Exit and Entry Screening Practices for Infectious Diseases among Travelers at Points of Entry: Looking for Evidence on Public Health Impact
Abstract
1. Introduction
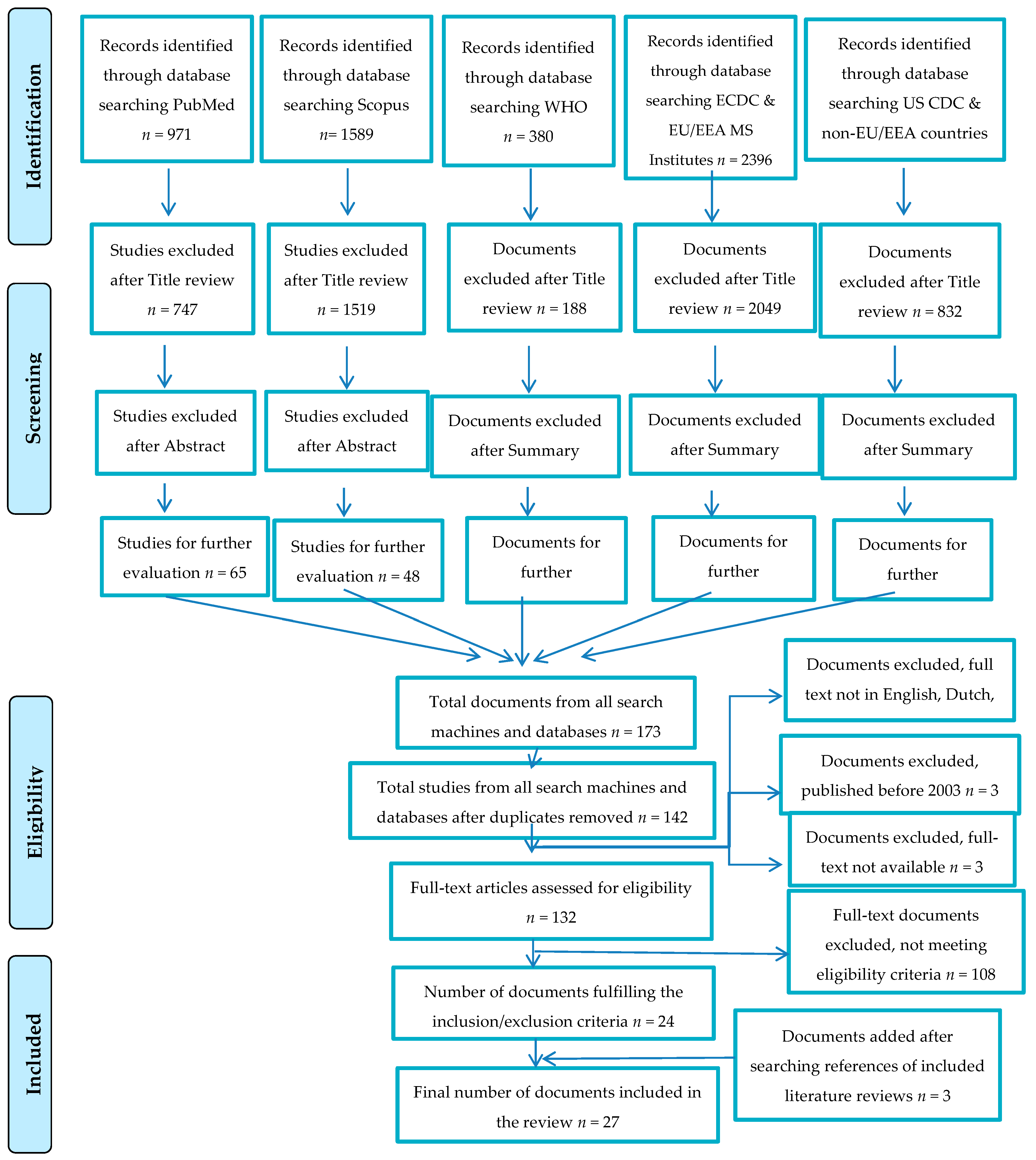
2. Materials and Methods
2.1. Methods for Scoping Search
2.1.1. Research Question
2.1.2. Search Strategy
2.1.3. Inclusion and Exclusion Criteria
2.2. Methods for Systematic Bibliographic Review
2.2.1. Research Questions
2.2.2. Specific Objectives
2.2.3. Search Strategy
2.2.4. Inclusion and Exclusion Criteria
2.2.5. Analysis of the Literature
- Type of screening (entry, exit)
- Types of infectious disease or diseases that entry and exit screening was targeting
- Type of points of entry: airports, ports, ground crossings
- Screening carried out on a routine basis or on an ad hoc basis after a public health event has occurred
- Methods used in entry/exit screening (primary, secondary, questionnaire, body temperature, technology used etc.)
- Type of technology used (thermometers, scan cameras etc.)
- After screening, the applied diagnosis protocol (laboratory and clinical examination)
- Number of cases identified and the total numbers of travelers screened
- Percentage of persons positive to screening finally diagnosed
- Percentage of persons diagnosed with a different disease from the initially targeted
- The applied protocol for diagnosis and management of cases
- Health measures applied to the traveler and the environment
- General screening or targeted screening: outbound country, travelers directly arriving from affected countries, nationality, travelers in-transit
- Inter-sectorial collaboration and coordination processes
- Involved officers: public health officers, ministry officers, regional health system, national health system, NGOs, else
- Concrete example of entry/exit screening
- Practices, experiences, and lessons learnt reported
- Challenges reported (limitations, failures, mishaps)
- Bad practices reported
- Methods used to assess the public health impact of the entry/exit screening and their result
- Methods used to appraise the cost-effectiveness of screening method and results
- Evaluation of method results: sensitivity, specificity, false positive/negative (of screening method), positive and negative predictive values
