Association between Sense of Coherence and Mental Health in Caregivers of Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Sample, and Settings
2.2. Data Collection
2.3. Ethical Considerations
2.4. Measurements
2.4.1. Sociodemographic Variables
2.4.2. Sense of Coherence
2.4.3. Subjective Burden
2.4.4. Anxiety and Depression
2.4.5. Quality of Life
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis
3.2. Multivariate Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Organisation for Economic Co-operation and Development O. Recipients of long-term care. In Health at a Glance; OECD Publishing: Paris, France, 2015; pp. 200–201. [Google Scholar]
- Eurocarers. The Gender Dimension of Informal Care. Eurocarers Newsletter (Serial on the Internet). 2018, Volume 30. Available online: http://www.eurocarers.org/userfiles/files/The%20gender%20dimension%20of%20informal%20care.pdf (accessed on 9 October 2019).
- Organisation for Economic Co-operation and Development, O. Informal carers. In Health at a Glance; OECD Publishing: Paris, France, 2015; pp. 202–203. [Google Scholar]
- Del-Pino-Casado, R. Factores Culturales y Sobrecarga Subjetiva en el Cuidado Familiar de Mayores Dependientes. (Cultural Factors and Subjective Overload in the Family Care of Elderly Dependents). Facultad de Ciencias de la Salud Departamento de Enfermería (serial on the Internet). 2013. Available online: http://ruja.ujaen.es/bitstream/10953/453/1/9788484397175.pdf (accessed on 9 October 2019).
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Rodríguez-Pérez, M.; Abreu-Sánchez, A.; Rojas-Ocaña, M.J.; del-Pino-Casado, R. Coping strategies and quality of life in caregivers of dependent elderly relatives. Health Qual. Life Outcomes 2017, 15, 1–71. [Google Scholar] [CrossRef]
- WHO QoLAG. Qué calidad de vida?/Grupo de la OMS sobre la calidad de vida. (What is quality of life?). Foro Mundial de la Salud. 1996, 17, 385–387. [Google Scholar]
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- Eriksson, M.; Lindström, B. A salutogenic interpretation of the Ottawa Charter. Health Promot. Int. 2008, 23, 190–199. [Google Scholar] [CrossRef]
- Lindström, B.; Eriksson, M. Salutogenesis. J. Epidemiol. Commun. Health 2005, 59, 440–442. [Google Scholar] [CrossRef]
- Eriksson, M.; Mittelmark, M.B. The sense of coherence and its measurement. In The Handbook of Salutogenesis; Springer: Basel, Switzerland, 2017; pp. 97–106. [Google Scholar]
- Hsiao, C.Y.; Tsai, Y.F. Factors of caregiver burden and family functioning among Taiwanese family caregivers living with schizophrenia. J. Clin. Nurs. 2014, 24, 1546–1556. [Google Scholar] [CrossRef]
- Mizuno, E.; Iwasaki, M.; Sakai, I.; Kamizawa, N. Sense of Coherence and Quality of Life in Family Caregivers of Persons With Schizophrenia Living in the Community. Arch. Psychiatr. Nurs. 2012, 26, 295–306. [Google Scholar] [CrossRef]
