. Relative Risk Functions
2.3.4. Population and Death Data, Totals
2.4. Statistical Analyses
2.5. Estimating Alcohol-Attributable Deaths: Net, Caused and Prevented
- Mortality counts, by country, health condition, gender, and age group, were enumerated from official data, see Data Sources. Health conditions were only enumerated if they appeared as the primary cause of death on a mortality record, not if they were listed as a contributing cause; this matches other studies [1,5].
- Net AAFs, by country, health condition, gender and age group were calculated by InterMAHP using our collected data sources as input, with no modification to the RR functions.
- Gross AAFs, by country, health condition, gender, and age group were calculated by InterMAHP, but RR functions were modified to have no protection, i.e., all RR values <1.0 were set to 1.0. This has the effect of calculating gross death as any protection is removed.
- Net and gross alcohol-attributable (AA) deaths were then calculated at this same level of granularity by multiplying both the net and gross AAF of each grouping by the corresponding number of enumerated deaths.
- Deaths prevented were then calculated as the difference between net deaths and gross deaths.
2.6. Creating Weighted Relative Risk Functions, by Gender
3. Results
3.1. Per Capita Consumption and Drinking Prevalence in Australia and Canada
3.2. Net, Gross, and Prevented Alcohol-Attributable Deaths under Three Cardioprotective Scenarios
3.3. Population- and Death-Based Rates of Net Alcohol-Attributable Deaths
3.4. Net Alcohol-Attributable Deaths, by Gender and Health Condition Category
3.5. Weighted Relative Risk Functions, by Cardioprotective Scenario
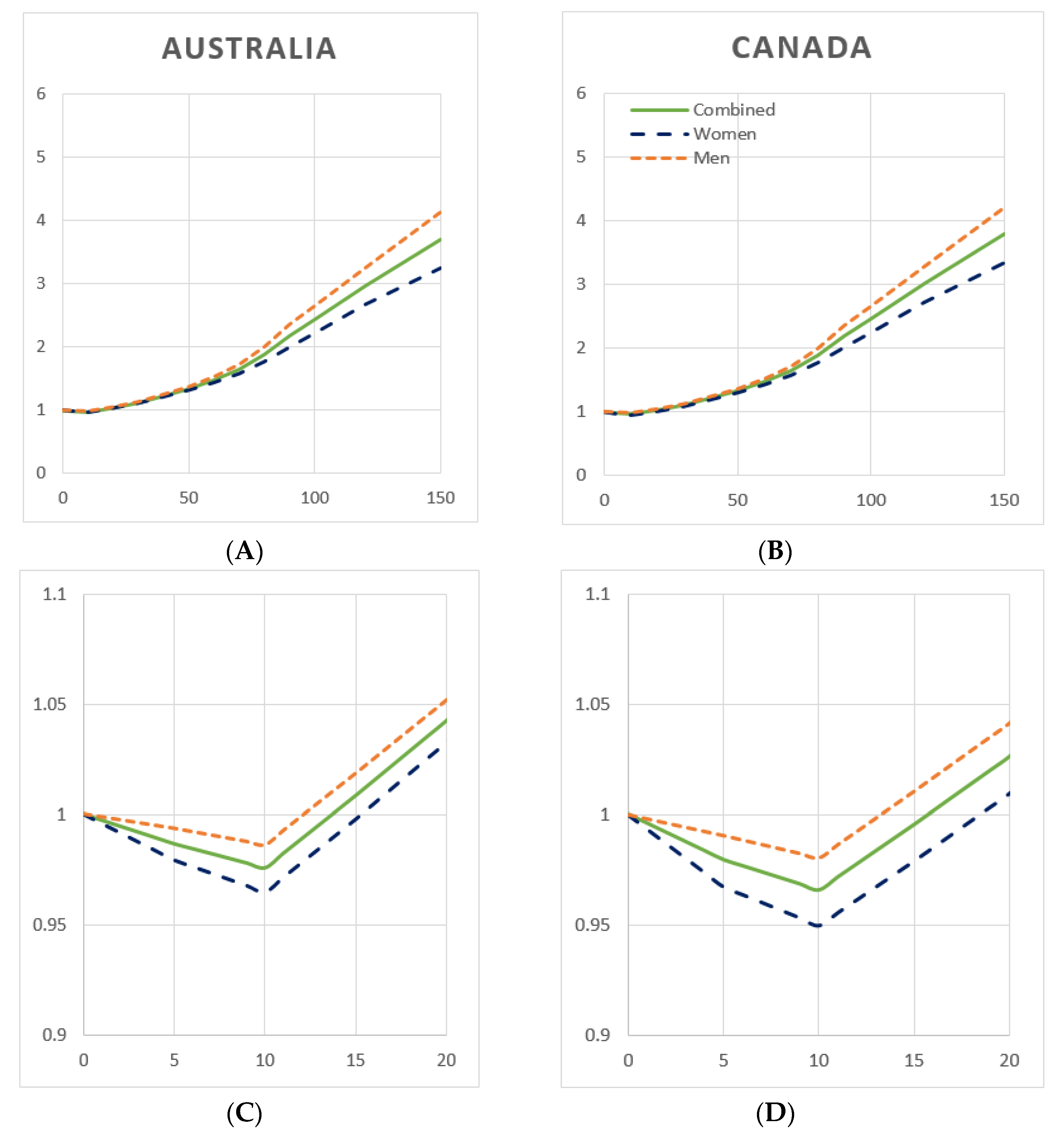
3.6. Weighted Relative Risk Functions, by Gender
3.7. Weighted Relative Risk Functions, by Net vs. Gross Harms
4. Discussion
- (A)
- Minimize risk, i.e., the theoretical minimum risk exposure level (TMREL);
- (B)
- equalize the risk of a drinker with that of a non-drinker, i.e., result in ‘no added risk’ from alcohol use, or;
- (C)
- be used to inform higher, ‘low risk drinking guidelines’, which advise guidelines based on a chosen level of ‘acceptable additional risk’ from alcohol use.
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef] [Green Version]
- Chikritzhs, T. Tools for policy and prevention: The Australian national alcohol indicators project. Contemp. Drug Probl. 2009, 36, 607–624. [Google Scholar] [CrossRef]
- Lensvelt, E.; Gilmore, W.; Liang, W.; Sherk, A.; Chikritzhs, T. Estimated Alcohol-Attributable Deaths and Hospitalisations in Australia, 2004 to 2015; National Drug Research Institute, Curtin University: Perth, Australia, 2018. [Google Scholar]