- Decision-making level: public health officers, ministry officers, regional, national, intersectoral collaboration, health, and border authorities
- Communication channels
- Notification practices between neighboring and possibly affected countries
- Specific timeframe referred and duration
2.2.6. Ethical Considerations
3. Results
3.1. Results of Scoping Search
- (a)
- Assessment for imported cases notification of infectious diseases
- (b)
- Dengue entry screening at airports
- (c)
- Preparedness and response planning for Ebola Virus Disease
- (d)
- Entry/exit screening measures for Ebola Virus Disease experience
- (e)
- Studies about evolution and predictions of Ebola Virus Disease spread
- (f)
- Entry/exit screening measures for infectious diseases
- (g)
- Influenza
- (h)
- Pandemic influenza preparedness
- (i)
- International air travel and infectious diseases
- (j)
- Preparedness planning for infectious disease
- (k)
- Screening measures at ground crossing
- (l)
- Sever Acute Respiratory Syndrome
- (m)
- Zika Virus Disease
| Degree of Success in Identifying Ill or Exposed Travelers | Limitations | Concomitant Effects | |
|---|---|---|---|
| Beneficial | Adverse | ||
| Influenza A(H1N1)pdm09˅ [20,21] Sensitivity: 6.67% (95% CI, 1.40%–18.27%) Specificity: 99.10% (95% CI, 99.00%–100.00%) EVD ˄ [22] Sensitivity: 0% Specificity: 99.79% SARS ˅ [8,9,13,23] Entry screening measures did not detect any confirmed SARS cases in Australia, Canada, and Singapore. | Influenza A(H1N1)pdm09
| Influenza A(H1N1)pdm09 and EVD
EVD
SARS | EVD
|
3.2. Results of Systematic Bibliographic Review
3.2.1. Entry and Exit Screening Measures in the Different Types of Point of Entry
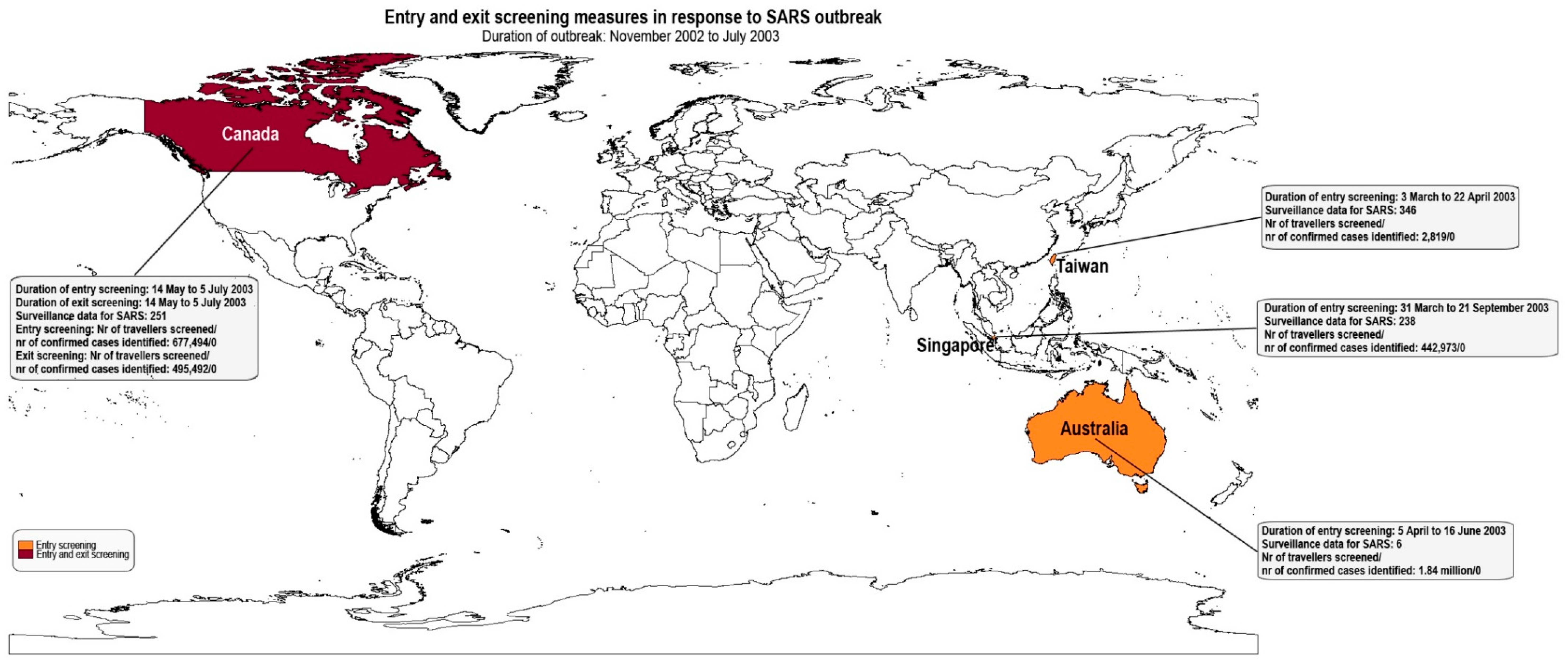
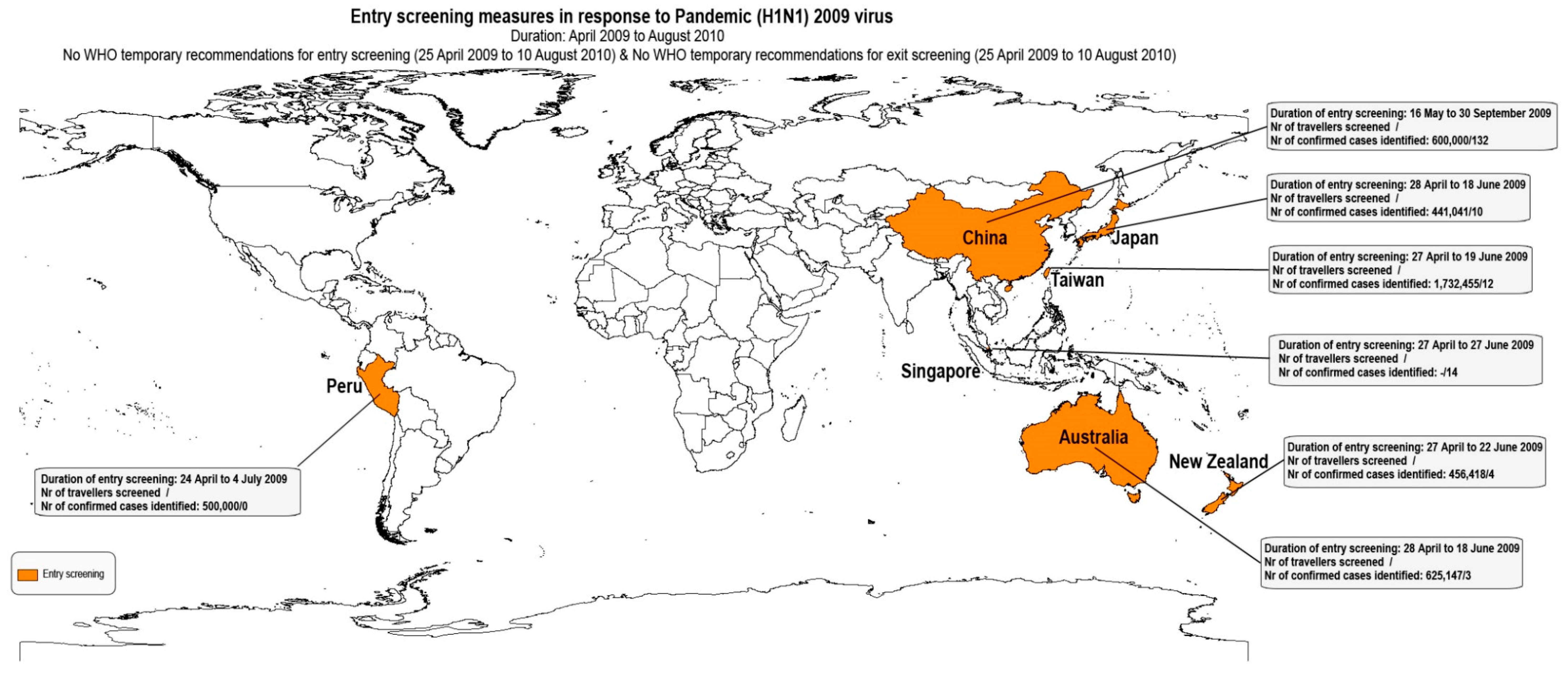
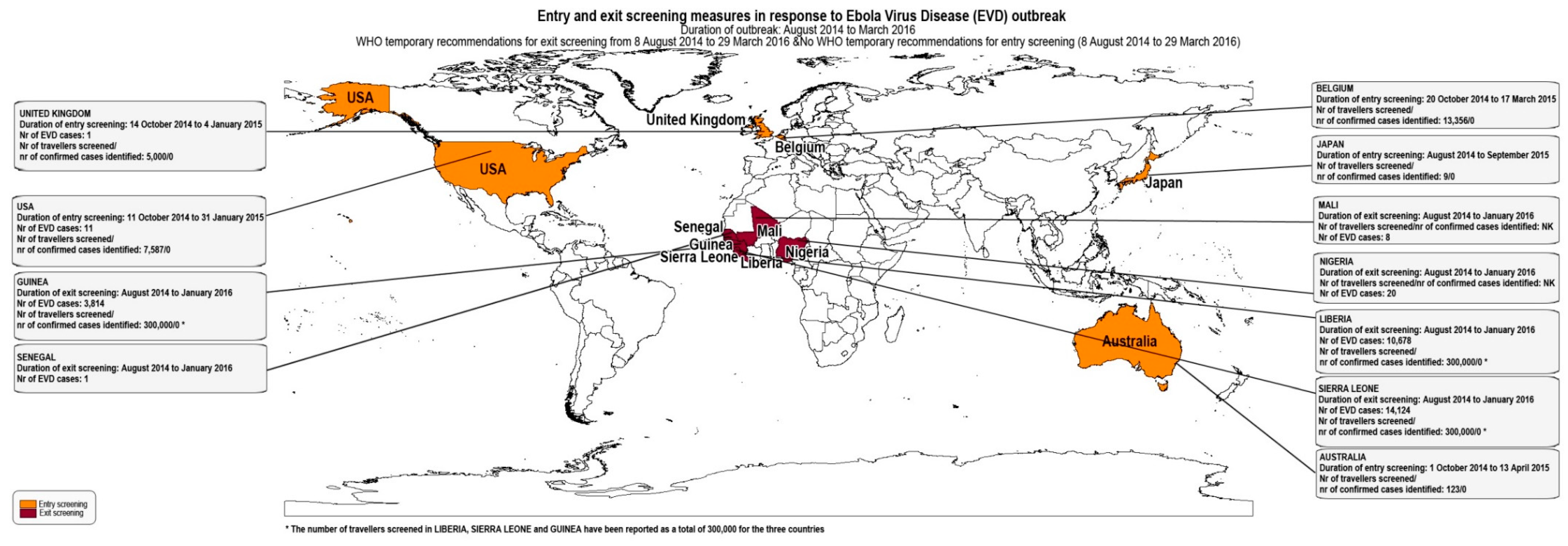
3.2.2. Timeframes of Public Health Events and Screening Measure implementation
3.2.3. Screening Measures on an Ad hoc Basis and as a Routine Measure
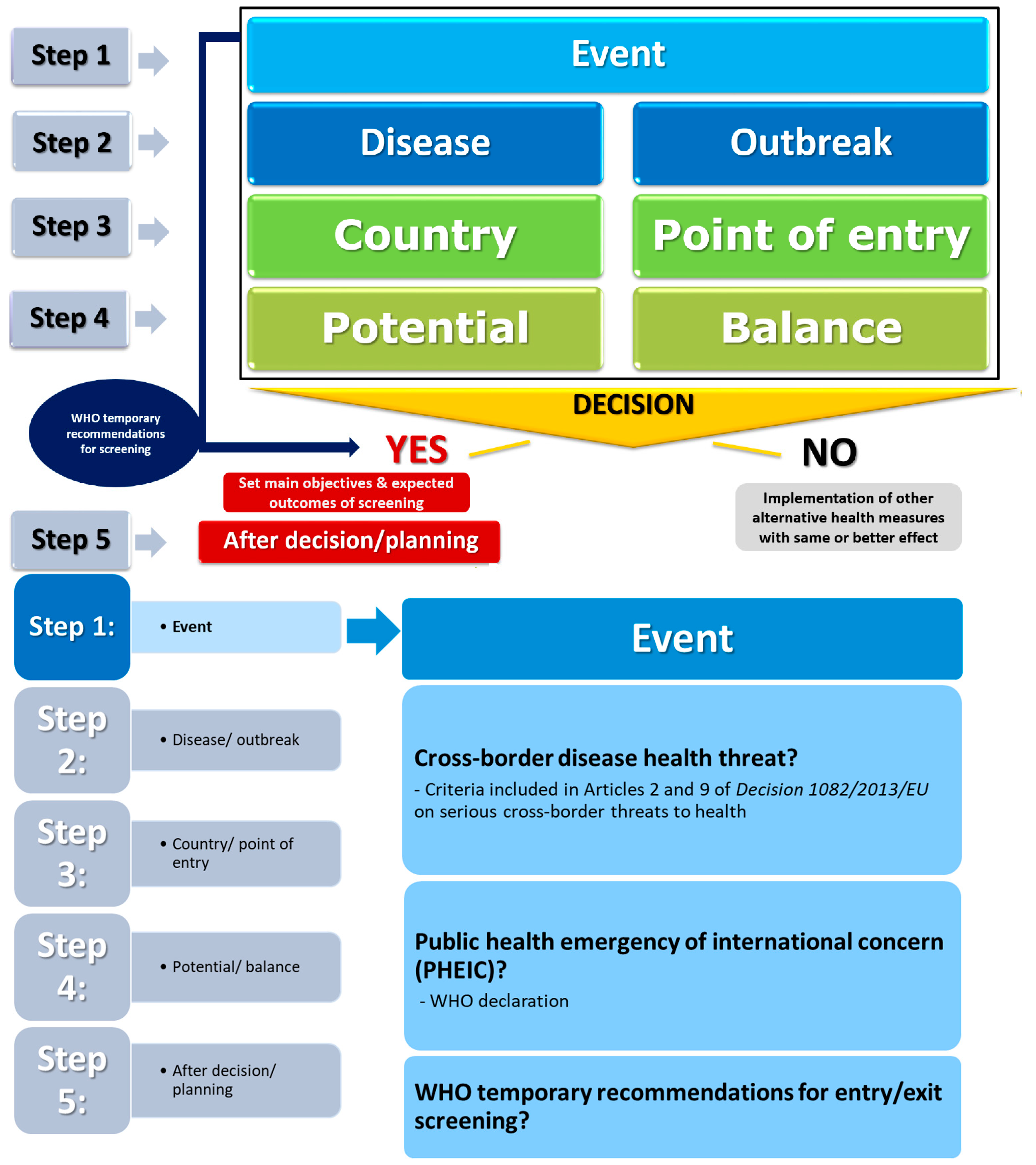
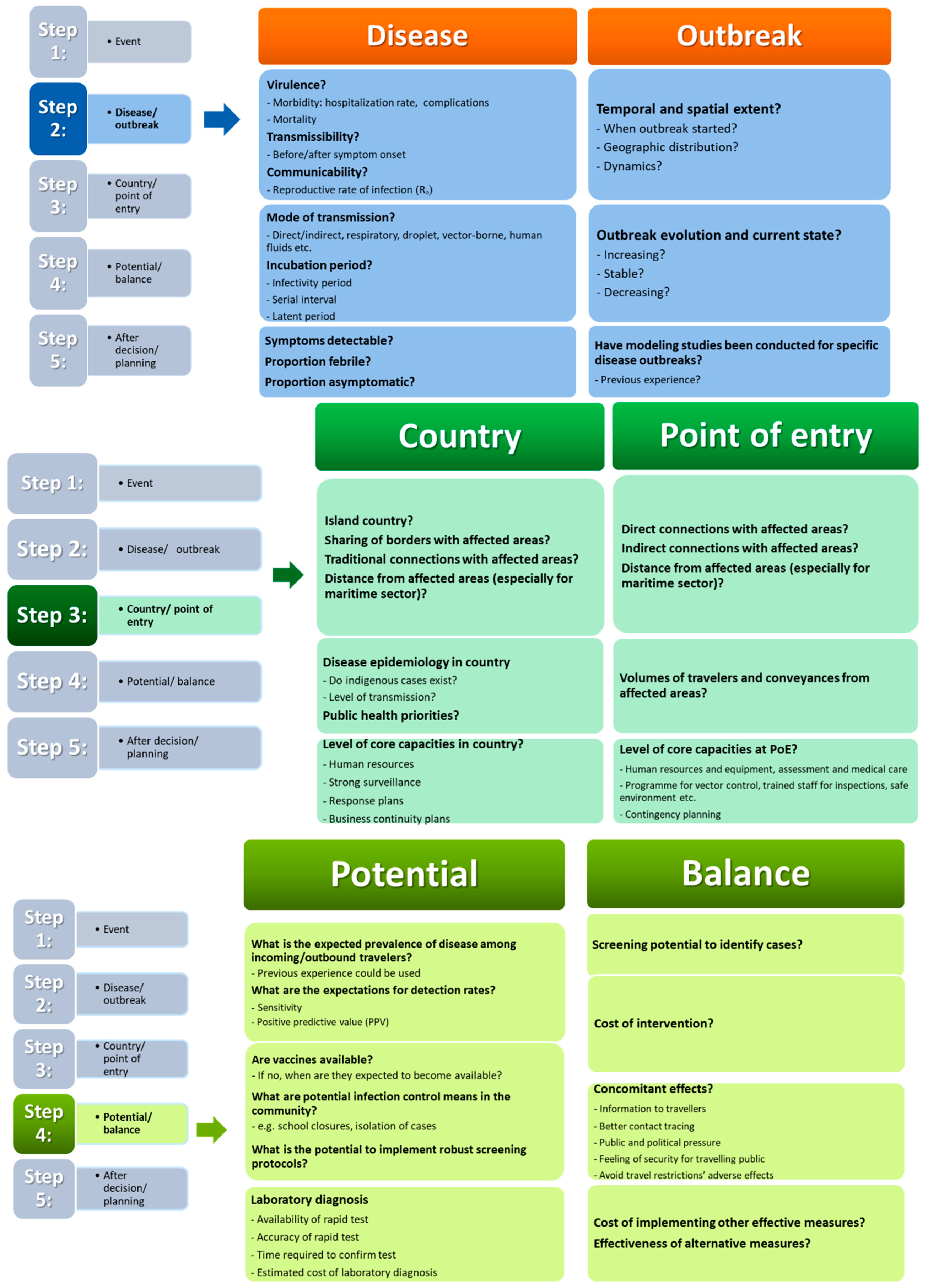
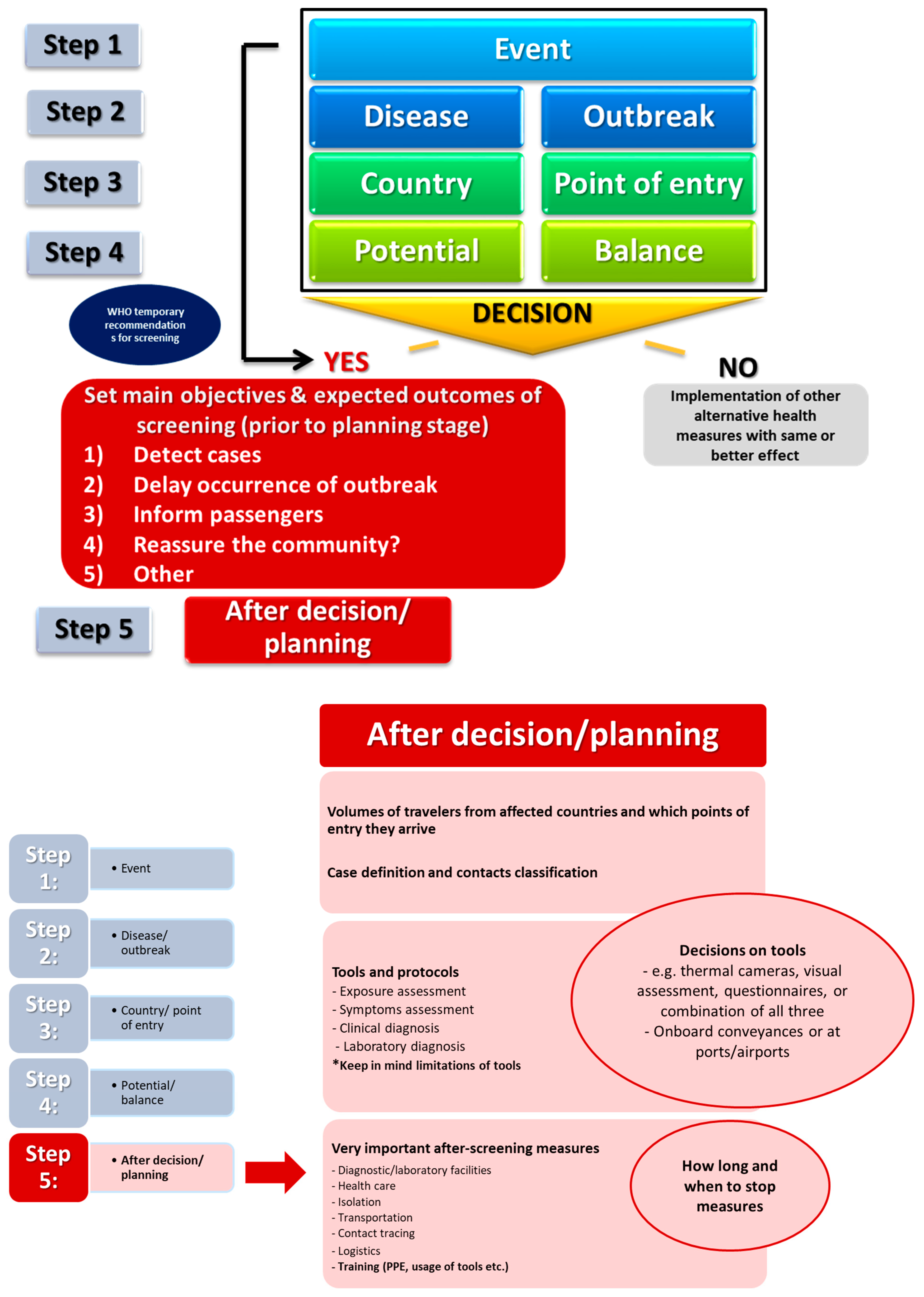
3.2.4. Decision-Making
3.2.5. Authorities Involved in Implementing Entry/Exit Screening Measures
