Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
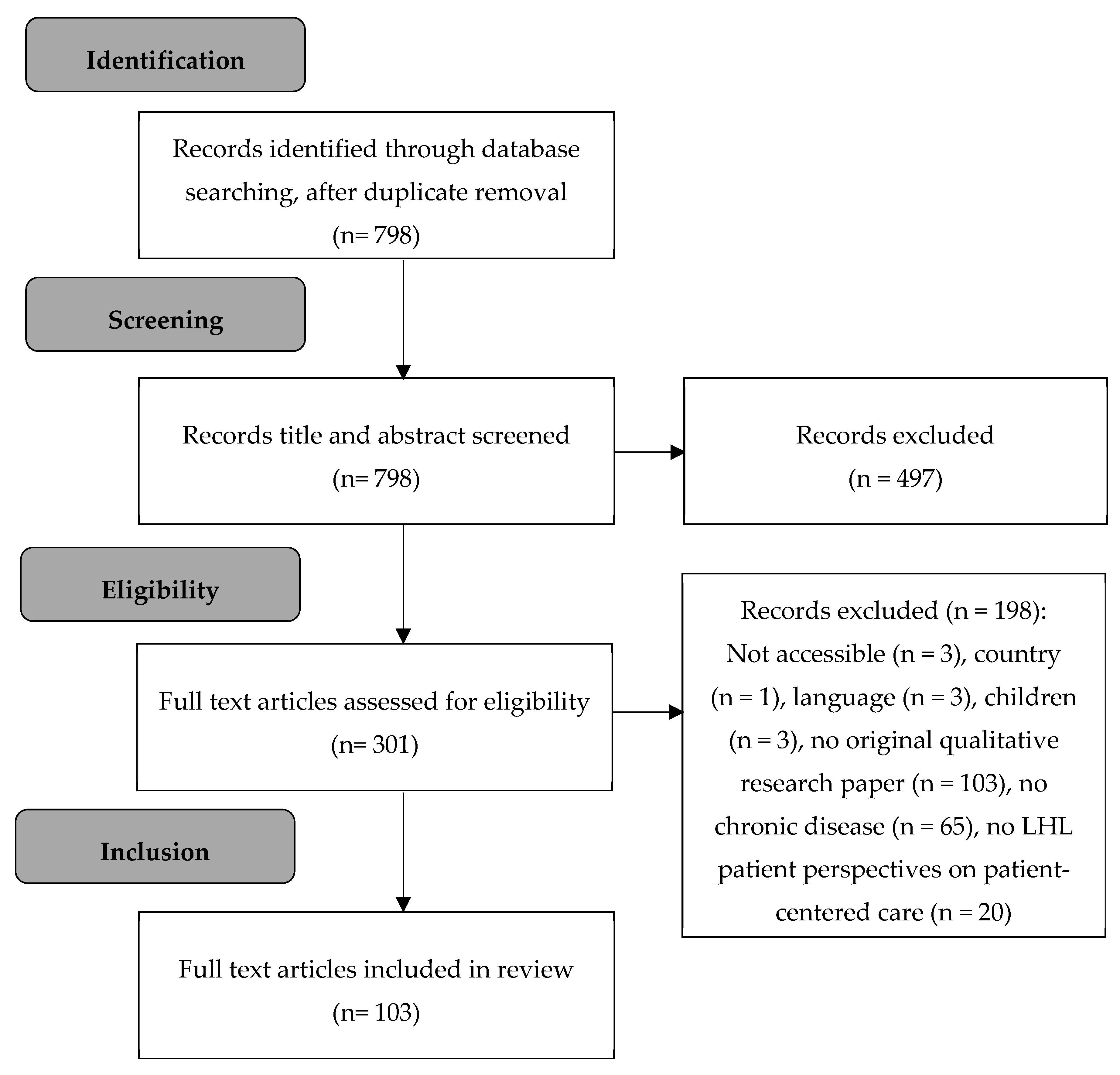
2.3. Selection of Articles
- They provided information on perspectives or experiences related to healthcare of adult participants (18+) with a chronic disease and LHL, described with qualitative research. Participants of all studies will be hereinafter referred to as ‘patients’. We identified patients with LHL as persons who have difficulty in accessing and understanding health information, and in appraising and applying such information in making decisions related to health and healthcare [1].
- Studies were conducted in developed countries (USA, Europe, New Zealand, or Australia).
- They were written in English, Italian, German or Dutch, as these languages were spoken within the research team.
- Experiences of healthy persons with LHL in the general population were described (e.g., articles on screening in the general population).
- They focused on HL research among children or adolescents; articles including participants with a large age range were not included if they did not describe results for adult patients specifically.
- They were research related articles (e.g., articles describing how persons with LHL struggle with informed consent within research or how HL impacts participation in research).
- They focused on perspectives of HCPs on patients with LHL.
2.4. Data-Extraction and Analysis (Phase I)
- “Descriptives”, such as country of study, language of the article, publication year, sample size, setting, study design, objectives or research questions, methods, topic area, target population, HL indicator (if used), type and stage of chronic disease, and type of HCPs (if applicable).
- “Content”, such as key concepts/themes identified, main experiences/ideas of patients, facilitating factors, barriers, quotations for illustration of patients and others, recommendations for healthcare.
2.5. Data-Extraction and Analysis (Phase II)
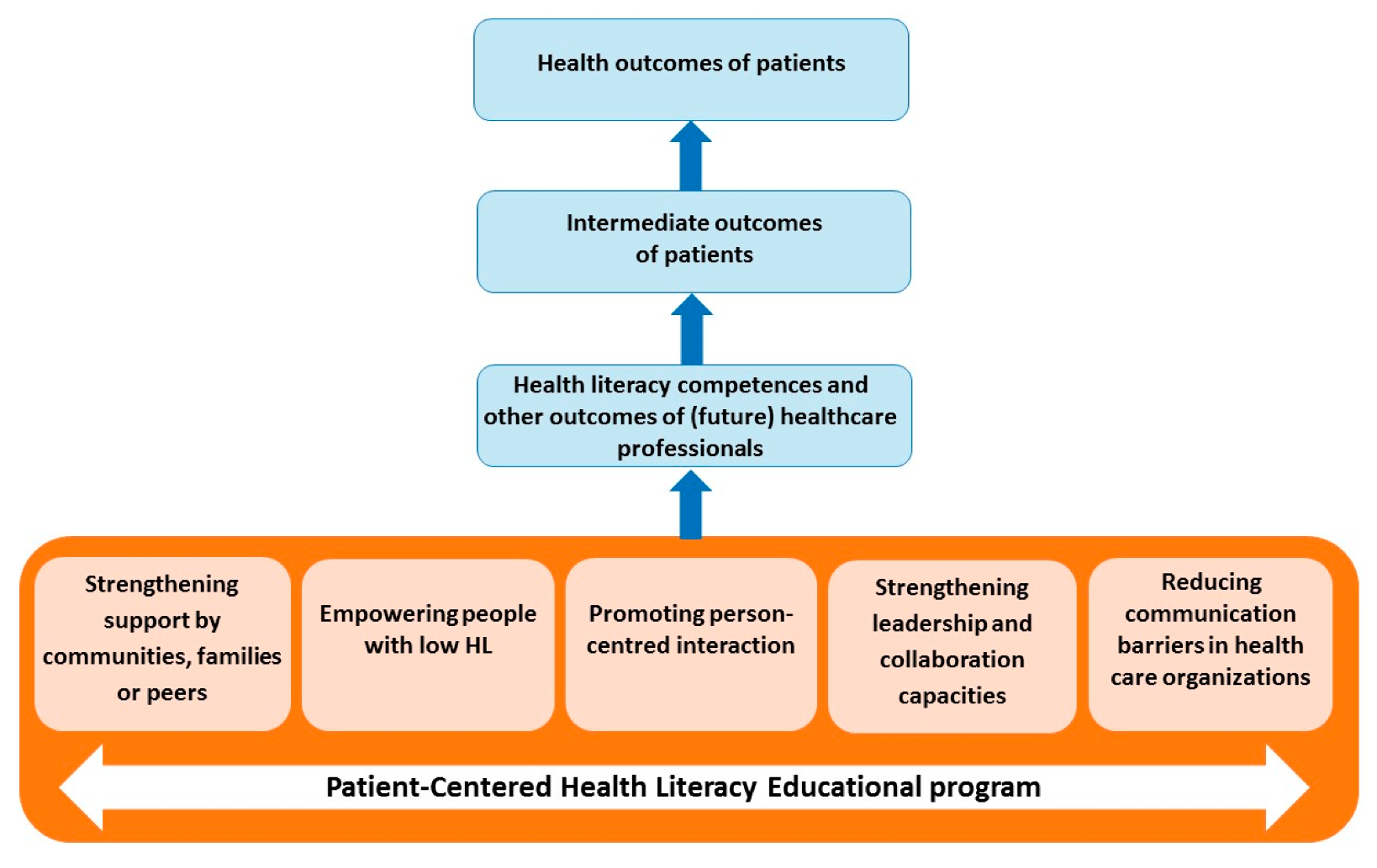
- Support system: defined as the social network of communities, families or peers supporting the patient with LHL.
