Mapping the Status of Healthcare Improvement Science through a Narrative Review in Six European Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Aim and Design
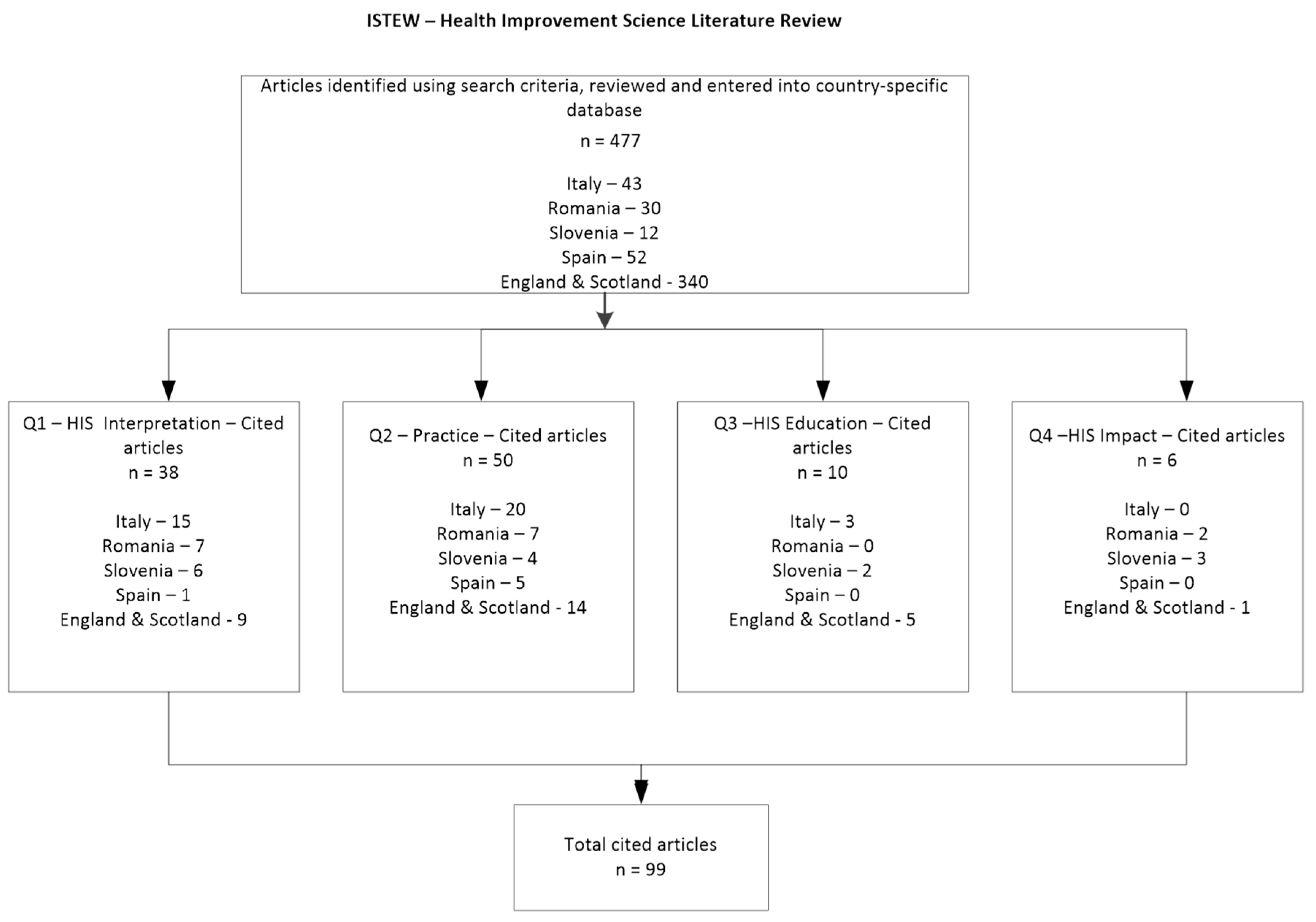
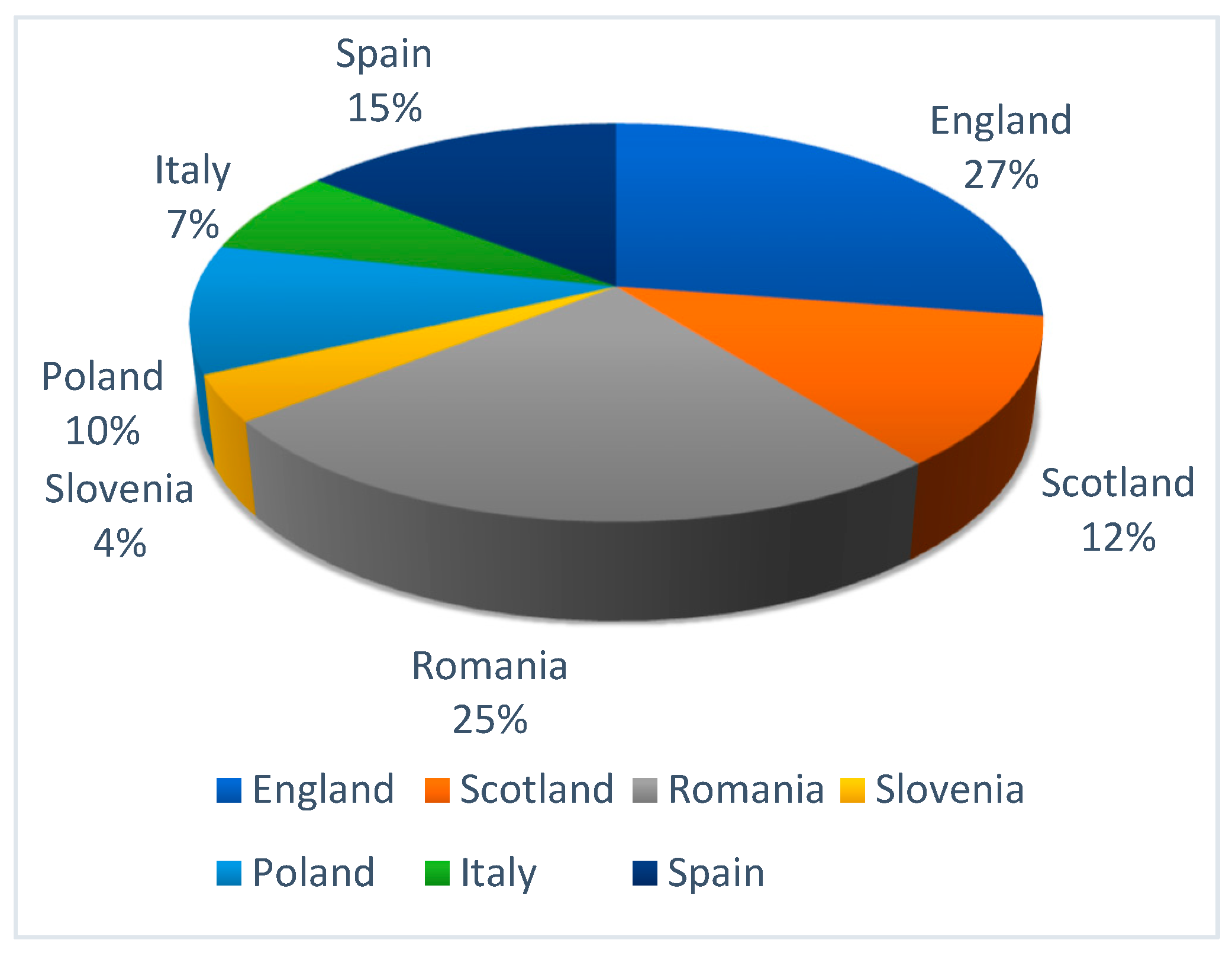
2.2. Search Methods and Outcome
2.3. Criteria for Inclusion
3. Results
3.1. How Is Improvement Science Interpreted?
3.2. How Is Improvement Science Practised?
3.3. How Are Multidisciplinary Health Students Educated in (the Various Components of) Improvement Science?
3.4. What Is the Impact of Education in Improvement Science on Service Provision?
4. Discussion
5. Discussion of Limitations
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Search Terms and Research Protocol
- Improvement N2 science OR “translation * research” OR “translation * science” OR “translation * knowledge”
- OR Implement N2 science (in abstracts and titles)
- AND
- Interpret * OR defin * OR framework * OR theor * OR technique* OR tool * OR method *
- Improvement N2 science OR “translation * research” OR “translation * science” OR “translation * knowledge”
- OR Implement N2 science (in abstracts and titles)
- AND
