Knowledge about the Care of People with Alzheimer’s Disease of the Nursing Staff of Nursing Homes in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Study Population and Sample
2.3. Variables and Instruments
- Socio-demographic variables: gender, age, and experience
- Education and training: attendance at courses and conferences
2.4. Data Collection
2.5. Data Analysis
3. Results
3.1. Study Sample Characteristics
3.2. Knowledge about Alzheimer’s Disease
3.3. Factors Associated with Knowledge about Alzheimer’s Care
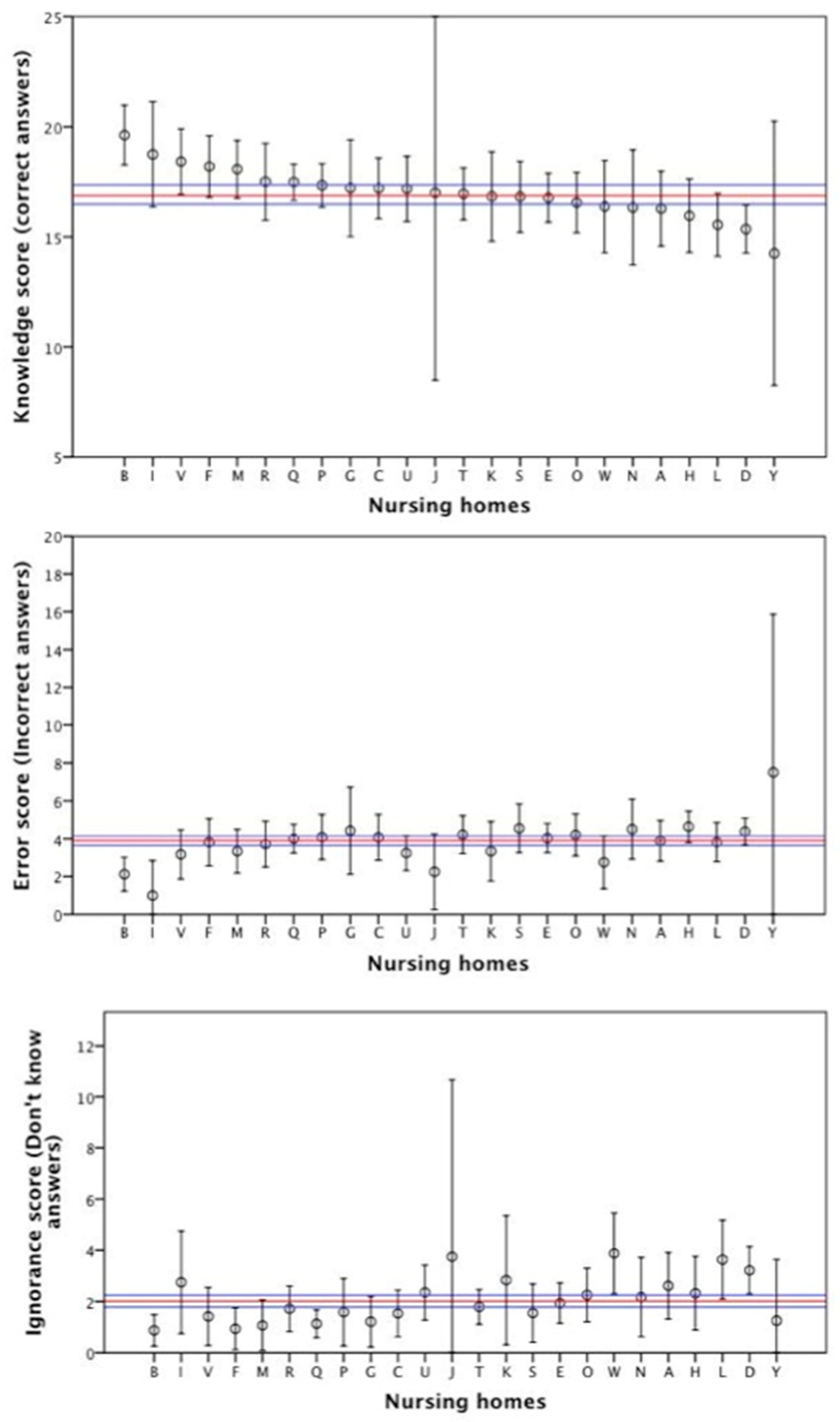
3.4. Knowledge about AD Care at Nursing Home Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. 10 Facts on Ageing and Health. 2017. Available online: https://www.who.int/features/factfiles/ageing/en/ (accessed on 10 June 2019).