- Patient empowerment: defined as the inherent capacity to be responsible for maintaining and promoting one’s own health.
- Patient–provider interaction: defined as verbal and non-verbal communication exchanges between HCPs and patients with LHL, as well as everything that might influence the interaction between the patient and the HCP (e.g., perceived time, respect).
- Leadership and collaboration: defined as competencies and actions initiated by a HCP in order to accommodate the patient with LHL (e.g., putting HL on the agenda, interaction between HCPs, and coordination of care).
- Communication barriers: defined as obstacles within the healthcare system that appear to be a barrier for patients with LHL (e.g., written materials, hospital navigation, front desks, hospital websites).
2.6. Development of Learning Outcomes
3. Results
3.1. Descriptives
3.2. Themes
3.3. Support System
3.3.1. Family and Friends
3.3.2. Peer Contact
3.3.3. Religion and Spirituality
3.3.4. Healthcare Provider Support
3.4. Patient Self-Management
3.4.1. Autonomy and Control
3.4.2. Gaining Knowledge
3.4.3. Motivators
3.4.4. Monitoring
3.5. HCPs Interpersonal Capacities
3.5.1. Respect and Understanding
3.5.2. Comprehensible Communication Style
3.5.3. Decision Making
3.6. Barriers in the Healthcare System
3.6.1. Comprehensibility of Medical Documents and Information
3.6.2. Availability and Accessibility of Health Care Providers
3.6.3. Collaboration among Health Sectors and HCPs
3.7. Cultural Sensitivity
3.8. eHealth
Learning Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sørensen, K.; Broucke, S.V.D.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Kwan, B.; Frankish, J.; Rootman, I. The Development and Validation of Measures of “Health Literacy” in Different Populations; Institute of Health Promotion Research, University of British Columbia: West Mall Vancouver, BC, Canada, 2006. [Google Scholar]
- Al Sayah, F.; Majumdar, S.R.; Williams, B.; Robertson, S.; Johnson, J.A. Health literacy and health outcomes in diabetes: A systematic review. J. Gen. Intern. Med. 2013, 28, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Caruso, R.; Magon, A.; Baroni, I.; Dellafiore, F.; Arrigoni, C.; Pittella, F.; Ausili, D. Health literacy in type 2 diabetes patients: A systematic review of systematic reviews. Acta Diabetol. 2018, 55, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Heijmans, M.; Waverijn, G.; Rademakers, J.; van der Vaart, R.; Rijken, M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ. Couns. 2015, 98, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Aboumatar, H.J.; Carson, K.A.; Beach, M.C.; Roter, D.L.; Cooper, L.A. The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension. J. Gen. Intern. Med. 2013, 28, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Geboers, B.; Reijneveld, S.; Koot, J.; de Winter, A. Moving towards a comprehensive approach for health literacy interventions: The development of a health literacy intervention model. Int. J. Environ. Res. Public Health 2018, 15, 1268. [Google Scholar] [CrossRef] [PubMed]
- Brainard, J.; Loke, Y.; Salter, C.; Koós, T.; Csizmadia, P.; Makai, A.; Gács, B.; Szepes, M.; Irohla Consortium. Healthy ageing in Europe: Prioritizing interventions to improve health literacy. BMC Res. Notes 2016, 9, 270. [Google Scholar] [CrossRef]
- Miller, T.A. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ. Couns. 2016, 99, 1079–1086. [Google Scholar] [CrossRef]
- Perazzo, J.; Reyes, D.; Webel, A. A systematic review of health literacy interventions for people living with HIV. AIDS Behav. 2017, 21, 812–821. [Google Scholar] [CrossRef]
- WHO. People-Centred Health Care. A Policy Framework. 2007. Available online: http://www.wpro.who.int/health_services/people_at_the_centre_of_care/documents/ENG-PCIPolicyFramework.pdf (accessed on 4 November 2019).
