Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
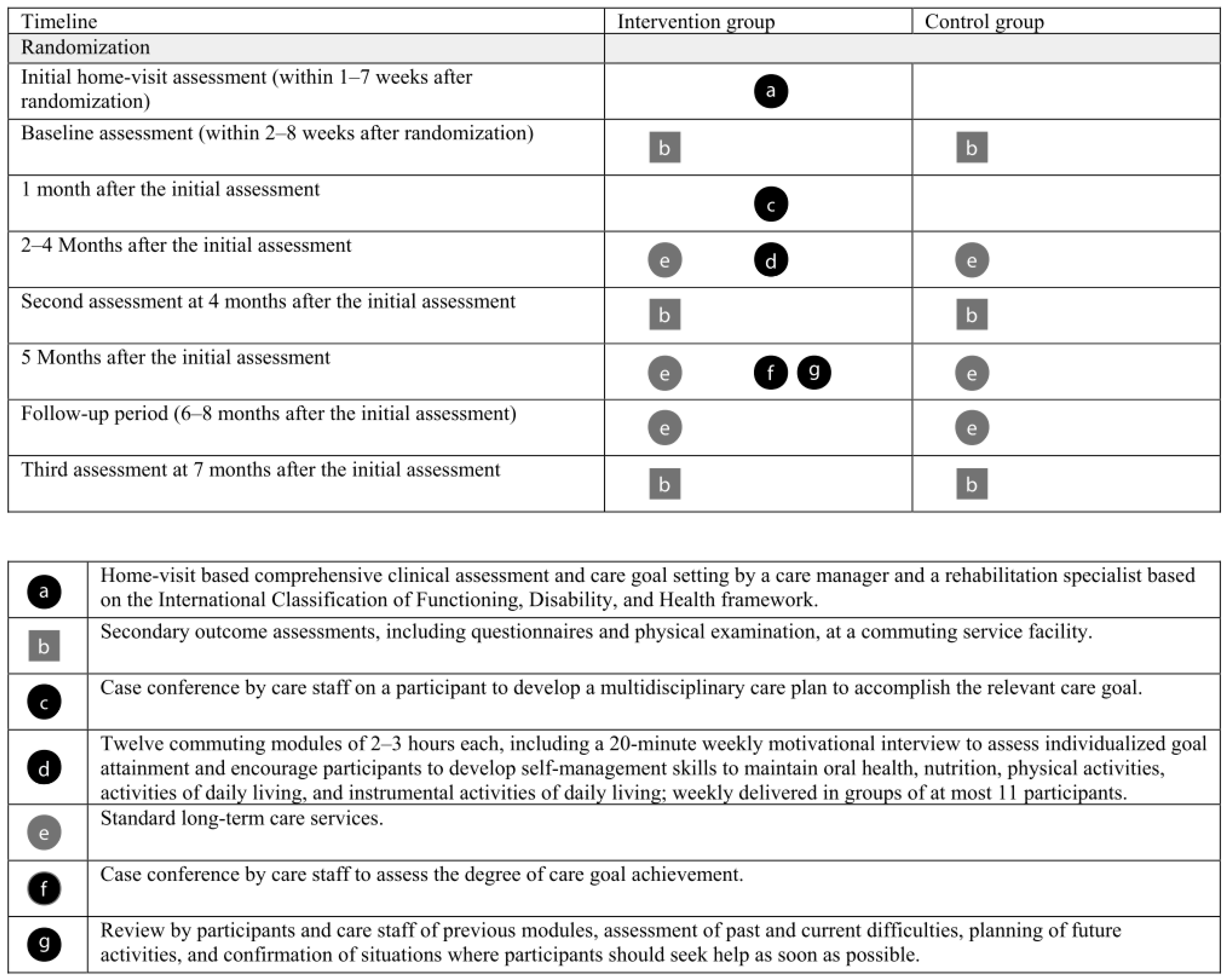
2.1. Design
2.2. Setting
2.3. Participants
2.4. Randomization
2.5. Intervention
2.5.1. Standard Care Group
2.5.2. CoMMIT Program Plus Standard Care Group
2.6. Therapist Training and Quality Assurance
2.7. Outcomes
2.8. Sample Size Estimation
2.9. Statistical Analyses
3. Results
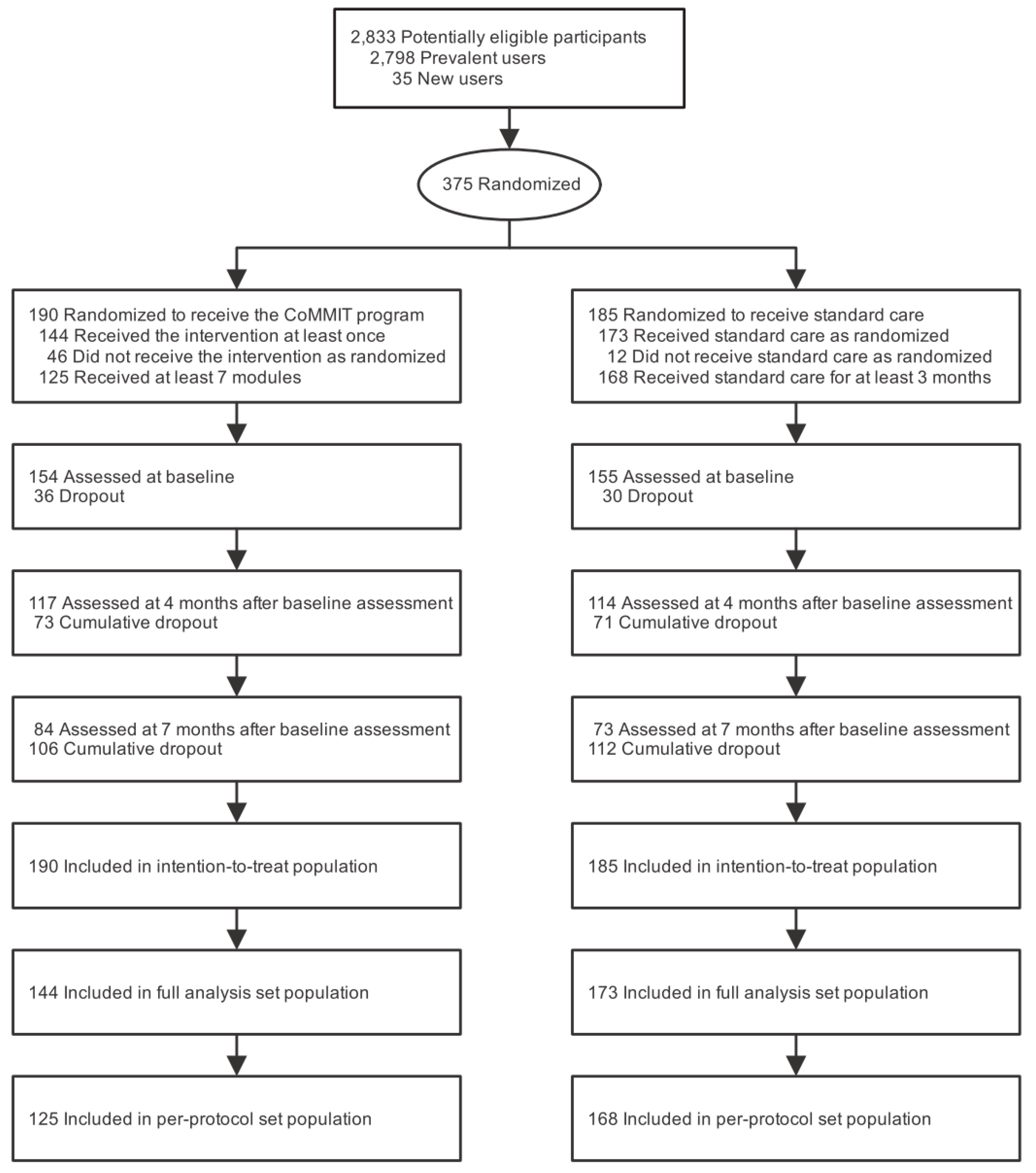
3.1. Participants
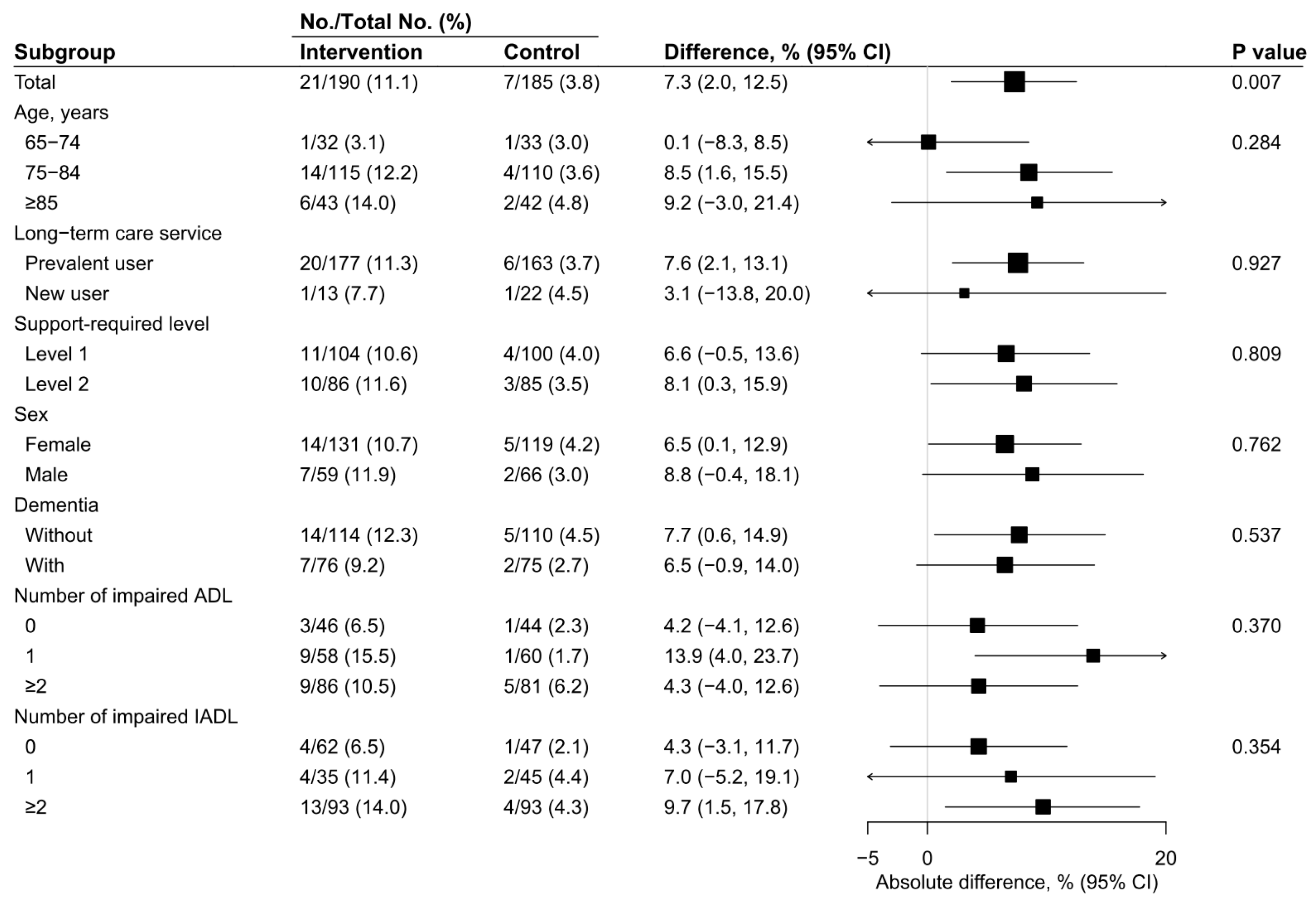
3.2. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ministry of Health. Labor and Welfare Society in which Healthy Life Expectancy is Extended. Available online: https://www.mhlw.go.jp/stf/houdou/0000019326.html (accessed on 7 June 2019). (In Japanese)
- Ministry of Health. Labor and Welfare Status Report on the Long-term Care Insurance. Available online: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450351&tstat=000001031648&cycle=8&tclass1=000001113661&second2=1 (accessed on 7 June 2019). (In Japanese)
- Ministry of Health. Labor and Welfare Guideline for Integrated Long-Term Care Prevention and Daily Life Support Programs. Available online: https://www.mhlw.go.jp/file/06-Seisakujouhou-12300000-Roukenkyoku/0000205730.pdf (accessed on 7 June 2019). (In Japanese)
- Ministry of Justice Long-Term Care Insurance Act. Available online: http://www.japaneselawtranslation.go.jp/law/detail/?id=94&vm=04&re=01&new=1 (accessed on 7 June 2019).