- Jaracz, K.; Grabowska-Fudala, B.; Kozubski, W. Caregiver burden after stroke: Towards a structural model. Neurol. Neurochir. Pol. 2012, 46, 224–232. [Google Scholar] [CrossRef]
- Orgeta, V.; Sterzo, E.L. Sense of coherence, burden, and affective symptoms in family carers of people with dementia. Int. Psychogeriatr. 2013, 25, 973–980. [Google Scholar] [CrossRef]
- Myaskovsky, L.; Dew, M.A.; Switzer, G.E.; McNulty, M.L.; DiMartini, A.F.; McCurry, K.R. Quality of life and coping strategies among lung transplant candidates and their family caregivers. Soc. Sci. Med. 2005, 60, 2321–2332. [Google Scholar] [CrossRef]
- Rodríguez-Sánchez, E.; Pérez-Peñaranda, A.; Losada-Baltar, A.; Pérez-Arechaederra, D.; Gómez-Marcos, M.Á.; Patino-Alonso, M.C.; García-Ortiz, L. Relationships between quality of life and family function in caregiver. BMC Family Pract. 2011, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Zarzycka, B.; Rydz, E. Explaining the relationship between post-critical beliefs and sense of coherence in Polish young, middle, and late adults. J. Relig. Health 2014, 53, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Kase, T.; Ueno, Y.; Oishi, K. The overlap of sense of coherence and the Big Five personality traits: A confirmatory study. Health Psychol. Open 2018, 5, 2055102918810654. [Google Scholar] [CrossRef] [PubMed]
- Hotelling, H. Relations between two sets of variates. Biometrika 1936, 28, 321–377. [Google Scholar] [CrossRef]
- Catena, A. Análisis Multivariado un Manual para Investigadores. (Multivariate Analysis a Manual for Researchers); Biblioteca Nueva: Madrid, Spain, 2003. [Google Scholar]
- Osterlind, S.J.; Tabachnick, B.G.; Fidell, L.S. SPSS for Window Workbook to Acompany Tabachnick and Fidell: Using Multivariate Statistics; Allyn and Bacon: Boston, MA, USA, 2001. [Google Scholar]
- Crespín Elías, E. Análisis Multivariante: Aplicaciones Con SPSS. (Multivariate Analysis: Applications with SPSS); Instituto de Ciencia, Tecnología e Innovación (ICTI): San Salvador, Salvador, 2016. [Google Scholar]
- Antonovsky, A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 1993, 36, 725–733. [Google Scholar] [CrossRef]
- Virués-Ortega, J.; Martínez-Martín, P.; del Barrio, J.L.; Lozano, L.M. Validación transcultural de la Escala de Sentido de Coherencia de Antonovsky (OLQ-13) en ancianos mayores de 70 años (Cross-cultural validation of the Antonovsky Consciousness Scale (OLQ-13) in elderly people over 70 years of age). Medicina Clínica 2007, 128, 486–492. [Google Scholar] [CrossRef]
- Robinson, B.C. Validation of a caregiver strain index. J. Gerontol. 1983, 38, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Moral Serrano, M.S.; Juan Ortega, J.; López Matoses, M.J.; Pellicer Magraner, P. Perfil y riesgo de morbilidad psíquica en cuidadores de pacientes ingresados en su domicilio (Profile and risk of psychic morbidity in caregivers of patients admitted to their home). Atención Primaria. 2003, 32, 77–83. [Google Scholar] [CrossRef]