- Institute of Medicine. Health Literacy: A Prescription to End Confusion; Institute of Medicine: Washington, DC, USA, 2004. [Google Scholar]
- Lambert, M.; Luke, J.; Downey, B.; Crengle, S.; Kelaher, M.; Reid, S.; Smylie, J. Health literacy: Health professionals’ understandings and their perceptions of barriers that Indigenous patients encounter. BMC Health Serv. Res. 2014, 14, 614. [Google Scholar] [CrossRef]
- Kaper, M.S.; Sixsmith, J.; Koot, J.A.; Meijering, L.B.; van Twillert, S.; Giammarchi, C.; Bevilacqua, R.; Barry, M.M.; Doyle, P.; Reijneveld, S.A.; et al. Developing and pilot testing a comprehensive health literacy communication training for health professionals in three European countries. Patient Educ. Couns. 2018, 101, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Saunders, C.; Palesy, D.; Lewis, J. Systematic review and conceptual framework for health literacy training in health professions education. Health Prof. Educ. 2018, 5, 13–29. [Google Scholar] [CrossRef]
- Kaper, M.S.; Reijneveld, S.A.; Van Es, F.D.; De Zeeuw, J.; Almansa, J.; Koot, J.A.R.; De Winter, A.F. Effectiveness of a comprehensive health literacy communication training for medical undergraduates: A randomized controlled trial. 2019. submitted. [Google Scholar]
- Coleman, C.A.; Hudson, S.; Maine, L.L. Health literacy practices and educational competencies for health professionals: A consensus study. J. Health Commun. 2013, 18, 82–102. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, C.; Porrit, K.; Munn, Z.; Rittenmeyer, L.; Salmond, S.; Bjerrum, M.; Loveday, H.; Carrier, J.; Stannard, D. Chapter 2, Systematic Reviews of Qualitative Evidence; Reviewers’ Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Turner, T.; Palazzi, D.; Ward, M.; Lorin, M. The clinician-educator’s handbook. MedEdPORTAL 2010, 6, 7749. [Google Scholar] [CrossRef]
- Reyes, J.; Tripp-Reimer, T.; Parker, E.; Muller, B.; Laroche, H. Factors influencing diabetes self-management among medically underserved patients with type II diabetes. Glob. Qual. Nurs. Res. 2017, 4. [Google Scholar] [CrossRef]
- Bhaloo, T.; Juma, M.; Criscuolo-Higgins, C. A solution-focused approach to understanding patient motivation in diabetes self-management: Gender differences and implications for primary care. Chronic Illn. 2018, 14, 243–255. [Google Scholar] [CrossRef]
- Cervantes, L.; Jones, J.; Linas, S.; Fischer, S. Qualitative Interviews Exploring Palliative Care Perspectives of Latinos on Dialysis. Clin. J. Am. Soc. Nephrol. 2017, 12, 788–798. [Google Scholar] [CrossRef]
- Jacobs, R.J.; Ownby, R.L.; Acevedo, A.; Waldrop-Valverde, D. A qualitative study examining health literacy and chronic illness self-management in Hispanic and non-Hispanic older adults. J. Multidiscip. Healthc. 2017, 10, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.D.; Huntington, S.J.; Satterly, L.; Rubinstein, R.A.; Keefe, R.H.; Amaus Project Student Researchers. Filling out the forms: Health literacy among the uninsured. Soc. Work Health Care 2017, 56, 686–699. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, T.G.; Reyes, D.; Eller, L.; Wantland, D.; Portillo, C.; Holzemer, W.L.; Matshediso, E.; Corless, I.; Kemppainen, J.; Mogobe, K.D.; et al. Understanding Health Literacy for People Living With HIV: Locations of Learning. J. Assoc. Nurses AIDS Care 2018, 29, 190–203. [Google Scholar] [CrossRef] [PubMed]
- Nesoff, E.D.; Brownstein, J.N.; Veazie, M.; O’Leary, M.; Brody, E.A. Time-to-treatment for myocardial infarction: Barriers and facilitators perceived by American Indians in three regions. J. Community Health 2017, 42, 129–138. [Google Scholar] [CrossRef]
- Robotin, M.C.; Porwal, M.; Hopwood, M.; Nguyen, D.; Sze, M.; Treloar, C.; George, J. Listening to the consumer voice: Developing multilingual cancer information resources for people affected by liver cancer. Health Expect. 2017, 20, 171–182. [Google Scholar] [CrossRef]
- Samuels-Kalow, M.; Rhodes, K.; Uspal, J.; Reyes Smith, A.; Hardy, E.; Mollen, C. Unmet needs at the time of emergency department discharge. Acad. Emerg. Med. 2016, 23, 279–287. [Google Scholar] [CrossRef]
- Stirling, C.; Campbell, B.; Bentley, M.; Bucher, H.; Morrissey, M. A qualitative study of patients’ experiences of a nurse-led memory clinic. Dementia 2016, 15, 22–33. [Google Scholar] [CrossRef]
- Shahid, S.; Teng, T.H.; Bessarab, D.; Aoun, S.; Baxi, S.; Thompson, S.C. Factors contributing to delayed diagnosis of cancer among Aboriginal people in Australia: A qualitative study. BMJ Open 2016, 6, e010909. [Google Scholar] [CrossRef]
- Worrall-Carter, L.; Daws, K.; Rahman, M.A.; MacLean, S.; Rowley, K.; Andrews, S.; MacIsaac, A.; Lau, P.M.; McEvedy, S.; Willis, J.; et al. Exploring Aboriginal patients’ experiences of cardiac care at a major metropolitan hospital in Melbourne. Aust. Health Rev. 2016, 40, 696–704. [Google Scholar] [CrossRef]
- Hayden, C.; Neame, R.; Tarrant, C. Patients’ adherence-related beliefs about methotrexate: A qualitative study of the role of written patient information. BMJ Open 2015, 5, e006918. [Google Scholar] [CrossRef]
- Rimando, M. Perceived Barriers to and Facilitators of Hypertension Management among Underserved African American Older Adults. Ethn. Dis. 2015, 25, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.J.; Donnell-Jackson, K.; Jhingan, R.; Golden, S.H.; Paranjape, A. Early readmission among patients with diabetes: A qualitative assessment of contributing factors. J. Diabetes Complicat. 2014, 28, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Tomiak, E.; Samson, A.; Spector, N.; Mackey, M.; Gilpin, C.; Smith, E.; Jonker, D.; Allanson, J.; Asmis, T. Reflex testing for Lynch syndrome: If we build it, will they come? Lessons learned from the uptake of clinical genetics services by individuals with newly diagnosed colorectal cancer (CRC). Fam. Cancer 2014, 13, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Wiley, J.; Westbrook, M.; Long, J.; Greenfield, J.R.; Day, R.O.; Braithwaite, J. Diabetes education: The experiences of young adults with type 1 diabetes. Diabetes Therapy 2014, 5, 299–321. [Google Scholar] [CrossRef]
- Wilkinson, E.; Randhawa, G.; Brown, E.A.; Da Silva Gane, M.; Stoves, J.; Warwick, G.; Akhtar, T.; Magee, R.; Sharman, S.; Farrington, K. Communication as care at end of life: An emerging issue from an exploratory action research study of renal end-of-life care for ethnic minorities in the U.K. J. Ren. Care 2014, 40, 23–29. [Google Scholar] [CrossRef]
- Cohen, M.Z.; Jenkins, D.; Holston, E.C.; Carlson, E.D. Understanding health literacy in patients receiving hematopoietic stem cell transplantation. Oncol. Nurs. Forum 2013, 40, 508–515. [Google Scholar] [CrossRef]
- Donnellan, C.; Martins, A.; Conlon, A.; Coughlan, T.; O’Neill, D.; Collins, D. Mapping patients’ experiences after stroke onto a patient-focused ontervention framework. Disabil. Rehabil. 2013, 35, 483–491. [Google Scholar] [CrossRef]
- Besser, S.J.; Anderson, J.E.; Weinman, J. How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Arch. Osteoporos 2012, 7, 115–124. [Google Scholar] [CrossRef]
- Edwards, M.; Wood, F.; Davies, M.; Edwards, A. The development of health literacy in patients with a long-term health condition: The health literacy pathway model. BMC Public Health 2012, 12, 130. [Google Scholar] [CrossRef]
