Understanding Discomfort in Order to Appropriately Treat Fever
Abstract
1. Introduction
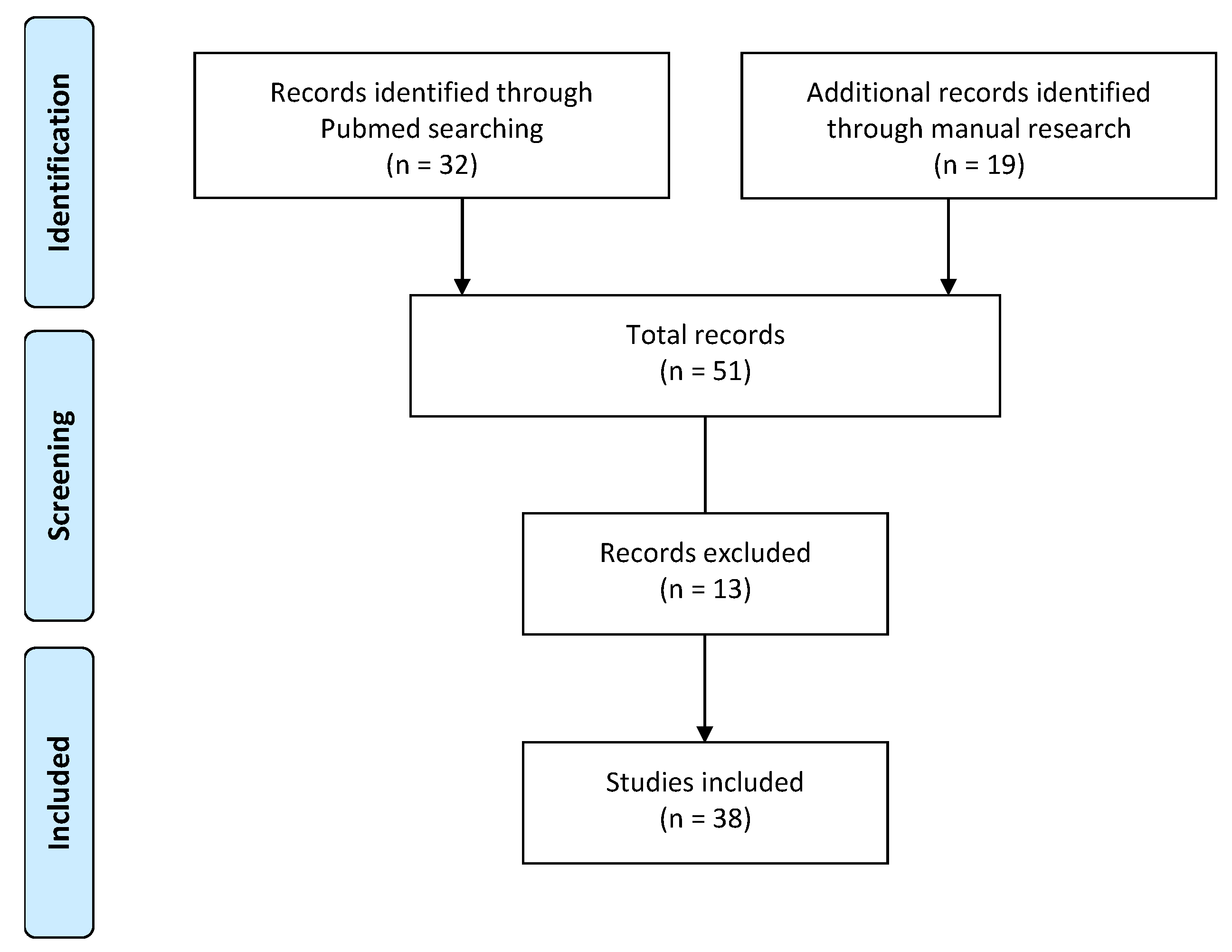
2. The Extent of the Problem
3. Materials and Methods
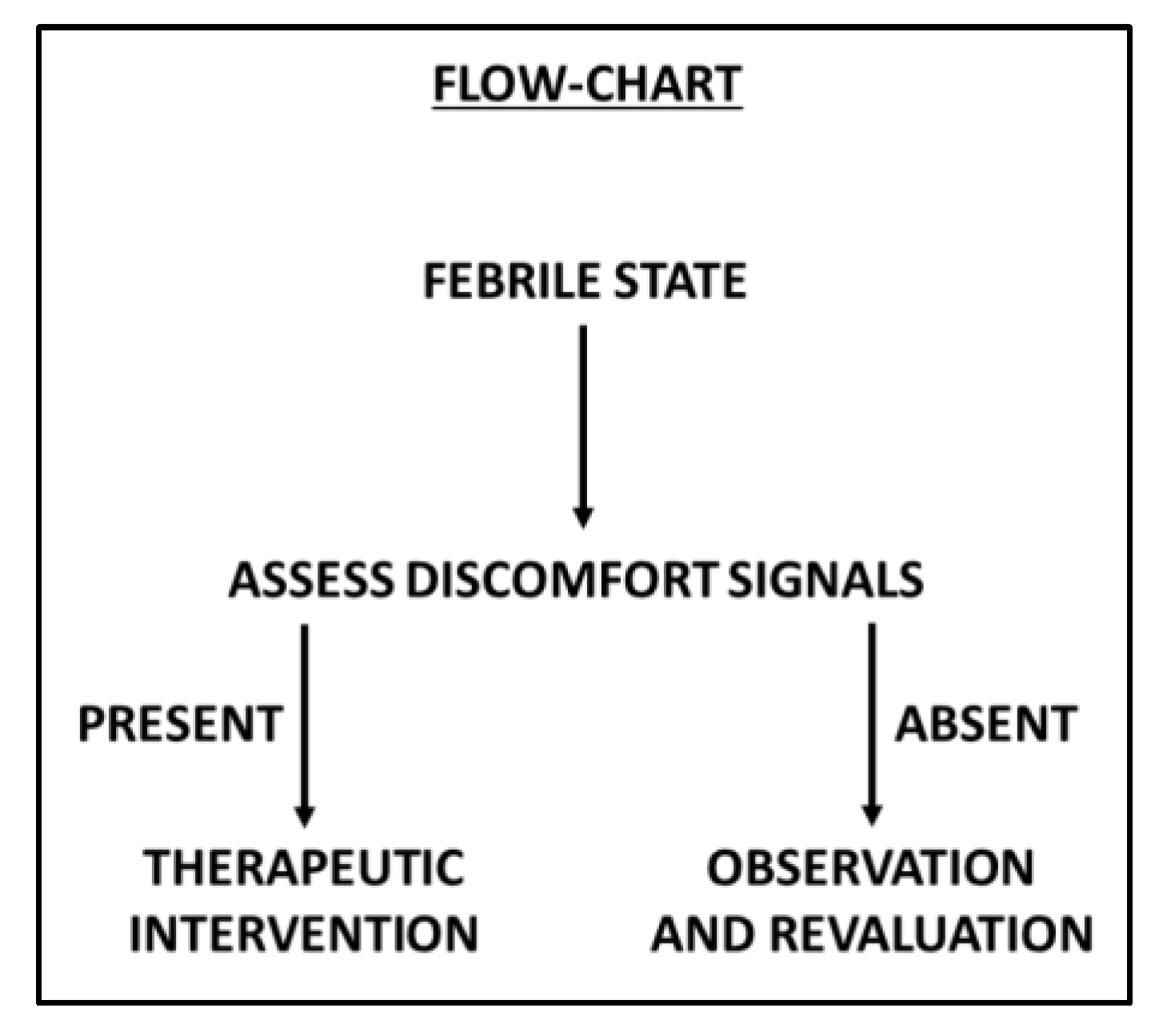
4. Results
5. Discussion
- behavioral changes;
- mood changes;
- alterations in the sleep–wake rhythm, in feeding, in activity level, in interest, in play;
- onset of symptoms of irritability and agitation, moaning, crying;
- withdrawal or dysfunction in social interactions.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Chiappini, E.; Venturini, E.; Remaschi, G.; Principi, N.; Longhi, R.; Tovo, P.A.; Becherucci, P.; Bonsignori, F.; Esposito, S.; Festini, F.; et al. Italian Pediatric Society Panel for the Management of Fever in Children. 2016 Update of the Italian Pediatric Society Guidelines for Management of Fever in Children. J. Pediatr. 2017, 180, 177–183. [Google Scholar] [CrossRef]
- NICE Fever in under 5s: Assessment and Initial Management. Available online: https://www.nice.org.uk/guidance/cg160/chapter/1-recommendations (accessed on 23 September 2019).