3.2.6. Contact Tracing, Data Management, and Communication Flows
3.2.7. Screening Protocols and Accompanying Measures
3.2.8. Technology for Body Temperature Measurement
3.2.9. Appraisal of Impact of Entry and Exit Screening Measures Based on Case Identification
3.2.10. Management of Suspected Cases
3.2.11. Limitations of Screening Measures and Challenges Reported
4. Discussion
4.1. Impact of Exit Screening Measures at Airports, Ports, and Ground Crossings
4.2. Impact of Entry Screening Measures
4.3. Cost-Effectiveness of Screening Measures
4.4. Decision-Making
4.5. Modeling
4.6. Resources and Logistics
4.7. Limitations of the Bibliographic Review
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
Appendix B. Questionnaire for Checking on Eligibility Criteria
- a.
- Type of screening (entry, exit) Yes ☐ No ☐
- b.
- Types of infectious disease or diseases that entry and exit screening was targeting Yes ☐ No ☐
- c.
- Type of points of entry (airports, ports, ground crossings) where measures were implemented Yes ☐ No ☐
- d.
- Screening carried out on a routine basis or on an ad hoc basis after a public health event has occurred and its purpose Yes ☐ No ☐
- e.
- Description of methods used in entry/exit screening (primary/secondary, questionnaire, body temperature check, technology used) Yes ☐ No ☐
- f.
- Type of technology used (thermometers, scan cameras, or other technology)
- g.
- After screening, the applied diagnosis protocol (laboratory and clinical examination)
- h.
- Number of cases identified for a specific timeframe Yes ☐ No ☐
- i.
- Total numbers of travelers screened for a specific timeframe Yes ☐ No ☐
- j.
- Percentage of persons positive to screening that were diagnosed with the targeted disease Yes ☐ No ☐
- k.
- Percentage of persons diagnosed with different disease from the initially targeted for the specific timeframe (positive and negative predictive values) Yes ☐ No ☐
- l.
- General screening or targeted screening (e.g., traveler from any affected outbound country, all travelers directly arriving only from affected countries/areas, nationality of travelers, travelers in-transit that have called an affected country/areas (West Africa)) Yes ☐ No ☐
- m.