- Ellis, J.; Mullan, J.; Worsley, A.; Pai, N. The role of health literacy and social networks in arthritis patients’ health information-seeking behavior: A qualitative study. Int. J. Fam. Med. 2012, 2012. [Google Scholar] [CrossRef]
- Shaw, S.J.; Armin, J.; Torres, C.H.; Orzech, K.M.; Vivian, J. Chronic disease self-management and health literacy in four ethnic groups. J. Health Commun. 2012, 17, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Valerio, M.A.; Kanjirath, P.P.; Klausner, C.P.; Peters, M.C. A qualitative examination of patient awareness and understanding of type 2 diabetes and oral health care needs. Diabetes Res. Clin. Pract. 2011, 93, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Jordan, J.E.; Buchbinder, R.; Osborne, R.H. Conceptualising health literacy from the patient perspective. Patient Educ. Couns. 2010, 79, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Longo, D.R.; Schubert, S.L.; Wright, B.A.; LeMaster, J.; Williams, C.D.; Clore, J.N. Health information seeking, receipt, and use in diabetes self-management. Ann. Fam. Med. 2010, 8, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Gakumo, C.A.; Enah, C.C.; Vance, D.E.; Sahinoglu, E.; Raper, J.L. “Keep it simple”: Older African Americans’ preferences for a health literacy intervention in HIV management. Patient Prefer. Adherence 2015, 9, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, S.; Brooks, D.; Goldstein, R.S. Patients’ and providers’ perceptions of the impact of health literacy on communication in pulmonary rehabilitation. Chronic Respir. Dis. 2013, 10, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Herzberg, H.; Bernateck, K.; Welti, F.; Joos, S.; Pohontsch, N.J.; Blozik, E.; Scherer, M. Patient Participation in Development of Quality Indicators using the Example of National Disease Management Guidelines for Chronic Heart Failure—A Qualitative Analysis of Collective Perspectives. Gesundheitswesen 2016, 78, 373–377. [Google Scholar]
- Lamb, E.; Liebl, P.; Köster, M.; Hübner, J. Analyse von Beiträgen im größten deutschen Chatforum für Tumorpatienten zum Thema Palliativmedizin. Tumordiagn Ther. 2016, 37, 509–515. [Google Scholar]
- Whealin, J.M.; Jenchura, E.C.; Wong, A.C.; Zulman, D.M. How veterans with post-traumatic stress disorder and comorbid health conditions use ehealth to manage their health care needs: A mixed-methods analysis. J. Med. Int. Res. 2016, 18, e280. [Google Scholar]
- Lopez-Vargas, P.A.; Tong, A.; Phoon, R.K.; Chadban, S.J.; Shen, Y.; Craig, J.C. Knowledge deficit of patients with stage 1–4 CKD: A focus group study. Nephrology 2014, 19, 234–243. [Google Scholar] [CrossRef]
- Smith, F.; Carlsson, E.; Kokkinakis, D.; Forsberg, M.; Kodeda, K.; Sawatzky, R.; Friberg, F.; Öhlén, J. Readability, suitability and comprehensibility in patient education materials for Swedish patients with colorectal cancer undergoing elective surgery: A mixed method design. Patient Educ. Couns. 2014, 94, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Storni, C. Diabetes self-care in-the-wild: Design challenges for personal health record systems and self-monitoring technologies. Inf. Technol. People 2014, 27, 397–420. [Google Scholar] [CrossRef]
- Khan, S.; Dasrath, F.; Farghaly, S.; Otobo, E.; Riaz, M.S.; Rogers, J.; Castillo, A.; Atreja, A.; Group, H.P.C. Unmet Communication and Information Needs for Patients with IBD: Implications for Mobile Health Technology. Br. J. Med. Med. Res. 2016, 12, 12119. [Google Scholar] [CrossRef]
- Poureslami, I.; Rootman, I.; Doyle-Waters, M.M.; Nimmon, L.; FitzGerald, J.M. Health literacy, language, and ethnicity-related factors in newcomer asthma patients to Canada: A qualitative study. J. Immigr. Minority Health 2011, 13, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Sakraida, T.J.; Robinson, M.V. Health literacy self-management by patients with type 2 diabetes and stage 3 chronic kidney disease. West. J. Nurs. Res. 2009, 31, 627–647. [Google Scholar] [CrossRef] [PubMed]
- Náfrádi, L.; Kostova, Z.; Nakamoto, K.; Schulz, P.J. The doctor–patient relationship and patient resilience in chronic pain: A qualitative approach to patients’ perspectives. Chronic Illn. 2018, 14, 256–270. [Google Scholar] [CrossRef]
- Cotugno, J.D.; Ferguson, M.; Harden, H.; Colquist, S.; Stack, A.A.; Zimmerman, J.I.; Russell, A.W.; Ball, L.E.; Hickman, I.J. “I wish they could be in my shoes”: patients’ insights into tertiary health care for type 2 diabetes mellitus. Patient Prefer. Adherence 2015, 9, 1647–1655. [Google Scholar]
- Plevinsky, J.; Gumidyala, A.; Fishman, L. Transition experience of young adults with inflammatory bowel diseases (IBD): A mixed methods study. Child. Care Health Dev. 2015, 41, 755–761. [Google Scholar] [CrossRef]
- Chen, A.T. The relationship between health management and information behavior over time: A study of the illness journeys of people living with fibromyalgia. J. Med. Internet Res. 2016, 18, e269. [Google Scholar] [CrossRef]
- Brunk, D.R.; Taylor, A.G.; Clark, M.L.; Williams, I.C.; Cox, D.J. A culturally appropriate self-management program for Hispanic adults with type 2 diabetes and low health literacy skills. J. Transcult Nurs. 2017, 28, 187–194. [Google Scholar] [CrossRef]
- Farias, A.J.; Ornelas, I.J.; Hohl, S.D.; Zeliadt, S.B.; Hansen, R.N.; Li, C.I.; Thompson, B. Exploring the role of physician communication about adjuvant endocrine therapy among breast cancer patients on active treatment: A qualitative analysis. Supportive Care Cancer 2017, 25, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Gainer, R.A.; Curran, J.; Buth, K.J.; David, J.G.; Légaré, J.; Hirsch, G.M. Toward optimal decision making among vulnerable patients referred for cardiac surgery: A qualitative analysis of patient and provider perspectives. Med. Decis. Mak. 2017, 37, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Mathiesen, A.S.; Thomsen, T.; Jensen, T.; Schiøtz, C.; Langberg, H.; Egerod, I. The influence of diabetes distress on digital interventions for diabetes management in vulnerable people with type 2 diabetes: A qualitative study of patient perspectives. J. Clin. Transl. Endocrinol. 2017, 9, 41–47. [Google Scholar] [CrossRef] [PubMed]
- McKenna, V.B.; Sixsmith, J.; Barry, M.M. The relevance of context in understanding health literacy skills: Findings from a qualitative study. Health Expect. 2017, 20, 1049–1060. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Chan, A.H. A review of technology acceptance by older adults. Gerontechnology 2011, 10, 1–12. [Google Scholar] [CrossRef]
- Liddy, C.; Johnston, S.; Irving, H.; Nash, K.; Ward, N. Improving awareness, accountability, and access through health coaching: Qualitative study of patients’ perspectives. Can. Fam. Phys. 2015, 61, e158–e164. [Google Scholar]
- Dhanireddy, S.; Walker, J.; Reisch, L.; Oster, N.; Delbanco, T.; Elmore, J.G. The urban underserved: Attitudes towards gaining full access to electronic medical records. Health Expect. 2014, 17, 724–732. [Google Scholar] [CrossRef]
- Melton, C.; Graff, C.; Holmes, G.N.; Brown, L.; Bailey, J. Health literacy and asthma management among African-American adults: An interpretative phenomenological analysis. J. Asthma 2014, 51, 703–713. [Google Scholar] [CrossRef]