- Gill, T.M. Disentangling the disabling process: Insights from the precipitating events project. Gerontologist 2014, 54, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Arnau, A.; Espaulella, J.; Serrarols, M.; Canudas, J.; Formiga, F.; Ferrer, M. Risk factors for functional decline in a population aged 75 years and older without total dependence: A one-year follow-up. Arch. Gerontol. Geriatr. 2016, 65, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Szanton, S.L.; Xue, Q.L.; Leff, B.; Guralnik, J.; Wolff, J.L.; Tanner, E.K.; Boyd, C.; Thorpe, R.J., Jr.; Bishai, D.; Gitlin, L.N. Effect of a biobehavioral environmental approach on disability among low-income older adults: A randomized clinical trial. JAMA Intern. Med. 2019, 179, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Winzer, E.; Dorner, T.E.; Grabovac, I.; Haider, S.; Kapan, A.; Lackinger, C.; Schindler, K. Behavior changes by a buddy-style intervention including physical training, and nutritional and social support. Geriatr. Gerontol. Int. 2019, 19, 323–329. [Google Scholar] [CrossRef]
- Whitehead, P.J.; Walker, M.F.; Parry, R.H.; Latif, Z.; McGeorge, I.D.; Drummond, A.E. Occupational Therapy in HomEcare Re-ablement Services (OTHERS): Results of a feasibility randomised controlled trial. BMJ Open 2016, 6, e011868. [Google Scholar] [CrossRef]
- Tuntland, H.; Aaslund, M.K.; Espehaug, B.; Forland, O.; Kjeken, I. Reablement in community-dwelling older adults: A randomised controlled trial. BMC Geriatr. 2015, 15, 145. [Google Scholar] [CrossRef]
- Lewin, G.; De San Miguel, K.; Knuiman, M.; Alan, J.; Boldy, D.; Hendrie, D.; Vandermeulen, S. A randomised controlled trial of the Home Independence Program, an Australian restorative home-care programme for older adults. Health Soc. Care Community 2013, 21, 69–78. [Google Scholar] [CrossRef]
- Burton, E.; Lewin, G.; Clemson, L.; Boldy, D. Effectiveness of a lifestyle exercise program for older people receiving a restorative home care service: A pragmatic randomized controlled trial. Clin. Interv. Aging 2013, 8, 1591–1601. [Google Scholar] [CrossRef]
- Cameron, I.D.; Fairhall, N.; Langron, C.; Lockwood, K.; Monaghan, N.; Aggar, C.; Sherrington, C.; Lord, S.R.; Kurrle, S.E. A multifactorial interdisciplinary intervention reduces frailty in older people: Randomized trial. BMC Med. 2013, 11, 65. [Google Scholar] [CrossRef]
- Szanton, S.L.; Thorpe, R.J.; Boyd, C.; Tanner, E.K.; Leff, B.; Agree, E.; Xue, Q.L.; Allen, J.K.; Seplaki, C.L.; Weiss, C.O.; et al. Community aging in place, advancing better living for elders: A bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J. Am. Geriatr. Soc. 2011, 59, 2314–2320. [Google Scholar] [CrossRef]
- Gitlin, L.N.; Winter, L.; Dennis, M.P.; Corcoran, M.; Schinfeld, S.; Hauck, W.W. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J. Am. Geriatr. Soc. 2006, 54, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Baker, D.; Gallo, W.T.; Nanda, A.; Charpentier, P.; O’Leary, J. Evaluation of restorative care vs. usual care for older adults receiving an acute episode of home care. JAMA Intern. Med. 2002, 287, 2098–2105. [Google Scholar] [CrossRef] [PubMed]
- Cochrane, A.; Furlong, M.; McGilloway, S.; Molloy, D.W.; Stevenson, M.; Donnelly, M. Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst. Rev. 2016, 10, CD010825. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Kitahara, R.; Hattori, S. Make a Care Plan for Preventive Long-Term Care and the Commuting Service Type C: Lessons Learn from Practices in Ikoma City; Institute of Social Insurance: Tokyo, Japan, 2017. (In Japanese) [Google Scholar]
- Japan Care Manager Association A Comparison of Care Managiment Functioning in Six Countries. Available online: https://www.jcma.or.jp/wp-content/uploads/2019/04/190408-roken3syo.pdf (accessed on 4 October 2019).