- Reporting on the assessment of the public health impact of the entry/exit screening measures or the cost-effectiveness of methods applied
Appendix C. Questionnaire for Data Extraction
- Type of screening: entry ☐ exit ☐
- Types of infectious disease or diseases that entry and exit screening was targeting
- Type of points of entry: airports ☐ ports ☐ ground crossings ☐
- Screening carried out on a routine basis ☐ or on an ad hoc basis ☐ after a public health event has occurred
- Methods used in entry/exit screening: primary ☐ secondary ☐ questionnaire ☐ body temperature ☐ technology used ☐ else
- Type of technology used: thermometers scan cameras
- After screening, the applied diagnosis protocol (laboratory and clinical examination)
- Number of cases identified and the total numbers of travelers screened
- Percentage of persons positive to screening finally diagnosed
- Percentage of persons diagnosed with different disease from the initially targeted
- The applied protocol after diagnosis and management of cases
- Health measures applied to the traveler and the environment
- General screening or targeted screening: outbound country ☐ travelers directly arriving from affected countries ☐ nationality ☐ travelers in-transit ☐
- Inter-sectorial collaboration and coordination processes
- Involved officers: Public health officers ☐ ministry officers ☐ regional health system ☐ national health system ☐ NGOs ☐ else ☐
- Concrete example of entry/exit screening
- Practices, experiences, and lessons learnt reported
- Challenges reported (limitations, failures, mishaps)
- Bad practices reported
- Methods used to assess the public health impact of the entry/exit screening and their result
- Methods used to appraise the cost-effectiveness of screening method and results
- Evaluation of method results: sensitivity ☐ specificity ☐ false positive/negative ☐ (of screening method) ☐ positive and negative predictive values
- Decision-making level: Public health officers ☐ ministry officers ☐ regional ☐ national ☐ intersectoral collaboration ☐ health and border authorities ☐
- Communication channels
- Notification practices between neighboring and possibly affected countries
- Specific timeframe referred Yes ☐ No ☐ Duration:
Appendix D. List of Publications Identified through the Scoping Search
Appendix E
Appendix F
| Public Health Event | WHO Statement/Date | |
|---|---|---|
| Title | Started/Ended | |
| Ebola Virus Disease outbreak in West Africa | 8 Aug 2014/29 Mar 2016 | Statement on the 1st/8 Aug 2014 Statement on the 2nd meeting/22 September 2014 Statement on the 3rd meeting/23 October 2014 Statement on the 4th meeting/21 January 2015 Statement on the 5th meeting/10 April 2015 Statement on the 6th meeting/7 July 2015 Statement on the 7th meeting/5 October 2015 Statement on the 8th meeting/18 December 2015 Statement on the 9th meeting/29 March 2016 |
| Poliovirus | 5 May 2014/15 Aug 2018 | Statement on the 3rd meeting/14 November 2014 Statement on the 6th meeting/17 August 2015 Statement on the 7th meeting/26 November 2015 Statement on the 8th meeting/1 March 2016 Statement on the 9th meeting/20 May 2016 Statement on the 10th meeting/22 August 2016 Statement on the 11th meeting/11 November 2016 Statement on the 12th meeting/13 February 2017 Statement on the 13th meeting/2 May 2017 Statement on the 14th meeting/3 August 2017 Statement on the 15th meeting/14 November 2017 Statement on the 16th meeting/14 February 2018 Statement on the 17th meeting/10 May 2018 Statement on the 18th meeting/15 Aug 2018 Statement on the 19th meeting/30 Nov 2018 |
| Ebola outbreak in DRC | 10 May 2018/25 July 2018 | Statement on the 1st meeting/18 May 2018 External situation report/11,14,18,20,25,29 May 2018 External situation report/1,5,8,12,19,22,26 June 2018 External situation report/1,12,25 July 2018 |
| 4 Aug 2018/5 Dec 2018, ongoing | External situation report/7,14,22,28 Aug 2018 External situation report/4,11,18,25 Sept 2018 External situation report/4,9,17,23,30 Oct 2018 External situation report/6,13,21,28 Nov 2018 External situation report/5 Dec 2018 | |
| MERS-CoV | 9 July 2013/3 Sept 2015 | WHO statement on the 10th meeting of the IHR Emergency Committee regarding MERS/ 3 September 2015 |
| Yellow fever | 31 Aug 2016/16 May 2017 | - |
| Zika virus | 8 Mar 2016/18 Nov 2016 | Statement on the 1st meeting/18 November 2016 WHO statement on the 2nd meeting/2 September 2016 WHO statement on the 3rd meeting/14 June 2016 WHO statement on the 4th meeting/8 March 2016 WHO statement on the 5th meeting/1 February 2016 |
| Plague | 4 Oct 2017/4 Dec 2017 | External situation report/4 October 2017 External situation report/9, 12, 17, 20, 26, 31 October 2017 External situation report/6, 9, 14, 17, 20, 27 November 2017 External situation report/4 December 2017 |
| SARS | 27 Mar 2003/24 Jun 2003 | Update 11—WHO recommends new measures to prevent travel-related spread of SARS/ 27 March 2003 Update 37—WHO extends its SARS-related travel advice to Beijing and Shanxi Province in China and to Toronto Canada/23 April 2003 Update 42—Travel advice for Toronto, situation in China/29 April 2003 Update 50—WHO extends its SARS-related travel advice to Tianjin, Inner Mongolia and Taipei in China/8 May 2003 Update 58—First global consultation on SARS epidemiology, travel recommendations for Hebei Province (China), situation in Singapore/17 May 2003 SARS Travel Recommendations/10 June 2003 Update 80—Change in travel recommendations for parts of China, situation in Toronto/13 June 2003 SARS Travel Recommendations/16 June 2003 Update 82—Change in travel recommendations for Taiwan/17 June 2003 Update 86—Hong Kong removed from list of areas with local transmission/23 June 2003 Update 87—World Health Organisation changes last remaining travel recommendation—for Beijing, China/24 June 2003 |
| Influenza Pandemic (H1N1) 2009 | 25 Apr 2009/10 Aug 2010 | 1st meeting/25 April 2009 2nd meeting/27 April 2009 3rd meeting/5 June 2009 4th meeting/11 June 2009 5th meeting/24 September 2009 6th meeting/26 November 2009 7th meeting/24 February 2010 8th meeting/3 June 2010 9th meeting/10 August 2010 |
References
- World Health Organization. Technical Note for Ebola Virus Disease Preparedness Planning for Entry Screening at Airports, Ports and Land Crossings. 2014. Available online: https://apps.who.int/iris/handle/10665/144819 (accessed on 8 August 2018).
- World Health Organization. Handbook for Management of Public Health Events on Board Ships. 2016. Available online: https://www.who.int/ihr/publications/9789241549462/en/ (accessed on 3 July 2018).
- World Health Organization. International Health Regulations (2005), 3rd ed.; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- European Council. Decision No 1082/2013/Eu of the European Parliament and of The Council of 22 October 2013 on serious cross-border threats to health and repealing Decision No 2119/98/EC. Off. J. Eur. Union 2013, L 293, 1–15. [Google Scholar]
- World Health Organization. International Health Regulations. IHR Procedures and Implementation. 2018. Available online: https://www.who.int/ihr/procedures/en/ (accessed on 8 November 2018).
- Brown, C.M.; Aranas, A.E.; Benenson, G.A.; Brunette, G.; Cetron, M.; Chen, T.-H.; Cohen, N.J.; Diaz, P.; Haber, Y.; Hale, C.R.; et al. Airport exit and entry screening for Ebola—August-November 10, 2014. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 1163–1167. [Google Scholar] [PubMed]
- Ho, L.L.; Tsai, Y.-H.; Lee, W.-P.; Liao, S.-T.; Wu, L.-G.; Wu, Y.-C. Taiwan’s Travel and Border Health Measures in Response to Zika. Health Secur. 2017, 15, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Samaan, G.; Patel, M.; Spencer, J.; Roberts, L. Border screening for SARS in Australia: What has been learnt? Med. J. Aust. 2004, 180, 220–223. [Google Scholar] [CrossRef] [PubMed]
- St John, R.K.; King, A.; de Jong, D.; Bodie-Collins, M.; Squires, S.G.; Tam, T.W.S. Border screening for SARS. Emerg. Infect. Dis. 2005, 11, 6–10. [Google Scholar]
- Kuan, M.M.; Chang, F.Y. Airport sentinel surveillance and entry quarantine for dengue infections following a fever screening program in Taiwan. BMC Infect. Dis. 2012, 12, 182. [Google Scholar]
- Kuan, M.-M.; Lin, T.; Chuang, J.-H.; Wu, H.-S. Epidemiological trends and the effect of airport fever screening on prevention of domestic dengue fever outbreaks in Taiwan, 1998–2007. Int. J. Infect. Dis. 2010, 14, e693–e697. [Google Scholar]
- CDC. Ebola Virus Disease (Ebola) Pre-Departure/Exit Screening at Points of Departure in Affected Countries; 2014. Available online: https://http//wwwnc.cdc.gov/travel/pdf/ebola-exit-screening.pdf (accessed on 8 August 2018).
- Selvey, A.L.; Antao, C.; Hall, R. Entry screening for infectious diseases in humans. Emerg. Infect. Dis. 2015, 21, 197–201. [Google Scholar] [CrossRef]
- Huizer, Y.L.; Swaan, C.M.; Leitmeyer, K.C.; Timen, A. Usefulness and applicability of infectious disease control measures in air travel: A review. Travel Med. Infect. Dis. 2015, 13, 19–30. [Google Scholar]
- Shu, P.-Y.; Chien, L.-J.; Chang, S.-F.; Su, C.-L.; Kuo, Y.-C.; Liao, T.-L.; Ho, M.-S.; Lin, T.-H.; Huang, J.-H. Fever Screening at Airports and Imported Dengue. Emerg. Infect. Dis. 2005, 11, 460–462. [Google Scholar]
- Cohen, N.J.; Brown, C.M.; Alvarado-Ramy, F.; Bair-Brake, H.; Benenson, G.A.; Chen, T.-H.; Demma, A.J.; Holton, N.K.; Kohl, K.S.; Lee, A.W.; et al. Travel and Border Health Measures to Prevent the International Spread of Ebola. MMWR Suppl. 2016, 65, 57–67. [Google Scholar] [CrossRef] [PubMed]
- European Commission Consumers Health Agriculture And Food Executive Agency. Health and Food Safety Unit, Tender Specifications for Requesting Specific Services; Request for Specific Services Chafea/2017/Health/27 under multiple Framework Contract Chafea/2015/Health/05 with reopening of competition for the “Scripting, planning, conduction and evaluation of exercises, training and assessment implementing the Decision no 1082/2013/EU on serious cross-border threats to health” to provide services for Organisation of a training on entry and exit screening (Lot 3); European Commission Consumers Health Agriculture And Food Executive Agency: Luxembourg, 2017. [Google Scholar]
- Gostic, K.M.; Kucharski, A.J.; Lloyd-Smith, J.O. Effectiveness of traveller screening for emerging pathogens is shaped by epidemiology and natural history of infection. eLife 2015, 4, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Nishiura, H.; Wilson, N.; Baker, M.G. Quarantine for pandemic influenza control at the borders of small island nations. BMC Infect. Dis. 2009, 9, 27–41. [Google Scholar] [CrossRef]
- Gunaratnam, P.J.; Tobin, S.; Seale, H.; Marich, A.; McAnulty, J. Airport arrivals screening during pandemic (H1N1) 2009 influenza in New South Wales, Australia. Med. J. Aust. 2014, 200, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Hale, M.J.; Hoskins, R.S.; Baker, M.G. Screening for Influenza A(H1N1)pdm09, Auckland International Airport, New Zealand. Emerg. Infect. Dis. 2012, 18, 866–868. [Google Scholar] [CrossRef]
- ECDC. Technical Report: Infection Prevention and Control Measures for Ebola Virus Disease, Entry and Exit Screening Measures. 2014. Available online: https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/Ebola-outbreak-technicalreport-exit-entry-screening-13Oct2014.pdf (accessed on 8 August 2018).