- López Alonso, S.R.; Moral Serrano, M.S. Validación del Índice de Esfuerzo del Cuidador en la población española (Validation of the Caregiver Strain Index in a Spanish population). Enfermería Comunitaria 2005, 1, 12–17. [Google Scholar]
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting anxiety and depression in general medical settings. BMJ Br. Med. J. 1988, 297, 897–899. [Google Scholar] [CrossRef]
- Montón Franco, C.; Pérez Echevarría, M.; Campos, R.; García Campayo, J.; Lobo, A. Escalas de ansiedad y depresión de Goldberg: Una guía de entrevista eficaz para la detección del malestar psíquico (Goldberg anxiety and depression scales: An effective interview guide for the detection of psychic distress). Atención Primaria. 1993, 12, 345–349. [Google Scholar]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Vilagut, G.; Garin, O.; Cunillera, O.; Tresserras, R.; Brugulat, P.; Alonso, J. Normas de referencia para el Cuestionario de Salud SF-12 versión 2 basadas en población general de Cataluña (Reference standards for the Health Questionnaire SF-12 version 2 based on the general population of Cataluña). Med. Clín. 2012, 139, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Box, G.E.; Cox, D.R. An analysis of transformations. J. R. Stat. Soc. Ser. B (Methodol.) 1964, 26, 211–252. [Google Scholar] [CrossRef]
- Eriksson, M.; Lindstrom, B.; Lilja, J. A sense of coherence and health. Salutogenesis in a societal context: Aland, a special case? J. Epidemiol. Community Health 2007, 61, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Lindström, B. Antonovsky’s sense of coherence scale and the relation with health: A systematic review. J. Epidemiol. Community Health 2006, 60, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.C.; Lee, J.L.; Ketheeswaran, P.; Jones, C.M.; Revicki, D.A.; Wu, A.W. Does personality affect health-related quality of life? A systematic review. PLoS ONE 2017, 12, e0173806. [Google Scholar] [CrossRef] [PubMed]
- Khanjari, S.; Oskouie, F.; Langius-Eklöf, A. Lower sense of coherence, negative religious coping, and disease severity as indicators of a decrease in quality of life in iranian family caregivers of relatives with breast cancer during the first 6 months after diagnosis. Cancer Nurs. 2012, 35, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Hao, Y.; George, S.M.; Wang, L. Factors associated with health-related quality of life among Chinese caregivers of the older adults living in the community: A cross-sectional study. Health Qual. Life Outcomes 2012, 10, 143. [Google Scholar] [CrossRef]
- Välimäki, T.H.; Vehviläinen-Julkunen, K.M.; Pietilä, A.-M.K.; Pirttilä, T.A. Caregiver depression is associated with a low sense of coherence and health-related quality of life. Aging Ment. Health 2009, 13, 799–807. [Google Scholar] [CrossRef]