- Canadian Substance Use Costs and Harms Scientific Working Group. Canadian Substance Use Costs and Harms Scientific Working Group: Canadian Substance Use Costs and Harms (2007–2014); (Prepared by the Canadian Institute for Substance Use Research and the Canadian Centre on Substance Use and Addiction); Canadian Centre on Substance Use and Addiction: Ottawa, ON, Canada, 2018. [Google Scholar]
- Institute for Health Metrics and Evaluation. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results; Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2017. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 11 October 2017).
- World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm; World Health Organizations: Geneva, Switzerland, 2000. [Google Scholar]
- Babor, T.; Caetano, R.; Casswell, S.; Edwards, G.; Giesbrecht, N.; Graham, K.; Grube, J.; Hill, L.; Holder, H.; Homel, R.; et al. Alcohol: No Ordinary Commodity: Research and Public Policy; Oxford University Press: New York, NY, UK, 2010. [Google Scholar]
- International Alliance for Responsible Drinking, Drinking Guidelines, General Population. Available online: http://www.iard.org/policy-tables/drinking-guidelines-general-population/ (accessed on 1 October 2019).
- Kalinowski, A.; Humphreys, K. Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction 2016, 111, 1293–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chikritzhs, T.; Stockwell, T.; Naimi, T.; Andreasson, S.; Dangardt, F.; Liang, W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed? Addiction 2015, 110, 726–727. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, T.; Zhao, J.; Panwar, S.; Roemer, A.; Naimi, T.; Chikritzhs, T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J. Stud. Alcohol Drugs 2016, 77, 185–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naimi, T.S.; Stockwell, T.; Zhao, J.; Xuan, Z.; Dangardt, F.; Saitz, R.; Liang, W.; Chikritzhs, T. Selection biases in observational studies affect associations between ‘moderate’ alcohol consumption and mortality. Addiction 2017, 112, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J. Why the relationship between level of alcohol-use and all-cause mortality cannot be addressed with meta-analyses of cohort studies. Drug Alcohol Rev. 2019, 38, 3–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistics Canada. CANSIM Table 13-10-0710-01: Deaths and Mortality Rates, by Age Group; Statistics Canada: Ottawa, ON, Canada, 2019. [Google Scholar]
- Cause of death unit record file dataset. In Queensland Registry of Births, Deaths and Marriages; Registry AC: Brisbane, Australia, 2015.