- Wilder-Smith, A.; Paton, N.I.; Goh, K.T. Experience of severe acute respiratory syndrome in singapore: Importation of cases, and defense strategies at the airport. J. Travel Med. 2003, 10, 259–262. [Google Scholar] [CrossRef]
- Nishiura, H.; Kamiya, K. Fever screening during the influenza (H1N1-2009) pandemic at Narita International Airport, Japan. BMC Infect. Dis. 2011, 11, 111. [Google Scholar] [CrossRef]
- Bell, D.M.I. World Health Organization Working Group on, and S. Community Transmission of, Public health interventions and SARS spread, 2003. Emerg. Infect. Dis. 2004, 10, 1900–1906. [Google Scholar]
- Fujita, M.; Sato, H.; Kaku, K.; Tokuno, S.; Kanatani, Y.; Suzuki, S.; Shinomiya, N. Airport quarantine inspection, follow-up observation, and the prevention of pandemic influenza. Aviat. Space Environ. Med. 2011, 82, 782–789. [Google Scholar] [CrossRef]
- ECDC. Public health Emergency Preparedness for Cases of Viral Haemorrhagic Fever (Ebola) in Belgium: A Peer Review–16–19 March 2015; ECDC: Stockholm, Sweden, 2015. [Google Scholar]
- Frieden, T.R.; Damon, I.K. Ebola in West Africa—CDC’s Role in Epidemic Detection, Control, and Prevention. Emerg. Infect. Dis. 2015, 21, 1897–1905. [Google Scholar] [CrossRef]
- Tan, C.-C. SARS in Singapore-key lessons from an epidemic. Ann. Acad. Med. Singap. 2006, 35, 345–349. [Google Scholar] [PubMed]
- Arwady, M.A.; Bawo, L.; Hunter, J.C.; Massaquoi, M.; Matanock, A.; Dahn, B.; Ayscue, P.; Nyenswah, T.; Forrester, J.D.; Hensley, L.E.; et al. Evolution of Ebola Virus Disease from Exotic Infection to Global Health Priority, Liberia, Mid-2014. Emerg. Infect. Dis. 2015, 21, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Patel, M.; Tobin, S.; Sheppeard, V. Monitoring travellers from Ebola-affected countries in New South Wales, Australia: What is the impact on travellers? BMC Public Health 2017, 17, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Gomez, J.; Munayco, C.V.; Arrasco, J.C.; Suarez, L.; Laguna-Torres, V.A.; Aguilar, P.V.; Chowell, G.; Kochel, T.J. Pandemic influenza in a southern hemisphere setting: The experience in Peru from May to September, 2009. Eurosurveillance 2009, 14, 1937–19377. [Google Scholar] [CrossRef]
- Kuo, J.S.; Lee, Y.-H.; Hsieh, J.-W.; Lin, M.-C.; Yang, S.-Y. Initial Evaluation on Screening of Novel Influenza A (H1N1) at International Ports in Taiwan. Taiwan Epidemiol. Bull. 2009, 25, 626–647. [Google Scholar]
- Koonin, L.M.; Jamieson, D.J.; Jernigan, J.A.; Van Beneden, C.A.; Kosmos, C.; Harvey, M.C.; Pietz, H.; Bertolli, J.; Perz, J.F.; Whitney, C.G.; et al. Systems for Rapidly Detecting and Treating Persons with Ebola Virus Disease—United States. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 222–225. [Google Scholar]
- Lee, C.-W.; Tsai, Y.-S.; Wong, T.-W.; Lau, C.-C. A loophole in international quarantine procedures disclosed during the SARS crisis. Travel Med. Infect. Dis. 2006, 4, 22–28. [Google Scholar] [CrossRef]
- Mukherjee, P.; Lim, P.L.; Chow, A.; Barkham, T.; Seow, E.; Win, M.K.; Chua, A.; Leo, Y.S.; Chen, M.I.-C. Epidemiology of Travel-associated Pandemic (H1N1) 2009 Infection in 116 Patients, Singapore. Emerg. Infect. Dis. 2010, 16, 21–26. [Google Scholar] [CrossRef][Green Version]
- Nunn, R.; Jawad, M.; Cruickshank, H.; Poole, R.; Vass, C.; Fraser, S.D. Perspectives on Ebola screening at ports of entry in the UK. Perspect. Public Health 2015, 135, 66–67. [Google Scholar] [CrossRef]
- Saito, T. Public health challenges and legacies of Japan’s response to the Ebola virus disease outbreak in West Africa 2014 to 2015. Eurosurveillance 2015, 20, 25–30. [Google Scholar] [CrossRef]
- Sakaguchi, H.; Tsunoda, M.; Wada, K.; Ohta, H.; Kawashima, M.; Yoshino, Y.; Aizawa, Y. Assessment of Border Control Measures and Community Containment Measures Used in Japan during the Early Stages of Pandemic (H1N1) 2009. PLoS ONE 2012, 7, e31289. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, P.; Liyanage, S.; Seale, H.; Deng, Y.; Pang, X.; Tian, L.; Liu, B.; Zhang, L.; Wang, Q. The characteristics of imported cases and the effectiveness of outbreak control strategies of pandemic influenza A (H1N1) in China. Asia Pac. J. Public Health 2012, 24, 932–939. [Google Scholar] [CrossRef] [PubMed]
- CDC. 2014-2016 Ebola Outbreak in West Africa; 27 December 2017. Available online: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html (accessed on 8 August 2018).
- WHO. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. 31 December 2003. Available online: http://www.who.int/csr/sars/country/table2004_04_21/en/ (accessed on 8 August 2018).
- Wang, S.-F.; Wang, W.-H.; Chang, K.; Chen, Y.-H.; Tseng, S.-P.; Yen, C.-H.; Wu, D.-C.; Chen, Y.-M.A. Severe Dengue Fever Outbreak in Taiwan. Am. J. Trop. Med. Hyg. 2016, 94, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.S.-E.; Shu, P.-Y.; Yang, C.-H. A new reportable disease is born: Taiwan Centers for Disease Control’s response to emerging Zika virus infection. J. Formos. Med Assoc. 2016, 115, 223–225. [Google Scholar] [CrossRef] [PubMed]
- CDC. Taiwan CDC Confirms Zika Virus Infection in Foreign Traveler Detected with Fever upon Arrival; 19 September 2017. Available online: https://www.cdc.gov.tw/En/Bulletin/Detail/n89n_zsHG7c1yBMtIm2XPQ?typeid=158 (accessed on 8 August 2018).
- Huang, J.H.; Yang, C.-F.; Su, C.-L.; Chang, S.-F.; Cheng, C.-H.; Yu, S.-K.; Lin, C.-C.; Shu, P.-Y. Imported chikungunya virus strains, Taiwan, 2006-2009. Emerg. Infect. Dis. 2009, 15, 1854–1856. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-F.; Su, C.-L.; Hsu, T.-C.; Chang, S.-F.; Lin, C.-C.; Huang, J.C.; Shu, P.-Y. Imported Chikungunya Virus Strains, Taiwan, 2006–2014. Emerg. Infect. Dis. 2016, 22, 1981–1984. [Google Scholar] [CrossRef]
- Hsieh, Y.-H. Dengue outbreaks in Taiwan, 1998-2017: Importation, serotype and temporal pattern. Asian Pac. J. Trop. Med. 2018, 11, 460–466. [Google Scholar] [CrossRef]
- ECDC. Technical Report: Infection Prevention and Control Measures for Ebola Virus Disease Public Health Management of Healthcare Workers Returning from Ebola-Affected Areas. 2014. Available online: https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/management-healthcare-workers-returning-Ebola-affected-areas.pdf (accessed on 8 August 2018).
- World Health Organization. Public health measures taken at international borders during early stages of pandemic influenza A (H1N1) 2009: Preliminary results. Wkly. Epidemiol. Rec. 2010, 85, 186–194. [Google Scholar]
- Brosh-Nissimov, T.; Poles, L.; Kassirer, M.; Singer, R.; Kaliner, E.; Shriki, D.D.; Anis, E.; Fogel, I.; Engelhard, D.; Grotto, I.; et al. Preparing for imported Ebola cases in Israel, 2014 to 2015. Euro Surveill. 2015, 20, 54–60. [Google Scholar] [CrossRef]
- Glynn, J.R.; Bower, H.; Johnson, S.; Houlihan, C.F.; Montesano, C.; Scott, J.T.; Semple, M.G.; Bangura, M.S.; Kamara, A.J.; Kamara, O.; et al. Asymptomatic infection and unrecognised Ebola virus disease in Ebola-affected households in Sierra Leone: A cross-sectional study using a new non-invasive assay for antibodies to Ebola virus. Lancet Infect. Dis. 2017, 17, 645–653. [Google Scholar] [CrossRef]
- Rhymer, W.; Speare, R. Countries’ response to WHO’s travel recommendations during the 2013-2016 Ebola outbreak. Bull. World Health Organ. 2017, 95, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Lau, L.L.; Wu, P.; Wong, H.W.; Fang, V.J.; Riley, S.; Nishiura, H. Entry screening to delay local transmission of 2009 pandemic influenza A (H1N1). BMC Infect. Dis. 2010, 10, 82. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, I.I.; Creatore, M.I.; Cetron, M.S.; Brownstein, J.S.; Pesik, N.; Miniota, J.; Tam, T.; Hu, W.; Nicolucci, A.; Ahmed, S.; et al. Assessment of the potential for international dissemination of Ebola virus via commercial air travel during the 2014 west African outbreak. Lancet 2015, 385, 29–35. [Google Scholar] [CrossRef]
- Malone, J.D.; Brigantic, R.; Muller, G.A.; Gadgil, A.; Delp, W.; McMahon, B.H.; Lee, R.; Kulesz, J.; Mihelic, F.M. U.S. airport entry screening in response to pandemic influenza: Modeling and analysis. Travel Med. Infect. Dis. 2009, 7, 181–191. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Strengthening Health Security by Implementing the International Health Regulations (2005). Concept Note. Development, Monitoring and Evaluation of Functional Core Capacity for Implementing the International Health Regulations (2005). 2015. Available online: https://www.who.int/ihr/publications/concept_note_201507/en/ (accessed on 8 August 2018).