- Winblad, B.; Amouyel, P.; Andrieu, S.; Ballard, C.; Brayne, C.; Brodaty, H. Defeating Alzheimer’s disease and other dementias: A priority for European science and society. Lancet Neurol. 2016, 15, 455–532. [Google Scholar] [CrossRef]
- Qiu, C.; De Ronchi, D.; Fratiglioni, L. The epidemiology of the dementias: An update. Curr. Opin. Psychiatry 2007, 20, 380. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Dementia. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 17 July 2019).
- de Pedro-Cuesta, J.; Virues-Ortega, J.; Vega, S.; Seijo-Martinez, M.; Saz, P.; Rodriguez, F. Prevalence of dementia and major dementia subtypes in Spanish populations: A reanalysis of dementia prevalence surveys, 1990−2008. BMC Neurol. 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- de Hoyos-Alonso, M.; Bonis, J.; Tapias-Merino, E.; Castell, M.; Otero, A. Estimated prevalence of dementia based on analysis of drug databases in the region of Madrid (Spain). Neurología 2016, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Molinuevo, J.; Peña-Casanova, J. Guía Oficial para la Práctica Clínica en Demencias: Conceptos, Criterios y Recomendaciones 2009; Thomson Reuters: Barcelona, Spain, 2009. [Google Scholar]
- Rist, P.M.; Nguyen, T.T.; Whitmer, R.A.; Glymour, M.M. Modifiable risk factors for nursing home admission among individuals with high and low dementia risk. Arch. Gerontol. Geriatr. 2016, 65, 140–145. [Google Scholar] [CrossRef]
- Mongil, R.L.; Trigo, J.A.L.; Sanz, F.J.C.; Gómez, S.T.; Colombo, T.L.; Grupo de Trabajo de Atención Sanitaria. Prevalencia de demencia en pacientes institucionalizados: Estudio Resydem. Rev. Esp. Geriatr. Gerontol. 2009, 44, 5–11. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Yu, F.; Davila, H.W.; Shippee, T. Alzheimer’s disease and nursing homes. Health Aff. 2014, 33, 650–657. [Google Scholar] [CrossRef]
- Spilsbury, K.; Hewitt, C.; Stirk, L.; Bowman, C. The relationship between nurse staffing and quality of care in nursing homes: A systematic review. Int. J. Nurs. Stud. 2011, 48, 732–750. [Google Scholar] [CrossRef]
- Smyth, W.; Fielding, E.; Beattie, E.; Gardner, A.; Moyle, W.; Franklin, S. A survey-based study of knowledge of Alzheimer’s disease among health care staff. BMC Geriatr. 2013, 13. [Google Scholar] [CrossRef]
- Annear, M.J.; Toye, C.M.; Eccleston, C.E.; McInerney, F.J.; Elliott, K.J.; Tranter, B.K. Dementia Knowledge Assessment Scale: Development and preliminary psychometric properties. J. Am. Geriatr. Soc. 2015, 63, 2375–2381. [Google Scholar] [CrossRef]
- Carpenter, B.D.; Balsis, S.; Otilingam, P.G.; Hanson, P.K.; Gatz, M. The Alzheimer’s disease knowledge scale: Development and psychometric properties. Gerontologist 2009, 49, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Spector, A.; Orrell, M.; Schepers, A.; Shanahan, N. A systematic review of ‘knowledge of dementia’ outcome measures. Ageing Res. Rev. 2012, 11, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Peterson, D.; Berg-Weger, M.; McGillick, J.; Schwartz, L. Basic Care I: The effect of dementia-specific training on certified nursing assistants and other staff. Am. J. Alzheimers Dis. Other Demenc. 