Health Care Financing Systems and Their Effectiveness: An Empirical Study of OECD Countries
Abstract
:1. Introduction
Literature Review
2. Materials and Methods
2.1. Aim of Research
2.2. Description of the Sample
2.3. Analytical Process Description
3. Results
3.1. Descriptive Analysis
3.2. Relation between Health Care Financing Systems and Selected Health Indicators
3.3. Impact of Health Expenditure on Selected Health Care Indicators
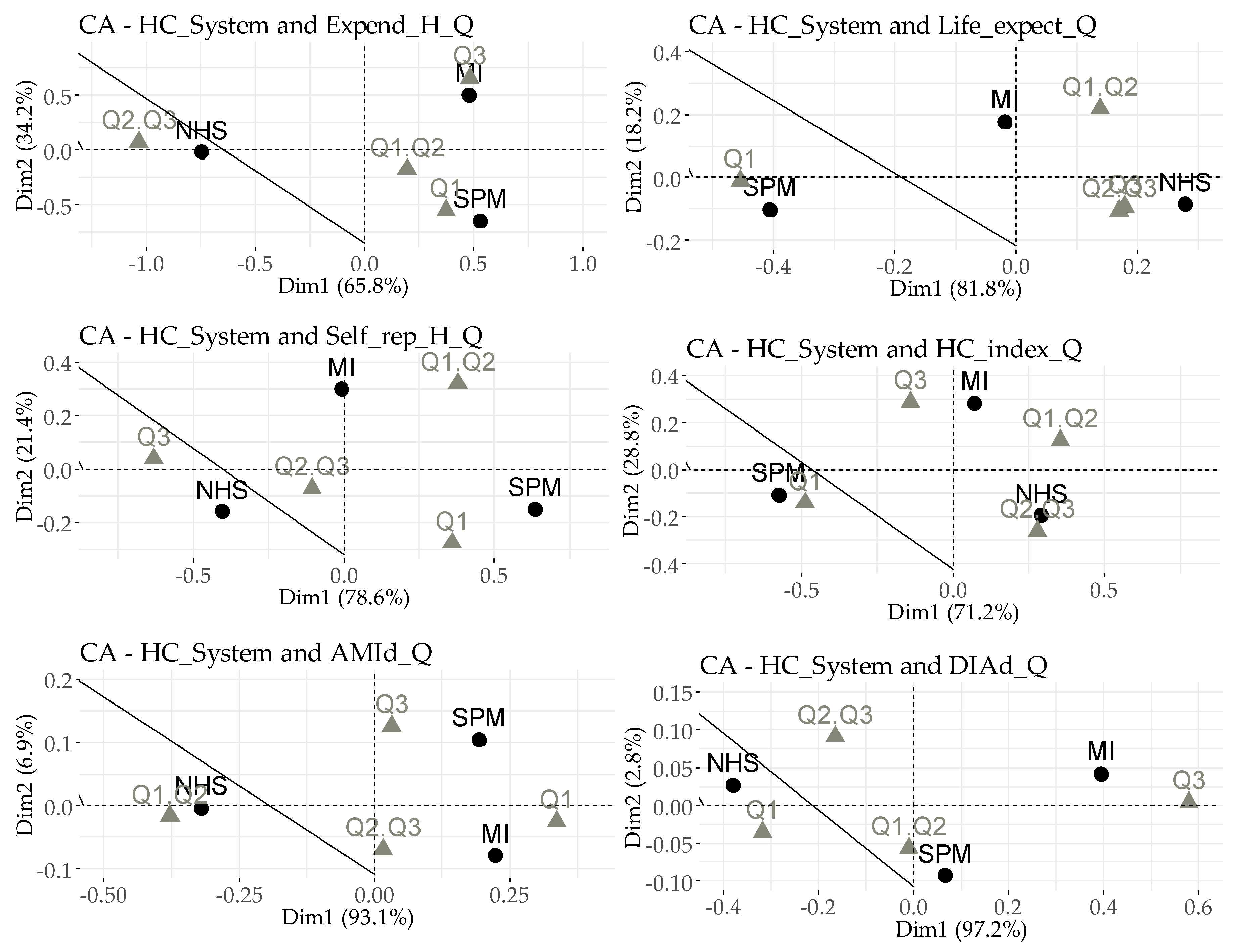
3.4. Correspondence Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AIS | Acute ischemic stroke |
| AMI | Acute myocardial infarction |
| AMId | Deaths from acute myocardial infarction |
| AMId_Q | Deaths from acute myocardial infarction - Quartile |
| DIAd | Deaths from diabetes mellitus |
| DIAd_Q | Deaths from diabetes mellitus - Quartile |
| Expend_H | Health expenditure in the percentage of GDP |
| Expend_H_Q | Expend_H - Quartile |
| GDP | Gross Domestic Product |
| HC_index | Health Care Index |
| HC_index_Q | HC_index - Quartile |
| HC_System | Health Care System |
| Life_expect | Average life expectancy at birth |
| Life_expect_Q | Life_expect - Quartile |
| MI | Multiple insurance funds or companies |
| NHS | A national health system covering the country as a whole |
| SPM | A single health insurance fund (single-payer model) |
| Self_rep_H | Perceived health status (surveyed 5-item scale - good and very good in percentage for all populations) |
| Self_rep_H_Q | Self_rep_H - Quartile |
References
- Devkota, S.; Panda, B. Socioeconomic gradients in early childhood health: Evidence from Bangladesh and Nepal. Int. J. Equity Health 2016, 15, 78. [Google Scholar] [CrossRef]
- The American Association of Pediatrics. Early Childhood Adversity, Toxic Stress, and the Role of the Pediatrician: Translating Developmental Science into Lifelong Health. Pediatrics 2012, 129, 224–231. Available online: http://aappolicy.aappublications.org/ cgi/reprint/pediatrics;129/1/e224.pdf (accessed on 24 December 2018). [CrossRef] [PubMed]
- Fernald, L.C.H.; Kariger, P.; Hidrobo, M.; Gertler, P.J. Socioeconomic gradients in child development in very young children: Evidence from India, Indonesia, Peru, and Senegal. Proc. Nat. Acad. Sci. USA 2012, 109, 17273–17280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, S.; Dansereau, E.A.; Murray, C.J.L. Does distance matter for institutional delivery in rural India? Appl. Econ. 2014, 46, 4091–4103. [Google Scholar] [CrossRef] [Green Version]
- Hanson, C.; Cox, J.; Mbaruku, G.; Manzi, F.; Gabrysch, S.; Schellenberg, D.; Tanner, M.; Ronsmans, C.; Schellenberg, J. Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: A secondary analysis of cross-sectional census data in 226 000 households. Lancet Glob. Health 2015, 3, 387–395. [Google Scholar] [CrossRef]