- Tang, S.T.; Cheng, C.C.J.; Lee, K.C.; Chen, C.H.; Liu, L.N. Mediating effects of sense of coherence on family caregivers’ depressive distress while caring for terminally ill cancer patients. Cancer Nurs. 2013, 36, E25–E33. [Google Scholar] [CrossRef]
- Del-Pino-Casado, R.; Espinosa-Medina, A.; López-Martínez, C.; Orgeta, V. Sense of coherence, burden and mental health in caregiving: A systematic review and meta-analysis. J. Affect. Disord. 2019, 242, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2003, 58, P112–P128. [Google Scholar] [CrossRef] [PubMed]
- Del-Pino-Casado, R.; Millán-Cobo, M.D.; Palomino-Moral, P.A.; Frías-Osuna, A. Cultural correlates of burden in primary caregivers of older relatives: A cross-sectional study. J. Nur. Scholarsh. 2014, 46, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Sutter, M.; Perrin, P.B.; Peralta, S.V.; Stolfi, M.E.; Morelli, E.; Pena Obeso, L.A.; Arango-Lasprilla, J.C. Beyond Strain: Personal Strengths and Mental Health of Mexican and Argentinean Dementia Caregivers. J. Transcult. Nurs. 2016, 27, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Watson, B.; Tatangelo, G.; McCabe, M. Depression and Anxiety Among Partner and Offspring Carers of People with Dementia: A Systematic Review. Gerontologist 2018. [Google Scholar] [CrossRef]
- Zhu, W.; Jiang, Y. A Meta-analytic Study of Predictors for Informal Caregiver Burden in Patients with Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 3636–3646. [Google Scholar] [CrossRef]
- Lim, H.; Han, K. Effects of the Family Resilience Enhancement Program for families of patients with chronic schizophrenia. J. Korean Acad. Nurs. 2013, 43, 133–142. [Google Scholar] [CrossRef]
- Odajima, Y.; Kawaharada, M.; Wada, N. Development and validation of an educational program to enhance sense of coherence in patients with diabetes mellitus type 2. Nagoya J. Med. Sci. 2017, 79, 363–374. [Google Scholar]
- Malm, D.; Fridlund, B.; Ekblad, H.; Karlstrom, P.; Hag, E.; Pakpour, A.H. Effects of brief mindfulness-based cognitive behavioural therapy on health-related quality of life and sense of coherence in atrial fibrillation patients. Eur. J. Cardiovasc. Nurs. 2018, 7, 589–597. [Google Scholar] [CrossRef]
- Forsberg, K.A.; Bjorkman, T.; Sandman, P.O.; Sandlund, M. Influence of a lifestyle intervention among persons with a psychiatric disability: A cluster randomised controlled trail on symptoms, quality of life and sense of coherence. J. Clinic. Nurs. 2010, 19, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, Y.; Togari, T.; Sakano, J. Asian Perspectives and Evidence on Health Promotion and Education. In Asian Perspectives and Evidence on Health Promotion and Education; Muto, T., Nakahara, T., Nam, E.W., Eds.; Springer: New York, NY, USA, 2011; pp. 118–132. [Google Scholar]
| Caregivers | ||
|---|---|---|
| n (%) or M (SD) [Range] | ||
| Age (years) | 56.3 (11.8) [23–89] | |
| Gender | Women | 114 (86.4%) |
| Men | 18 (13.6%) | |
| Kinship tie | Spouse | 17 (12.9%) |
| Offspring | 98 (74%) | |