- Statistics Canada. CANSIM Table 13-10-0392-01: Deaths and Age-Specific Mortality Rates, by Selected Grouped Causes. Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039201 (accessed on 29 September 2019).
- Australian Bureau of Statistics. Deaths, Year of Occurrence, Age at Death, Age-Specific Death Rates, Sex, States, Territories and Australia; Australian Bureau of Statistics: Canberra, Australia, 2019.
- Roerecke, M.; Rehm, J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: A systematic review and meta-analysis. Addiction 2012, 107, 1246–1260. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Stockwell, T.; Roemer, A.; Naimi, T.S.; Chikritzhs, T. Alcohol consumption and mortality from coronary heart disease: An updated meta-analysis of cohort studies. J. Stud. Alcohol Drugs 2017, 78, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, T.; Sherk, A.; Norström, T.; Angus, C.; Ramstedt, M.; Andréasson, S.; Chikritzhs, T.; Gripenberg, J.; Holder, H.; Holmes, J.; et al. Estimating the public health impact of disbanding a government alcohol monopoly: Application of new methods to the case of Sweden. BMC Public Health 2018, 18, 1400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherk, A.; Stockwell, T.; Rehm, J.; Dorocicz, J.; Shield, K.D. The International Model of Alcohol Harms and Policies (InterMAHP): A Comprehensive Guide to the Estimation of Alcohol-Attributable Morbidity and Mortality, Version 1.0; Canadian Institute for Substance Use Research, University of Victoria: British Columbia, BC, Canada, 2017. Available online: www.intermahp.cisur.ca. 2017 (accessed on 04 September 2019).
- Rothman, K.J.; Greenland, S.; Lash, T.L. Modern Epidemiology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- United States Centers for Disease Control and Prevention. Alcohol-Related Disease Impact (ARDI) Tool; CDC: Atlanta, GA, USA, 2008. [Google Scholar]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E. Alcohol consumption and site-specific cancer risk: A comprehensive dose–response meta-analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef] [PubMed]
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Personal Habits and Indoor Combustion; IARC: Lyon, France, 2012. [Google Scholar]
- Kehoe, T.; Gmel, G.; Shield, K.D.; Gmel, G.; Rehm, J. Determining the best population-level alcohol consumption model and its impact on estimates of alcohol-attributable harms. Popul. Health Metr. 2012, 10, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gmel, G.; Shield, K.D.; Kehoe-Chan, T.A.; Rehm, J. The effects of capping the alcohol consumption distribution and relative risk functions on the estimated number of deaths attributable to alcohol consumption in the European Union in 2004. BMC Med. Res. Methodol. 2013, 13, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 04 February 2018).
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Australian Bureau of Statistics. 4307.0.55.001 Apparent Consumption of Alcohol, Australia, 2012–2013; ABS: Canberra, Australia, 2017. [Google Scholar]
- Stockwell, T.; Zhao, J.; Chikritzhs, T.; Greenfield, T.K. What did you drink yesterday? Public health relevance of a recent recall method used in the 2004 Australian National Drug Strategy Household Survey. Addiction 2008, 103, 919–928. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, S. Unrecorded alcohol consumption in Ontario, Canada: Estimation procedures and research implications. Drug Alcohol Rev. 1999, 18, 21–29. [Google Scholar] [CrossRef]
- Australian Institute for Health and Welfare. Australian Institute for Health and Welfare: National Drug Strategy Household Survey Detailed Report: 2013; AIHW: Canberra, Australia, 2014. [Google Scholar]
- Statistics Canada. Canadian Tobacco, Alcohol and Drug Survey; Statistics Canada: Ottawa, ON, Canada, 2019. [Google Scholar]
- Australian Bureau of Statistics. 3101.0 Australian Demographic Statistics, Dec 2017; ABS: Canberra, Austrania, 2017. [Google Scholar]
- Statistics Canada. CANSIM Table 17-10-0005-01: Population Estimates on July 1st, by Age and Sex; Statistics Canada: Ottawa, ON, Canada, 2018. [Google Scholar]
- Shield, K.; Centre for Addiction and Mental Health, Toronto, Ontario, Canada. Personal Correspondence, 3 October 2019.