- World Health Organization. Joint External Evaluation Tool: International Health Regulations (2005), 2nd ed.; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Gaber, W.; Goetsch, U.; Diel, R.; Doerr, H.W.; Gottschalk, R. Screening for Infectious Diseases at International Airports: The Frankfurt Model. Aviat. Space Environ. Med. 2009, 80, 595–600. [Google Scholar] [CrossRef] [PubMed]
| Public Health Event | Type of Measure | Population of Interest (Humans) | Setting |
|---|---|---|---|
| Biological Biochemical Bacteriological Viral Microbiological Pathogen Public health risk Public health hazard Public health danger Hygiene Threat Exposure Pandemic Epidemic SARS H1N1 Flu Ebola Zika Plague Disease Influenza Infection Infectious Contagious Contagion Contamination Sick Sickness Illness Ailment | Exit/entry screening Entry/exit screening Entry and exit screening Exit and entry screening Entry screening Exit screening Border measure Border control Health assessment Health check | Patient Ill Sick Unhealthy Unwell Infected Affected Exposed Symptomatic Case Human Person Individual People Consumer Client Passenger Traveler Traveler Crew Refugee Migrant Immigrant Emigrant | Departure Exodus Debarkation Decampment Gateway Passageway Arrival Embarkation Checkpoint Airport Aerodrome Airdrome Air station Air terminal Flight terminal Aviation terminal Airfield Landing field Landing place Seaport Port Harbor Harbour Dock Pier Marine terminal Anchorage Port of embarkation Rail terminal Bus terminal Taxi (van) Ground crossing Land crossing Land-crossing Border crossing Frontier Terminal |
| (Biological OR Biochemical OR Bacteriological OR Viral OR Microbiological OR Pathogen OR Public health risk OR Public health hazard OR Public health danger OR Hygiene OR Threat OR Exposure OR Pandemic OR Epidemic OR SARS OR H1N1 OR Flu OR Ebola OR Zika OR Plague OR Disease OR Influenza OR Infection OR Infectious OR Contagious OR Contagion OR Contamination OR Sick OR Sickness OR Illness OR Ailment) AND (Exit/entry screening OR Entry/exit screening OR Entry screening OR Exit screening OR Entry and exit screening OR Exit and Entry screening OR Border measure OR Border control OR Health assessment OR Health check) AND (Patient OR Ill OR Sick OR Unhealthy OR Unwell OR Infected OR Affected OR Exposed OR Symptomatic OR Case OR Human OR Person OR Individual OR People OR Consumer OR Client OR Passenger OR Traveler OR Traveler OR Crew OR Refugee OR Migrant OR Immigrant OR Emigrant) AND (Departure OR Exodus OR Debarkation OR Decampment OR Gateway OR Passageway OR Arrival OR Embarkation OR Checkpoint OR Airport OR Aerodrome OR Airdrome OR Air station OR Air terminal OR Flight terminal OR Aviation terminal OR Airfield OR Landing field OR Landing place OR Seaport OR Port OR Harbor OR Harbour OR Dock OR Pier OR Marine terminal OR Anchorage OR Port of embarkation OR Rail terminal OR Bus terminal OR Taxi OR Ground crossing OR Land crossing OR Land-crossing OR Border crossing OR Frontier OR Terminal) | |||
| Inclusion Criteria |
|
|
| Exclusion criteria |
|
| Disease | Country | Type of Screening | Type of Point of Entry | ||||
|---|---|---|---|---|---|---|---|
| Entry | Exit | Airports | Seaports | Ground Crossings | |||
| Respiratory infections | Severe Acute Respiratory Syndrome | Australia [8] | X | - | X | X | - |
| Singapore [23,29] | X | - | X | X | X | ||
| Taiwan [35] | X | - | X | - | - | ||
| Canada [9] | X | X | X | - | - | ||
| Influenza Pandemic (H1N1) 2009 | Australia [20], China [40], Japan [24,26,39], New Zealand [21], Peru [32], Singapore [36], Taiwan [33] | X | - | X | - | - | |
| Vector-borne diseases | Dengue fever * | Taiwan [7,10,11,15] | X | - | X | - | - |
| Zika virus disease | Taiwan [7] | X | - | X | - | - | |
| Chikungunya infection * | Taiwan [7] | X | - | X | - | - | |
| Other | Ebola virus disease | Australia [31], Japan [38], United States [6], Canada [22] | X | - | X | - | - |
| Belgium [22,27] | X | - | X | X | - | ||
| United Kingdom [22,27,37] | X | - | X | X | X | ||
| Guinea, Liberia, Sierra Leone [6,16,22,28] | - | X | X | X | X | ||
| Nigeria, Senegal, Mali [6,16,22,28] | - | X | X | - | - | ||
| Public Health Event | WHO Emergency Committee | WHO Temporary Recommendations | |||
|---|---|---|---|---|---|
| Title | Started/Ended | PHEIC Yes/No (Date) | |||
| Entry/Exit Screening (Timeframe of Implementation) | On Travel Restrictions (Timeframe of Implementation) | ||||
| Ebola outbreak in Democratic Republic of the Congo (DRC) | 10 May 2018/25 July 2018 | No | IHR Emergency Committee regarding the Ebola outbreak in 2018 | Exit screening at airports (Mbandaka, Kinshasa), ports on the Congo river and congregation sites (23/5 to 25/7/2018) | Νo international travel or trade restrictions (10/5/2018 to 25/7/2018) |
| 4 August 2018/ongoing | No | Exit screening at defined points of entry in DRC (14/8/2018, ongoing, latest report on 5/12/2018) | Νo international travel or trade restrictions (4/8/2018, ongoing, latest report on 5/12/2018) | ||
| Ebola virus disease outbreak in West Africa | 8 August 2014/29 March 2016 | Yes (8/8/2014) | 2014–2016 IHR Emergency Committee for Ebola virus disease | Exit screening in affected countries *, at international airports, seaports and major land crossings (8/8/2014 to 29/3/2016) | No general ban on international travel (8/8/2014 to 18/12/2015) |
| No restrictions on travel and trade with Guinea, Liberia, and Sierra Leone (29/3/2016) | |||||
| MERS | 9 July 2013/ongoing, latest report on 3 September 2015 | No | IHR Emergency Committee concerning Middle East respiratory syndrome coronavirus | No | Νo international travel or trade restrictions (17/6/2015, ongoing, latest report on 3/9/2015) |
| Influenza Pandemic (H1N1) 2009 | 25 April 2009/10 August 2010 | Yes (25/4/2009) | IHR Emergency Committee concerning Influenza Pandemic (H1N1) 2009 | No | Countries should not close borders or restrict international traffic and trade; If ill, it is prudent to delay international travel (if ill after travel seek care) (25/4/2009 to 10/8/2010) |
| Plague | 4 October 2017/4 December 2017 | No | WHO Regional Office for Africa | No | Νo international travel or trade restrictions (4/10/2017) |
| Exit screening at International Airport in Antananarivo, Madagascar (9/10 to 4/12/2017) | Νo international travel or trade restrictions (4/10/2017 to 4/12/2017) | ||||
| Poliomyelitis | 5 May 2014/ongoing | Yes (5/5/2014) | IHR Emergency Committee concerning ongoing events and context involving transmission and international spread of poliovirus | Νo | Νo international travel or trade restrictions (5/5/2014 to 30/11/2018, ongoing) |
| SARS | 27 March 2003/24 June 2003 | Νο | WHO Scientific Research Advisory Committee SARS | Exit screening in affected countries (27/3 to 24/6/2003) | Νo international travel or trade restrictions (27/3/2003 to 24/6/2003) |
| Yellow fever | 31 August 2016/16 May 2017 | No | IHR Emergency Committee on yellow fever | No | Νo international travel or trade restrictions (31/8/2016 to 16/5/2017) |
| Zika virus disease | 1 February 2016/18 November 2016 | Yes (1/2/2016) | IHR Emergency Committee on Zika virus disease and observed increase in neurological disorders and neonatal malformations | No | Νo international travel or trade restrictions (1/2/2016 to 18/11/2016) |
| Country/PoE/Type of Screening/Disease/Year(s) | Site of Assessment | Primary Screening | Secondary Screening | Accompanying Measures and Response Measures | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Exposure Assessment | Symptom Assessment | Type of TMD * | Exposure Assessment | Symptom Assessment | Type of TMD | Accompanying Measures at the Border | Microbiological Tests | Quarantine/Isolation | ||
| Taiwan/airport/entry/Zika virus disease /2016 [7] | On board by crew or at aircraft site by airport officials | (-) * | Visual checks on board and at the terminal and temperature screening | Infrared cameras | Interview, questionnaire | In-person assessment | Ear thermometer | Risk communication (video), information about seeking medical assistance | Blood and urine samples sent to the Taiwan CDC’s laboratory (flaviviruses) | - |
| Taiwan/airport/entry/Dengue fever and Chikungunya infection/2013-2016 [7] | On board by crew or at airport site by airport officials | - | Visual checks on board and at the terminal and temperature screening | Infrared cameras | Interview, questionnaire | In-person assessment | Ear thermometer | Risk communication (video), information about seeking medical assistance | Dengue NS1 antigen rapid test (at airport), blood and urine samples sent to the Taiwan CDC’s laboratory (flaviviruses) | - |
| Taiwan/airport/entry/Dengue fever/2003-2007 [11] | Airport screening by airport clinicians | Questionnaire | Visual checks and temperature screening | Thermal scanning by non-contact infrared thermometers or infrared thermal camera | - | - | Ear thermometer | - | Real-time RT-PCR, and/or serological diagnosis by capture IgM/IgG ELISA | Not specified/at hospital |
| Taiwan/airport/entry/Dengue fever/2007-2010 [10] | Airport screening by quarantine officers | - | Questionnaire, temperature screening | Non-contact infrared thermometers (NCITs) with infrared thermal camera | Questionnaire | - | Ear thermometer | - | Dengue NS1 Rapid Test Kit (Bio-Rad, USA) (at airport), real-time RT-PCR, and/or serological diagnosis by capture IgM/IgG ELISA) | - |
| Australia/airport/entry/Ebola virus disease/2014-2015 [31] | At airport by public health staff and at public health units by infectious disease physician and public health unit staff | Questionnaire at terminal | Questionnaire at terminal | - | - | - | - | Risk communication, declaration of travel to EVD-affected countries on separate EVD-specific arrivals card, information about seeking medical assistance | PCR | At home/at designated Viral Hemorrhagic Fever hospital and local tertiary hospital |
| Belgium/airport/entry/Ebola virus disease/2014 [27] | - | - | Symptoms assessment (not specified) and temperature screening | Temperature screening (not specified) | - | - | - | Passenger locator card | In-house RT-PCR targets the GP gene; the large polymerase gene is targeted with an Altona commercial kit by Diagnostics GmbH, Hamburg, Germany | - |