- Chiappini, E.; Cangelosi, A.; Becherucci, P.; Pierattelli, M.; Galli, L.; de Martino, M. Knowledge, attitudes and misconceptions of Italian healthcare professionals regarding fever management in children. BMC Pediatr. 2018, 18, 194. [Google Scholar] [CrossRef]
- Clericetti, C.M.; Milani, G.P.; Bianchetti, M.G.; Simonetti, G.D.; Fossali, E.F.; Balestra, A.M.; Bozzini, M.A.; Agostoni, C.; Lava, S.A.G. Systematic review finds that fever phobiais a worldwide issue among caregivers and healthcare providers. Acta Paediatr. 2019, 108, 1393–1397. [Google Scholar]
- Chiappini, E.; D’Elios, S.; Mazzantini, R.; Becherucci, P.; Pierattelli, M.; Galli, L.; de Martino, M. Adherence among Italian paediatricians to the Italian guidelines for the management of fever in children: A cross sectional survey. BMC Pediatr. 2013, 13, 210. [Google Scholar] [CrossRef]
- Bertille, N.; Purssell, E.; Hjelm, N.; Bilenko, N.; Chiappini, E.; de Bont, E.G.P.M.; Kramer, M.S.; Lepage, P.; Lava, S.A.G.; Mintegi, S.; et al. Symptomatic Management of Febrile Illnesses in Children: A Systematic Review and Meta-Analysis of Parents’ Knowledge and Behaviors and Their Evolution Over Time. Front. Pediatr. 2018, 6, 279. [Google Scholar] [CrossRef]
- Chiappini, E.; Bortone, B.; Galli, L.; de Martino, M. Guidelines for the symptomatic management of fever in children: Systematic review of the literature and quality appraisal with AGREE II. BMJ Open 2017, 7, e015404. [Google Scholar] [CrossRef]
- Elena, C. La Gestione Della Febbre in età Pediatrica; Edit-Symposia Pediatria & Neonatologia; Editeam: Ferrara, Italy, 2018. [Google Scholar]
- Raffaeli, G.; Orenti, A.; Gambino, M.; Peves Rios, W.; Bosis, S.; Bianchini, S.; Tagliabue, C.; Esposito, S. Fever and Pain Management in Childhood: Healthcare Providers’ and Parents’ Adherence to Current Recommendations. Int. J. Environ. Res. Public Health 2016, 13, 499. [Google Scholar] [CrossRef] [PubMed]
- Autret-Leca, E.; Gibb, I.A.; Goulder, M.A. Ibuprofen versus paracetamol in pediatric fever: Objective and subjective findings from a randomized, blinded study. Curr. Med. Res. Opin. 2007, 23, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Gupta, H.; Shah, D.; Gupta, P.; Sharma, K.K. Role of paracetamol in treatment of childhood Fever: A double-blind randomized placebo-controlled trial. Indian Pediatr. 2007, 44, 903–911. [Google Scholar] [PubMed]
- Cranswick, N.; Coghlan, D. Paracetamol efficacy and safety in children: The first 40 years. Am. J. Ther. 2000, 7, 135–141. [Google Scholar] [CrossRef]
- de Martino, M.; Chiarugi, A. Recent Advances in Pediatric Use of Oral Paracetamol in Fever and Pain Management. Pain Ther. 2015, 4, 149–168. [Google Scholar] [CrossRef] [PubMed]
- Trippella, G.; Ciarcià, M.; de Martino, M.; Chiappini, E. Prescribing Controversies: An Updated Review and Meta-Analysis on Combined/Alternating Use of Ibuprofen and Paracetamol in Febrile Children. Front Pediatr. 2019, 7, 217. [Google Scholar] [CrossRef] [PubMed]