- Shield, K.D.; Gmel, G.; Mäkelä, P.; Probst, C.; Room, R.; Rehm, J. Life-time risk of mortality due to different levels of alcohol consumption in seven European countries: Implications for low-risk drinking guidelines. Addiction 2017, 112, 1535–1544. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Guidelines to Reduce Health Risks from Drinking Alcohol; Commonwealth of Australia: Canberra, Australia, 2009. [Google Scholar]
- Patra, J.; Taylor, B.; Irving, H.; Roerecke, M.; Baliunas, D.; Mohapatra, S.; Rehm, J. Alcohol consumption and the risk of morbidity and mortality for different stroke types-a systematic review and meta-analysis. BMC Public Health 2010, 10, 2581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehm, J.; Taylor, B.; Mohapatra, S.; Irving, H.; Baliunas, D.; Patra, J.; Roerecke, M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug Alcohol Rev. 2010, 29, 437–445. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report on Alcohol and Health; WHO Press: Geneva, Switzerland, 2011. [Google Scholar]
- Witbrodt, J.; Mulia, N.; Zemore, S.E.; Kerr, W.C. Racial/ethnic disparities in alcohol-related problems: Differences by gender and level of heavy drinking. Alcohol. Clin. Exp. Res. 2014, 38, 1662–1670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Gender | Age Group | Australia (APC = 9.90 L) | Canada (APC = 9.69 L) | ||||
|---|---|---|---|---|---|---|---|
| Current Drinkers | Former Drinkers | Lifetime Abstainers | Current Drinkers | Former Drinkers | Lifetime Abstainers | ||
| Male | 15 to 34 | 0.75 | 0.05 | 0.21 | 0.81 | 0.07 | 0.12 |
| 35 to 64 | 0.85 | 0.06 | 0.08 | 0.82 | 0.12 | 0.06 | |
| 65+ | 0.80 | 0.13 | 0.08 | 0.74 | 0.20 | 0.05 | |
| Female | 15 to 34 | 0.72 | 0.05 | 0.23 | 0.75 | 0.09 | 0.17 |
| 35 to 64 | 0.81 | 0.08 | 0.11 | 0.77 | 0.14 | 0.09 | |
| 65+ | 0.68 | 0.14 | 0.18 | 0.65 | 0.24 | 0.12 | |
| Total | 0.78 | 0.07 | 0.15 | 0.77 | 0.13 | 0.10 | |
| Health Category and Condition | Australia | Canada | ||||
|---|---|---|---|---|---|---|
| Scen. 1: GBD | Scen. 2: GBD + R&R | Scen. 3: GBD + Zhao/R&R | Scen. 1: GBD | Scen. 2: GBD + R&R | Scen. 3: GBD + Zhao/R&R | |
| Cancers | ||||||
| Breast cancer | 293.1 | 528.9 | ||||
| Colorectal cancer | 430.8 | 854.8 | ||||
| Laryngeal cancer | 51.6 | 94.7 | ||||
| Liver cancer | 161.4 | 262.8 | ||||
| Oesophageal cancer | 136.2 | 207.2 | ||||
| Oropharyngeal cancer | 275.6 | 383.5 | ||||
| Subtotal | 1348.6 | 2331.8 | ||||
| Cardiovascular Conditions | ||||||
| Atrial fibrillation and flutter | 171.8 | 313.8 | ||||
| Haemorrhagic stroke | 280.8 | 418.4 | ||||
| Hypertensive heart disease | 271.7 | 417.8 | ||||
| Ischaemic heart disease | ||||||
| Deaths caused: | 186.0 | 1268.6 | 900.7 | 295.7 | 1925.4 | 1414.5 |
| Deaths prevented: | 1489.0 | 1603.7 | 567.3 | 2877.4 | 3231.4 | 1151.3 |