| Japan/airport/entry/Ebola virus disease/2014-2015 [38] | At quarantine station, by immigration control officers | Interview | Questionnaire and temperature screening | Temperature screening (not specified) | - | - | - | Risk communication: posters at quarantine stations and in-flight announcements, information about seeking medical assistance | Laboratory test (not specified) | Not specified / hospital |
| UK/airport/entry/Ebola virus disease/2014-2015 [27,37] | At airport, by infectious disease physician | Questionnaire | Questionnaire and temperature screening | Ear thermometer | - | - | - | Information about seeking medical assistance | - | At home (asymptomatic but of high risk of EVD)/ At local acute hospital or designated specialist hospital |
| UK/train station/entry/Ebola virus disease/2014-2015 [27,37] | At train station, by infectious disease physician | Questionnaire | Questionnaire and temperature screening | Ear thermometer | - | - | - | Information about seeking medical assistance | - | Not specified/ At local acute hospital or designated specialist hospital |
| US/airport/entry/Ebola virus disease/2014-2015 [34] | At airport facilities | - | Temperature screening | Non-contact infrared thermometers | - | - | - | Risk communication, provision with Check and Report Ebola (CARE) kits that include health education materials, a thermometer, and ways to connect with their state or local health department, including a prepaid cell phone, information about seeking medical assistance | - | Unknown/Frontline health care facilities, Ebola assessment hospitals, and designated Ebola treatment centers |
| Guinea, Liberia, and Sierra Leone/airport/exit/Ebola virus disease/2014-2016 [6,16] | - | Questionnaire at terminal | Questionnaire at terminal, visual check, and temperature screening | Non-contact handheld infrared thermometer | Questionnaire at terminal | Questionnaire at terminal | Handheld non-contact thermometer | Risk communication, denied boarding | - | - |
| Guinea, Liberia, and Sierra Leone/land borders/exit /Ebola virus disease/2014-2016 [16] | - | - | Visual checks | - | - | - | - | - | - | - |
| Guinea, Liberia, and Sierra Leone/seaport/exit/Ebola virus disease/2014-2016 [16] | - | - | Temperature screening | - | - | - | - | Restricted access to vessels in port and disembarkation of seafarers, including cancellation of shore passes and crew transfers Protective equipment requirements for staff required to board vessels | - | Established on-site isolation facilities |
| China/airport/entry/Influenza Pandemic (H1N1) 2009 [40] | At quarantine station of the airport | - | Visual checks on board and temperature screening on board | - | Questionnaire at terminal | Questionnaire at terminal | - | Information about seeking medical assistance | RT- PCR | Not specified/ At the community hospitals or quarantine station, by general practitioners or public health workers |
| Japan/airport/entry/Influenza Pandemic (H1N1) 2009# [39] | On board, at terminal | Questionnaire | Questionnaire and temperature screening | Handheld infrared thermoscanner and axillary or oral on board, a fixed infrared thermoscanner at terminal | Questionnaire | Questionnaire | Ear or axillary thermometer | Information about seeking medical assistance, entry card | Rapid influenza test (on board), RT-PCR | Close contacts were quarantined at designated hotels/at designated medical institution |
| Japan/airport/entry/ Influenza Pandemic (H1N1) 2009 ‡ [39] | On board, at terminal | Questionnaire | Questionnaire and temperature screening | Handheld infrared thermoscanner on board, a fixed infrared thermoscanner at terminal | Questionnaire | Questionnaire | - | Information about seeking medical assistance, entry card | Rapid influenza test (on board and at terminal), RT-PCR | At designated medical institution |
| New Zealand/airport/entry/Influenza Pandemic (H1N1) 2009 [21] | - | - | Visual checks | - | - | - | - | Risk communication (in-flight scripted health message, signs), locator card completion | RT-PCR | At home or a facility for isolation |
| Peru/airport/entry/Influenza Pandemic (H1N1) 2009 [32] | - | Temperature screening | - | - | - | - | RT-PCR | |||
| Singapore/airport/entry/Influenza Pandemic (H1N1) 2009 [36] | - | - | Temperature screening | Thermal scanners | - | - | - | Risk communication (health advisories), information about seeking medical assistance | RT-PCR | At designated screening center at Hospital |
| Australia /airport/entry/Influenza Pandemic (H1N1) 2009 [20] | At terminal | Health declaration card | Health declaration card | Non-contact thermal imaging scanners | - | Brief clinical assessment | - | - | - | - |
| Taiwan/airport/entry/Influenza Pandemic (H1N1) 2009 [33] | - | - | Temperature screening | Infrared fever cameras | - | - | - | Health protection materials, such as masks and gloves, risk communication (broadcasting voice recording and distributing education sheets), information about seeking medical assistance | Laboratory test (not specified) | Not specified/At contract hospitals |
| Australia/airport/entry/SARS/2003 [8] | On board/at terminal | - | - | - | - | In-person assessment | Ear thermometer | Risk communication (in-flight notification by airline staff) | - | At home, by nurse and Chief Quarantine Officer/At designated state or territory hospital, by nurse and Chief Quarantine Officer |
| Australia/seaport/entry/SARS/2003 [8] | On board/at terminal | - | - | - | - | In-person assessment | Ear thermometer | Risk communication | - | |
| Canada/airport/entry/ exit/SARS/2003 [9] | - | Questionnaire (health alert notice) | Questionnaire (health alert notice) and temperature screening | Thermal scanning machines | Questionnaire | Questionnaire | Oral thermometer | Risk communication (posters and health alert notices) information about seeking medical assistance, traveler contact information form | PCR, serological test | Unknown/ At a predetermined hospital |
| Singapore/airport, seaport, road entry points/entry/SARS/2003 [23,29] | - | Health declaration cards | Visual checks and temperature screening | Thermal scanners | - | - | - | Risk communication, information about seeking medical assistance | Serology, SARS antibodies, and/or SARS coronavirus PCR | Home/ At specific hospital |
| Taiwan/airport/entry/SARS/2003 [35] | - | - | Interview, questionnaire | Infrared cameras | - | - | Ear electronic thermometer | Risk communication (public media), information about seeking medical assistance | White blood cell count, Chest X-ray findings | At specific hospital |
| Targeting Disease/s | Country | Timeframe | Number of Travelers | Sensitivity | Specificity | Country Surveillance Data/ Imported Cases ** | Reference | ||
|---|---|---|---|---|---|---|---|---|---|
| Screened | Suspected | Confirmed Detected | |||||||
| SARS | Taiwan | 3 March to 22 April 2003 | 2819 | 46 | 0 | - | - | 346/unknown | [35] |
| Canada | 14 May to 5 July 2003 | For health alert notices inbound: 677,494; For thermal imaging scanner inbound: 467,870 | For health alert notices inbound: 2478; For thermal imaging scanner inbound: 95 | 0 | - | - | 251/unknown | [9] | |
| Australia | 5 April to 16 June 2003 | 1.84 million arrivals | 794 were referred for screening to quarantine and inspection service staff. Of these, 734 (92.4%) were referred by quarantine/inspection service staff to the nurses at airports. 19 (2.4%) were then referred to the Chief Quarantine Officer | 0 | - | - | 6/unknown | [8] | |
| Singapore | 31 March to 31 May 2003 | 442,973 | 136 | 0 | - | - | 238/unknown | [23] | |
| Singapore | 9 April to 21 Sept 2003 | No information available | 4044 travelers were detected to have temperatures >37.5 °C through screening at the airport and sea terminals. Of these travelers, 327 were referred to hospital for assessment and 39 were admitted for further evaluation and isolation. | 0 | - | - | 238/unknown | [29] | |
| Influenza Pandemic (H1N1) 2009 | Singapore | 27 April to 27 June 2009 | - | - | 14 | - | - | [36] | |
| Australia | 28 April to 18 June 2009 | 625,147 | 5845 (0.93%) identified as symptomatic or febrile, 1296 (22.17%) identified as requiring further clinical assessment | 3 | 6.67% (95% CI, 1.40–18.27%) * | 99.10% (95% CI, 99.00–100.00%) * | [20] | ||
| Japan | 28 April to 20 June | 120,069 | 391 cases (0.33%) | 5 (1.28%) influenza type A 1 as influenza type B | - | - | [26] | ||
| Japan | 28 April to 18 June 2009 | 441,041 passengers and 30,692 airline crew members | 805 | 15 | - | - | [24] | ||
| Japan | 1 September 2009 to 31 January 2010 | 9,140,435 | 1049 | 10 | - | - | [24] | ||
| Japan | Period I: 28 April to 21 May 2009, Period II: 22 May to 18 June 2009 | Period I: 20,603; Period II: 265,696 | Period I: 561, Period II: 244 | Period I: 4, Period II: 5 | - | - | [39] | ||
| Taiwan | From 27 April to 19 June 2009 | 1,732,455 | 2685 were detected £ to have suspicious symptoms, including 1303 fever cases. Among these fever cases, 184 were sent to hospitals for further diagnosis and treatment after they were evaluated in terms of travel history and symptoms, by quarantine physicians or quarantine officers. | 12 | [33] | ||||
| China | 16 May to 30 September 2009 | 600,000 | 132 | - | - | [40] | |||
| Peru | 24 April to 4 July 2009 | 500,000 | 0 | 0 | - | - | [32] | ||
| New Zealand | 27 April to 22 June 2009 | 456,518 | 406 (0.09%) of these were referred for medical assessment. Of those, 109 (27%) met the case definition and received virologic testing. | 4 | 5.8% (95% CI 2.3–14.0%) † | - | [21] | ||
| Ebola virus disease | US | No information available | >1200 travelers were referred to CDC for additional screening because of illness or, more commonly, to assess possible exposures; 28 persons were referred for medical evaluation. | 0 | - | - | - | [28] | |
| US | 11 October to 10 November 2014 | 1993 | 86 (4.3%) | 0 | - | - | - | [6] | |
| US | 11 October 2014 to 31 January 2015 | 7587 | 543 (7.2%) were referred to on-site CDC screening at the airport for additional exposure risk assessment. At the time of assessment, 12 (0.16%) travelers were referred for medical evaluation at a local hospital. | 0 | - | - | 11/9 | [34] | |
| Australia | 1 October 2014 to 13 April 2015 | 123 | 6 | 0 | - | - | - | [31] | |
| Belgium | 20 October 2014 to 17 March 2015 | 13,356 | 0 | 0 | - | - | - | [27] | |
| UK | October 2014 to March 2015 | Approximately 5000 | 9 | 0 | - | - | 1/1 | [27] | |
