Potential Effects of Lung Function Reduction on Health-Related Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Lung Function
2.3. Assessment of HRQOL Scale
2.4. Covariates
2.5. Ethical Approval
2.6. Statistical Analysis
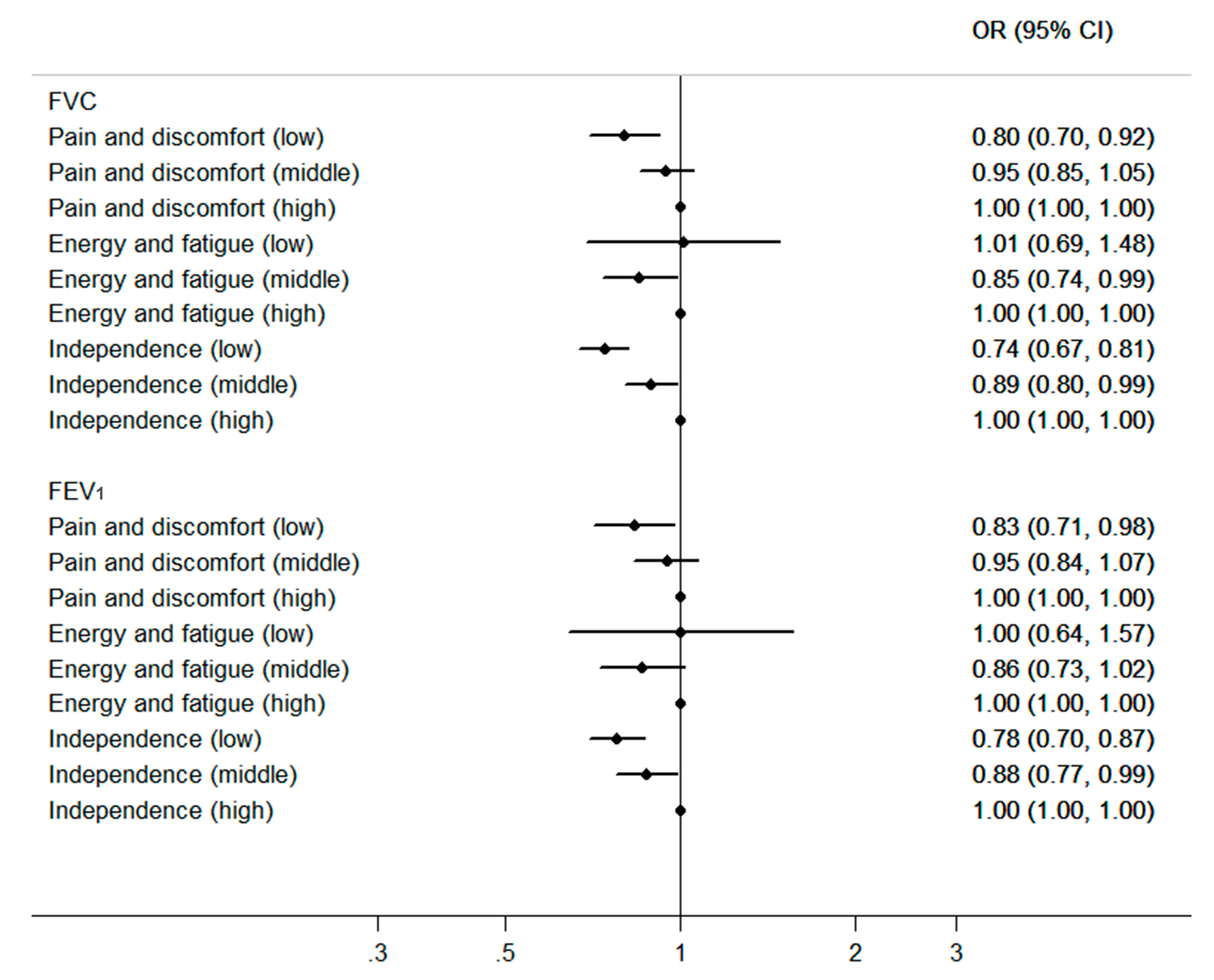
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- Programme on Mental Health WHOQOL User Manual. Available online: http://www.who.int/mental_health/evidence/who_qol_user_manual_98.pdf (accessed on 4 May 2017).