- Practic * OR impact * OR implement * OR deliver * OR integrat * OR embed * OR “service provision” OR application *
- Improvement N2 science OR “translation * research” OR “translation * science” OR “translation * knowledge”
- OR Implement N2 science (in abstracts and titles)
- AND
- Education * OR curriculum OR training OR course * OR facult *
- AND
- Student * OR cohort *
- Improvement N2 science OR “translation * research” OR “translation * science” OR “translation * knowledge”
- OR Implement N2 science (in abstracts and titles)
- AND
- Education * OR curriculum OR training OR course * OR facult *
- AND
References
- New-European Parliament. MEPs Propose Blueprint for Safer Healthcare. 2015. Available online: http://www.europarl.europa.eu/news/en/press-room/20150513IPR55317/meps-propose-blueprint-for-safer-healthcare (accessed on 5 January 2017).
- Griffin, F.A.; Resar, R.K. IHI Global Trigger Tool for Measuring Adverse Events, 2nd ed.; IHI Innovation Series White Paper; Institute for Healthcare Improvement: Cambridge, MA, USA, 2009. [Google Scholar]
- Skela-Savič, B.; Macrae, R.; Lillo-Crespo, M.; Rooney, K.D. The development of a consensus definition for healthcare improvement science (HIS) in seven European countries: A consensus methods approach. Slov. J. Public Heal. 2017, 56, 82–90. [Google Scholar] [CrossRef] [PubMed]
- University of the West of Scotland. ISTEW Project. 2015. Available online: http://www.uws.ac.uk/improvementscience/ (accessed on 10 March 2017).
- Lillo-Crespo, M.; Sierras-Davó, M.C.; Macrae, R.; Rooney, K. Developing a framework for evaluating the impact of Healthcare Improvement Science Education across Europe: A qualitative study. J. Educ. Eval. Heal. Prof. 2017, 14, 28. [Google Scholar] [CrossRef] [PubMed]
- Macrae, R.; Rooney, K.D.; Taylor, A.; Ritters, K.; Sansoni, J.; Crespo, M.L.; Skela-Savič, B.; O’Donnell, B.; O’Donnell, B. Making it easy to do the right thing in healthcare: Advancing improvement science education through accredited pan European higher education modules. Nurse Educ. Today 2016, 42, 41–46. [Google Scholar] [CrossRef] [PubMed][Green Version]
- University of Alicante, International Summer Programme on HIS Introduction and Immersion. Available online: https://web.ua.es/es/verano/documentos/2019/dipticos/immersion.pdf (accessed on 2 May 2019).