2002, 17, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.J.; Haley, W.E.; Harrell, L.E.; Powers, R.E. Knowledge about Alzheimer disease among primary care physicians, psychologists, nurses, and social workers. Alzheimer Dis. Assoc. Dis. 1997, 11, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Annear, M.J.; Toye, C.; Elliott, K.J.; McInerney, F.; Eccleston, C.; Robinson, A. Dementia knowledge assessment scale (DKAS): Confirmatory factor analysis and comparative subscale scores among an international cohort. BMC Geriatr. 2017, 17. [Google Scholar] [CrossRef]
- Moyle, W.; Borbasi, S.; Wallis, M.; Olorenshaw, R.; Gracia, N. Acute care management of older people with dementia: A qualitative perspective. J. Clin. Nurs. 2011, 20, 420–428. [Google Scholar] [CrossRef]
- Forsetlund, L.; Bjørndal, A.; Rashidian, A.; Jamtvedt, G.; O’Brien, M.; Wolf, F.M. Continuing education meetings and workshops: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2009, 15. [Google Scholar] [CrossRef]
- Hughes, J.; Bagley, H.; Reilly, S.; Burns, A.; Challis, D. Care staff working with people with dementia: Training, knowledge and confidence. Dementia 2008, 7, 227–238. [Google Scholar] [CrossRef]
- Poltroniere, S.; Cecchetto, F.H.; de Souza, E.N. Doença de Alzheimer e demandas de cuidados: O que os enfermeiros sabem. Rev. Gaúcha Enferm 2011, 32, 270–278. [Google Scholar] [CrossRef][Green Version]
- Robinson, A.; Eccleston, C.; Annear, M.; Elliott, K.; Andrews, S.; Stirling, C. Who knows, who cares? Dementia knowledge among nurses, care workers, and family members of people living with dementia. J. Palliat. Care 2014, 30, 158–165. [Google Scholar] [CrossRef]
- STROBE Statement. Strengthening the Reporting of Observational Studies in Epidemiology. Available online: https://www.strobe-statement.org/index.php?id=strobe-home (accessed on 5 September 2019).
- Parra-Anguita, L.; Sánchez-García, I.; del Pino-Casado, R.; Pancorbo-Hidalgo, P.L. Measuring knowledge of Alzheimer’s: Development and psychometric testing of the UJA Alzheimer’s Care Scale. BMC Geriatr. 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Parra-Anguita, L.; Moreno Cámara, S.; López-Franco, M.D.; Pancorbo-Hidalgo, P.L. Validation of the Spanish Version of the Dementia Knowledge Assessment Tool 2. J. Alzheimers Dis. 2018, 65, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Toye, C.; Lester, L.; Popescu, A.; McInerney, F.; Andrews, S.; Robinson, A.L. Dementia Knowledge Assessment Tool Version Two: Development of a tool to inform preparation for care planning and delivery in families and care staff. Dementia 2014, 13, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Annear, M.J.; Eccleston, C.E.; McInerney, F.J.; Elliott, K.J.; Toye, C.M.; Tranter, B.K. A new standard in dementia knowledge measurement: Comparative validation of the Dementia Knowledge Assessment Scale and the Alzheimer’s Disease Knowledge Scale. J. Am. Geriatr. Soc. 2016, 64, 1329–1334. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Hu, X.; Li, Y.; Zhen, X.; Gu, Y.; Sun, X. The quality of caregivers for the elderly in long-term care institutions in Zhejiang Province, China. Int. J. Environ. Res. Public Health 2019, 16, 2164. [Google Scholar] [CrossRef]