- Barberi, S.; Bona, G.; Capecchi, E.; Chiappini, E.; De Angelis, G.L.; De Martino, M.; Di Mauro, G.; Lavarazzo, L.; Marchisio, P.; Marseglia, G.L.; et al. La Gestione Di Febbre E Dolore in Età Pediatrica; Supplemento al numero 3 ANNO XII—Sintesi InfoMedica S.r.l: Legnano (MI), Italy, 2017. [Google Scholar]
- Meremikwu, M.; Oyo-Ita, A. Physical methods for treating fever in children. Cochrane Database Syst. Rev. 2003, 2, CD004264. [Google Scholar] [CrossRef]
- Chiappini, E.; Parretti, A.; Becherucci, P.; Pierattelli, M.; Galli, L.; de Martino, M. Risultati Di Un Questionario Distribuito a 644 Genitori Di Bambini Di età 0-6 Anni Di 12 Scuole Del Comune Di LASTRA a Signa; Periodi ciclo: Marzo-giugno, Firenze, 2010. [Google Scholar]
- Choi, A.-R.; Kim, J.S. Fever Phobia: A Survey of Children’s Parents in a Pediatric Outpatient Clinic. Child Health Nurs. Res. 2014, 20, 113–122. [Google Scholar] [CrossRef]
- Spiers, J.A.; Enarson, M.C.; Ali, S.; Vandermeer, B.; Wright, R.B.; Klassen, T.P. Beliefs and Expectations of Canadian Parents Who Bring Febrile Children for Medical Care. Pediatrics 2012, 130, 905–912. [Google Scholar] [CrossRef]
- Chiappini, E.; Parretti, A.; Becherucci, P.; Pierattelli, M.; Bonsignori, F.; Galli, L.; de Martino, M. Parental and medical knowledge and management of fever in Italian pre-school children. BMC Pediatr. 2012, 12, 97. [Google Scholar] [CrossRef] [PubMed]
- Corrard, F.; Copin, C.; Wollner, A.; Elbez, A.; Derkx, V.; Bechet, S.; Levy, C.; Boucherat, M.; Cohen, R. Sickness behavior in feverish children is independent of the severity of fever. PLoS ONE 2017, 12, e0171670. [Google Scholar] [CrossRef] [PubMed]
- Staphorst, M.; Benninga, M.; Bisschoff, M.; Bon, I.; Busschbach, J.; Diederen, K.; van Goudoever, J.; Haarman, E.; Hunfeld, J.; Jaddoe, V.; et al. The child’s perspective on discomfort during medical research procedures: A descriptive study. BMJ Open 2017, 7, e016077. [Google Scholar]
- Kanabar, D. A Practical Approach to the Treatment of Low-Risk Childhood Fever. Drugs 2014, 14, 45–55. [Google Scholar] [CrossRef][Green Version]
- Dantzer, R.; Kelley, K.W. Twenty years of research on cytokine-induced sickness behavior. Brain Behav. Immun. 2007, 21, 153–160. [Google Scholar] [CrossRef]
- Kramer, M.S.; Naimark, L.E.; Roberts-BraÈuer, R.; McDougall, A.; Leduc, D.G. Risks and benefits of paracetamol antipyresis in young children with fever of presumed viral origin. Lancet 1991, 337, 591–594. [Google Scholar] [CrossRef]