| UK | 14 October 2014 to 4 January 2015 | 3388 passengers screened at UK ports of entry | 125 low risk passengers 5 high-risk passengers | 0 | - | - | 1/1 | [37] | |
| Japan | August 2014 to September 2015 | 9 | 9 | 0 | - | - | - | [38] | |
| Zika virus disease | Taiwan | January to October 2016 | 21,083,404 | 21,721 were identified as potentially ill through fever screening or passengers’ self-reporting. Upon evaluation, 3199 specimens were collected. | 5 | - | 17/17 | [7] | |
| Dengue fever | Taiwan | 2007 to 2010 | 52,047,769 | 48,115 | 406 | 40.22% (2007), 44.44% (2008), 53.2% (2009), 41.86% (2010) * | 99.96% (2007), 99.96% (2008), 99.97% (2009), 99.97% (2010) * | 5,800/910 | [10] |
| Taiwan | 2013 to 2016 | 85,464,274 | 67,704 ill passengers detected by entry screening, 9944 specimens collected | 518 | - | - | 61,118/1,249 | [7] | |
| Taiwan | 2003 to 2007 | - | - | 4119/539 | [11] | ||||
| Taiwan | July 2003 to June 2004 | 8,000,000 | ≈22,000 passengers were identified as fever patients. After clinical diagnosis, 3011 serum samples were sent for laboratory diagnosis of Dengue virus infection. | 40 | - | - | 6005/73 | [15] | |
| Chikungunya infection | Taiwan | 2013 to 2016 | 85,464,274 | 67,704 ill passengers detected by entry screening, 9944 specimens collected | 29 | - | - | 91/48 | [7] |
| Country | Targeting Disease/s | Timeframe | Number of Travelers | Sensitivity | Specificity | Reference | |||
|---|---|---|---|---|---|---|---|---|---|
| Screened | Suspected | Confirmed Detected | Confirmed Not Detected | ||||||
| Guinea, Liberia, Sierra Leone | Ebola virus disease | August to October 2014 | 80,000 | 0 | No | - | - | [6] | |
| Canada | SARS | 14 May to 5 July 2003 | For health alert notices: 495,492 For thermal imaging scanner: 295,212 | For health alert notices: 411 For thermal imaging scanner: 96 | 0 | No | - | - | [9] |
| Guinea, Liberia, Sierra Leone, Nigeria, Senegal, and Mali | Ebola virus disease | >200,000 travelers leaving Guinea, Liberia, and Sierra Leone had been screened and >150,000 in Nigeria | - | - | [28] | ||||
| Guinea, Liberia, and Sierra Leone | Ebola virus disease | 12 August to 12 October 2014 | 36,000 | 77 | 0 | 1 | 0% * | 99.79% * | [49] |
| Guinea, Liberia, and Sierra Leone | Ebola virus disease | August 2014 to January 2016 | 300,000 | 0 | 4 (none of them was overtly symptomatic at the time of travel) | - | - | [16] | |
| Disease | Type of Screening and Setting | Cost of Measures | Recommendations | Reference |
|---|---|---|---|---|
| Severe Acute Respiratory Syndrome | General, ad hoc entry/exit screening at airport in Canada | An estimated Can$ 7.55 million was invested in airport screening measures from March 18 to July 5, 2003. | “Rather than investing in airport screening measures to detect rare infectious diseases, investments should be used to strengthen screening and infection control capacities at points of entry into the healthcare system.” | [9] |
| Influenza Pandemic (H1N1) 2009 | General, ad hoc entry screening at airport in New South Wales (NSW), Australia | The cost of staffing airport clinics in NSW has been estimated at about US$50,000 per case detected (NSW Ministry of Health, unpublished data, 2012). | “Given the costs associated with staffing airport clinics, careful consideration should be given to deploying resources to airports for largely ineffective screening measures, compared with other activities such as contact tracing in the community”. | [20] |
| Dengue fever | General, entry screening at airport on routine basis in Taiwan | Not addressed. | “Our evaluation of the routine border screening for Dengue using NCITs yielded a low Positive Predictive Value, which suggested a low cost-effectiveness”. | [10] |
| The airport fever screening method requires an infrared thermal camera, which costs approximately US$ 43,000 for each set of instruments. In addition, one additional worker is needed to monitor this alarm system. | “The cost of identifying Dengue virus infections with airport fever screening is similar to that of other surveillance methods. The porting procedure and clinical and laboratory diagnoses are similar to those of surveillance methods. Therefore, the method is a cost-effective means of identifying imported Dengue cases”. | [15] |
| Disease/Type of Screening/ Point of Entry/Country | Methods | Results | References |
|---|---|---|---|
| Dengue fever/ Entry screening on routine basis/ Airport/Taiwan | Comparing confirmed cases identified at points of entry with total imported cases | “Airport fever screening was successful in identifying 45% (244/542; 95% confidence interval 33.1–57.8%) of imported Dengue cases with fever.” | [11] |
| Dengue fever/ Entry screening on routine basis/ Airport/Taiwan | Fluctuations in the number of symptomatic imported Dengue cases identified in the airports (X) were associated with the total number of imported Dengue cases (Y) based on a regression analysis of a biweekly surveillance | “By implementing the airport fever screening program followed by laboratory confirmation, nearly half of the imported symptomatic Dengue cases were detected at entry.” “An analysis of the dataset according to the geographical areas (25 counties/cities) indicated that there were significant correlations between the annual cumulative number of Dengue importations identified at the airports (X) and the number of Dengue importations reported from community clinics (Y) (n = 96, Y = 0.93X + 1.208, R2 = 0.57, p < 0.0001).” | [10] |
| Dengue fever/ Entry screening on routine basis/ Airport/Taiwan | Comparing confirmed cases identified at points of entry with total imported cases | “518/1188 confirmed cases identified at points of entry/total imported cases (43.6%)” | [7] |
| Dengue fever/ Entry screening on routine basis/ Airport/Taiwan | Comparing confirmed cases identified at points of entry with total imported cases. Comparing numbers of imported cases before and after screening measure implementation | “Airport fever screening alone identified 40 (83.3%) of 48 of all imported cases identified by the active surveillance system.” “Fever screening at the airports has also dramatically increased the proportion of imported Dengue cases identified by active surveillance, 48 (65.8%), of 73 which is significantly higher than the number identified during years before fever screening were implemented (p < 0.0001 by chi-square test)” | [15] |
| Influenza Pandemic (H1N1) 2009/ Entry screening ad hoc/ Airport/Japan | Comparing cases in the community and imported cases identified through screening | “In spite of the quarantine inspection, the number of Japanese patients with novel influenza reached 633 by June 18, 2009. Only 11 patients were found by the airport quarantine inspection, but importantly, about 20% of all patients had an overseas travel history and had passed through the quarantine inspection.” | [26] |
| Influenza Pandemic (H1N1) 2009/ Entry screening ad hoc/ Airport/Japan | Comparing surveillance data of imported cases with entry screening results and investigating imported cases’ travel history and time of symptoms onset | “6.6% (10/151) of the individuals infected during international travel were identified by the border control measures upon entry in May and June 2009.” “2 individuals among those identified later in Japan to be infected had been missed at entry despite being symptomatic. 22 others were identified after entry into Japan despite being symptomatic at entry screening.” “Health monitoring identified 8 infected individuals. Enhanced surveillance identified 812 individuals, 141 (18%) of whom had a history of international travel. 24 these 141 passengers picked up by enhanced surveillance had been developing symptoms on entry and were missed at screening.” | [39] |
| Influenza Pandemic (H1N1) 2009/ Entry screening ad hoc/ Airport/Taiwan | Comparing surveillance data of imported cases with entry screening results | “Cases identified among passengers screened out by quarantine measures and transferred to hospitals by quarantine officers account for 20.3% (12 cases) of all imported cases.” | [33] |
| Zika virus disease/ Entry screening ad hoc/ Airport/ Taiwan | Comparing confirmed cases identified at points of entry with total imported cases | “As of October 31, 2016, Taiwan has no locally acquired Zika infections, but 13 imported cases have been identified, of which 38% were identified by airport border screening.” | [7] |
| Chikungunya infection / Entry screening ad hoc/ Airport/ Taiwan | Comparing confirmed cases identified at points of entry with total imported cases | “29/48 Confirmed cases identified at points of entry/total imported cases (60.4%)” | [7] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mouchtouri, V.A.; Christoforidou, E.P.; an der Heiden, M.; Menel Lemos, C.; Fanos, M.; Rexroth, U.; Grote, U.; Belfroid, E.; Swaan, C.; Hadjichristodoulou, C. Exit and Entry Screening Practices for Infectious Diseases among Travelers at Points of Entry: Looking for Evidence on Public Health Impact. Int. J. Environ. Res. Public Health 2019, 16, 4638. https://doi.org/10.3390/ijerph16234638
Mouchtouri VA, Christoforidou EP, an der Heiden M, Menel Lemos C, Fanos M, Rexroth U, Grote U, Belfroid E, Swaan C, Hadjichristodoulou C. Exit and Entry Screening Practices for Infectious Diseases among Travelers at Points of Entry: Looking for Evidence on Public Health Impact. International Journal of Environmental Research and Public Health. 2019; 16(23):4638. https://doi.org/10.3390/ijerph16234638
Chicago/Turabian StyleMouchtouri, Varvara A., Eleni P. Christoforidou, Maria an der Heiden, Cinthia Menel Lemos, Margherita Fanos, Ute Rexroth, Ulrike Grote, Evelien Belfroid, Corien Swaan, and Christos Hadjichristodoulou. 2019. "Exit and Entry Screening Practices for Infectious Diseases among Travelers at Points of Entry: Looking for Evidence on Public Health Impact" International Journal of Environmental Research and Public Health 16, no. 23: 4638. https://doi.org/10.3390/ijerph16234638
APA StyleMouchtouri, V. A., Christoforidou, E. P., an der Heiden, M., Menel Lemos, C., Fanos, M., Rexroth, U., Grote, U., Belfroid, E., Swaan, C., & Hadjichristodoulou, C. (2019). Exit and Entry Screening Practices for Infectious Diseases among Travelers at Points of Entry: Looking for Evidence on Public Health Impact. International Journal of Environmental Research and Public Health, 16(23), 4638. https://doi.org/10.3390/ijerph16234638