The Low Prevalence of Overweight and Obesity in Czech Breastfed Infants and Young Children: An Anthropological Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Recruitment and Data Collection
2.2. Czech References
2.3. Statistical Analysis
2.4. Ethical Considerations
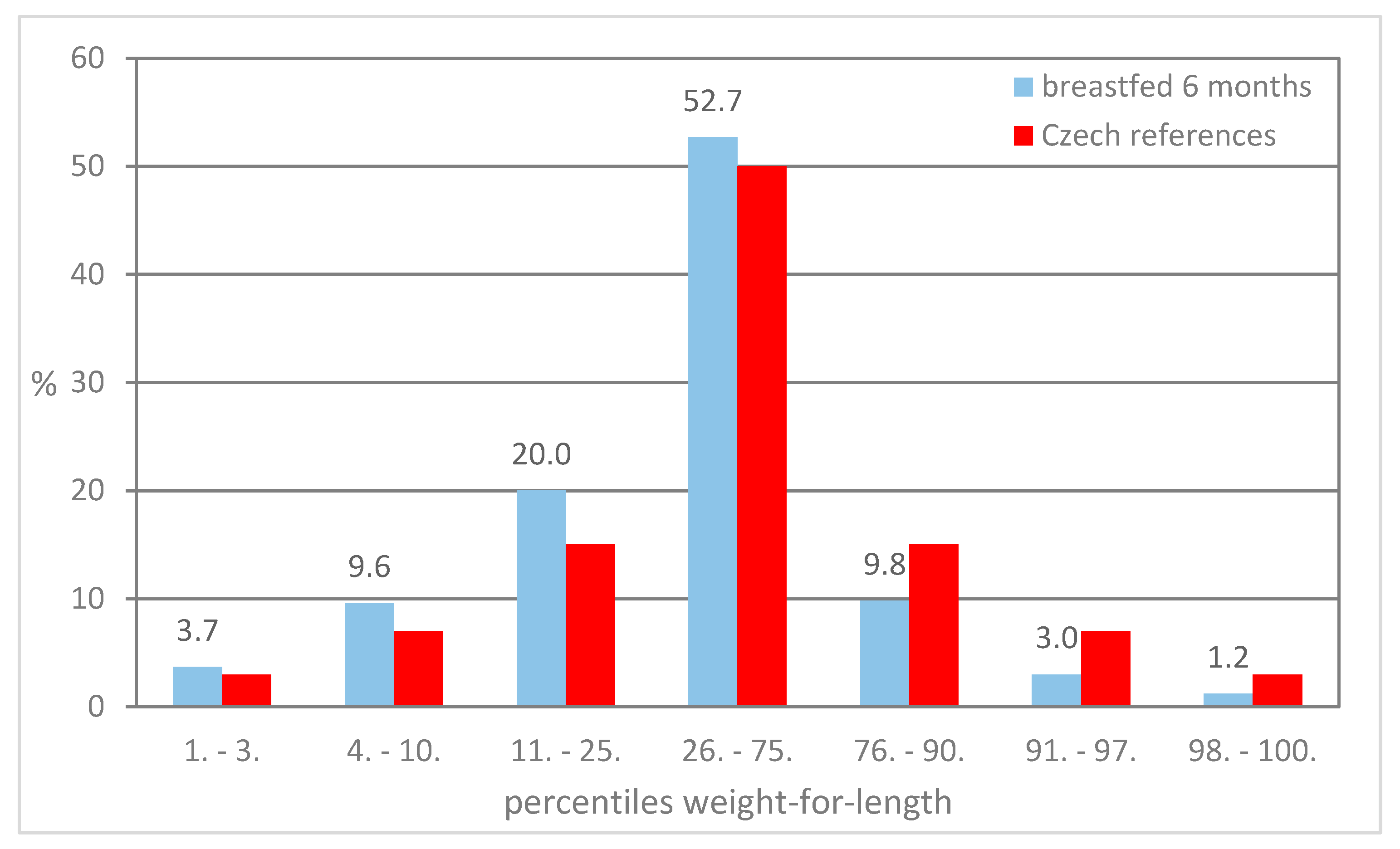
