Characteristics of Traditional Chinese Medicine Use for Carpal Tunnel Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
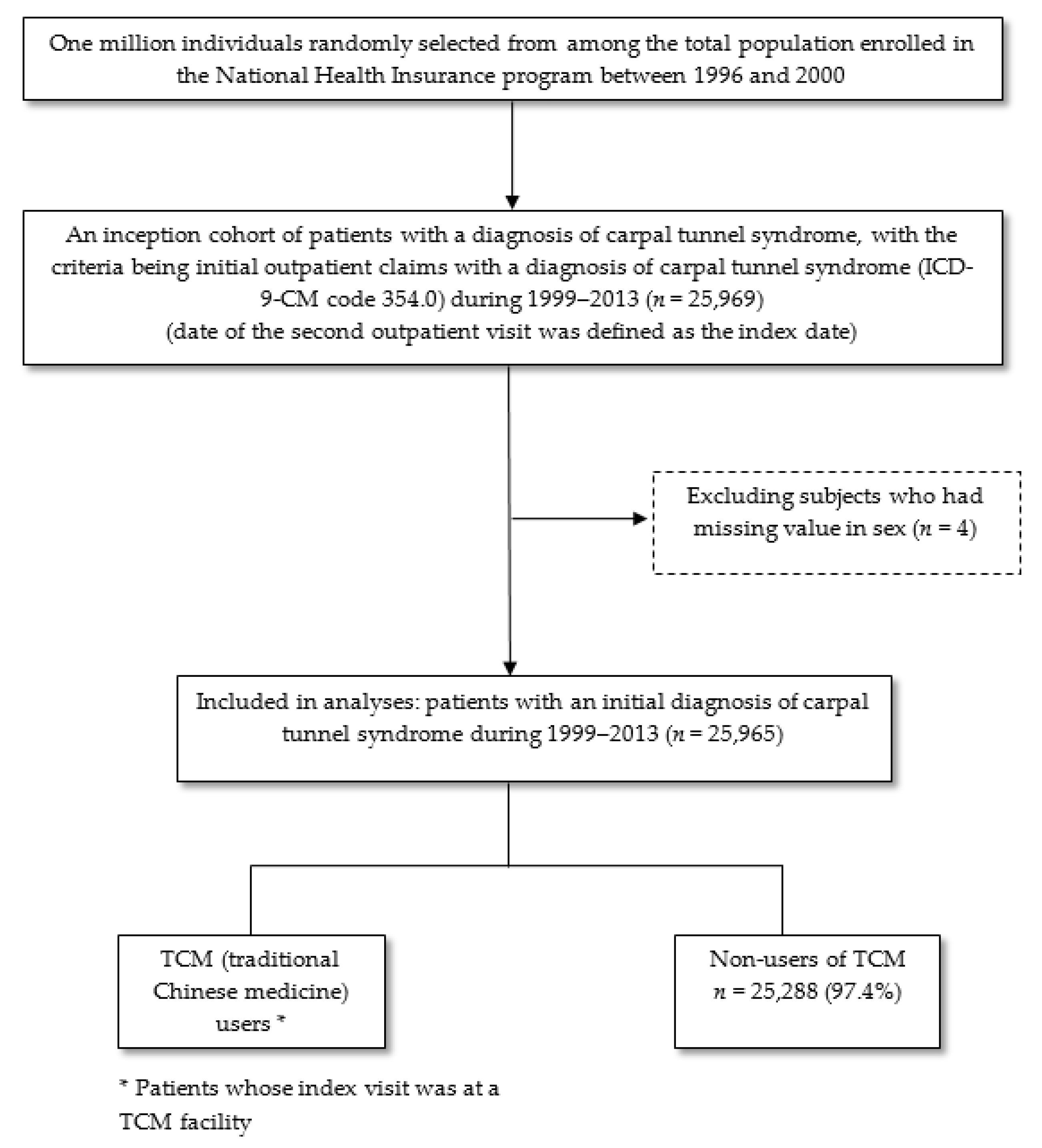
2.2. Study Sample
2.3. Patient Characteristics
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Riccò, M.; Signorelli, C. Personal and occupational risk factors for carpal tunnel syndrome in meat processing industry workers in Northern Italy. Med. Pr. 2017, 68, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Jackson, R.; Beckman, J.; Frederick, M.; Musolin, K.; Harrison, R. Rates of Carpal Tunnel Syndrome in a State Workers’ Compensation Information System, by Industry and Occupation—California, 2007–2014. Morb. Mortal. Wkly. Rep. 2018, 67, 1094–1097. [Google Scholar] [CrossRef] [PubMed]
- Meroni, R.; Alberti, P.; Boria, P.; Giordano, S.; Cavaletti, G. Distal pain and carpal tunnel syndrome diagnosis among cashiers: A longitudinal study. Int. Arch. Occup. Environ. Health. 2017, 90, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Nazari, G.; Shah, N.; MacDermid, J.C.; Woodhouse, L. The Impact of Sensory, Motor and Pain Impairments on Patient–Reported and Performance Based Function in Carpal Tunnel Syndrome. Open Orthop. J. 2017, 11, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Wolny, T.; Linek, P.; Saulicz, E. Assessment of manual dysfunction in occupationally active women with carpal tunnel syndrome. Int. J. Occup. Med. Environ. Health. 2019, 32, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Bickel, K.D. Carpal tunnel syndrome. J. Hand Surg. 2010, 35, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Jerosch-Herold, C.; Houghton, J.; Blake, J.; Shaikh, A.; Wilson, E.C.; Shepstone, L. Association of psychological distress, quality of life and costs with carpal tunnel syndrome severity: A cross-sectional analysis of the PALMS cohort. BMJ Open 2017, 7, e017732. [Google Scholar] [CrossRef] [PubMed]