- Takigawa, Y. Criteria for evaluating the degree of independence of dementia elderly performing activities of daily living. J. Public Health Pract. 1994, 58, 73–75. [Google Scholar]
- Kanatani, Y.; Tomita, N.; Sato, Y.; Eto, A.; Omoe, H.; Mizushima, H. National registry of designated intractable diseases in Japan: Present status and future prospects. Neurol. Medico-Chirurg. 2017, 57, 1–7. [Google Scholar] [CrossRef]
- Narasimhan, B. SRS: A Subject Randomization Syste. Available online: https://r-forge.r-project.org/scm/viewvc.php/*checkout*/pkg/SRS/inst/doc/SRS.pdf?root=srs (accessed on 7 June 2019).
- Pocock, S.J.; Simon, R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1975, 31, 103–115. [Google Scholar] [CrossRef]
- Perera, R.; Heneghan, C.; Yudkin, P. Graphical method for depicting randomised trials of complex interventions. BMJ Open 2007, 334, 127–129. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Gordon, G.; Drummond, R.; Maureen, O.M.; Deborah, J.C. Users’ Guides to the Medical Literature: Essentials of Evidence-Based Clinical Practice, 3rd ed.; McGraw-Hill Education: New York, NY, USA, 2014; p. 1. [Google Scholar]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gotzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ Open 2010, 340, c869. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.; Kunz, R.; Brozek, J.; Alonso-Coello, P.; Montori, V.; Akl, E.A.; Djulbegovic, B.; Falck-Ytter, Y.; et al. GRADE guidelines: 4. Rating the quality of evidence—Study limitations (risk of bias). J. Clin. Epidemiol. 2011, 64, 407–415. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ Open 2019, 366, l4898. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Sultan, S.; Glasziou, P.; Akl, E.A.; Alonso-Coello, P.; Atkins, D.; Kunz, R.; Brozek, J.; Montori, V.; et al. GRADE guidelines: 9. Rating up the quality of evidence. J. Clin. Epidemiol. 2011, 64, 1311–1316. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | ITT Population | FAS Population | PPS Population | |||
|---|---|---|---|---|---|---|
| Intervention Group (n = 190) | Control Group (n = 185) | Intervention Group (n = 144) | Control Group (n = 173) | Intervention group (n = 125) | Control Group (n = 168) | |
| Age, median (IQR), years | 80.0 (76.3–84.0) | 80.0 (76.0–84.0) | 80.0 (76.0–83.3) | 80.0 (76.0–84.0) | 80.0 (76.0–84.0) | 80.0 (76.0–84.0) |
| Age group, y, No. (%) | ||||||
| 65–74 | 32 (16.8) | 33 (17.8) | 25 (17.4) | 32 (18.5) | 23 (18.4) | 32 (19.0) |
| 75–84 | 115 (60.5) | 110 (59.5) | 90 (62.5) | 101 (58.4) | 74 (59.2) | 96 (57.1) |
| ≥85 | 43 (22.6) | 42 (22.7) | 29 (20.1) | 40 (23.1) | 28 (22.4) | 40 (23.8) |
| Sex, No. (%) | ||||||
| Female | 131 (68.9) | 119 (64.3) | 100 (69.4) | 110 (63.6) | 83 (66.4) | 108 (64.3) |
| Male | 59 (31.1) | 66 (35.7) | 44 (30.6) | 63 (36.4) | 42 (33.6) | 60 (35.7) |