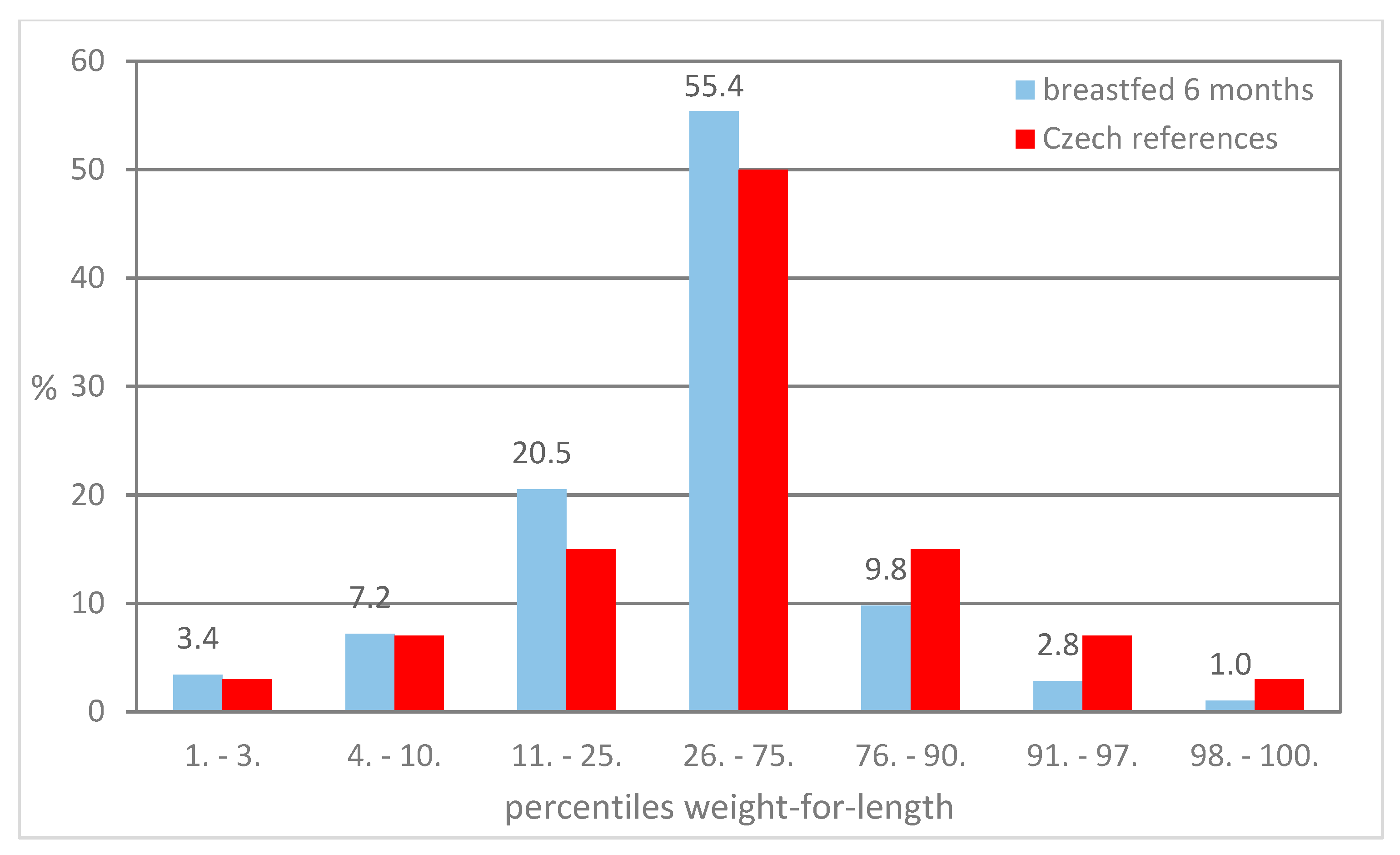
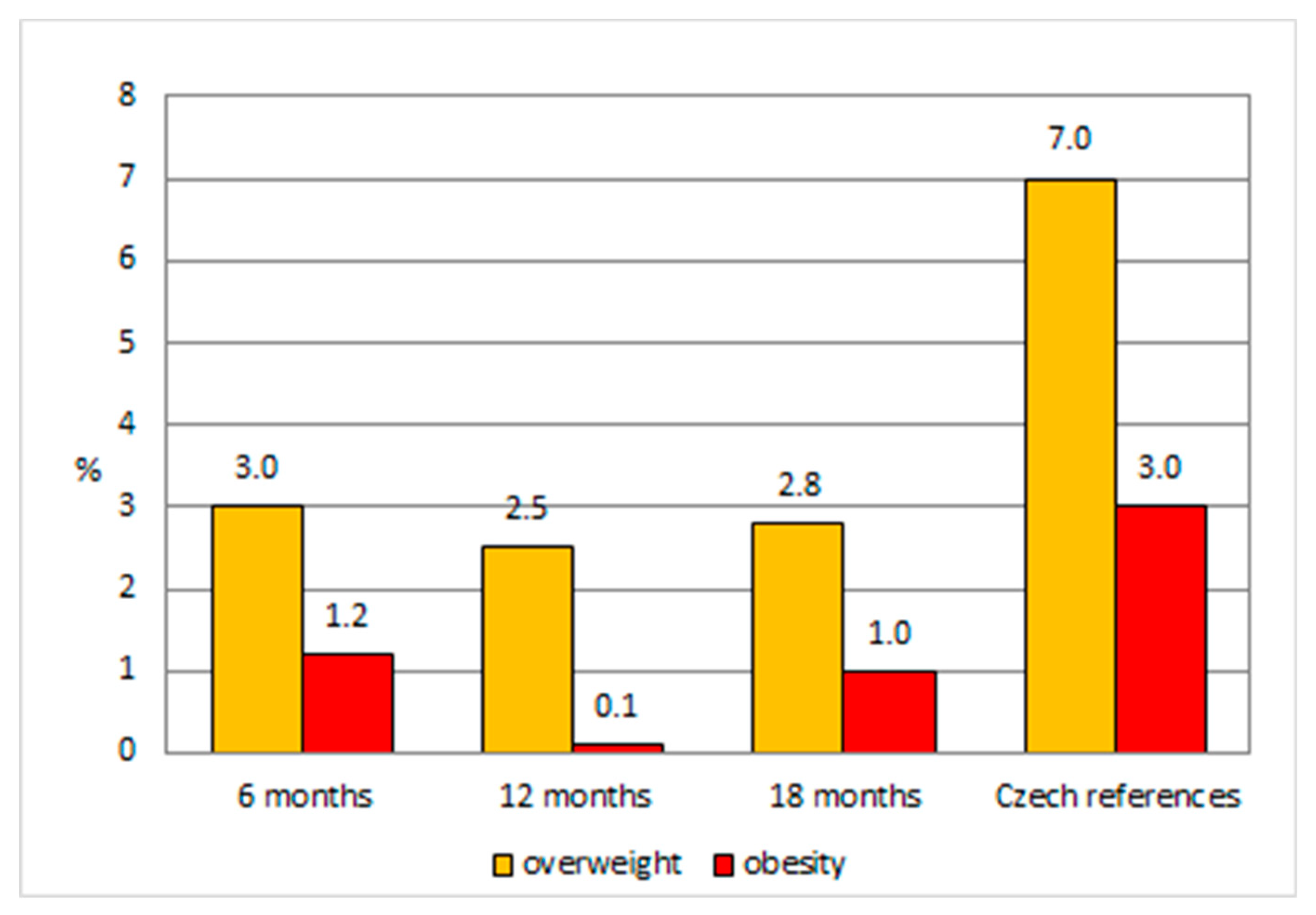
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. Available online: http://who.int/elena/titles/exclusive_breastfeeding/en (accessed on 23 July 2019).
- World Health Organization. Infant and Young Child Feeding. Geneva. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding/ (accessed on 23 July 2019).
- World Health Organization. Global Targets 2025. To Improve Maternal, Infant and Young Child Nutrition; World Health Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/nutrition/topics/nutrition_globaltargets2025/en/ (accessed on 23 July 2019).