- Ladin, K.; Buttafarro, K.; Hahn, E.; Koch-Weser, S.; Weiner, D.E. “End-of-Life Care? I’m not Going to Worry About That Yet.” Health Literacy Gaps and End-of-Life Planning Among Elderly Dialysis Patients. Gerontologist 2017, 58, 290–299. [Google Scholar] [CrossRef]
- Parekh, N.; Jiang, J.; Buchan, M.; Meyers, M.; Gibbs, H.; Krebs, P. Nutrition literacy among cancer survivors: Feasibility results from the Healthy Eating and Living Against Breast Cancer (HEAL-BCa) study: A pilot randomized controlled trial. J. Cancer Educ. 2018, 33, 1239–1249. [Google Scholar] [CrossRef]
- Schumacher, J.R.; Lutz, B.J.; Hall, A.G.; Pines, J.M.; Jones, A.L.; Hendry, P.; Kalynych, C.; Carden, D.L. Feasibility of an ED-to-Home Intervention to Engage Patients: A Mixed-Methods Investigation. West. J. Emerg. Med. 2017, 18, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Hawk, M.; Coulter, R.W.; Egan, J.E.; Friedman, M.R.; Meanley, S.; Fisk, S.; Watson, C.; Kinsky, S. Exploring the Healthcare Environment and Associations with Clinical Outcomes of People Living with HIV/AIDS. AIDS Patient Care STDs 2017, 31, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.; Zúñiga, M.L.; Peacher, D.; Palomino, H.; Watson, M. Efficacy of cancer care communication between clinicians and Latino patients in a rural US-Mexico border region: A qualitative study of barriers and facilitators to better communication. J. Cancer Educ. 2018, 33, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.P.; Beune, E.J.; Baim-Lance, A.M.; Bruessing, R.C.; Essink-Bot, M. Diabetes self-management support for patients with low health literacy: Perceptions of patients and providers. J. Diabetes 2015, 7, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Prakash, S.; McGrail, A.; Lewis, S.A.; Schold, J.; Lawless, M.E.; Sehgal, A.R.; Perzynski, A.T. Behavioral stage of change and dialysis decision-making. Clin. J. Am. Soc. Nephrol. 2015, 10, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Schook, R.M.; Linssen, C.; Schramel, F.M.; Festen, J.; Lammers, E.; Smit, E.F.; Postmus, P.E.; Westerman, M.J. Why do patients and caregivers seek answers from the Internet and online lung specialists? A qualitative study. J. Med. Internet Res. 2014, 16, e37. [Google Scholar] [CrossRef]
- McDougald Scott, A.M.; Jackson, G.P.; Ho, Y.X.; Yan, Z.; Davison, C.; Rosenbloom, S.T. Adapting comparative effectiveness research summaries for delivery to patients and providers through a patient portal. AMIA Annu. Symp. Proc. 2013, 2013, 959–968. [Google Scholar]
- Wortz, K.; Cade, A.; Menard, J.R.; Lurie, S.; Lykens, K.; Bae, S.; Jackson, B.; Su, F.; Singh, K.; Coultas, D. A qualitative study of patients’ goals and expectations for self-management of COPD. Prim. Care Respir. J. 2012, 21, 384. [Google Scholar] [CrossRef]
- Haslbeck, J.; Schaeffer, D. Selbstverantwortung im Gesundheitswesen, diskutiert am Medikamentenmanagement aus Sicht chronisch kranker Patienten. Das. Gesundh. 2011, 73, e44–e50. [Google Scholar] [CrossRef]
- Winston, R.A.; Shaya, F.T.; Pradel, F.G.; Laird, A.; Saunders, E. Barriers to self-management of diabetes: A qualitative study among low-income minority diabetics. Ethn. Dis. 2011, 21, 27. [Google Scholar]
- Renfrew, M.R.; Taing, E.; Cohen, M.J.; Betancourt, J.R.; Pasinski, R.; Green, A.R. Barriers to care for Cambodian patients with diabetes: Results from a qualitative study. J. Health Care Poor Underserved 2013, 24, 633–655. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Hayes, E.M.; Fish, A.; Daskivich, L.P.; Ogunyemi, O.I. Understanding the Knowledge Gap Experienced by U.S. Safety Net Patients in Teleretinal Screening. AMIA Annu. Symp. Proc. 2017, 2016, 590–599. [Google Scholar] [PubMed]
- Holtzman, C.W.; Shea, J.A.; Glanz, K.; Jacobs, L.M.; Gross, R.; Hines, J.; Mounzer, K.; Samuel, R.; Metlay, J.P.; Yehia, B.R. Mapping patient-identified barriers and facilitators to retention in HIV care and antiretroviral therapy adherence to Andersen’s Behavioral Model. AIDS Care 2015, 27, 817–828. [Google Scholar] [CrossRef]
- Horevitz, E.; Organista, K.C.; Arean, P.A. Depression treatment uptake in integrated primary care: How a “warm handoff” and other factors affect decision making by Latinos. Psychiatr. Serv. 2015, 66, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Tieu, L.; Sarkar, U.; Schillinger, D.; Ralston, J.D.; Ratanawongsa, N.; Pasick, R.; Lyles, C.R. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: A qualitative study. J. Med. Internet Res. 2015, 17, e275. [Google Scholar] [CrossRef] [PubMed]
- Salter, C.; Brainard, J.; McDaid, L.; Loke, Y. Challenges and opportunities: What can we learn from patients living with chronic musculoskeletal conditions, health professionals and carers about the concept of health literacy using qualitative methods of inquiry? PLoS ONE 2014, 9, e112041. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Donate, A.P.; Halverson, J.; Simon, N.; Strickland, J.S.; Trentham-Dietz, A.; Smith, P.D.; Linskens, R.; Wang, X. Identifying health literacy and health system navigation needs among rural cancer patients: Findings from the Rural Oncology Literacy Enhancement Study (ROLES). J. Cancer Educ. 2013, 28, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Jowsey, T.; Yen, L.; Wells, R.; Leeder, S. National Health and Hospital Reform Commission final report and patient-centred suggestions for reform. Aust. J. Prim. Health 2011, 17, 162–168. [Google Scholar] [CrossRef]
- Dailey, R.; Schwartz, K.L.; Binienda, J.; Moorman, J.; Neale, A.V. Challenges in making therapeutic lifestyle changes among hypercholesterolemic African-American patients and their physicians. J. Natl. Med. Assoc. 2006, 98, 1895. [Google Scholar] [PubMed]
- Baars, J.; van Dulmen, A.; Velthuizen, M.; van Riel, E.; Ausems, M. Breast cancer genetic counseling among Dutch patients from Turkish and Moroccan descent: Participation determinants and perspectives of patients and healthcare professionals. J. Community Genet. 2017, 8, 97–108. [Google Scholar] [CrossRef][Green Version]
- Schnitzler, L.; Smith, S.K.; Shepherd, H.L.; Shaw, J.; Dong, S.; Carpenter, D.M.; Nguyen, F.; Dhillon, H.M. Communication during radiation therapy education sessions: The role of medical jargon and emotional support in clarifying patient confusion. Patient Educ. Couns. 2017, 100, 112–120. [Google Scholar] [CrossRef]
- Dawson-Rose, C.; Cuca, Y.P.; Webel, A.R.; Báez, S.S.S.; Holzemer, W.L.; Rivero-Méndez, M.; Eller, L.S.; Reid, P.; Johnson, M.O.; Kemppainen, J.; et al. Building trust and relationships between patients and providers: An essential complement to health literacy in HIV care. J. Assoc. Nurses AIDS Care 2016, 27, 574–584. [Google Scholar] [CrossRef] [PubMed]
- McKillop, G.; Joy, J. Patients’ experience and perceptions of polypharmacy in chronic kidney disease and its impact on adherent behaviour. J. Ren. Care 2013, 39, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Sevilla, C.; Wieslander, C.K.; Alas, A.N.; Dunivan, G.C.; Khan, A.A.; Maliski, S.L.; Rogers, R.G.; Anger, J.T. Communication between physicians and Spanish-speaking Latin American women with pelvic floor disorders: A cycle of misunderstanding? Female Pelvic. Med. Reconstr. Surg. 2013, 19, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Raven, M.C.; Gillespie, C.C.; DiBennardo, R.; Van Busum, K.; Elbel, B. Vulnerable patients’ perceptions of health care quality and quality data. Med. Decis. Mak. 2012, 32, 311–326. [Google Scholar] [CrossRef]