- Devkota, S.; Panda, B. Childhood Immunization and Access to Health Care: Evidence from Nepal. Asia Pac. J. Public Health 2016, 28, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Bijwaard, G.E.; Myrskyla, M.; Tynelius, P.; Rasmussen, F. Educational gains in cause-specific mortality: Accounting for cognitive ability and family-level confounders using propensity score weighting. Soc. Sci. Med. 2017, 184, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Hamad, R.; Elser, H.; Tran, D.C.; Rehkopf, D.H.; Goodman, S.N. How and why studies disagree about the effects of education on health: A systematic review and meta-analysis of studies of compulsory schooling laws. Soc. Sci. Med. 2018, 212, 168–178. [Google Scholar] [CrossRef]
- Huebener, M. Life expectancy and parental education. Soc. Sci. Med. 2019, 232, 351–365. [Google Scholar] [CrossRef] [Green Version]
- Cameron, L.; Suarez, D.C.; Cornwell, K. Understanding the determinants of maternal mortality: An observational study using the Indonesian Population Census. PLoS ONE 2019, 14, 217386. [Google Scholar] [CrossRef]
- Diener, E.; Chan, M.Y. Happy People Live Longer: Subjective Well-Being Contributes to Health and Longevity. Appl. Psychol. Health Well-Being 2011, 3, 1–43. [Google Scholar] [CrossRef]
- See, K.F.; Yen, S.H. Does happiness matter to health system efficiency? A performance analysis. Health Econ. Rev. 2018, 8, 33. [Google Scholar] [CrossRef]
- Urbanos-Garrido, R.M.; Lopez-Valcarcel, B.G. The influence of the economic crisis on the association between unemployment and health: An empirical analysis for Spain. Eur. J. Health Econ. 2015, 16, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Argaw, M.D.; Binyam, F.D.; Temesgen, A.B.; Abebe, D.A. Improved performance of district health systems through implementing health center clinical and administrative standards in the Amhara region of Ethiopia. Health Serv. Res. 2019, 127. [Google Scholar] [CrossRef] [PubMed]
- Karlsberg Schaffer, S.; Sussex, J.; Devlin, N.; Walker, A. Local health care expenditure plans and their opportunity costs. Health Policy 2015, 119, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Vandersteegen, T.; Marneffe, W.; Cleemput, I.; Vereeck, L. The impact of no-fault compensation on health care expenditures: An empirical study of OECD countries. Health Policy 2015, 119, 367–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Commission. Joint Report on Health Care and Long-Term Care Systems and Fiscal Sustainability. 2016. Available online: https://ec.europa.eu/info/publications/economy-finance/joint-report-health-care-and-long-term-care-systems-fiscal-sustainability-0_en (accessed on 24 December 2018).
- OECD. Fiscal Sustainability of Health Systems: Bridging Health and Finance Perspectives; OECD Publishing: Paris, France, 2015. Available online: https://www.oecd.org/gov/budgeting/Fiscal-Sustainability-of-Health-Systems-Policy-Brief-ENG.pdf (accessed on 24 December 2018).
- OECD/EU. Health at a Glance: Europe 2016: State of Health in the EU Cycle; OECD Publishing: Paris, France, 2016; Available online: https://www.oecd.org/els/health-systems/Health-at-a-Glance-Europe-2016-CHARTSET.pdf (accessed on 24 December 2018).