- Morinis, J.; Maguire, J.; Khovratovich, M.; McCrindle, B.W.; Parkin, P.C.; Birken, C.S. Paediatric obesity research in early childhood and the primary care setting: The TARGet Kids! research network. Int. J. Environ. Res. Public Health 2012, 9, 1343–1354. [Google Scholar] [CrossRef] [PubMed]
- Paulová, M.; Vignerová, J.; Lhotská, L.; Hrušková, M. Rizika přijetí nových standardů Světové zdravotnické organizace pro hodnocení růstu české dětské populace (0–5 let) (Risks related to implementation of new standards of the WHO for growth assessment of Czech children population (0–5 years). Česko-Slovenská. Pediatrie. 2008, 63, 465–472. [Google Scholar]
- WHO Working Group on Infant Growth. An evaluation of infant growth: The use and interpretation of anthropometry in infants. Bull. WHO 1995, 73, 165–174. [Google Scholar]
- Salmenpera, L.; Perheentupa, J.; Siimes, M.A. Exclusively breast-fed healthy infants grow slower than reference infants. Pediatr. Res. 1985, 19, 307–312. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. A Growth Chart for International Use in Maternal and Health Care. Guidelines for Primary Health Care Personnel; WHO: Geneva, Switzerland, 1978. [Google Scholar]
- World Health Organization. WHO Child Growth Standards: Length/height-for-age, Weight-for-age, Weight-for-length, Weight-for-height and Body Mass Index-for-age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. Breastfeeding in the WHO Multicentre Growth Reference Study. Acta Paediatr. Suppl. 2006, 450, 16–27. [Google Scholar]
- De Onis, M.; Onyango, A.; Borghi, E.; Siyam, A.; Blössner, M.; Lutter, C. Worldwide implementation of the WHO Child Growth. Public Health Nutr. 2012, 15, 1603–1610. [Google Scholar] [CrossRef]
- De Onis, M.; Wijnhoven, T.M.A.; Onyango, A.W. Worldwide practices in child growth monitoring. J. Pediatr. 2004, 144, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Dewey, K.G.; Heinig, M.J.; Nommsen, L.A.; Peerson, J.M.; Lönnerdal, B. Growth of breast-fed and formula-fed infants from 0 to 18 months: The DARLING study. Pediatrics 1992, 89, 1035–1041. [Google Scholar]
- Vignerová, J.; Shriver, L.; Paulová, M.; Brabec, M.; Schneidrová, D.; Růžková, R.; Procházka, B.; Riedlová, J. Growth of Czech breastfed infants in comparison with the World Health Organization standards. Cent Eur. J. Public Health 2015, 23, 32–38. [Google Scholar] [CrossRef][Green Version]
- Vignerová, J.; Paulová, M.; Shriver, L.H.; Riedlová, J.; Schneidrová, D.; Kudlová, E.; Lhotská, L. The prevalence of wasting in Czech infants: A comparison of the WHO child growth standards and the Czech growth references. Matern Child Nutr. 2012, 8, 249–258. [Google Scholar] [CrossRef]
- Lhotská, L.; Bláha, P.; Vignerová, J.; Roth, Z.; Prokopec, M.V. Celostátní antropologický výzkum dětí a mládeže 1991 (České země) Antropometrické charakteristiky. (Nationwide anthropological research in children and youth 1991 (Czech countries) Anthropometric characteristics.); National Institute of Public Health: Prague, Czech Republic, 1993.
- Vignerová, J.; Riedlová, J.; Bláha, P.; Kobzová, J.; Krejčovský, L.; Brabec, M.; Hrušková, M. 6. Celostátní antropologický výzkum dětí a mládeže 2001. Česká republika. Souhrnné výsledky. (Nationwide anthropological research in children and youth 2001. Czech Republic); Summary Results; National Institute of Public Health: Prague, Czech Republic, 2006; ISBN 80-86561-30-5.
- Riedlová, J.; Vignerová, J.; Paulová, M.; Musil, V.; Brabec, M.; Schneidrová, D. Body parameters of Czech breastfed children compared to the Czech references and WHO growth standards. Ann. Hum. Biol. 2017, 44, 593–599. [Google Scholar] [CrossRef]
- De Onis, M.; Garza, C.; Victora, C.G.; Onyango, A.W.; Frongillo, E.A.; Martines, J. The WHO Multicentre Growth Reference Study: Planning, study design, and methodology. Food Nutr. 2004, 25, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; Saller, K. Lehrbuch der Anthropologie in Systematischer Darstellung mit Besonderer Berücksichtigung der Anthropologischen Methoden, 3rd ed.; Gustav Fischer Verlag: Stuttgart, Germany, 1957. [Google Scholar]
- Bláha, P.; Vignerová, J.; Riedlová, J.; Kobzová, J.; Krejčovský, L. RůstCZ: Program pro hodnocení růstu dítěte: (GrowthCZ: Programme for the Assessment of Child Growth); Version 2.3. 2011. Available online: http://www.szu.cz/publikace/data/program-rustcz-ke-stazeni/ (accessed on 23 July 2019).