- Mihaescu, T. Review of Available HIS Training. Intern. ISTEW Doc. 2014, in press. [Google Scholar]
- Glowacka, M. Gap Analysis of Available HIS Education/Training. Intern. ISTEW Doc. 2014, in press. [Google Scholar]
- Sansoni, J. Clarification of HIS Competencies and Capabilities. Intern. ISTEW Doc. 2014, in press. [Google Scholar]
- Zurc, J.; Skela-Savic, B. The definition of HIS. Intern. ISTEW Doc. 2014, in press. [Google Scholar]
- Bernardo, W.M.; Nobre, M.R.C.; Jatene, F.B. A prática clínica baseada em evidências: Parte II—Buscando as Evidências em Fontes de Informação. Rev. Bras. Reum. 2004, 44, 403–409. [Google Scholar] [CrossRef]
- Broome, M.E. Integrative Literature Reviews for the Development of Concepts. In Concept Development in Nursing: Foundations, Techniques and Applications; WB Saunders Company: Philadelphia, PA, USA, 2000; pp. 231–250. [Google Scholar]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Perla, R.J.; Provost, L.P.; Parry, G.J. Seven propositions of the science of improvement: Exploring foundations. Qual. Manag. Healthc. 2013, 22, 170–186. [Google Scholar] [CrossRef]
- The Health Foundation. Improvement Science—Research Scan; The Health Foundation: London, UK, 2011. [Google Scholar]
- Mitchell, S.A.; Fisher, C.A.; Hastings, C.E.; Silverman, L.B.; Wallen, G.R. A thematic analysis of theoretical models for translational science in nursing: Mapping the field. Nurs. Outlook 2010, 58, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Verboncu, I.; Ganescu, R. Hospital Performances, a Key Component as Part of the Health Reform Process from Romania. Adm. Manag. Public 2010, 14, 130. [Google Scholar]
- Herbei, M.H. Performance Model of the Public and Private Health Systems from Romania. Ann. Univ. Craiova Econ. Sci. Ser. 2011, 4, 9–14. [Google Scholar]
- Amodio, E.; Avitabile, R.; Meloni, C.; Riti, F.; Giancotti, E.; Coda, V. Ascolto nel silenzio-Rianimazione a misura d’uomo. QA 2009, 19, 14–17. [Google Scholar]
- Tomasini, I.; Vincenzi, D.; Monacelli, S.; Baraccani, C.; Omelkova, B. The procedures for authorisation and accreditation of Transfusion Structures and blood donation centres: What are the requisites? The experience of the Transfusion Service and AVIS blood donation centres in Ravenna. High Speed Blood Transfus. Equip. 2010, 8, 170–177. [Google Scholar]
- Odetto, L.; Sacco, M. L’Ospedale Pediatrico L’Ospedale Pediatrico per intensità di cure: l’esperienza torinese. Giornale Italiano di Scienze Infermieristiche Pediatriche 2011, 3, 15–19. [Google Scholar]
- Saiani, L.; Chiari, P.; Palese, A. Raccomandazioni e standard italiani per dotazioni infermieristiche ospedaliere sicure. Ig Sanità Pubbl 2011, 67, 777–792. [Google Scholar]
- Fusco, D.; Barone, A.P.; Sorge, C.; D’Ovidio, M.; Stafoggia, M.; Lallo, A.; Davoli, M.; Perucci, C. P.Re.Val.E.: Outcome research program for the evaluation of health care quality in Lazio, Italy. BMC Heal. Serv. Res. 2012, 12, 25. [Google Scholar] [CrossRef]
- Toccafondi, G.; Albolino, S.; Tartaglia, R.; Guidi, S.; Molisso, A.; Venneri, F.; Peris, A.; Pieralli, F.; Magnelli, E.; Librenti, M.; et al. The collaborative communication model for patient handover at the interface between high-acuity and low-acuity care. BMJ Qual. Saf. 2012, 21, 58–66. [Google Scholar] [CrossRef]
- Toccafondi, G.; Albolino, S.; Bellandi, T.; Venneri, F. Handover process: How to improve quality and safety through an ergonomic solution. Work 2012, 41, 2941–2945. [Google Scholar]
- Vanhaecht, K.; Sermeus, W.; Peers, J.; Lodewijckx, C.; Deneckere, S.; Leigheb, F.; Boonen, S.; Sermon, A.; Boto, P.; Mendes, R.V.; et al. The impact of care pathways for patients with proximal femur fracture: Rationale and design of a cluster-randomized controlled trial. BMC Heal. Serv. Res. 2012, 12, 124. [Google Scholar] [CrossRef] [PubMed]