- Seradge, H.; Parker, W.; Baer, C.; Mayfield, K.; Schall, L. Conservative treatment of carpal tunnel syndrome: An outcome study of adjunct exercises. J. Okla. State Med. Assoc. 2002, 95, 7–14. [Google Scholar] [PubMed]
- Lim, M.K.; Sadarangani, P.; Chan, H.L.; Heng, J.Y. Complementary and alternative medicine use in multiracial Singapore. Complement. Ther. Med. 2005, 13, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.; Chappell, N. Use of Traditional Chinese Medicine by older Chinese immigrants in Canada. Fam. Pract. 2007, 24, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Chung, V.; Wong, E.; Woo, J.; Lo, S.V.; Griffiths, S. Use of traditional Chinese medicine in the Hong Kong special administrative region of China. J. Altern. Complement. Med. 2007, 13, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.P.; Chen, T.J.; Kung, Y.Y.; Chen, Y.C.; Chou, L.F.; Chen, F.J.; Hwang, S.J. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv. Res. 2007, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. Announcement of Total Medical Expenses and Distribution in 2019. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=0404F75C81EB1977&topn=D39E2B72B0BDFA15 (accessed on 25 August 2019).
- Lu, J.F.; Hsiao, W.C. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff. (Millwood) 2003, 22, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Accounting and Statistics: National Statistics of Regional Standard Classification Data from Directorate-General Budget. Available online: https://eng.stat.gov.tw/mp.asp?mp=5 (accessed on 25 August 2019).