- Shaw, A.; Ibrahim, S.; Reid, F.; Ussher, M.; Rowlands, G. Patients’ perspectives of the doctor–patient relationship and information giving across a range of literacy levels. Patient Educ. Couns. 2009, 75, 114–120. [Google Scholar] [CrossRef]
- Joseph, G.; Pasick, R.J.; Schillinger, D.; Luce, J.; Guerra, C.; Cheng, J.K.Y. Information mismatch: Cancer risk counseling with diverse underserved patients. J. Genet. Couns. 2017, 26, 1090–1104. [Google Scholar] [CrossRef]
- Browne, K.; Divilly, D.; McGarry, M.; Sweeney, C.; Kelly, M.E. Chronic Disease Management—The Patient’s Perspective. Ir. Med. J. 2017, 110, 511. [Google Scholar]
- Gakumo, C.A.; Raper, J.L.; Cerice, D.K.; Stand-Gravois, M.J.; Mugavero, M.J. A Qualitative Study on Health Numeracy and Patient–Provider Communication of Laboratory Numbers in Older African Americans with HI.V. J. Assoc. Nurses AIDS Care 2016, 27, 826–834. [Google Scholar] [CrossRef]
- Bachmann, V.; Volkner, M.; Bosnerr, S.; Donner-Banzhoff, N. The experiences of Russian-speaking migrants in primary care consultations. Dtsch Arztebl Int. 2014, 111, 871–876. [Google Scholar] [CrossRef]
- Barker, K.L.; Reid, M.; Minns Lowe, C.J. What does the language we use about arthritis mean to people who have osteoarthritis? A qualitative study. Disabil. Rehabil. 2014, 36, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, M.A.; Swanson, V.; Pappas, E.; O’Carroll, R.E.; Holdsworth, R.J. Illness beliefs and walking behavior after revascularization for intermittent claudication: A qualitative study. J. Cardiopulm. Rehabil. Prev. 2014, 34, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.; Bukulatjpi, S.; Sharma, S.; Davis, J.; Johnston, V. “Only your blood can tell the story”—A qualitative research study using semi-structured interviews to explore the hepatitis B related knowledge, perceptions and experiences of remote dwelling Indigenous Australians and their health care providers in northern Australia. BMC Public Health 2014, 14, 1233. [Google Scholar]
- Griffiths, H.; Davies, R. Understanding Barrett’s columnar lined oesophagus from the patients’ perspective: Qualitative analysis of semistructured interviews with patients. Frontline Gastroenterol. 2011, 2, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.L.; Nissim, H.A.; Le, T.X.; Khan, A.; Maliski, S.L.; Litwin, M.S.; Sarkisian, C.A.; Raz, S.; Rodríguez, L.V.; Anger, J.T. Misconceptions and miscommunication among aging women with overactive bladder symptoms. Urology 2011, 77, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Kenning, C.; Protheroe, J.; Gray, N.; Ashcroft, D.; Bower, P. The potential for using a Universal Medication Schedule (UMS) to improve adherence in patients taking multiple medications in the UK: A qualitative evaluation. BMC Health Serv. Res. 2015, 15, 94. [Google Scholar] [CrossRef] [PubMed]
- Izard, J.; Hartzler, A.; Avery, D.I.; Shih, C.; Dalkin, B.L.; Gore, J.L. User-centered design of quality of life reports for clinical care of patients with prostate cancer. Surgery 2014, 155, 789–796. [Google Scholar] [CrossRef]
- Kennedy, A.; Rogers, A.; Blickem, C.; Daker-White, G.; Bowen, R. Developing cartoons for long-term condition self-management information. BMC Health Serv. Res. 2014, 14, 60. [Google Scholar] [CrossRef]
- Pavlik, V.; Brown, A.E.; Nash, S.; Gossey, J.T. Association of patient recall, satisfaction, and adherence to content of an electronic health record (EHR)-generated after visit summary: A randomized clinical trial. J. Am. Board Fam. Med. 2014, 27, 209–218. [Google Scholar] [CrossRef]
- Papadimitriou, C.; Magasi, S.; DeMark, H.; Taylor, C.; Wolf, M.S.; Heinemann, A.W.; Deutsch, A. Eliciting patient and caregiver perspectives to improve the public reporting of rehabilitation quality measures. Rehabil. Nurs. 2013, 38, 24–31. [Google Scholar] [CrossRef]
- Treloar, C.; Gray, R.; Brener, L.; Jackson, C.; Saunders, V.; Johnson, P.; Harris, M.; Butow, P.; Newman, C. Health literacy in relation to cancer: Addressing the silence about and absence of cancer discussion among A boriginal people, communities and health services. Health Soc. Care Community 2013, 21, 655–664. [Google Scholar] [CrossRef] [PubMed]
- Ameling, J.M.; Auguste, P.; Ephraim, P.L.; Lewis-Boyer, L.; DePasquale, N.; Greer, R.C.; Crews, D.C.; Powe, N.R.; Rabb, H.; Boulware, L.E. Development of a decision aid to inform patients’ and families’ renal replacement therapy selection decisions. BMC Med. Inf. Decis. Mak. 2012, 12, 140. [Google Scholar] [CrossRef] [PubMed]
- Shue, C.K.; O’Hara, L.L.; Marini, D.; McKenzie, J.; Schreiner, M. Diabetes and low-health literacy: A preliminary outcome report of a mediated intervention to enhance patient-physician communication. Commun. Educ. 2010, 59, 360–373. [Google Scholar] [CrossRef]
- Burke, N.J.; Napoles, T.M.; Banks, P.J.; Orenstein, F.S.; Luce, J.A.; Joseph, G. Survivorship care plan information needs: Perspectives of safety-net breast cancer patients. PLoS ONE 2016, 11, e0168383. [Google Scholar] [CrossRef]
- Kaplan, C.P.; Napoles, A.; Davis, S.; Lopez, M.; Pasick, R.J.; Livaudais-Toman, J.; Pérez-Stable, E.J. Latinos and Cancer Information: Perspectives of Patients, Health Professionals and Telephone Cancer Information Specialists. J. Health Disparities Res. Pract. 2016, 9, 154–167. [Google Scholar]
- Knight, B.A.; McIntyre, H.D.; Hickman, I.J.; Noud, M. Qualitative assessment of user experiences of a novel smart phone application designed to support flexible intensive insulin therapy in type 1 diabetes. BMC Med. Inf. Decis. Mak. 2016, 16, 119. [Google Scholar] [CrossRef]
- Sieck, C.J.; Hefner, J.L.; Schnierle, J.; Florian, H.; Agarwal, A.; Rundell, K.; McAlearney, A.S. The rules of engagement: Perspectives on secure messaging from experienced ambulatory patient portal users. JMIR Med. Inf. 2017, 5, e13. [Google Scholar] [CrossRef]
- Van der Vaart, R.; Drossaert, C.H.; de Heus, M.; Taal, E.; van de Laar, M.A. Measuring actual eHealth literacy among patients with rheumatic diseases: A qualitative analysis of problems encountered using Health 1.0 and Health 2.0 applications. J. Med. Internet Res. 2013, 15, e27. [Google Scholar] [CrossRef]
- Hopmans, W.; Damman, O.C.; Timmermans, D.R.; Haasbeek, C.J.; Slotman, B.J.; Senan, S. Communicating cancer treatment information using the Web: Using the patient’s perspective in website development. BMC Med. Inf. Decis. Mak. 2014, 14, 116. [Google Scholar] [CrossRef]
- Karuranga, S.; Sørensen, K.; Coleman, C.; Mahmud, A.J. Health literacy competencies for European health care personnel. HLRP 2017, 1, e247–e256. [Google Scholar] [CrossRef]
- Coleman, C.; Hudson, S.; Pederson, B. Prioritized health literacy and clear communication practices for health care professionals. HLRP 2017, 1, e91–e99. [Google Scholar] [CrossRef] [PubMed]
- Lie, D.; Carter-Pokras, O.; Braun, B.; Coleman, C. What do health literacy and cultural competence have in common? Calling for a collaborative health professional pedagogy. J. Health Commun. 2012, 17, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Smedley, B.D.; Stith, A.Y.; Nelson, A.R. Interventions: Cross-cultural education in the health professions. In Anonymous Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; National Academies Press (US): Washington, DC, USA, 2003. [Google Scholar]