- Hope, A.C.A. A simplified Monte Carlo significance test procedure. J. Roystatist. Soc. B 1968, 30, 582–598. [Google Scholar] [CrossRef]
- Kramer, M.S.; Kakuma, R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012, 8, CD003517. [Google Scholar] [CrossRef] [PubMed]
- Rito, A.I.; Buoncristiano, M.; Spinelli, A.; Salanave, B.; Kunešová, M.; Hejgaard, T.; García Solano, M.; Fijałkowska, A.; Sturua, L.; Hyska, J.; et al. Association between characteristics at birth, breastfeeding and obesity in 22 countries: The WHO European Childhood Obesity Surveillance Initiative—COSI 2015/2017. Obes. Facts. 2019, 12, 226–243. [Google Scholar] [CrossRef]
- Tambalis, K.D.; Mourtakos, S.; Panagiotakos, D.B.; Sidossis, L.S. Association of exclusive breastfeeding with risk of obesity in childhood and early adulthood. Breastfeed. Med. 2018, 13, 687–693. [Google Scholar] [CrossRef]
- Moschonis, G.; Grammatikaki, E.; Manios, Y. Perinatal predictors of overweight at infancy and preschool childhood: The GENESIS study. Int. J. Obes. 2008, 32, 39–47. [Google Scholar] [CrossRef]
- Wallby, T.; Lagerberg, D.; Magnusson, M. Relationship between breastfeeding and early childhood obesity: Results of a prospective longitudinal study from birth to 4 years. Breastfeed. Med. 2017, 12, 48–53. [Google Scholar] [CrossRef]
- Horta, B.L.; de Mola, C.L.; Victora, C.G. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef]
- Yan, J.; Liu, L.; Zhu, Y.; Huang, G.; Wang, P.P. The association between breastfeeding and childhood obesity: A meta-analysis. BMC Public Health 2014, 14, 1267. [Google Scholar] [CrossRef]
- Weng, S.F.; Redsell, S.A.; Swift, J.A.; Yang, M.; Glazebrook, C.P. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch. Dis. Child. 2012, 97, 1019–1026. [Google Scholar] [CrossRef]
- Marchand, V. Member of the Collaborative Statement Advisory Group, Nutrition and Gastroenterology Committee, promoting optimal monitoring of child growth in Canada: Using the new World Health Organization growth charts. Paediatr. Child. Health 2010, 15, 77–79. [Google Scholar]
- Barlow, S.E. Committee at E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120, 164–192. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Early Childhood Obesity Prevention Policies; Institute of Medicine (IoM): Washington, DC, USA, 2011. [Google Scholar]
- Tully, L.; Wright, C.M.; McCormick, D.; Garcia, A.D. Assessing the potential for integrating routine data collection on complementary feeding to child health visits: A mixed-methods study. Int. J. Environ. Res. Public Health 2019, 16, 1722. [Google Scholar] [CrossRef] [PubMed]

| Time Period | Activity |
|---|---|
| 2008 | Preparation of the study. |
| February–March 2009 | GP pediatricians addressed by professional associations at several educational meetings. |
| March 2009 | GP pediatricians who agreed to participate in the study got written instructions on the methodology of anthropometrical measurements and administration of the questionnaire. |
| April 2009–May 2010 | Data collection by GP pediatricians. |
| May–June 2010 | Collection of questionnaires from GP pediatricians. |
| June 2010 | Data processed with the EpiData Entry. |
| July–August 2010 | Formal and logical control of data; corrections based on consultations with GP pediatricians. |
| August–December 2010 | The construction and control of the individual growth curves of all children; corrections based on consultations with GP pediatricians. |
| January–March 2011 | Sampling of breastfed children, statistical analysis of data, and construction of growth curves of breastfed children. |