| Use of long-term care insurance, No. (%) | ||||||
| Prevalent user | 177 (93.2) | 163 (88.1) | 133 (92.4) | 155 (89.6) | 116 (92.8) | 151 (89.9) |
| New user | 13 (6.8) | 22 (11.9) | 11 (7.6) | 18 (10.4) | 9 (7.2) | 17 (10.1) |
| Support-required level, No. (%) | ||||||
| Level 1 | 104 (54.7) | 100 (54.1) | 80 (55.6) | 94 (54.3) | 66 (52.8) | 93 (55.4) |
| Level 2 | 86 (45.3) | 85 (45.9) | 64 (44.4) | 79 (45.7) | 59 (47.2) | 75 (44.6) |
| Dementia, No. (%) | ||||||
| Without | 114 (60.0) | 110 (59.5) | 88 (61.1) | 102 (59.0) | 78 (62.4) | 99 (58.9) |
| I | 51 (26.8) | 49 (26.5) | 36 (25.0) | 48 (27.7) | 31 (24.8) | 46 (27.4) |
| II | 25 (13.2) | 26 (14.1) | 20 (13.9) | 23 (13.3) | 16 (12.8) | 23 (13.7) |
| Number of impaired ADL, No. (%) | ||||||
| 0 | 46 (24.2) | 44 (23.8) | 32 (22.2) | 42 (24.3) | 26 (20.8) | 42 (25.0) |
| 1 | 58 (30.5) | 60 (32.4) | 45 (31.2) | 57 (32.9) | 39 (31.2) | 55 (32.7) |
| ≥2 | 86 (45.3) | 81 (43.8) | 67 (46.5) | 74 (42.8) | 60 (48.0) | 71 (42.3) |
| Number of impaired IADL, No. (%) | ||||||
| 0 | 62 (32.6) | 47 (25.4) | 48 (33.3) | 44 (25.4) | 42 (33.6) | 42 (25.0) |
| 1 | 35 (18.4) | 45 (24.3) | 31 (21.5) | 41 (23.7) | 24 (19.2) | 41 (24.4) |
| ≥2 | 93 (48.9) | 93 (50.3) | 65 (45.1) | 88 (50.9) | 59 (47.2) | 85 (50.6) |
| Population | Number of Events/Total Number (%) | p Value | |
|---|---|---|---|
| Intervention Group | Control Group | ||
| ITT population | |||
| Any serious adverse event | 20/190 (10.5) | 16/185 (8.6) | 0.659 |
| Death | 2/190 (1.1) | 3/185 (1.6) | 0.976 |
| Hospitalization | 20/190 (10.5) | 15/185 (8.1) | 0.530 |
| FAS population | |||
| Any serious adverse event | 11/144 (7.6) | 16/173 (9.2) | 0.757 |
| Death | 1/144 (0.7) | 3/173 (1.7) | 0.749 |
| Hospitalization | 11/144 (7.6) | 15/173 (8.7) | 0.898 |
| PPS population | |||
| Any serious adverse event | 10/125 (8.0) | 13/168 (7.7) | 1.000 |
| Death | 1/125 (0.8) | 3/168 (1.8) | 0.834 |
| Hospitalization | 10/125 (8.0) | 12/168 (7.1) | 0.959 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hattori, S.; Yoshida, T.; Okumura, Y.; Kondo, K. Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 3954. https://doi.org/10.3390/ijerph16203954
Hattori S, Yoshida T, Okumura Y, Kondo K. Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(20):3954. https://doi.org/10.3390/ijerph16203954
Chicago/Turabian StyleHattori, Shinji, Toshiyuki Yoshida, Yasuyuki Okumura, and Katsunori Kondo. 2019. "Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 20: 3954. https://doi.org/10.3390/ijerph16203954
APA StyleHattori, S., Yoshida, T., Okumura, Y., & Kondo, K. (2019). Effects of Reablement on the Independence of Community-Dwelling Older Adults with Mild Disability: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(20), 3954. https://doi.org/10.3390/ijerph16203954