- Van den Heuvel, W.J.A.; Olaroiu, M. How Important Are Health Care Expenditures for Life Expectancy? A Comparative, European Analysis. J. Am. Med. Dir. Assoc. 2017, 18, 276–279. [Google Scholar] [CrossRef]
- Quercioli, C.; Nisticò, F.; Troiano, G.; Maccari, M.; Messina, G.; Barducci, M.; Carriero, G.; Golinelli, D.; Nante, N. Developing a new predictor of health expenditure: Preliminary results from a primary healthcare setting. Public Health 2018, 163, 121–127. [Google Scholar] [CrossRef]
- Obrizan, M.; Wehby, G.L. Health Expenditures and Global Inequalities in Longevity. World Dev. 2018, 101, 28–36. [Google Scholar] [CrossRef]
- Atilgan, E.; Kilic, D.; Ertugrul, H.M. The dynamic relationship between health expenditure and economic growth: Is the health-led growth hypothesis valid for Turkey? Eur. J. Health Econ. 2017, 18, 567–574. [Google Scholar] [CrossRef]
- Verulava, T.; Dangadze, B. Health capital and economic growth: Evidence from Georgia. Open Public Health J. 2018, 11, 401–406. [Google Scholar] [CrossRef]
- Kumar, S. Systems GMM estimates of the health care spending and GDP relationship: A note. Eur. J. Health Econ. 2013, 14, 503–506. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R. Health and economic growth: Evidence from dynamic panel data of 143 years. PLoS ONE 2018. [Google Scholar] [CrossRef] [PubMed]
- Boachie, M.K. Health and Economic Growth in Ghana: An Empirical Investigation. Fudan J. Humanit. Soc. Sci. 2017, 10, 253–265. [Google Scholar] [CrossRef]
- Barros, P.P. The black box of health care expenditure growth determinants. Health Econ. 1998, 7, 533–544. [Google Scholar] [CrossRef] [Green Version]
- Farag, M.; Nandakumar, A.; Wallack, S.; Hodgkin, D.; Gaumer, G.; Erbil, C. The income elasticity of health care spending in developing and developed countries. Int. J. Health Care Financ. Econ. 2012, 12, 145–162. [Google Scholar] [CrossRef] [PubMed]
- Howdon, D.; Rice, N. Health care expenditures, age, proximity to death and morbidity: Implications for an ageing population. J. Health Econ. 2018, 57, 60–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaba, E.; Balan, C.B.; Robu, L.B. The Relationship between Life Expectancy at Birth and Health Expenditures Estimated by a Cross-country and Time-series Analysis. Procedia Econ. Financ. 2014, 15, 108–114. [Google Scholar] [CrossRef] [Green Version]
- Linden, M.; Ray, D. Life expectancy effects of public and private health expenditures in OECD countries 1970–2012: Panel time series approach. Econ. Anal. Policy 2017, 56, 101–113. [Google Scholar] [CrossRef]
- Farag, M.; Nandakumar, A.; Wallack, S.; Hodgkin, D.; Gaumer, G.; Erbil, C. Health expenditures, health outcomes and the role of good governance. Int. J. Health Care Financ. Econ. 2013, 13, 33–52. [Google Scholar] [CrossRef]
- Cervantes, P.A.M.; Lopez, N.R.; Rambaud, S.C. A Causal Analysis of Life Expectancy at Birth. Evidence from Spain. Int. J. Environ. Res. Public Health 2019, 16, 2367. [Google Scholar] [CrossRef] [PubMed]
- Tobias, M.; Yeh, L. How much does health care contribute to health gain and to health inequality? Trends in amenable mortality in New Zealand 1981–2004. Aust. N. Z. J. Public Health 2009, 33, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Van Baal, P.H.; Wong, A. Time to death and the forecasting of macro-level health care expenditures: Some further considerations. J. Health Econ. 2012, 31, 876–887. [Google Scholar] [CrossRef] [PubMed]
- Bein, M.A.; Unlucan, D.; Olowu, G.; Kalifa, W. Healthcare spending and health outcomes: Evidence from selected East African countries. Afr. Health Sci. 2017, 17, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, M.M.; Avendano, M. Social Policy Expenditures and Life Expectancy in High-Income Countries. Am. J. Prev. Med. 2018, 54, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.H.; Elkins, B.R.; Herrin, J.; Elbel, B. Health and social services expenditures: Associations with health outcomes. BMJ Qual. Saf. 2011, 20, 826–831. [Google Scholar] [CrossRef]
- Crossley, T.F.; Kennedy, S. The reliability of self-assessed health status. J. Health Econ. 2002, 21, 643–658. [Google Scholar] [CrossRef]
- Au, N.; Johnston, D.W. Self-assessed health: What does it mean and what does it hide? Soc. Sci. Med. 2014, 121, 21–28. [Google Scholar] [CrossRef]
- Rivera, B. The effects of public health spending on self-assessed health status: An ordered probit model. Appl. Econ. 2001, 33, 1313–1319. [Google Scholar] [CrossRef]
- Pierard, E. The effect of health care expenditures on self-rated health status and the Health Utility Index: Evidence from Canada. Int. J. Health Econ. Manag. 2016, 16, 1–21. [Google Scholar] [CrossRef]
- Heijink, R.; Koolman, X.; Westert, G.P. Spending more money, saving more lives? The relationship between avoidable mortality and healthcare spending in 14 countries. Eur. J. Health Econ. 2013, 14, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Golinelli, D.; Bucci, A.; Toscano, F.; Filicori, F.; Fantini, M.P. Real and predicted mortality under health spending constraints in Italy: A time trend analysis through artificial neural networks. BMC Health Serv. Res. 2018, 18, 671. [Google Scholar] [CrossRef] [PubMed]
- Bokhari, F.A.S.; Gai, Y.W.; Gottret, P. Government health expenditures and health outcomes. Health Econ. 2007, 16, 257–273. [Google Scholar] [CrossRef] [PubMed]