- McIntyre, J.; Hull, D. Comparing efficacy and tolerability of ibuprofen and paracetamol in fever. Arch. Dis. Child. 1996, 74, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Autret, E.; Reboul-Marty, J.; Henry-Launois, B.; Laborde, C.; Courcier, S.; Goehrs, J.M.; Languillat, G.; Launois, R. Evaluation of ibuprofen versus aspirin and paracetamol on efficacy and comfort in children with fever. Eur. J. Clin. Pharm. 1997, 51, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Sarrell, E.M.; Wielunsky, E.; Cohen, H.A. Antipyretic treatment in young children with fever: Acetaminophen, ibuprofen, or both alternating in a randomized, double-blind study. Arch. Pediatr. Adolesc. Med. 2006, 160, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.C.; Richards, P.A.; Thompson, A.M.; Harper, D.P.; Fairchok, M.P. Alternating antipyretics: Antipyretic efficacy of acetaminophen versus acetaminophen alternated with ibuprofen in children. Clin. Pediatr. (Phila.) 2008, 47, 907–911. [Google Scholar] [CrossRef]
- Hay, A.D.; Costelloe, C.; Redmond, N.M.; Montgomery, A.A.; Fletcher, M.; Hollinghurst, S.; Peters, T.J. Paracetamol plus ibuprofen for the treatment of fever in children (PITCH): Randomized controlled trial. BMJ 2008, 337, a130215. [Google Scholar] [CrossRef]
- Guarino, A. Psiconcologia Dell’età Evolutiva; Ericson, Ed.; Centro Studi Erickson: Trento, Italy, 2006. [Google Scholar]
| Signals of Discomfort | Variations of Sleep-Wake Rhythm | delayed sleep phase |
| early sleep phase | ||
| night awakenings | ||
| Appetite Variations | eat less | |
| no liquid intake | ||
| Variation in Motor Activity | restlessness | |
| agitation | ||
| weakness | ||
| fatigue | ||
| Change in Mood | irritability | |
| anger | ||
| weeping | ||
| Variation in Daily Habits | no play | |
| no interests shown | ||
| seeking comfort | ||
| uncooperative | ||
| Variation of Facial Expression | changed look | |
| clenched teeth | ||
| curled lips | ||
| wrinkled forehead | ||
| paleness/colour change | ||
| Other Signals | tachypnoea | |
| chills | ||
| widespread pain |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doria, M.; Careddu, D.; Ceschin, F.; Libranti, M.; Pierattelli, M.; Perelli, V.; Laterza, C.; Chieti, A.; Chiappini, E. Understanding Discomfort in Order to Appropriately Treat Fever. Int. J. Environ. Res. Public Health 2019, 16, 4487. https://doi.org/10.3390/ijerph16224487
Doria M, Careddu D, Ceschin F, Libranti M, Pierattelli M, Perelli V, Laterza C, Chieti A, Chiappini E. Understanding Discomfort in Order to Appropriately Treat Fever. International Journal of Environmental Research and Public Health. 2019; 16(22):4487. https://doi.org/10.3390/ijerph16224487
Chicago/Turabian StyleDoria, Mattia, Domenico Careddu, Flavia Ceschin, Maria Libranti, Monica Pierattelli, Valentina Perelli, Claudia Laterza, Annarita Chieti, and Elena Chiappini. 2019. "Understanding Discomfort in Order to Appropriately Treat Fever" International Journal of Environmental Research and Public Health 16, no. 22: 4487. https://doi.org/10.3390/ijerph16224487
APA StyleDoria, M., Careddu, D., Ceschin, F., Libranti, M., Pierattelli, M., Perelli, V., Laterza, C., Chieti, A., & Chiappini, E. (2019). Understanding Discomfort in Order to Appropriately Treat Fever. International Journal of Environmental Research and Public Health, 16(22), 4487. https://doi.org/10.3390/ijerph16224487