- Tan, H.F.; Tseng, H.F.; Chang, C.K.; Lin, W.; Hsiao, S.H. Accessibility assessment of the Health Care Improvement Program in rural Taiwan. J. Rural Health 2005, 21, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.Y.; Chang, H.H.; Sung, F.C.; Chen, P.C. Characteristics of Traditional Chinese Medicine Use in Pediatric Dislocations, Sprains and Strains. Int. J. Environ. Res. Public Health 2017, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.C.; Pai, F.T.; Lin, C.C.; Chang, C.M.; Chang, H.H.; Lee, Y.C.; Sun, M.F.; Yen, H.R. Characteristics of traditional Chinese medicine use in patients with rheumatoid arthritis in Taiwan: A nationwide population-based study. J. Ethnopharmacol. 2015, 176, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.K.; Tsai, Y.T.; Lai, J.N.; Wu, C.T. Demographic and medication characteristics of traditional Chinese medicine users among dementia patients in Taiwan: A nationwide database study. J. Ethnopharmacol. 2015, 161, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.C.; Lee, Y.C.; Lin, C.C.; Chang, C.H.; Chiu, C.D.; Chou, L.W.; Sun, M.F.; Yen, H.R. Characteristics of traditional Chinese medicine usage in patients with stroke in Taiwan: A nationwide population-based study. J. Ethnopharmacol. 2016, 186, 311–321. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. The National Health Insurance Statistics, 2017. National Health Insurance Annual Statistical Report 2017. Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=0D39BCF70F478274&topn=616B97F8DF2C3614 (accessed on 25 August 2019).
| Characteristics | Total | Non-Users of TCM | TCM Users | p |
|---|---|---|---|---|
| N = 25,965 | N = 25,288 (97.4%) | N = 677 (2.61%) | ||
| Age at diagnosis, yr, n (%) | <0.0001 | |||
| <18 | 54 (0.21) | 52 (0.21) | 2 (0.30) | |
| 18–30 | 1644 (6.33) | 1580 (6.25) | 64 (9.45) | |
| 31–45 | 7689 (29.6) | 7424 (29.4) | 265 (39.1) | |
| 46–65 | 13,360 (51.5) | 13,058 (51.6) | 302 (44.6) | |
| >65 | 3218 (12.4) | 3174 (12.6) | 44 (6.50) | |
| Mean(SD) | 50.4 (12.9) | 50.5 (1.29) | 46.3 (12.2) | <0.0001 |
| Female, n (%) | 18,505 (71.3) | 17,972 (71.1) | 533 (78.7) | <0.0001 |
| Geographic region of registration units for NHI, n (%) | <0.0001 | |||
| Northern | 11,793 (45.4) | 11,573 (45.8) | 220 (32.5) | |
| Central | 5148 (19.8) | 4998 (19.8) | 150 (22.2) | |
| Southern | 7692 (29.6) | 7425 (29.4) | 267 (39.4) | |
| Eastern | 1332 (5.12) | 1292 (5.11) | 40 (5.91) | |
| Urbanization level of registration units for NHI *, n (%) | 0.01 | |||
| Urban | 15,856 (61.1) | 15,459 (61.1) | 397 (58.6) | |
| Satellite | 7743 (29.8) | 7547 (29.8) | 196 (29.0) | |
| Rural | 2366 (9.11) | 2282 (9.02) | 84 (12.4) | |
| Previous medical conditions †, n (%) | ||||
| Month income (NTD), n (%) | 0.02 | |||
| <15,840 | 8429 (32.5) | 8176 (32.3) | 253 (37.4) | |