| Preventive Examination (months) | Sex | n | Body Length (cm) | SDS Body Length | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | |||
| 6 | boys | 334 | 68.9 | 2.46 | 62.0 | 77.0 | 0.04 | 0.80 |
| girls | 362 | 67.2 | 2.43 | 60.0 | 78.0 | 0.13 | 0.83 | |
| 12 | boys | 355 | 77.1 | 2.60 | 70.0 | 86.0 | 0.08 | 0.82 |
| girls | 376 | 75.4 | 2.65 | 67.0 | 83.0 | 0.06 | 0.85 | |
| 18 | boys | 313 | 83.5 | 3.05 | 74.0 | 91.5 | 0.14 | 0.89 |
| girls | 302 | 81.8 | 2.84 | 72.0 | 90.0 | 0.04 | 0.85 | |
| Preventive Examination (months) | Sex | n | Body Weight (g) | SDS Body Weight | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | |||
| 6 | boys | 335 | 7926.3 | 895.49 | 5530 | 11,450 | −0.08 | 0.94 |
| girls | 367 | 7288.5 | 796.24 | 5290 | 10,070 | −0.12 | 0.92 | |
| 12 | boys | 355 | 10,000.6 | 1035.27 | 7600 | 13,950 | −0.31 | 0.90 |
| girls | 376 | 9283.8 | 963.38 | 6680 | 12,570 | −0.39 | 0.93 | |
| 18 | boys | 314 | 11,574.6 | 1241.60 | 8000 | 15,600 | −0.18 | 0.95 |
| girls | 302 | 10,877.2 | 1179.60 | 7480 | 15,440 | −0.25 | 0.96 | |
| Preventive Examination (months) | Weight-for-Length (percentiles) | Excl.BF = 6 m | Excl.BF > 6 m | Czech References | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| 6 | overweight | 18 | 3.3 | 3 | 1.9 | 7 |
| obesity | 6 | 1.1 | 2 | 1.3 | 3 | |
| 12 | overweight | 14 | 2.5 | 4 | 2.4 | 7 |
| obesity | 1 | 0.2 | 0 | 0.0 | 3 | |
| 18 | overweight | 17 | 3.5 | 0 | 0.0 | 7 |
| obesity | 4 | 0.8 | 2 | 1.5 | 3 | |
| Sex | SDS of Weight-for-Length | Breastfeeding (months) | |||
|---|---|---|---|---|---|
| 6 Months | 12 Months | 18 Months | Exclusive or Predominant | Total | |
| girl | 1.10 | 0.40 | 2.04 | 6 | 10 |
| boy | 2.15 | 0.56 | 1.86 | 6 | 12 |
| girl | −0.17 1 | 0.69 | 2.16 | 6 | 11 |
| girl | 1.08 | 1.28 | 2.32 | 6 | 11 |
| girl | 1.29 | 0.76 2 | 2.30 | 6 | 8.25 |
| girl | 2.03 | 1.54 | 1.35 | 6 | 14 |
| girl | 2.24 | 0.92 | 0.51 | 6 | 11 |
| boy | 2.88 | 1.56 | 1.20 | 6 | 18 |
| boy | 2.18 | 1.63 3 | 1.23 | 6 | 8 |
| boy | 2.15 | 2.52 | 2.42 4 | 6 | 18 |
| girl | 2.13 | 1.28 | 2.08 | 8 | 12 |
| boy | 2.21 | 1.49 | 2.08 | 8 | 18 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riedlová, J.; Paulová, M.; Vignerová, J.; Brabec, M.; Sedlak, P.; Schneidrová, D. The Low Prevalence of Overweight and Obesity in Czech Breastfed Infants and Young Children: An Anthropological Survey. Int. J. Environ. Res. Public Health 2019, 16, 4198. https://doi.org/10.3390/ijerph16214198
Riedlová J, Paulová M, Vignerová J, Brabec M, Sedlak P, Schneidrová D. The Low Prevalence of Overweight and Obesity in Czech Breastfed Infants and Young Children: An Anthropological Survey. International Journal of Environmental Research and Public Health. 2019; 16(21):4198. https://doi.org/10.3390/ijerph16214198
Chicago/Turabian StyleRiedlová, Jitka, Markéta Paulová, Jana Vignerová, Marek Brabec, Petr Sedlak, and Dagmar Schneidrová. 2019. "The Low Prevalence of Overweight and Obesity in Czech Breastfed Infants and Young Children: An Anthropological Survey" International Journal of Environmental Research and Public Health 16, no. 21: 4198. https://doi.org/10.3390/ijerph16214198
APA StyleRiedlová, J., Paulová, M., Vignerová, J., Brabec, M., Sedlak, P., & Schneidrová, D. (2019). The Low Prevalence of Overweight and Obesity in Czech Breastfed Infants and Young Children: An Anthropological Survey. International Journal of Environmental Research and Public Health, 16(21), 4198. https://doi.org/10.3390/ijerph16214198