- Bettamio, V.; Fernandez Del Rio, M.D.P.; Radaelli, G. Miglioramento della qualità del processo terapeutico in ambito ospedaliero. La Scheda Unica di Terapia. QA 2009, 19, 119–124. [Google Scholar]
- Gori, F.; Gori, S. L’infermiere della TIN e l’errore di terapia: Studio trasversale sulle percezioni degli infermieri in tre neonatologie toscane. Giornale Italiano di Scienze Infermieristiche Pediatriche 2009, 1, 31–37. [Google Scholar]
- Ferraresi, A. Qualità delle prescrizioni farmacologiche mediche scritte e orali e prevenzione degli errori: Revisione della letteratura. L’infermiere 2010, 47, 27–36. [Google Scholar]
- D’Ascenzo, P.; Mambelli, T. La somministrazione controllata. Personalizzazione e sicurezza del processo terapeutico in Pediatria. Ter. Pediatr. 2011, 3, 139–141. [Google Scholar]
- Difonzo, M.; Coppolecchia, M.; Colagrande, G. Gli errori da somministrazione di farmaci: Una survey per valutare le percezioni degli infermieri. Settembre 2013, 5, e1000057. [Google Scholar]
- Federici, E. Importanza ed effetti della comunicazione tra utente e struttura sanitaria: I processi cognitivi e decisionali applicati al caso dei programmi di screening oncologico. QA 2011, 21, 12–15. [Google Scholar]
- Fumagalli, C.; Franzosi, L.; Quadrino, S.; Bezze, E.; Colombo, L.; Plevani, L. La comunicazione in TIN: Valutazione della qualità percepita dai genitori mediante il” progetto comunicazione”. Child. Nurses Ital. J. Pediatric Nurs. Sci. 2013, 5, 124–128. [Google Scholar]
- Skela-Savič, B. Nursing care and research: Some factors influencing the development of nursing as a scientific discipline in Slovenia. Obzor Zdr 2009, 43, 209–222. [Google Scholar]
- Bulc, M.; Kersnik, J.; Boerma, W.; Pelny, M. Raziskava o zagotavljanju kakovosti v slovenskem osnovnem zdravstvu. Zdrav Var 2009, 48, 1–17. [Google Scholar]
- Lillo-Crespo, M.; Sierras-Davó, M.C. Quality Improvement with Compassion: Developing Healthcare Improvement Science in the European Health Professions’ Education. In Values of the University in a Time of Uncertainty; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2019; pp. 231–240. [Google Scholar]
- Storey, J. Factors affecting the adoption of quality assurance technologies in healthcare. J. Heal. Organ. Manag. 2013, 27, 498–519. [Google Scholar] [CrossRef]
- Alexander, J.A.; Hearld, L.R. The science of quality improvement implementation: Developing capacity to make a difference. Med Care 2011, 49, 6–20. [Google Scholar] [CrossRef]
- Ogilvie, D.; Craig, P.; Griffin, S.; MacIntyre, S.; Wareham, N.J. A translational framework for public health research. BMC Public Heal. 2009, 9, 116. [Google Scholar] [CrossRef]
- Boström, A.-M.; Slaughter, S.E.; Chojecki, D.; Estabrooks, C.A. What Do We Know About Knowledge Translation in the Care of Older Adults? A Scoping Review. J. Am. Med Dir. Assoc. 2012, 13, 210–219. [Google Scholar] [CrossRef]
- Paynter, R.A. Evidence-based research in the applied social sciences. Ref. Serv. Rev. 2009, 37, 435–450. [Google Scholar] [CrossRef]
- O’Donnell, B.A. Quality Improvement, or Quality Care: An Ethnographic Study of Frontline National Health Service Staff Engagement with a Quality Improvement Initiative. Ph.D. Thesis, University of the West of Scotland, Glasgow, UK, 2018. [Google Scholar]
- Benucci, G.; Carlini, L.; Gallina, G.; Rossi, R.; Lancia, M.; Garippa, M.A.; Suadoni, F.; Pezzulli, S.; Bacci, M.; Conforti, F. Epidemiology of medical errors in a medium size town of central Italy: An investigation of malpractice claims in the period 1997–2004. QA 2009, 19, 166–167. [Google Scholar]
- Salmoiraghi, M.; Delvecchio, G.; Bombana, E.; Valsecchi, D.; Locati, F.; Goglio, A.; Ferrazzi, P.; Giordano, D.; Novellino, L.; Lotti, M.; et al. Profilassi antibiotica perioperatoria: Esperienza sul campo. QA 2009, 19, 115–118. [Google Scholar]