| 15,840–25,000 | 11,656 (44.9) | 11,369 (45.0) | 287 (42.4) | |
| >25,000 | 5880 (22.7) | 5743 (22.7) | 137 (20.2) | |
| Occupation, n (%) | 0.99 | |||
| White collar | 13,099 (50.5) | 12,758 (50.5) | 341 (50.4) | |
| Blue collar | 11,022 (42.5) | 10,734 (42.5) | 288 (42.5) | |
| Others | 1844 (7.10) | 1796 (7.10) | 48 (7.09) | |
| Infectious and parasitic diseases | 3449 (13.3) | 3366 (13.3) | 83 (12.3) | 0.43 |
| Neoplasms | 2067 (7.96) | 2030 (8.03) | 37 (5.47) | 0.02 |
| Endocrine, nutritional, blood and metabolic diseases, and immunity disorders | 6504 (25.1) | 6386 (25.3) | 118 (17.4) | <0.0001 |
| Mental disorders, diseases of the nervous system and sense organs | 16,042 (61.8) | 15,667 (62.0) | 375 (55.4) | 0.0005 |
| Diseases of the circulatory system | 7852 (30.2) | 7711 (30.5) | 141 (20.8) | <0.0001 |
| Diseases of the respiratory system | 17,108 (65.9) | 17,108 (67.7) | 457 (67.5) | 0.93 |
| Diseases of the digestive system | 15,854 (61.1) | 15,444 (61.1) | 410 (60.6) | 0.79 |
| Diseases of the genitourinary system | 8745 (33.7) | 8520 (33.7) | 225 (33.2) | 0.80 |
| Diseases of the skin and subcutaneous tissue | 6780 (26.1) | 6625 (26.2) | 155 (22.9) | 0.054 |
| Diseases of the musculoskeletal system and connective tissue | 17,174 (66.1) | 16,838 (66.6) | 336 (49.6) | <0.0001 |
| Symptoms, signs, and ill-defined conditions | 11,786 (45.4) | 11,493 (45.5) | 293 (43.3) | 0.26 |
| Injury and poisoning | 8435 (32.5) | 8230 (32.6) | 205 (30.3) | 0.21 |
| Supplementary classification | 4456 (17.2) | 4348 (17.2) | 108 (16.0) | 0.40 |
| Others | 215 (0.83) | 210 (0.83) | 5 (0.74) | 0.79 |
| Health care utilization †, n (%) | ||||
| Number of outpatient visit | <0.0001 | |||
| Q1 (25%) | 13 | 13 | 12 | |
| Q2 (50%) | 23 | 23 | 20 | |
| Q3 (75%) | 37 | 37 | 33 | |
| Median (interquartile range) | 23 (24) | 23 (24) | 20 (21) | |
| Number of inpatient visit | 0.009 | |||
| Q1 (25%) | 0 | 0 | 0 | |
| Q2 (50%) | 0 | 0 | 0 | |
| Q3 (75%) | 0 | 0 | 0 | |
| Median (interquartile range) | 0 (0) | 0 (0) | 0 (0) | |
| Number of TCM visit | <0.0001 | |||
| Q1 (25%) | 0 | 0 | 2 | |
| Q2 (50%) | 0 | 0 | 4 | |
| Q3 (75%) | 3 | 3 | 8 | |
| Median (interquartile range) | 0 (3) | 0 (3) | 4 (6) |
| Characteristics | Total | Non-Users of TCM | TCM Users | p |
|---|---|---|---|---|
| N = 25,965 | N = 25,288 | N = 677 | ||
| Locations of hospital where subjects received the diagnosis, n (%) | <0.0001 | |||
| Northern | 11,517 (44.4) | 11,319 (44.8) | 198 (29.3) | |
| Central | 5337 (20.6) | 5184 (20.5) | 153 (22.6) | |
| Southern | 7849 (30.2) | 7568 (29.9) | 281 (41.5) | |
| Eastern | 1262 (4.9) | 1217 (4.8) | 45 (6.7) | |
| Accreditation level of hospital where subjects received the diagnosis, n (%) | <0.0001 | |||
| Medical center | 5097 (19.6) | 5067 (20.0) | 30 (4.4) | |