- Evripidou, M.; Charalambous, A.; Middleton, N.; Papastavrou, E. Nurses’ knowledge and attitudes about dementia care: Systematic literature review. Perspect. Psychiatr. Care 2019, 55, 48–60. [Google Scholar] [CrossRef]
- Zwakhalen, S.M.; Hamers, J.P.; Peijnenburg, R.H.; Berger, M.P. Nursing staff knowledge and beliefs about pain in elderly nursing home residents with dementia. Pain Res. Manag. 2007, 12, 177–184. [Google Scholar] [CrossRef]
- Low, L.; Fletcher, J.; Goodenough, B.; Jeon, Y.; Etherton-Beer, C.; MacAndrew, M. A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLoS ONE 2015, 10, e0140711. [Google Scholar] [CrossRef]
- Schütze, H.; Shell, A.; Brodaty, H. Development, implementation and evaluation of Australia’s first national continuing medical education program for the timely diagnosis and management of dementia in general practice. BMC Med. Educ. 2018, 18. [Google Scholar] [CrossRef]
- Jennings, A.; McLoughlin, K.; Boyle, S.; Thackeray, K.; Quinn, A.; O’Sullivan, T. Development and evaluation of a primary care interprofessional education intervention to support people with dementia. J. Interprof. Care 2018, 33, 579–582. [Google Scholar] [CrossRef]
- Matsuda, Y.; Hashimoto, R.; Takemoto, S.; Yoshioka, Y.; Uehara, T.; Kawasaki, Y. Educational benefits for nurses and nursing students of the dementia supporter training program in Japan. PLoS ONE 2018, 13, e0200586. [Google Scholar] [CrossRef] [PubMed]
| Variables | Frequency (%) | |
|---|---|---|
| RNs (n = 69) | ANs and EWs * (n = 292) | |
| Age; mean (SD) | 33.21 (8.78) | 38.87 (10.31) |
| Gender | ||
| Female | 65 (94.2%) | 275 (94.2%) |
| Male | 4 (5.8%) | 15 (5.1%) |
| Work experience (years) | ||
| <5 | 25 (36.2%) | 111 (38%) |
| 5–15 | 26 (37.7%) | 149 (51%) |
| >15 | 18 (26.1%) | 31 (10.6%) |
| Attendance at courses on dementia (any time) | ||
| Yes | 61 (88.4%) | 227 (77.7%) |
| No | 8 (11.6%) | 64 (21.9%) |
| Attendance at courses on dementia (last 3 years) | ||
| Yes | 31 (44.9%) | 106 (36.3%) |
| No | 21 (30.4%) | 87 (29.8%) |
| Attendance at conferences or meetings (any time) | ||
| Yes | 27 (39.1%) | 79 (27.1%) |
| No | 42 (60.9%) | 203 (69.5%) |
| Scores | Mean (SD); CI 95% | |
|---|---|---|
| RNs (n = 69) | ANs and EWs * (n = 292) | |
| Knowledge score | 19.16 (2.48); 18.56–19.76 | 16.46 (2.91); 16.08–16.76 |
| Error score | 2.65 (1.95); 2.18–3.12 | 4.19 (2.32); 3.92–4.46 |
| Don’t know score | 0.99 (1.54); 0.61–1.36 | 2.25 (2.28); 1.98–2.51 |
| UJA Alzheimer’s Care Scale | RNs | ANs and EWs | ||||
|---|---|---|---|---|---|---|
| Correct | Errors | “Don’t Know” | Correct | Errors | “Don’t Know” | |
| 9 a. The application of mechanical restraints, type and date of application, reason, care provided and informed consent should be recorded in the patient medical record. | 100% | 93.5% | 3.1% | 3.4% | ||
| 14. Inform the carer about the disease and its possible complications, and the social resources and support systems available. | 100% | 92.1% | 5.8% | 1.4% | ||
| 10. Palliative care must include psychosocial, spiritual, cultural and family support aspects. | 98.6% | 1.4% | 89% | 6.5% | 4.5% | |