- Baur, C. Calling the nation to act: Implementing the national action plan to improve health literacy. Nurs. Outlook 2011, 59, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Andrulis, D.P.; Brach, C. Integrating literacy, culture, and language to improve health care quality for diverse populations. Am. J. Health Behav. 2007, 31, S122–S133. [Google Scholar] [CrossRef] [PubMed]
- Day, K.; Gu, Y. Influencing factors for adopting personal health record (PHR). Stud Health Technol. Inform. 2012, 178, 39–44. [Google Scholar] [PubMed]
- Noblin, A.M.; Wan, T.T.; Fottler, M. The impact of health literacy on a patient’s decision to adopt a personal health record. Perspect. Health Inf. Manag. 2012, 9, 1–13. [Google Scholar] [PubMed]
- Manganello, J.; Gerstner, G.; Pergolino, K.; Graham, Y.; Falisi, A.; Strogatz, D. The relationship of health literacy with use of digital technology for health information: Implications for public health practice. J. Public Health Manag. Pract. 2017, 23, 380–387. [Google Scholar] [CrossRef]
- Denniston, C.; Molloy, E.; Nestel, D.; Woodward-Kron, R.; Keating, J.L. Learning outcomes for communication skills across the health professions: A systematic literature review and qualitative synthesis. BMJ Open 2017, 7, e014570. [Google Scholar] [CrossRef]
- Leung, L. Validity, reliability, and generalizability in qualitative research. J. Fam. Med. Prim. Care 2015, 4, 324–327. [Google Scholar] [CrossRef]
| Study Characteristics | N | % | |
|---|---|---|---|
| Countries | |||
| USA | 54 | 51.9 | |
| UK | 13 | 12.5 | |
| Australia | 14 | 13.5 | |
| Canada | 5 | 4.8 | |
| Germany | 4 | 3.8 | |
| Netherlands | 5 | 4.8 | |
| Denmark | 1 | 1.0 | |
| Ireland | 3 | 2.9 | |
| Switzerland | 1 | 1.0 | |
| Sweden | 1 | 1.0 | |
| More than one country | 3 | 2.9 | |
| Qualitative methodology | |||
| Interviews | 63 | 61.2 | |
| Focus groups | 27 | 26.2 | |
| Interviews and focus groups | 7 | 6.8 | |
| Type of chronic disease of the participants included in the study | |||
| Diabetes | 21 | 21.6 | |
| Cancer | 18 | 18.5 | |
| Cardiovascular diseases (including stroke, hypercholesterolemia, hypertension, peripheral artery disease) | 15 | 15.5 | |
| Chronic kidney disease | 8 | 8.2 | |
| Musculosketal diseases (Arthritis/rheumatism; fibromyalgia; osteoporosis/osteopenia) | 7 | 7.2 | |
| HIV/AIDS | 7 | 7.2 | |
| Multiple chronic diseases within one study | 7 | 7.2 | |
| Gastroenterological diseases (Barrett’s columnar lined esophagus (CLO); Inflammatory bowel disease; Hepatitis B) | 6 | 6.1 | |
| Respiratory disease (Asthma/COPD) | 6 | 6.1 | |
| Other (chronic pain, disorders of the hematopoietic system) | 4 | 4.1 | |
| Mental health (depression, cognitive impairment) | 2 | 2.1 | |
| Urinary incontinence (overactive bladder symptoms, pelvic organ prolapse/urinary incontinence) | 2 | 2.1 | |
| Theme | Frequency of Occurrence (n) |
|---|---|
| Support system | 42 |
| Patient self-management | 60 |
| Health care providers’ interpersonal capacities | 62 |
| Barriers in healthcare systems | 34 |
| Themes and Sub-Themes | Example Quotations | Articles 1 | |
|---|---|---|---|
| Support system | |||
| Family and Friends | “It helps if you have someone eating along with you saying don’t eat this or don’t eat that. My sister encourages me to buy healthy food like I buy wheat noodles instead of regular noodles.” [22] | [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48] | |
| Peer contact | “[..] They [other patients] can better inform you that as far as, versus a health provider that does not have the disease; they know how to treat the disease, but living with it is, is, you know, a different story.” [49] | [27,29,38,40,46,49,50,51,52,53,54,55,56,57,58] | |
| Religion and Spirituality | “So anyway, I went to the doctor […] we sat and we talked […] with all of the information that I received. Then I just thought. I said, “Listen, Alma, you’re a big girl, and these things happen.” I just began talking to myself, and I’m a believer in God. I just said I’m gonna put it in his hands. Whatever happens, whatever the diagnosis, if I have to have the mastectomy or whatever has to be done, I’m just gonna go ahead and have it done […] take your burden to the Lord and leave it there. I just really believe that God hears, and he answers prayers.” [25] | [25,32,40] | |
| Healthcare provider support | “I like the provider when he or she is concerned with me and the results and didn’t just turn their back and say “Oh, this is serious” and shut up.” [59] | [22,23,26,35,39,40,41,48,53,57,59,60,61,62] | |
| Patient self-management | |||
| Autonomy and control | “It took me a long time to be the manager of my own health system. I expected doctors to kind of manage my life for me. It took me a long time to realize that no, I’m in charge of this. The doctors that work for me are a team, and I manage that team.” [63] | [25,36,41,48,54,60,64,65,66,67,68,69,70,71,72] | |
| Gaining knowledge | “The only way I’m able to cope is to have knowledge, which [doctors] think, if you don’t know, that’s how you’re going to be able to cope.” [73] | [22,25,30,31,34,35,37,38,44,46,48,52,54,55,56,71,73,74,75,76,77,78,79,80,81,82,83,84,85] | |
| Motivators | “The group leader has told us do it [control our blood sugar levels] for your [own] health and do it for your son. I don’t want my child to have this [diabetes]. I feel bad about having diabetes, having to take medications, worrying about what [to] eat . . . and sometimes get [ting] upset [because you don’t want your child to have diabetes]. I want to do whatever I can do to need less medication. We have to do our part.” [64] | [23,35,61,64,68,70,75,78,86,87,88,89,90,91,92,93] | |
| Monitoring | “… I know I’m working with someone that has access to my information and my dietary habits and what not, then that will mean that I’m going to try and stay within my dietary, good dietary, habits” [70] | [32,43,53,55,57,70,87,89] | |
| Healthcare providers’ interpersonal capacities | |||
| Showing respect and understanding | “I didn’t feel like they were really interested. They were just talking… I just want my doctor to recognize who I am.. and they say: well let’s see how you doing.” [72] “The doctor understands me, devotes his time and listens to me. The patient also needs this aspect: to develop trust, to have a human relationship with the physician.” [60] “He [oncologist] knew me by my name, my face. When I came in, it was like they treated you like you were a person and not just cattle coming through. He used to call me his most delicate patient.” [65] | [22,23,28,30,31,42,48,50,52,57,59,60,61,62,65,68,72,76,77,87,88,90,91,94,95,96,97,98,99,100] | |
| Comprehensible communication | “[The doctor] was rattling off all these things that I needed to do…and my brain just shuts off. It was overload.” [91] “It’s the ability to explain in simple terms and not be abstruse. To say look, on the list here it says you’re to have 15 g of carbohydrates. Now that’s a slice of bread or that’s a medium sized potato.” [92] “I really didn’t pick up too much. I just feel that sometimes doctors go in and they’re using all these words and stuff. No. Tell me layman’s terms, because I’m not dumb, but something like that I don’t really understand.” [101] | [24,29,30,31,34,41,42,43,46,48,50,57,65,66,68,72,76,80,83,86,91,92,95,98,101,102,103,104,105,106,107,108,109] | |