| Political children | 6 (4.5%) | |
| Other | 11 (8.3%) | |
| Duration (years) | 9.19 (7.879) [0.67–47] | |
| Sense of coherence | 63.6 (13.6) [13–91] | |
| Meaningfulness | 21.29 (5.059) [4–28] | |
| Manageability | 19.20 (5.068) [4–28] | |
| Comprehensibility | 23.11 (6.084) [5–35] | |
| Subjective burden | 5.39 (3.165) [0–13] | |
| Anxiety | 4.06 (2.931) [0–9] | |
| Depressive symptoms | 2.91 (2.742) [0–9] | |
| Quality of life (mental component) | 34.38 (9.090) [0–100] | |
| Care Recipients | ||
| n (%) or M (SD) [Range] | ||
| Age (in years) | 85.30 (6.16) [67–100] | |
| Gender | Women | 100 (75.8%) |
| Men | 32 (24.2%) | |
| Type of dependence | Physical | 79 (59.8%) |
| Mixed | 52 (39.4%) | |
| Psychic | 1 (0.8%) | |
| Cause of dependence | Chronic problems | 62 (47%) |
| Physical impairment | 39 (29.6%) | |
| Cognitive impairment | 15 (11.4%) | |
| Terminal patient | 10 (7.6%) | |
| Stroke | 4 (3.1%) | |
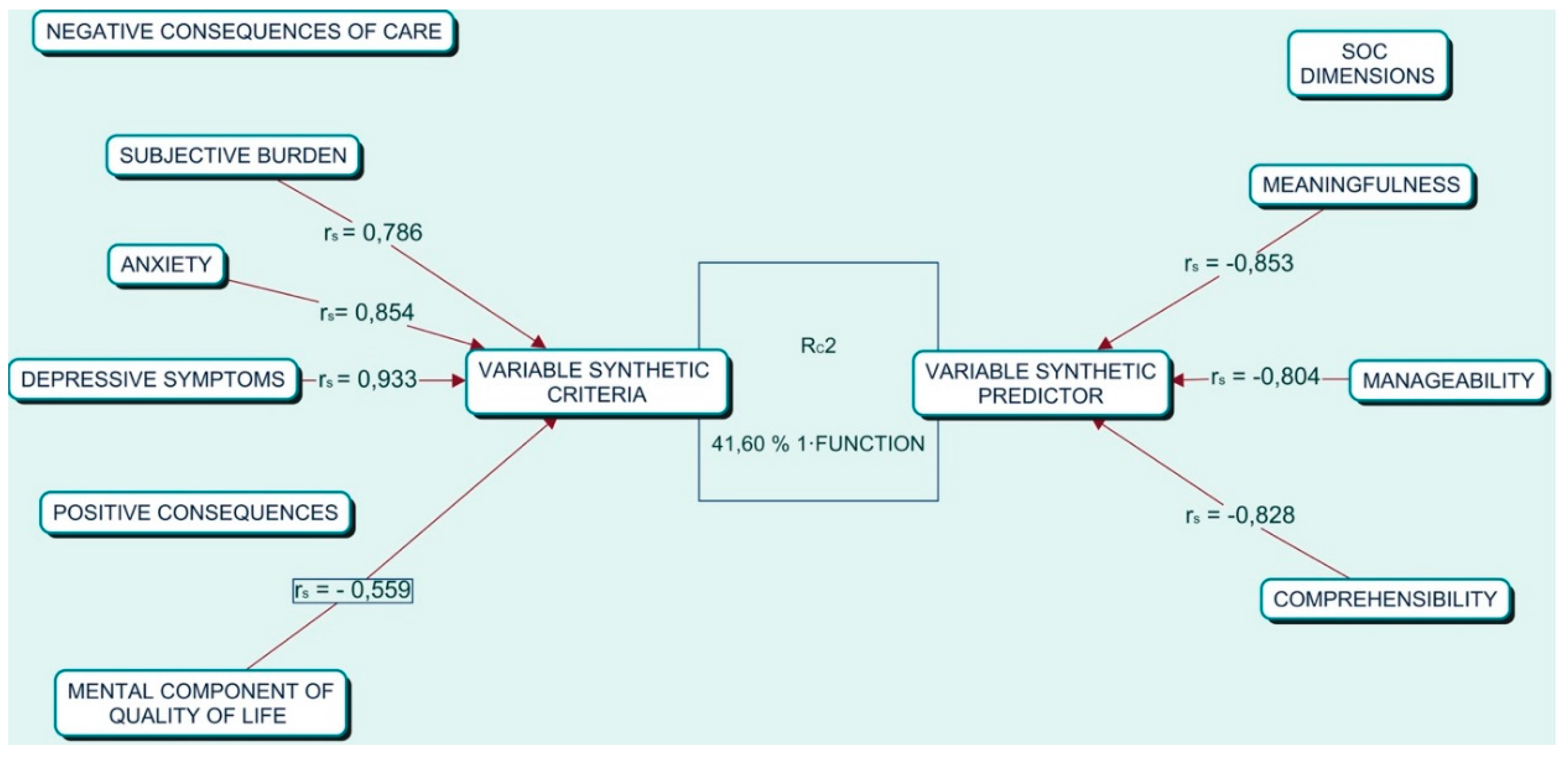
| Variables | Function 1 | Function 2 | h2 | ||||
|---|---|---|---|---|---|---|---|
| Coef. | rs | rs2 (%) | Coef. | rs | rs2 (%) | ||
| Meaningfulness | −0.519 | −0.853 | 72.76 | 0.718 | 0.400 | 16 | 88.76 |
| Manageability | −0.366 | −0.804 | 64.64 | −1.179 | −0.594 | 35.28 | 99.92 |
| Comprehensibility | −0.317 | −0.828 | 68.55 | 0.406 | 0.030 | 0.09 | 68.64 |
| RC2 | 41.60 | 14.66 | |||||
| Subjective burden | 0.329 | 0.786 | 61.77 | −0.386 | −0.061 | 0.37 | 62.14 |
| Anxiety | 0.177 | 0.854 | 72.93 | 1.433 | 0.474 | 22.46 | 95.39 |
| Depressive symptom | 0.572 | 0.933 | 87.04 | −1.166 | −0.170 | 2.89 | 89.93 |
| Quality of Life/mental component | −0.101 | −0.559 | 31.24 | −0.300 | −0.331 | 10.95 | 42.19 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Martínez, C.; Serrano-Ortega, N.; Moreno-Cámara, S.; del-Pino-Casado, R. Association between Sense of Coherence and Mental Health in Caregivers of Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 3800. https://doi.org/10.3390/ijerph16203800
López-Martínez C, Serrano-Ortega N, Moreno-Cámara S, del-Pino-Casado R. Association between Sense of Coherence and Mental Health in Caregivers of Older Adults. International Journal of Environmental Research and Public Health. 2019; 16(20):3800. https://doi.org/10.3390/ijerph16203800
Chicago/Turabian StyleLópez-Martínez, Catalina, Natalia Serrano-Ortega, Sara Moreno-Cámara, and Rafael del-Pino-Casado. 2019. "Association between Sense of Coherence and Mental Health in Caregivers of Older Adults" International Journal of Environmental Research and Public Health 16, no. 20: 3800. https://doi.org/10.3390/ijerph16203800
APA StyleLópez-Martínez, C., Serrano-Ortega, N., Moreno-Cámara, S., & del-Pino-Casado, R. (2019). Association between Sense of Coherence and Mental Health in Caregivers of Older Adults. International Journal of Environmental Research and Public Health, 16(20), 3800. https://doi.org/10.3390/ijerph16203800