- Budhdeo, S.; Watkins, J.; Atun, R.; Williams, C.; Zeltner, T.; Maruthappu, M. Changes in government spending on healthcare and population mortality in the European union, 1995–2010: A cross-sectional ecological study. J. R. Soc. Med. 2015, 108, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.H.; Canavan, M.; Rogan, E.; Talbert-Slagle, K.; Ndumele, C.; Taylor, L.; Curry, L.A. Variation in Health Outcomes: The Role of Spending on Social Services, Public Health, and Health Care, 2000-09. Health Aff. 2016, 35, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Moscone, F.; Skinner, J.; Tosetti, E.; Yasaitis, L. The association between medical care utilization and health outcomes: A spatial analysis. Reg. Sci. Urban Econ. 2019, 77, 306–314. [Google Scholar] [CrossRef]
- Likosky, D.S.; Van Parys, J.; Zhou, W.P.; Borden, W.B.; Weinstein, M.C.; Skinner, J.S. Association Between Medicare Expenditure Growth and Mortality Rates in Patients with Acute Myocardial Infarction a Comparison from 1999 Through 2014. Jama Cardiol. 2018, 3, 114–122. [Google Scholar] [CrossRef]
- Zhou, X.; Shrestha, S.S.; Luman, E.; Wang, G.; Zhang, P. Medical Expenditures Associated with Diabetes in Myocardial Infarction and Ischemic Stroke Patients. Am. J. Prev. Med. 2017, 53, 190–196. [Google Scholar] [CrossRef]
- Fezer, Z.; Kovacs, L. The Economic Impact of Diabetes. In Proceedings of the 15th IEEE International Symposium on Intelligent Systems and Informatics, Subotica, Serbia, 14–16 September 2017; pp. 77–82. [Google Scholar]
- Fernandes, J.R.; Ogurtsova, K.; Linnenkamp, U.; Guariguata, L.; Seuring, T.; Zhang, P.; Cavan, D.; Makaroff, L.E. IDF Diabetes Atlas estimates of 2014 global health expenditures on diabetes. Diabetes Res. Clin. Pract. 2016, 117, 48–54. [Google Scholar] [CrossRef] [Green Version]
- Charbonnel, B.; Simon, B.; Dallongeville, J.; Bureau, I.; Dejager, S.; Levy-Bachelot, L.; Gourmelen, J.; Detournay, B. Direct Medical Costs of Type 2 Diabetes in France: An Insurance Claims Database Analysis. Pharmacoecon. Open 2018, 2, 209–219. [Google Scholar] [CrossRef]
- Jonsson, B. The Economic Impact of Diabetes. Diabetes Care 1998, 21, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Baudot, F.O.; Aguade, A.S.; Barnay, T.; Gastaldi-Menager, C.; Fagot-Campagna, A. Impact of type 2 diabetes on health expenditure: Estimation based on individual administrative data. Eur. J. Health Econ. 2019, 20, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Schofield, D.; Shrestha, R.N.; Cunich, M.M.; Passey, M.E.; Veerman, L.; Tanton, R.; Kelly, S.J. The costs of diabetes among Australians aged 45–64 years from 2015 to 2030: Projections of lost productive life years (PLYs), lost personal income, lost taxation revenue, extra welfare payments and lost gross domestic product from Health&WealthMOD2030. BMJ Open 2017, 7, 13158. [Google Scholar] [CrossRef]
- Hussey, P.S.; Wertheimer, S.; Mehrotra, A. The association between health care quality and cost: A systematic review. Ann. Intern. Med. 2013, 158, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.D.; Daneshvar, S. Efficiency Analysis of Healthcare System in Lebanon Using Modified Data Envelopment Analysis. J. Healthc. Eng. 2018. [Google Scholar] [CrossRef] [PubMed]
- Gavurova, B.; Balloni, A.J.; Tarhanicova, M.; Kovac, V. Information and Communication Technology in the Role of Information System of Healthcare Facility in the Slovak Republic. Economies 2018, 6, 47. [Google Scholar] [CrossRef]
- Stefko, R.; Gavurova, B.; Kocisova, K. Healthcare efficiency assessment using DEA analysis in the Slovak Republic. Health Econ. Rev. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Schley, K. Health care service provision in Europe and regional diversity: A stochastic metafrontier approach. Health Econ. Rev. 2018. [Google Scholar] [CrossRef] [PubMed]
- Braendle, T.; Colombier, C. What drives public health care expenditure growth? Evidence from Swiss cantons, 1970–2012. Health Policy 2016, 120, 1051–1060. [Google Scholar] [CrossRef]
- OECDa. List of OECD Member Countries—Ratification of the Convention on the OECD. 2018. Available online: http://www.oecd.org/about/membersandpartners/list-oecd-member-countries.htm (accessed on 24 December 2018).
- OECDb. Health Spending. 2018. Available online: https://data.oecd.org/healthres/health-spending.htm (accessed on 24 December 2018).
- OECDc. Life Expectancy at Birth. 2018. Available online: https://data.oecd.org/healthstat/life-expectancy-at-birth.htm (accessed on 24 December 2018).
- OECDd. Perceived Health Status, Acute Myocardial Infarction, Diabetes Mellitus. 2018. Available online: https://stats.oecd.org/ (accessed on 24 December 2018).
- NUMBEO. Health Care. 2018. Available online: https://www.numbeo.com/health-care/ (accessed on 24 December 2018).
- Mendis, S.; Thygesen, K.; Kuulasmaa, K.; Giampaoli, S.; Mähönen, M.; Ngu Blackett, K.; Lisheng, L.; Writing group on behalf of the participating experts of the WHO consultation for revision of WHO definition of myocardial infarction. World Health Organization definition of myocardial infarction: 2008-09 revision. Int. J. Epidemiol. 2011, 40, 139–146. [Google Scholar] [CrossRef]
- World Health Organisation. about Diabetes. 2014. Available online: https://web.archive.org/web/20140331094533/http://www.who.int/diabetes/action_online/basics/en/# (accessed on 15 September 2019).
- OECDb. Health Systems Characteristics Survey. 2016. Available online: http://www.oecd.org/els/health-systems/OECD-HSC-Survey-2016-Project-outline.pdf (accessed on 24 December 2018).