| District hospital | 8367 (32.2) | 8314 (32.9) | 53 (7.8) | |
| Local hospital | 5707 (22.0) | 5681 (22.5) | 26 (3.8) | |
| Clinics and others | 6794 (26.2) | 6226 (24.6) | 568 (83.9) |
| Characteristics | Odds Ratio (95% Confidence Interval) † | ||||
|---|---|---|---|---|---|
| Crude Model | Age and Sex Adjusted Model | Selected Variables Adjusted Model * | All Variables Adjusted Model | Multilevel Model | |
| Age at diagnosis, year (vs. ≤30) | |||||
| 31–45 | 0.90 (0.68–1.21) | - | 1.08 (0.79–1.47) | 1.07 (0.78–1.47) | 1.05 (0.76–1.44) |
| 46–65 | 0.58 (0.44–0.78) | - | 0.90 (0.65–1.24) | 0.87 (0.63–1.22) | 0.86 (0.62–1.20) |
| >65 | 0.35 (0.23–0.52) | - | 0.78 (0.51–1.22) | 0.73 (0.47–1.15) | 0.73 (0.46–1.15) |
| Female (vs. Male) | 1.51 (1.25–1.82) | - | 1.33 (1.10–1.62) | 1.35 (1.11–1.66) | 1.36 (1.11–1.66) |
| Geographic region of registration units for NHI (vs. northern) | |||||
| Central | 1.58 (1.28–1.95) | 1.56 (1.26–1.92) | 1.41 (1.12–1.77) | 1.43 (1.13–1.79) | 1.36 (1.01–1.82) |
| Southern | 1.89 (1.58–2.27) | 1.90 (1.58–2.27) | 1.86 (1.54–2.26) | 1.86 (1.53–2.26) | 1.91 (1.47–2.48) |
| Eastern | 1.63 (1.16–2.29) | 1.64 (1.16–2.30) | 1.85 (1.29–2.65) | 1.82 (1.26–2.61) | 1.84 (1.19–2.84) |
| Urbanization level of registration units for NHI * (vs. urban) | |||||
| Satellite | 1.01 (0.85–1.20) | 1.01 (0.85–1.20) | 0.89 (0.74–1.07) | 0.90 (0.75–1.08) | 0.93 (0.74–1.17) |
| Rural | 1.43 (1.13–1.82) | 1.47 (1.15–1.86) | 1.32 (1.02–1.71) | 1.33 (1.02–1.72) | 1.33 (0.98–1.81) |
| Month income (vs. >25,000) | |||||
| <15,840 | 1.30 (1.05–1.60) | 1.09 (0.88–1.36) | 1.09 (0.87–1.37) | 1.09 (0.86–1.39) | 1.12 (0.88–1.43) |
| 15,840–25,000 | 1.06 (0.86–1.30) | 1.03 (0.84–1.27) | 0.98 (0.79–1.21) | 0.98 (0.77–1.23) | 1.00 (0.79–1.27) |
| Occupation (vs. white collar) | |||||
| Blue collar | 1.00 (0.86–1.18) | 1.05 (0.89–1.23) | - | 1.02 (0.84–1.24) | 0.99 (0.81–1.22) |
| Others | 1.00 (0.74–1.36) | 1.11 (0.81–1.50) | - | 1.06 (0.76–1.47) | 1.09 (0.85–1.39) |
| Common conditions of pediatric patients in outpatient settings †, (yes vs. no) | |||||
| Infectious and parasitic diseases | 0.91 (0.72–1.15) | 0.95 (0.75–1.20) | - | 1.08 (0.84–1.38) | 1.09 (0.85–1.39) |
| Neoplasms | 0.66 (0.47–0.93) | 0.68 (0.48–0.95) | 0.76 (0.54–1.07) | 0.76 (0.54–1.08) | 0.76 (0.54–1.08) |
| Endocrine, nutritional, blood and metabolic diseases, and immunity disorders | 0.63 (0.51–0.76) | 0.77 (0.62–0.94) | 0.91 (0.73–1.13) | 0.90 (0.72–1.12) | 0.91 (0.73–1.13) |
| Mental disorders, diseases of the nervous system and sense organs | 0.76 (0.65–0.89) | 0.83 (0.71–0.97) | 0.86 (0.72–1.01) | 0.86 (0.72–1.01) | 0.85 (0.72–1.01) |
| Diseases of the circulatory system | 0.60 (0.50–0.72) | 0.80 (0.65–0.97) | 0.95 (0.76–1.18) | 0.95 (0.76–1.18) | 0.93 (0.75–1.16) |