| 16. Identify who is the patient’s representative to include him or her in decision-making and care planning. | 98.6% | 92.1% | 5.8% | 2.1% | ||
| 21. Record in the patient medical record data on the form of onset, progression, psychological and behavioral symptoms. | 97.1% | 2.9% | 91.4% | 5.5% | 3.1% | |
| 5. Non-pharmacological and pharmacological measures should be used together to manage the different behavioral and psychological symptoms of dementia. | 95.7% | 2.9% | 1.4% | 78.1% | 7.9% | 13% |
| 22. Care plans should address activities of daily living to maximize independent activity, maintain function, and adapt and develop skills. | 95.7% | 2.9% | 1.4% | 93.5% | 1.7% | 4.1% |
| 6. Reporting the existence or suspicion of abuse is not a matter for nurses or elderly care workers, but for other professionals. | 94.2% | 2.9% | 1.4% | 68.8% | 27.1% | 3.8% |
| 19. Provide comprehensive care to the carer, including counselling and emotional support. | 94.2% | 1.4% | 2.9% | 92.5% | 3.4% | 3.8% |
| 17. Carers should be informed and trained to prevent the onset of behavioral and psychological symptoms of dementia. | 89.9% | 5.8% | 1.4% | 88.7% | 7.9% | 3.1% |
| 7. The management of extreme agitation, violence and aggressiveness must take place in a safe, low-stimulation environment, separate from other users of the service. | 87% | 5.8% | 5.8% | 78.4% | 15.4% | 5.1% |
| 11. Conduct long-term physical activity programs to maintain the functional capacity of institutionalized dementia patients. | 87% | 7.2% | 2.9% | 87.7% | 6.2% | 5.5% |
| 4. Provide a normal diet, while assessing the causes of dysphagia. | 81.2% | 10.1% | 8.7% | 68.8% | 20.5% | 10.3% |
| 2. The Zarit scale is used to quantify the carer’s burden. | 78.3% | 5.8% | 14.5% | 31.5% | 9.6% | 55.8% |
| 12. Use the oral route for fluid supply at the end of life, whenever possible. | 76.8% | 18.8% | 4.3% | 83.2% | 11.3% | 4.8% |
| 15. Behavior modification, programmed hygiene and induced micturition increase urinary incontinence in patients with dementia. | 76.8% | 15.9% | 7.2% | 44.5% | 39.4% | 15.1% |
| 1. If needed, mechanical restraints can be used as a substitute for surveillance or for the convenience of professionals. | 79.3% | 21.7% | 4.3% | 63.7% | 30.1% | 5.5% |
| 20. Intervention programs in activities of daily living do not reduce the carer’s burden in the medium term. | 73.9% | 17.4% | 7.2% | 52.1% | 31.8% | 15.8% |
| 3. When families cannot guarantee care for people with dementia, admission to a facility may avoid social isolation and prevent abuse. | 72.5% | 20.3% | 4.3% | 70.9% | 25.7% | 2.7% |
| 18. Advise the person with dementia to prepare a living will document in the early stages of the disease. | 71% | 17.4% | 11.6% | 54.8% | 23.3% | 21.2% |
| 13. Informing family and carers of the near death status does not improve care in the last few days. | 66.7% | 27.5% | 4.3% | 53.1% | 39.7% | 6.5% |
| 8. Specific drugs are the first option for treatment of psychological and behavioral disorders. | 53.6% | 39.1% | 7.2% | 44.2% | 37% | 17.5% |