- National Health Insurance Fund under the Ministry of Health Health Insurance System. 2018. Available online: http://www.vlk.lt/sites/en/health-insurance-in-Lithuania/health-insurance-system (accessed on 24 December 2018).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Gallardo-Albarran, D. Health and economic development since 1900. Econ. Hum. Biol. 2018, 31, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Wang, F. The roles of preventive and curative health care in economic development. PLoS ONE 2018, 13, 206808. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Make Every Mother and Child Count; The World Health Report; WHO: Geneva, Switzerland, 2005. [Google Scholar]
- Ye, L.P.; Zhang, X.P. Nonlinear Granger Causality between Health Care Expenditure and Economic Growth in the OECD and Major Developing Countries. Int. J. Environ. Res. Public Health 2018, 15, 1953. [Google Scholar] [CrossRef] [PubMed]
| Country | HC_System | Expend_H | Life_expect | Self_rep_H | HC_index | AMId | DIAd |
|---|---|---|---|---|---|---|---|
| Australia | NHS | 9.03167 | 82.383 | 85.200 | 74.6717 | 36.620 | 19.260 |
| Austria | MI | 10.33950 | 81.417 | 69.733 | 80.2350 | 44.683 | 28.883 |
| Belgium | MI | 10.32900 | 81.133 | 74.417 | 79.4300 | 32.480 | 11.000 |
| Canada | NHS | 10.47967 | 81.817 | 88.583 | 70.6950 | 37.775 | 19.050 |
| Czech Republic | MI | 7.35200 | 78.717 | 60.650 | 67.8233 | 47.400 | 30.217 |
| Denmark | NHS | 10.18317 | 80.700 | 71.667 | 83.0300 | 26.725 | 20.650 |
| Estonia | SPM | 6.21217 | 77.450 | 52.383 | 73.0217 | 30.640 | 9.340 |
| Finland | NHS | 9.43467 | 81.317 | 68.500 | 73.4600 | 51.300 | 7.400 |
| France | SPM | 11.43650 | 82.467 | 67.483 | 82.0150 | 18.000 | 13.150 |
| Germany | MI | 11.02250 | 80.883 | 65.100 | 74.7783 | 45.680 | 20.520 |
| Greece | SPM | 8.27700 | 81.267 | 74.100 | 55.1667 | 44.520 | 10.140 |
| Hungary | SPM | 7.13433 | 75.767 | 57.483 | 52.4433 | 54.317 | 24.367 |
| Chile | MI | 8.01283 | 79.600 | 60.533 | 60.0033 | 51.440 | 37.160 |
| Iceland | NHS | 8.21933 | 82.583 | 76.380 | 65.7850 | 39.567 | 9.733 |
| Ireland | NHS | 8.75350 | 81.467 | 82.617 | 47.6450 | 55.600 | 14.375 |
| Israel | MI | 7.19067 | 82.217 | 81.567 | 80.2233 | 20.420 | 39.180 |
| Italy | NHS | 8.93800 | 82.867 | 69.267 | 66.2417 | 29.425 | 23.000 |
| Japan | MI | 10.84383 | 83.750 | 35.467 | 84.5583 | 18.020 | 6.360 |
| Korea | SPM | 6.96850 | 81.883 | 32.567 | 80.0100 | 26.360 | 27.240 |
| Latvia | NHS | 5.69433 | 74.400 | 45.883 | 66.0650 | 48.025 | 19.325 |
| Lithuania | NHS | 6.36650 | 74.617 | 44.133 | 68.4767 | 33.483 | 9.067 |
| Luxembourg | SPM | 5.62433 | 82.183 | 71.500 | 76.1100 | 29.340 | 13.600 |
| Mexico | MI | 5.68717 | 74.900 | 65.500 | 71.4750 | 134.480 | 153.200 |
| Netherlands | MI | 10.40267 | 81.567 | 76.117 | 70.5833 | 29.100 | 14.980 |
| New Zealand | NHS | 9.36783 | 81.567 | 89.183 | 76.0783 | 56.000 | 18.900 |
| Norway | NHS | 9.68067 | 82.183 | 77.667 | 76.5233 | 46.380 | 11.540 |
| Poland | SPM | 6.36900 | 77.533 | 58.183 | 58.1983 | 35.520 | 19.220 |
| Portugal | NHS | 9.07333 | 81.067 | 47.133 | 66.8917 | 32.520 | 31.420 |
| Slovak Republic | MI | 7.10600 | 76.817 | 65.917 | 62.0650 | 47.367 | 18.033 |
| Slovenia | SPM | 8.53717 | 80.850 | 64.533 | 65.5067 | 41.675 | 13.100 |
| Spain | NHS | 9.01150 | 83.117 | 72.917 | 74.4083 | 27.080 | 15.360 |
| Switzerland | MI | 11.71950 | 83.217 | 79.767 | 70.9450 | 22.660 | 12.620 |
| Turkey | SPM | 4.31633 | 77.450 | 68.183 | 69.6817 | 98.380 | 40.240 |
| United Kingdom | NHS | 9.47117 | 81.167 | 71.983 | 73.5050 | 35.940 | 8.280 |
| United States | MI | 16.66000 | 78.750 | 87.850 | 67.5983 | 36.320 | 24.460 |
| HC_System | Expend_H | Life_expect | Self_rep_H | HC_index | AMId | DIAd | |
|---|---|---|---|---|---|---|---|
| Total | N | 210 | 209 | 208 | 198 | 169 | 169 |