| Diseases of the respiratory system | 0.99 (0.84–1.17) | 0.95 (0.81–1.12) | - | 0.99 (0.83–1.19) | 1.00 (0.83–1.19) |
| Diseases of the digestive system | 0.98 (0.84–1.14) | 1.03 (0.88–1.21) | - | 1.11 (0.93–1.31) | 1.09 (0.92–1.30) |
| Diseases of the genitourinary system | 0.98 (0.83–1.15) | 0.88 (0.74–1.04) | - | 0.91 (0.76–1.10) | 0.91 (0.76–1.10) |
| Diseases of the skin and subcutaneous tissue | 0.84 (0.70–1.00) | 0.83 (0.69–0.99) | - | 0.87 (0.72–1.06) | 0.87 (0.72–1.06) |
| Diseases of the musculoskeletal system and connective tissue | 0.49 (0.42–0.58) | 0.55 (0.47–0.64) | 0.44 (0.37–0.52) | 0.44 (0.37–0.52) | 0.44 (0.37–0.53) |
| Symptoms, signs, and ill-defined conditions | 0.92 (0.79–1.07) | 0.96 (0.82–1.12) | - | 0.81 (0.68–0.96) | 0.81 (0.68–0.97) |
| Injury and poisoning | 0.90 (0.76–1.06) | 0.92 (0.78–1.09) | - | 0.79 (0.66–0.95) | 0.80 (0.64–0.95) |
| Supplementary classification | 0.91 (0.74–1.13) | 1.01 (0.82–1.25) | - | 1.13 (0.90–1.42) | 1.12 (0.89–1.41) |
| Others | 0.89 (0.37–2.16) | 0.95 (0.39–2.31) | - | 0.93 (0.37–2.30) | 0.93 (0.37–2.32) |
| Health care utilization † | |||||
| Number of outpatient visit (vs. <Q1) | |||||
| Q1–Q2 | 0.96 (0.79–1.18) | 0.98 (0.80–1.21) | 0.80 (0.64–1.00) | 0.84 (0.66–1.07) | 0.85 (0.67–1.08) |
| Q2–Q3 | 0.79 (0.64–0.97) | 0.84 (0.68–1.05) | 0.62 (0.48–0.79) | 0.68 (0.51–0.91) | 0.69 (0.52–0.93) |
| ≥Q3 | 0.63 (0.50–0.79) | 0.78 (0.62–0.99) | 0.53 (0.39–0.71) | 0.62 (0.43–0.89) | 0.62 (0.43–0.89) |
| Number of inpatient visit (vs. no) | 0.72 (0.55–0.93) | 0.79 (0.60–1.02) | 0.95 (0.72–1.25) | 0.97 (0.73–1.28) | 0.97 (0.73–1.28) |
| Number of TCM visit (vs. <Q3) | 3.82 (3.27–4.47) | 3.67 (3.14–4.29) | 5.41 (4.54–6.46) | 5.80 (4.84–6.96) | 5.79 (4.83–6.95) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, M.-C.; Kuo, Y.-H.; Muo, C.-H.; Chou, L.-W.; Lu, C.-Y. Characteristics of Traditional Chinese Medicine Use for Carpal Tunnel Syndrome. Int. J. Environ. Res. Public Health 2019, 16, 4086. https://doi.org/10.3390/ijerph16214086
Tsai M-C, Kuo Y-H, Muo C-H, Chou L-W, Lu C-Y. Characteristics of Traditional Chinese Medicine Use for Carpal Tunnel Syndrome. International Journal of Environmental Research and Public Health. 2019; 16(21):4086. https://doi.org/10.3390/ijerph16214086
Chicago/Turabian StyleTsai, Meng-Chuan, Yu-Hsien Kuo, Chih-Hsin Muo, Li-Wei Chou, and Chung-Yen Lu. 2019. "Characteristics of Traditional Chinese Medicine Use for Carpal Tunnel Syndrome" International Journal of Environmental Research and Public Health 16, no. 21: 4086. https://doi.org/10.3390/ijerph16214086
APA StyleTsai, M.-C., Kuo, Y.-H., Muo, C.-H., Chou, L.-W., & Lu, C.-Y. (2019). Characteristics of Traditional Chinese Medicine Use for Carpal Tunnel Syndrome. International Journal of Environmental Research and Public Health, 16(21), 4086. https://doi.org/10.3390/ijerph16214086