| Net deaths: | −1303.0 | −335.1 | 333.4 | −2581.6 | −1306.0 | 262.3 |
| Ischaemic stroke | Deaths caused: 54.9 | Deaths caused: 262.5 | ||||
| Deaths prevented: 103.9 | Deaths prevented: 628.4 | |||||
| Net deaths: −49.0 | Net deaths: −365.9 | |||||
| Alcoholic cardiomyopathy | 54.0 | 80.0 | ||||
| Subtotal | ||||||
| Deaths caused: | 1019.4 | 2102.0 | 1734.1 | 1788.5 | 3418.2 | 2907.3 |
| Deaths prevented: | 1593.2 | 1707.8 | 671.4 | 3506.1 | 3860.2 | 1780.1 |
| Net deaths: | −573.8 | 394.2 | 1062.7 | −1717.6 | −442.0 | 1127.2 |
| Diabetes | ||||||
| Subtotal | Deaths caused: 35.6 | Deaths caused: 110.8 | ||||
| Deaths prevented: 162.0 | Deaths prevented: 569.6 | |||||
| Net deaths: −126.4 | Net deaths: −458.8 | |||||
| Digestive Conditions | ||||||
| Cirrhosis of the liver | 849.6 | 1842.6 | ||||
| Pancreatitis | 45.8 | 106.9 | ||||
| Subtotal | 895.4 | 1949.6 | ||||
| Infectious Diseases | ||||||
| Tuberculosis | 14.3 | 33.1 | ||||
| Lower respiratory infections | 145.3 | 315.1 | ||||
| Subtotal | 159.6 | 348.3 | ||||
| Neuropsychiatric Conditions | ||||||
| Alcohol use disorders | 248.0 | 888.0 | ||||
| Epilepsy | 54.2 | 56.3 | ||||
| Subtotal | 302.2 | 944.3 | ||||
| Injuries | ||||||
| Alcohol poisoning | 68.0 | 281.0 | ||||
| Interpersonal violence | 27.4 | 63.4 | ||||
| Self-harm | 501 | 780.0 | ||||
| Transport injuries | 147.9 | 276.1 | ||||
| Unintentional injuries | 183.2 | 381.3 | ||||
| Subtotal | 927.5 | 1781.9 | ||||
| Grand Total | ||||||
| Deaths caused: | 4688.3 | 5770.9 | 5403.0 | 9255.0 | 10,884.7 | 10,373,8 |
| Deaths prevented: | 1755.2 | 1869.0 | 833.5 | 4075.8 | 4429.8 | 2349.7 |
| Net deaths: | 2933.1 | 3901.0 | 4569.5 | 5179.2 | 6454.9 | 8024.1 |
| Health Category | Australia | Canada | ||||
|---|---|---|---|---|---|---|
| Scen 1: GBD | Scen 2: GBD + R&R | Scen 3: GBD + Zhao/R&R | Scen 1: GBD | Scen 2: GBD + R&R | Scen 3: GBD + Zhao/R&R | |
| Rate per 1,000,000 Population | ||||||
| Cancer | 71.9 | 78.0 | ||||
| Cardiovascular conditions | −30.6 | 21.0 | 56.6 | −57.4 | −14.8 | 37.7 |
| Ischaemic heart disease | −69.4 | −17.9 | 17.8 | −86.3 | −43.7 | 8.8 |
| Diabetes | −6.7 | −15.3 | ||||
| Digestive conditions | 47.7 | 65.2 | ||||
| Infectious diseases | 8.5 | 11.6 | ||||
| Neuropsychiatric conditions | 16.1 | 31.6 | ||||
| Injuries | 49.4 | 59.6 | ||||
| Total | 156.3 | 207.9 | 243.5 | 173.2 | 215.8 | 268.3 |
| Rate per 10,000 Deaths | ||||||
| Cancer | 86.6 | 89.0 | ||||
| Cardiovascular conditions | −36.8 | 25.3 | 68.2 | −65.6 | −16.9 | 43.0 |
| Ischaemic heart disease | −83.6 | −21.5 | 21.4 | −98.6 | −49.9 | 10.0 |
| Diabetes | −8.1 | −17.5 | ||||
| Digestive conditions | 57.5 | 74.4 | ||||
| Infectious diseases | 10.2 | 13.3 | ||||
| Neuropsychiatric conditions | 19.4 | 36.1 | ||||
| Injuries | 59.5 | 68.0 | ||||
| Total | 188.3 | 250.4 | 293.3 | 197.7 | 246.4 | 306.4 |