| M | 8.72132 | 80.320 | 67.399 | 70.3823 | 41.904 | 22.944 | |
| σ | 2.325369 | 2.6279 | 14.1619 | 9.55523 | 22.4545 | 24.6967 | |
| NHS | N | 84 | 84 | 83 | 78 | 65 | 65 |
| M | 8.83610 | 80.804 | 70.727 | 70.5773 | 39.165 | 15.714 | |
| σ | 1.372807 | 2.6960 | 14.8475 | 8.78958 | 9.9542 | 6.8487 | |
| SPM | N | 54 | 54 | 54 | 48 | 44 | 44 |
| M | 7.20837 | 79.650 | 60.713 | 66.9242 | 42.918 | 19.320 | |
| σ | 1.963008 | 2.5097 | 12.1298 | 11.45886 | 23.8262 | 9.8700 | |
| MI | N | 72 | 71 | 71 | 72 | 60 | 60 |
| M | 9.72214 | 80.256 | 68.594 | 72.4765 | 44.127 | 33.435 | |
| σ | 2.839983 | 2.5499 | 13.2052 | 8.36971 | 30.0071 | 37.8888 | |
| Dependent Variable | Expend_H | Life_expect | Self_rep_H | HC_index | AMId | DIAd |
|---|---|---|---|---|---|---|
| Value (η2) | 0.173889 | 0.030625 | 0.082944 | 0.049729 | 0.009801 | 0.103041 |
| Effect size | Medium | Small | Small | Small | Negligible | Small |
| Test output | MCE | Deviance | Hoslem | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Training | Testing | Difference | Null | Residual | Difference | X2 | df | Sig. | |
| Model 1 glm | 0.25781 | 0.16129 | 0.09652 | 164.73000 | 113.37000 | 51.36000 | 13.4880 | 8 | 0.096 |
| Model 2 glm | 0.24219 | 0.09677 | 0.14541 | 170.35000 | 148.98000 | 21.37000 | 34.5900 | 8 | 3.175 × 105 |
| Model 3 glm | 0.15625 | 0.12903 | 0.02722 | 146.11400 | 95.28500 | 50.82900 | 87.0820 | 8 | 1.776 × 1015 |
| Test output | Coefficients | Estimate | Std. Error | z Value | Sig. |
|---|---|---|---|---|---|
| Model 1 (MI) | Intercept | 18.6161043 | 12.1882920 | 1.527 | 0.126668 |
| Expend_H | 0.8688680 | 0.2297883 | 3.781 | 0.000156 | |
| Life_expect | −0.3812744 | 0.1700773 | −2.242 | 0.024976 | |
| Self_rep_H | 0.0005497 | 0.0182596 | 0.030 | 0.975986 | |
| HC_index | 0.0330331 | 0.0286964 | 1.151 | 0.249682 | |
| AMId | −0.0379316 | 0.0240201 | −1.579 | 0.114300 | |
| DIAd | 0.1360077 | 0.0315794 | 4.307 | 1.66 × 105 | |
| Model 2 (NHS) | Intercept | −9.635026 | 8.634763 | −1.116 | 0.26449 |
| Expend_H | −0.231847 | 0.140848 | −1.646 | 0.09975 | |
| Life_expect | 0.112180 | 0.117958 | 0.951 | 0.34160 | |
| Self_rep_H | 0.040759 | 0.018538 | 2.199 | 0.02790 | |
| HC_index | 0.011036 | 0.021793 | 0.506 | 0.61259 | |
| AMId | 0.001823 | 0.015020 | 0.121 | 0.90341 | |
| DIAd | −0.073380 | 0.025037 | −2.931 | 0.00338 | |
| Model 3 (SPM) | Intercept | −14.70290 | 10.06726 | −1.460 | 0.14416 |
| Expend_H | −1.00709 | 0.26322 | −3.826 | 0.00013 | |
| Life_expect | 0.39186 | 0.15651 | 2.504 | 0.01229 | |
| Self_rep_H | −0.06377 | 0.02635 | −2.420 | 0.01552 | |
| HC_index | −0.07570 | 0.03161 | −2.395 | 0.01663 | |
| AMId | 0.01956 | 0.02249 | 0.870 | 0.38448 | |
| DIAd | −0.06013 | 0.03085 | −1.950 | 0.05123 |
| System | Model | N | Model Variable | Unit Roots | Stationary | Outlier | Heteroscedasticityy | Regressioin Model | R2 |
|---|---|---|---|---|---|---|---|---|---|
| MI | Model 1 | 71 | Expend_H --> Life_expect | 0,9749 | <0.01 | 0.0510 | 0.2408 | OLS | 0.1497 |
| Model 2 | 71 | Expend_H --> Self_rep_H | 0.9998 | <0.01 | 0.0045 | 0.3926 | LTS | 0.6276 | |
| Model 3 | 72 | Expend_H --> HC_index | 0.6009 | <0.01 | 0.0043 | 0.3850 | LTS | 0.0946 | |
| Model 4 | 60 | Expend_H --> AMId | 0.9981 | <0.01 | 0.0006 * | 0.0171 | OLS HC3 | 0.0382 | |
| Model 5 | 60 | Expend_H --> DIAd | 0.9848 | <0.01 | 0.0016 * | 0.5756 | OLS | 0.1429 | |
| NHS | Model 6 | 84 | Expend_H --> Life_expect | 0.8630 | <0.01 | 0.0269 | 0.0002 | OLS HC3 | 0.5716 |
| Model 7 | 83 | Expend_H --> Self_rep_H | 0.9996 | <0.01 | 0.0187 | 0.6007 | OLS | 0.4212 | |
| Model 8 | 78 | Expend_H --> HC_index | 0.9585 | <0.01 | 0.0000 | 0.1742 | LTS | 0.1332 | |
| Model 9 | 65 | Expend_H --> AMId | 0.1152 | <0.01 | 0.0096 | 0.0641 | LTS | 0.0410 | |
| Model 10 | 65 | Expend_H --> DIAd | 0.8851 | <0.01 | 0.0034 | 0.7392 | LTS | 0.0389 | |