| 23. Use nasogastric tube or percutaneous gastrostomy in patients with advanced dementia as a regular feeding route, if dysphagia present. | 53.6% | 7.7% | 7.2% | 28.8% | 54.8% | 16.1% |
| Variables | RNs (n = 69) | ANs and EWs * (n = 292) | ||
|---|---|---|---|---|
| Score Mean (SD) | p-Value 1 | Score Mean (SD) | p-Value | |
| Gender | ||||
| Female | 19.14 (2.55) | 0.779 | 16.48 (2.95) | 0.141 |
| Male | 19.50 (1.0) | 15.33 (2.19) | ||
| Work experience (years) | ||||
| <5 | 18.00 (2.65) | 0.006 2 | 16.19 (3.09) | 0.455 |
| 5–14.9 | 19.46 (2.16) | 16.51 (2.79) | ||
| 15 years or more | 20.33 (2.09) | 16.87 (2.93) | ||
| Attendance at courses on dementia (any time) | ||||
| Yes | 19.41 (2.39) | 0.02 | 16.64 (2.86) | 0.01 |
| No | 17.25 (2.49) | 15.63 (3.01) | ||
| Attendance at courses on dementia (last 3 years) | ||||
| Yes | 19.84 (1.98) | 0.039 | 17.22 (2.61) | <0.0001 |
| No | 18.61 (2.73) | 15.96 (2.99) | ||
| Attendance at conferences or meetings (any time) | ||||
| Yes | 19.59 (2.41) | 0.248 | 17.08 (2.19) | 0.01 |
| No | 18.88 (2.52) | 16.47 (3.12) | ||
| Variables | Nursing Homes Number (%) 5 | Knowledge Score; Mean (SD) | p-Value |
|---|---|---|---|
| Number of residents | |||
| Up to 100 | 15 (62.5%) | 17.16 (2.85) | 0.19 |
| More than 100 | 8 (33.3%) | 16.73 (3.22) | |
| Staff experience 1 | |||
| 1 Very low | 4 (16.7%) | 15.53 (3.10) | 0.001 2 |
| 2 Low– | 8 (33.3%) | 17.42 (2.88) | |
| 3 Medium | 9 (37.5%) | 16.93 (2.87) | |
| 4 High | 3 (12.5%) | 17.43 (3.50) | |
| Percentage of staff that have attended dementia courses in last 3 years 3 | |||
| 1 Low | 9 (37.5%) | 16.39 (3.11) | 0.002 4 |
| 2 Medium | 13 (54.2%) | 17.07 (2.93) | |
| 3 High | 2 (8.3%) | 18.73 (2.90) | |
| Ratio of residents per staff member | |||
| Low (Up to 2.90) | 10 (41.7%) | 16.71 (3.11) | 0.19 |
| High (2.91 or more) | 9 (37.5%) | 17.18 (3.07) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parra-Anguita, L.; García-Fernández, F.P.; del-Pino-Casado, R.; Pancorbo-Hidalgo, P.L. Knowledge about the Care of People with Alzheimer’s Disease of the Nursing Staff of Nursing Homes in Spain. Int. J. Environ. Res. Public Health 2019, 16, 4907. https://doi.org/10.3390/ijerph16244907
Parra-Anguita L, García-Fernández FP, del-Pino-Casado R, Pancorbo-Hidalgo PL. Knowledge about the Care of People with Alzheimer’s Disease of the Nursing Staff of Nursing Homes in Spain. International Journal of Environmental Research and Public Health. 2019; 16(24):4907. https://doi.org/10.3390/ijerph16244907
Chicago/Turabian StyleParra-Anguita, Laura, Francisco P. García-Fernández, Rafael del-Pino-Casado, and Pedro L. Pancorbo-Hidalgo. 2019. "Knowledge about the Care of People with Alzheimer’s Disease of the Nursing Staff of Nursing Homes in Spain" International Journal of Environmental Research and Public Health 16, no. 24: 4907. https://doi.org/10.3390/ijerph16244907
APA StyleParra-Anguita, L., García-Fernández, F. P., del-Pino-Casado, R., & Pancorbo-Hidalgo, P. L. (2019). Knowledge about the Care of People with Alzheimer’s Disease of the Nursing Staff of Nursing Homes in Spain. International Journal of Environmental Research and Public Health, 16(24), 4907. https://doi.org/10.3390/ijerph16244907