- Di Iorio, B.R.; Bellizzi, V.; Cucciniello, E.; Brogna, A.; Visconti, L.; Pascarella, M.L.; Landolfi, R. Staff Burnout decreases Health Services Efficacy and Effectiveness as well as Patient Satisfaction. QA 2009, 19, 67–74. [Google Scholar]
- Brioschi, D.; Menegon, F.; Alastra, V. Il sistema sperimentale di rilevazione della qualità percepita della degenza presso il Presidio Ospedaliero dell’AslBI. QA 2010, 20, 112–119. [Google Scholar]
- Napoli, V.; Cerullo, F.; Ferri, P. Le qualità distintive del bravo Infermiere secondo i bambini ospedalizzati: Uno studio fenomenologico. Gli Infermieri dei Bambini 2011, 3, 4–6. [Google Scholar]
- Koudriavtseva, T.; Onesti, E.; Pestalozza, I.F.; Sperduti, I.; Jandolo, B. The importance of physician–patient relationship for improvement of adherence to long-term therapy: Data of survey in a cohort of multiple sclerosis patients with mild and moderate disability. Neurol. Sci. 2012, 33, 575–584. [Google Scholar] [CrossRef]
- WHO (World Health Organisation). World Health Statistics; WHO Document Production Services: Geneva, Switzerland, 2013. [Google Scholar]
- Anton, S.G. Financing health care in Romania and implications on the access to health services. USV Ann. Econ. Public Adm. 2013, 12, 195–200. [Google Scholar]
- Vozila, S.; Sorta-Bilajac, I. In Ethical Dilemmas of Nurses and Physiciansin the Primary Health Care Setting. In Proceedings of the 5th International Scientific Conference, Quality Health Care Treatment in the Framework of Education, Research and Multiprofessional Collaboration—Towards the Health of Individuals and the Society, Jesenice, Slovenija, 7–8 June 2012. [Google Scholar]
- Donik, B. How introducing changes and innovations in clinical practice? Obzor Zdr N. 2006, 40, 243–246. [Google Scholar]
- García Mochón, L.; Bermúdez Tamayo, C. Incorporación de nuevas tecnologías en los hospitales españoles. In Informe de Evaluación de Tecnologías Sanitarias; Agencia de Evaluación de Tecnologías Sanitarias de Andalucía (AETSA): Sevilla, Spain, 2011. [Google Scholar]
- Lillo-Crespo, M. Hacia una cultura de seguridad del paciente: El futuro de la profesión de enfermería. Aquichan 2017, 17, 377–379. [Google Scholar] [CrossRef]
- Ilemi, K. An ethnographic approach to the concepts of health and disease in the Turkana tribe: A project to improve the health of the nomads of the Ilemi Triangle, Kenya. Salud Colect. 2016, 12, 173–188. [Google Scholar]
- Øvretveit, J.; Garofalo, L.; Mittman, B. Scaling up improvements more quickly and effectively. Int. J. Qual. Heal. Care 2017, 29, 1–6. [Google Scholar] [CrossRef]
- Ovretveit, J.; Mittman, B.; Rubenstein, L.; Ganz, D.A. Using implementation tools to design and conduct quality improvement projects for faster and more effective improvement. Int. J. Heal. Care Qual. Assur. 2017, 30, 755–768. [Google Scholar] [CrossRef]
- McGaghie, W.C.; Issenberg, S.B.; Barsuk, J.H.; Wayne, D.B. A critical review of simulation-based mastery learning with translational outcomes. Med. Educ. 2014, 48, 375–385. [Google Scholar] [CrossRef]
- Jones, A.; Williams, A.; Carson-Stevens, A. Integrating quality improvement into pre-registration education. Nurs. Stand. 2013, 27, 44–48. [Google Scholar] [CrossRef]
- Brody, A.A.; Galvin, J.E. A review of interprofessional dissemination and education interventions for recognizing and managing dementia. Gerontol. Geriatr. Educ. 2013, 34, 225–256. [Google Scholar] [CrossRef]
- Robinson, L.A.; Levy, J.I. The [R]evolving Relationship Between Risk Assessment and Risk Management. Risk Anal. 2011, 31, 1334–1344. [Google Scholar] [CrossRef]
- NHS. Healthcare Improvement Scotland. Available online: http://www.healthcareimprovementscotland.org/our_work/technologies_and_medicines/programme_resources/medicines_delivery_plan.aspx (accessed on 20 March 2018).