| NHS | Model 11 | 54 | Expend_H --> Life_expect | 0.7907 | <0.01 | 0.0337 | 0.0183 | OLS HC3 | 0.2397 |
| Model 12 | 54 | Expend_H --> Self_rep_H | 1,0000 | <0.01 | 0.0075 | 0.4002 | LTS | 0.2423 | |
| Model 13 | 48 | Expend_H --> HC_index | 0.9942 | <0.01 | 0.0732 | 0.3909 | OLS | 0.0508 | |
| Model 14 | 44 | Expend_H --> AMId | 0.9997 | <0.01 | 0.0066 | 0.0001 | OLS HC3 | 0.2670 | |
| Model 15 | 44 | Expend_H --> DIAd | 0.9718 | <0.01 | 0.0357 | 0.0002 | OLS HC3 | 0.2778 |
| MI | NHS | SPM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | B | Est. | Sig. | Model | B | Est | Sig. | Model | B | Est. | Sig. |
| Model 1 (Life_expect) | α | 76.90 | 2.00 × 10−16 | Model 6 (Life_expect) | α | 67.68 | 2.20 × 10−16 | Model 11 (Life_expect) | α | 75.14 | 2.20 × 10−16 |
| β1 | 0.35 | 8.59 × 10−4 | β1 | 1.48 | 3.17 × 10−13 | β1 | 0.63 | 5.71 × 10−8 | |||
| Model 2 (Self_rep_H) | α | 48.44 | 2.00 × 10−16 | Model 7 (Self_rep_H) | α | 8.98 | 2.73 × 10−1 | Model 12 (Self_rep_H) | α | 41.02 | 3.17 × 10−10 |
| β1 | 2.32 | 2.86 × 10−14 | β1 | 6.98 | 3.23 × 10−11 | β1 | 2.67 | 3.27 × 10−4 | |||
| Model 3 (HC_index) | α | 64.17 | 2.00 × 10−16 | Model 8 (HC_index) | α | 57.31 | 2.00 × 10−16 | Model 13 (HC_index) | α | 57.43 | 6.20 × 10−12 |
| β1 | 0.93 | 9.09 × 10−3 | β1 | 1.66 | 1.75 × 10−3 | β1 | 1.29 | 1.24 × 10−1 | |||
| sModel 4 (AMId) | α | 45.18 | 5.84 × 10−9 | Model 9 (AMId) | α | 47.97 | 3.61 × 10−9 | Model 14 (AMId) | α | 89.39 | 5.82 × 10−9 |
| β1 | −1.91 | 1.14 × 10−1 | β1 | −1.25 | 1.18 × 10−1 | β1 | −6.56 | 3.29 × 10−4 | |||
| Model 5 (DIAd) | α | 38.38 | 4.86 × 10−9 | Model 10 (DIAd) | α | 7.65 | 9.36 × 10−2 | Model 15 (DIAd) | α | 38.96 | 2.24 × 10−7 |
| β1 | −1.56 | 4.43 × 10−3 | β1 | 0.78 | 1.28 × 10−1 | β1 | −2.77 | 9.83 × 10−4 | |||
| MI | NHS | SPM | |||
|---|---|---|---|---|---|
| Model | Y | Model | Y | Model | Y |
| Model 1 (Life_expect) | 79.91 ** | Model 6 (Life_expect) | 80.63 | Model 11 (Life_expect) | 80.60 * |
| Model 2 (Self_rep_H) | 68.62 | Model 7 (Self_rep_H) | 69.87 + | Model 12 (Self_rep_H) | 64.30 * |
| Model 3 (HC_index) | 72.24 ** | Model 8 (HC_index) | 71.74 ** | Model 13 (HC_index) | - |
| Model 4 (AMId) | - | Model 9 (AMId) | - | Model 14 (AMId) | 32.16 * |
| Model 5 (DIAd) | 24.78 ** | Model 10 (DIAd) | - | Model 15 (DIAd) | 14.77 * |
| Correlation ρ | MI | NHS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | A | B | C | D | E | F | |
| Expend_H | 0.482 | 0.292 | 0.173 | −0.431 | −0.617 | 0.081 | 0.460 | 0.323 | 0.009 | 0.085 | ||
| Life_expect | 0.000 | 0.145 | 0.548 | −0.806 | −0.513 | 0.462 | 0.502 | 0.013 | −0.188 | 0.022 | ||
| Self_rep_H | 0.013 | 0.230 | 0.050 | −0.333 | 0.015 | 0.000 | 0.000 | 0.213 | 0.348 | 0.088 | ||
| HC_index | 0.147 | 0.000 | 0.681 | −0.425 | −0.246 | 0.004 | 0.908 | 0.063 | 0.008 | 0.015 | ||
| AMId | 0.001 | 0.000 | 0.009 | 0.001 | 0.586 | 0.944 | 0.133 | 0.005 | 0.950 | −0.263 | ||
| DIAd | 0.000 | 0.000 | 0.910 | 0.058 | 0.000 | 0.499 | 0.860 | 0.489 | 0.911 | 0.034 | ||
| SPM | TOTAL | |||||||||||
| Expend_H | 0.365 | 0.072 | 0.132 | −0.248 | −0.359 | 0.490 | 0.430 | 0.348 | −0.272 | −0.225 | ||
| Life_expect | 0.007 | 0.344 | 0.566 | −0.662 | −0.286 | 0.000 | 0.436 | 0.381 | −0.553 | −0.299 | ||
| Self_rep_H | 0.603 | 0.011 | −0.165 | 0.201 | −0.259 | 0.000 | 0.000 | 0.088 | −0.004 | −0.042 | ||
| HC_index | 0.370 | 0.000 | 0.261 | −0.648 | −0.033 | 0.000 | 0.000 | 0.222 | −0.382 | −0.089 | ||
| AMId | 0.105 | 0.000 | 0.190 | 0.000 | 0.361 | 0.000 | 0.000 | 0.963 | 0.000 | 0.317 | ||
| DIAd | 0.017 | 0.059 | 0.090 | 0.841 | 0.016 | 0.003 | 0.000 | 0.591 | 0.261 | 0.000 | ||
| Country | HC_System | Expend_H | Life_expect | Self_rep_H | HC_index | AMId | DIAd |
|---|---|---|---|---|---|---|---|
| Australia | NHS | Q2–Q3 | Q3 | Q3 | Q2–Q3 | Q1–Q2 | Q2–Q3 |