| Health Category | Australia | Canada | ||||
|---|---|---|---|---|---|---|
| Scen 1: GBD | Scen 2: GBD + R&R | Scen 3: GBD + Zhao/R&R | Scen 1: GBD | Scen 2: GBD + R&R | Scen 3: GBD + Zhao/R&R | |
| Men | ||||||
| Cancer | 807.3 | 1,397.1 | ||||
| Cardiovascular conditions | −140.4 | 371.5 | 1040.0 | −404.4 | 324.0 | 1893.2 |
| Ischaemic heart disease | −667.8 | −156 | 512.6 | −1362.3 | −633.9 | 935.2 |
| Diabetes | 2.5 | −5.3 | ||||
| Digestive conditions | 705.5 | 1549.9 | ||||
| Infectious diseases | 119.3 | 271.9 | ||||
| Neuropsychiatric conditions | 237.5 | 727.4 | ||||
| Injuries | 733.9 | 1399.9 | ||||
| Subtotal | 2465.5 | 2977.4 | 3645.9 | 4936.4 | 5664.8 | 7234.0 |
| Percent of total | 84.1% | 76.3% | 79.8% | 95.3% | 87.8% | 90.2% |
| Women | ||||||
| Cancer | 541.4 | 934.7 | ||||
| Cardiovascular conditions | −433.4 | 22.7 | 22.7 | −1313.3 | −766.0 | −766.0 |
| Ischaemic heart disease | −635.2 | −179.1 | −179.1 | −1219.4 | −672.1 | −672.1 |
| Diabetes | −128.9 | −453.5 | ||||
| Digestive conditions | 189.9 | 399.6 | ||||
| Infectious diseases | 40.3 | 76.4 | ||||
| Neuropsychiatric conditions | 64.7 | 216.9 | ||||
| Injuries | 193.6 | 382.0 | ||||
| Subtotal | 467.6 | 923.7 | 923.7 | 242.8 | 790.1 | 790.1 |
| Percent of total | 15.9% | 23.7% | 20.2% | 4.7% | 12.2% | 9.8% |
| Both Genders | ||||||
| Cancer | 1348.6 | 2331.8 | ||||
| Cardiovascular conditions | −573.8 | 394.2 | 1062.7 | −1717.6 | −442.0 | 1127.2 |
| Ischaemic heart disease | −1303.0 | −335.1 | 333.4 | −2581.6 | −1306.0 | 263.2 |
| Diabetes | −126.4 | −458.8 | ||||
| Digestive conditions | 895.4 | 1949.4 | ||||
| Infectious diseases | 159.6 | 348.3 | ||||
| Neuropsychiatric conditions | 302.2 | 944.3 | ||||
| Injuries | 927.5 | 1781.9 | ||||
| Grand Total | 2933.1 | 3901.0 | 4569.5 | 5179.2 | 6454.9 | 8024.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sherk, A.; Gilmore, W.; Churchill, S.; Lensvelt, E.; Stockwell, T.; Chikritzhs, T. Implications of Cardioprotective Assumptions for National Drinking Guidelines and Alcohol Harm Monitoring Systems. Int. J. Environ. Res. Public Health 2019, 16, 4956. https://doi.org/10.3390/ijerph16244956
Sherk A, Gilmore W, Churchill S, Lensvelt E, Stockwell T, Chikritzhs T. Implications of Cardioprotective Assumptions for National Drinking Guidelines and Alcohol Harm Monitoring Systems. International Journal of Environmental Research and Public Health. 2019; 16(24):4956. https://doi.org/10.3390/ijerph16244956
Chicago/Turabian StyleSherk, Adam, William Gilmore, Samuel Churchill, Eveline Lensvelt, Tim Stockwell, and Tanya Chikritzhs. 2019. "Implications of Cardioprotective Assumptions for National Drinking Guidelines and Alcohol Harm Monitoring Systems" International Journal of Environmental Research and Public Health 16, no. 24: 4956. https://doi.org/10.3390/ijerph16244956