- Burnett, S. Improving Patient Safety: Learning from the Safer Patients Initiative. Health Care Risk Rep. 2009, 16, 16–17. [Google Scholar]
- White, M.; Butterworth, T.; Wells, J.S. Healthcare Quality Improvement and ‘work engagement’; concluding results from a national, longitudinal, cross-sectional study of the ‘Productive Ward-Releasing Time to Care’Programme. BMC Health Serv. Res. 2017, 17, 510. [Google Scholar] [CrossRef]
- Van Bogaert, P.; Clarke, S. The Organizational Context of Nursing Practice: Concepts, Evidence, and Interventions for Improvement; Springer: Cham, Switzerland, 2018. [Google Scholar]
- The Institute for Healthcare Improvement. Science of Improvement. 2018. Available online: http://www.ihi.org/about/Pages/ScienceofImprovement.aspx. (accessed on 2 May 2019).
- The Health Foundation. Available online: https://www.health.org.uk/ (accessed on 5 May 2019).
| Country | Frequency | ||||
|---|---|---|---|---|---|
| Leadership | Improvement | Management | Healthcare Studies | Evidence Based Practice | |
| England | 18/66 | ||||
| Scotland | 2/8 | ||||
| Romania | 9/60 | ||||
| Italy | 7/16 | ||||
| Poland | 10/27 | ||||
| Slovenia | 4/9 | ||||
| Spain | 20/35 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lillo-Crespo, M.; Sierras-Davó, M.C.; Taylor, A.; Ritters, K.; Karapostoli, A. Mapping the Status of Healthcare Improvement Science through a Narrative Review in Six European Countries. Int. J. Environ. Res. Public Health 2019, 16, 4480. https://doi.org/10.3390/ijerph16224480
Lillo-Crespo M, Sierras-Davó MC, Taylor A, Ritters K, Karapostoli A. Mapping the Status of Healthcare Improvement Science through a Narrative Review in Six European Countries. International Journal of Environmental Research and Public Health. 2019; 16(22):4480. https://doi.org/10.3390/ijerph16224480
Chicago/Turabian StyleLillo-Crespo, Manuel, Maria Cristina Sierras-Davó, Alan Taylor, Katrina Ritters, and Aimilia Karapostoli. 2019. "Mapping the Status of Healthcare Improvement Science through a Narrative Review in Six European Countries" International Journal of Environmental Research and Public Health 16, no. 22: 4480. https://doi.org/10.3390/ijerph16224480
APA StyleLillo-Crespo, M., Sierras-Davó, M. C., Taylor, A., Ritters, K., & Karapostoli, A. (2019). Mapping the Status of Healthcare Improvement Science through a Narrative Review in Six European Countries. International Journal of Environmental Research and Public Health, 16(22), 4480. https://doi.org/10.3390/ijerph16224480