| Austria | MI | Q3 | Q2–Q3 | Q2–Q3 | Q3 | Q2–Q3 | Q3 |
| Belgium | MI | Q2–Q3 | Q1–Q2 | Q2–Q3 | Q3 | Q1–Q2 | Q1 |
| Canada | NHS | Q3 | Q2–Q3 | Q3 | Q1–Q2 | Q2–Q3 | Q2–Q3 |
| Czech_R | MI | Q1–Q2 | Q1 | Q1–Q2 | Q1–Q2 | Q2–Q3 | Q3 |
| Denmark | NHS | Q2–Q3 | Q1–Q2 | Q2–Q3 | Q3 | Q1 | Q2–Q3 |
| Estonia | SPM | Q1 | Q1 | Q1 | Q2–Q3 | Q1–Q2 | Q1 |
| Finland | NHS | Q2–Q3 | Q2–Q3 | Q1–Q2 | Q2–Q3 | Q3 | Q1 |
| France | SPM | Q3 | Q3 | Q1–Q2 | Q3 | Q1 | Q1–Q2 |
| Germany | MI | Q3 | Q1–Q2 | Q1–Q2 | Q2–Q3 | Q2–Q3 | Q2–Q3 |
| Greece | SPM | Q1–Q2 | Q1–Q2 | Q2–Q3 | Q1 | Q2–Q3 | Q1 |
| Hungary | SPM | Q1–Q2 | Q1 | Q1 | Q1 | Q3 | Q2–Q3 |
| Chile | MI | Q1–Q2 | Q1–Q2 | Q1 | Q1 | Q3 | Q3 |
| Iceland | NHS | Q1–Q2 | Q3 | Q2–Q3 | Q1 | Q2–Q3 | Q1 |
| Ireland | NHS | Q1–Q2 | Q2–Q3 | Q3 | Q1 | Q3 | Q1–Q2 |
| Israel | MI | Q1–Q2 | Q3 | Q3 | Q3 | Q1 | Q3 |
| Italy | NHS | Q1–Q2 | Q3 | Q1–Q2 | Q1–Q2 | Q1–Q2 | Q2–Q3 |
| Japan | MI | Q3 | Q3 | Q1 | Q3 | Q1 | Q1 |
| Korea | SPM | Q1 | Q2–Q3 | Q1 | Q3 | Q1 | Q3 |
| Latvia | NHS | Q1 | Q1 | Q1 | Q1 | Q3 | Q2–Q3 |
| Lithuania | NHS | Q1 | Q1 | Q1 | Q1–Q2 | Q1–Q2 | Q1 |
| Luxembourg | SPM | Q1 | Q2-Q3 | Q2–Q3 | Q2–Q3 | Q1 | Q1–Q2 |
| Mexico | MI | Q1 | Q1 | Q1–Q2 | Q2–Q3 | Q3 | Q3 |
| Netherlands | MI | Q3 | Q2–Q3 | Q2–Q3 | Q1–Q2 | Q1 | Q1-Q2 |
| New Zealand | NHS | Q2–Q3 | Q2–Q3 | Q3 | Q2–Q3 | Q3 | Q1-Q2 |
| Norway | NHS | Q2–Q3 | Q2–Q3 | Q3 | Q3 | Q2-Q3 | Q1 |
| Poland | SPM | Q1 | Q1 | Q1 | Q1 | Q1-Q2 | Q2-Q3 |
| Portugal | NHS | Q2–Q3 | Q1–Q2 | Q1 | Q1–Q2 | Q1-Q2 | Q3 |
| Slovak_R | MI | Q1 | Q1 | Q1–Q2 | Q1 | Q2-Q3 | Q1-Q2 |
| Slovenia | SPM | Q1–Q2 | Q1–Q2 | Q1–Q2 | Q1 | Q2–Q3 | Q1–Q2 |
| Spain | NHS | Q2–Q3 | Q3 | Q2–Q3 | Q2–Q3 | Q1 | Q1–Q2 |
| Switzerland | MI | Q3 | Q3 | Q3 | Q1–Q2 | Q1 | Q1–Q2 |
| Turkey | SPM | Q1 | Q1 | Q1–Q2 | Q1–Q2 | Q3 | Q3 |
| United Kingdom | NHS | Q2–Q3 | Q1–Q2 | Q2–Q3 | Q2–Q3 | Q1–Q2 | Q1 |
| United States | MI | Q3 | Q1–Q2 | Q3 | Q1–Q2 | Q1–Q2 | Q2–Q3 |
| Test output | Expend_H | Life_expect | Self_rep_H | HC_index | AMId | DIAd | |
|---|---|---|---|---|---|---|---|
| Eigenvalues | Variance (Dim 1) | 0.3720 | 0.0740 | 0.1700 | 0.1150 | 0.0690 | 0.1370 |
| % of var. (Dim 1) | 65.7930 | 81.8040 | 78.6160 | 71.2470 | 99.3840 | 97.5630 | |
| Variance (Dim 2) | 0.1930 | 0.0160 | 0.0460 | 0.0470 | 0.0000 | 0.0030 | |
| % of var. (Dim 2) | 34.2070 | 18.1960 | 21.3840 | 28.7530 | 0.6160 | 2.4370 | |
| Χ2 | Value | 118.7589 | 18.9051 | 45.0550 | 32.0890 | 11.7886 | 23.7699 |
| Sig. | 2.97 × 10−23 | 4.33 × 10−3 | 4.56 × 10−8 | 1.57 × 10−5 | 6.69 × 10-2 | 5.76 × 10−4 | |
| Correlation (π) | 0.7520 | 0.3008 | 0.4654 | 0.4026 | 0.2641 | 0.3750 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanková, V.; Kotulič, R.; Gonos, J.; Rigelský, M. Health Care Financing Systems and Their Effectiveness: An Empirical Study of OECD Countries. Int. J. Environ. Res. Public Health 2019, 16, 3839. https://doi.org/10.3390/ijerph16203839
Ivanková V, Kotulič R, Gonos J, Rigelský M. Health Care Financing Systems and Their Effectiveness: An Empirical Study of OECD Countries. International Journal of Environmental Research and Public Health. 2019; 16(20):3839. https://doi.org/10.3390/ijerph16203839
Chicago/Turabian StyleIvanková, Viera, Rastislav Kotulič, Jaroslav Gonos, and Martin Rigelský. 2019. "Health Care Financing Systems and Their Effectiveness: An Empirical Study of OECD Countries" International Journal of Environmental Research and Public Health 16, no. 20: 3839. https://doi.org/10.3390/ijerph16203839
APA StyleIvanková, V., Kotulič, R., Gonos, J., & Rigelský, M. (2019). Health Care Financing Systems and Their Effectiveness: An Empirical Study of OECD Countries. International Journal of Environmental Research and Public Health, 16(20), 3839. https://doi.org/10.3390/ijerph16203839