| Enabling shared decision-making | “I know what each one of those pills are, what they’re for. I know that because I’m involved with my treatment, you know? Me and the doctor, we actually sit down and talk about me. I ask questions, you know? I’ve learned a lot. I mean, I’ve learned so much, really.” [76] | [34,37,38,43,56,60,62,65,66,70,73,76,79,83,91,100,101] | |
| Barriers in health care systems | |||
| Comprehensibility of medical documents and information | “There’s too much jargon (in health leaflets) they’re not written for lay people”. [100] | [26,30,33,36,46,50,55,58,66,92,100,110,111,112,113,114,115,116,117] | |
| Availability and accessibility of healthcare providers | “[My] doctor would [not be able to see me at] ‘that particular time of day,’ so [I] just went on to emergency.” [75] | [31,33,36,47,52,61,75,87,88] | |
| Collaboration among health sectors and healthcare providers | “I had the pharmacist at the hospital phone me to double check I was having blood tests regularly and ask if everything had been explained to me and they double checked.” [43] “I think it would help more if we saw the same person every time, if possible. Because you go in there and you think, well, do they know all about me?” [90] | [23,43,62,68,87,90,92,102,118] | |
| Cultural sensitivity | |||
| “…If you take the herbals you must put the medicines aside. If you take the medicines, you must leave the herbals aside.” [85] “I can say majority (sic) of the printed information is in English and the medical terminologies are very difficult for me to understand.” [58] | [22,24,28,29,32,33,39,46,58,85,88,90,92,94,104,107,119] | ||
| eHealth | |||
| “I have relied on the Internet in the sense of making contact with other patients with the same disease in the world” [50] “What I love…was that it told me how much to have and I didn’t overeat. The number of times that I overeat from hypos is ridiculous; it would be 99 % of times.” [120] “About the email, the one thing that I really like is that the doctor has always got somebody waiting for him, so the nurses are the ones that were logging in to the email and doing the routing of the-and letting him know what’s going on, what the-and I really like that ! That’s the sort of addresses the issue that you brought up.” [53] | [27,29,34,38,40,50,52,53,56,57,67,71,72,89,110,120,121,122] | ||
| Themes | Learning Outcomes |
|---|---|
| Key themes | |
| Promoting person-centred care | Students should be able to… demonstrate a positive attitude towards person-centeredness and person-centred behaviours. … provide an overview of different communication goals and understand what these mean for the patient and the care process. … apply the concept of person-centred care and how to integrate this into practice. |
| Support system | Students should be able to… … explain the relevance, benefits, and potential negative impact of the involvement of family members, friends, peers and healthcare providers (support system) in the patient’s care process. … demonstrate the ability to identify the patient’s needs and preferences for the involvement of their support system. … demonstrate the ability to involve family members and friends based on individual patient’s needs and preferences. …recognize when a patient is facing a lack of support due to life circumstances. …reflect on their own support practices in order to improve these in patient care. |
| Patient self-management | Students should be able to… … provide patients with information (sources) that are understandable, reliable, relevant, accessible, and practically applicable. … appraise monitoring systems and positive accountability to promote patient-related outcomes (e.g., motivation, self-management skills). |
| Healthcare providers’ interpersonal capacities | Students should be able to… … demonstrate the ability to develop a positive provider-patient relationship based on mutual understanding and trust. … appraise the importance of comprehensible and comprehensive information. … translate medical information into easily and understandable information for patients to help them explore preferences and make decisions. … demonstrate the ability to use patients’ needs and preferences as the frame of reference for information exchange and making healthcare decisions. … recognize the influence of discontinuity of care at patient level. |
| Barriers in health care systems | Students should be able to… … explain the relevance of comprehensible written information for patients’ knowledge, motivation, participation and other outcomes. … understand the added value of information material such as images and videos to increase patient understanding and include this in their consultations. … initiate and support developments to enhance the comprehensibility of information provision in their health organization. … judge the importance to collaborate and communicate with fellow providers to ensure continuity of care. … demonstrate the ability to support patients struggling with the healthcare system and assist them in navigating it. |
| Recurring themes | |
| Cultural sensitivity | Students should be able to… … understand cultural health beliefs and norms, family values and decision-making, and language, … apply their knowledge of cultural aspects in the care process to by tailoring their communication to patients’ needs and preferences. … be aware of the beliefs and norms of the most prominent cultures/ethnicities in their work area. … communicate in a culturally sensitive way taking into account patients’ needs and preferences, e.g., by providing written information sources in their own native language, or facilitate the presence of an interpreter during the consultations. |
| eHealth | Students should be able to… … value the benefits of eHealth as an additional source of information and support. … facilitate the use of eHealth and integrate this in prevention and care. … provide patients with relevant information about eHealth tools beneficial for their specific care process. … value the latest developments on eHealth. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jager, M.; de Zeeuw, J.; Tullius, J.; Papa, R.; Giammarchi, C.; Whittal, A.; de Winter, A.F. Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies. Int. J. Environ. Res. Public Health 2019, 16, 4300. https://doi.org/10.3390/ijerph16214300
Jager M, de Zeeuw J, Tullius J, Papa R, Giammarchi C, Whittal A, de Winter AF. Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies. International Journal of Environmental Research and Public Health. 2019; 16(21):4300. https://doi.org/10.3390/ijerph16214300
Chicago/Turabian StyleJager, Margot, Janine de Zeeuw, Janne Tullius, Roberta Papa, Cinzia Giammarchi, Amanda Whittal, and Andrea F. de Winter. 2019. "Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies" International Journal of Environmental Research and Public Health 16, no. 21: 4300. https://doi.org/10.3390/ijerph16214300
APA StyleJager, M., de Zeeuw, J., Tullius, J., Papa, R., Giammarchi, C., Whittal, A., & de Winter, A. F. (2019). Patient Perspectives to Inform a Health Literacy Educational Program: A Systematic Review and Thematic Synthesis of Qualitative Studies. International Journal of Environmental Research and Public Health, 16(21), 4300. https://doi.org/10.3390/ijerph16214300