- Carone, M.; Bertolotti, G.; Anchisi, F.; Zotti, A.M.; Donner, C.F.; Jones, P.W. Analysis of factors that characterize health impairment in patients with chronic respiratory failure. Eur. Respir. J. 1999, 13, 1293–1300. [Google Scholar] [CrossRef] [PubMed]
- Koinis-Mitchell, D.; Kopel, S.J.; Seifer, R.; LeBourgeois, M.; McQuaid, E.L.; Esteban, C.A.; Boergers, J.; Nassau, J.; Farrow, M.; Fritz, G.K.; et al. Asthma-related lung function, sleep quality, and sleep duration in urban children. Sleep Health 2017, 3, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Ketelaars, C.A.J.; Schlosser, M.A.G.; Mostert, R.; Abu-Saad, H.H.; Halfen, R.J.G.; Wouters, E.F.M. Determinants of health-related quality of life in patients with chronic obstructive pulmonary disease. Thorax 1996, 51, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Berry, C.E.; Drummond, M.B.; Han, M.K.; Li, D.; Fuller, C.; Limper, A.H.; Martinez, F.J.; Schwarz, M.I.; Sciurba, F.C.; Wise, R.A. Relationship between lung function impairment and health-related quality of life in COPD and interstitial lung disease. Chest 2012, 142, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, A.; Brand, P.L.; Dekkert, F.W.; Kerstjens, H.A.M.; Postma, D.S.; Sluiter, H.J. Quality-of-life in a long-term multicentre trial in chronic nonspecific lung disease: Assessment at baseline. Eur. Respir. J. 1993, 6, 1479–1484. [Google Scholar] [PubMed]
- Bentsen, S.B.; Rokne, B.; Wahl, A.K. Comparison of health-related quality of life between patients with chronic obstructive pulmonary disease and the general population. Scand. J. Caring Sci. 2013, 27, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Salık, Y.; Ozalevli, S.; Cımrın, A.H. Cognitive function and its effects on the quality of life status in the patients with chronic obstructive pulmonary disease (COPD). Arch. Gerontol. Geriatr. 2007, 45, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Lirong, L.; Yingxiang, L.; Ting, Y.; Hong, Z.; Jie, L.; Chen, W. Determinants of health-related quality of life worsening in patients with chronic obstructive pulmonary disease at one year. Chin. Med. J. 2014, 127, 4–10. [Google Scholar] [CrossRef]
- Habraken, J.M.; van der Wal, W.M.; ter Riet, G.; Weersink, E.J.M.; Toben, F.; Bindels, P.J.E. Health-related quality of life and functional status in end-stage COPD: A longitudinal study. Eur. Respir. J. 2010, 37, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Hindu, K.; Rani, N.V.; Prasad, B.H.; Kannan, G.; Thennarasu, P. Impact of severity of the disease on cost of illness and quality of life of patients with chronic obstructive pulmonary disease. J. Young Pharm. 2015, 7, 106–112. [Google Scholar] [CrossRef]
- Abbott, J.; Hurley, M.A.; Morton, A.M.; Conway, S.P. Longitudinal association between lung function and health-related quality of life in cystic fibrosis. Thorax 2013, 68, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Cho, E.J.; Kim, M.H.; Cho, W.H.; Jeon, D.S.; Kim, Y.S.; Lee, M.K. Association of health-related quality of life with disease severity in patients with chronic obstructive pulmonary disease. Chest 2013, 144, 720A. [Google Scholar] [CrossRef]
- Garcia-Gordillo, M.Á.; Collado-Mateo, D.; Olivares, P.R.; Adsuar, J.C.; Merellano-Navarro, E. A cross-sectional assessment of health-related quality of life among patients with chronic obstructive pulmonary disease. Chest 2017, 144, 1046–1053. [Google Scholar]
- Wang, F.; Zhu, J.; Yao, P.; Li, X.; He, M.; Liu, Y.; Yuan, J.; Chen, W.; Zhou, L.; Min, X.; et al. Cohort Profile: The Dongfeng–Tongji cohort study of retired workers. Int. J. Epidemiol. 2013, 42, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Wheaton, A.G.; Ford, E.S.; Thompson, W.W.; Greenlund, K.J.; Presley-Cantrell, L.R.; Croft, J.B. Pulmonary function, chronic respiratory symptoms, and health-related quality of life among adults in the United States—National Health and Nutrition Examination Survey 2007–2010. BMC Public Health 2013, 13, 854. [Google Scholar] [CrossRef] [PubMed]
- Christopher, D.J.; Seema, A.S.; Ezhilarasu, P.; Bechtel, J.J.; Augustine, J. Correlation of health-related quality of life with other disease severity indices in Indian chronic obstructive pulmonary disease patients. Int. J. Chronic Obstr. Pulm. Dis. 2012, 7, 291–296. [Google Scholar] [CrossRef]
- Ferrer, M.; Villasante, C.; Alonso, J.; Sobradillo, V.; Gabriel, R.; Vilagut, G.; Masa, J.F.; Viejo, J.L.; Jimenez-Ruiz, C.A.; Miravitlles, M. Interpretation of quality of life scores from the St George’s Respiratory Questionnaire. Eur. Respir. J. 2002, 19, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Abbott, J.; Morton, A.M.; Hurley, M.A.; Conway, S.P. Longitudinal impact of demographic and clinical variables on health-related quality of life in cystic fibrosis. BMJ Open 2015, 5, e007418. [Google Scholar] [CrossRef]
- Engstrom, C.P.; Persson, L.O.; Larsson, S.; Sullivan, M. Health-related quality of life in COPD: Why both disease-specific and generic measures should be used. Eur. Respir. J. 2001, 18, 69–76. [Google Scholar] [CrossRef]
- Luzak, A.; Karrasch, S.; Wacker, M.; Thorand, B.; Nowak, D.; Peters, A.; Schulz, H. Association of generic health-related quality of life (EQ-5D dimensions) and inactivity with lung function in lung-healthy German adults: Results from the KORA studies F4L and Age. Qual. Life Res. 2018, 27, 735–745. [Google Scholar] [CrossRef] [PubMed]
- Corlateanu, A.; Botnaru, V.; Covantev, S.; Dumitru, S.; Siafakas, N. Predicting health-related quality of life in patients with chronic obstructive pulmonary disease: The impact of age. Respiration 2016, 92, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Pickard, A.S.; Yang, Y.; Lee, T.A. Comparison of health-related quality of life measures in chronic obstructive pulmonary disease. Health Qual. Life Outcomes 2011, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Mekov, E.V.; Slavova, Y.G.; Genova, M.P.; Tsakova, A.D.; Kostadinov, D.T.; Minchev, D.D.; Marinova, D.M.; Boyanov, M.A. Diabetes mellitus type 2 in hospitalized COPD Patients: Impact on quality of life and lung function. Folia Med. 2016, 58, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Tay, T.R.; Radhakrishna, N.; Hore-Lacy, F.; Smith, C.; Hoy, R.; Dabscheck, E.; Hew, M. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology 2016, 21, 1384–1390. [Google Scholar] [CrossRef] [PubMed]
- Margaritopoulos, G.A.; Antoniou, K.M.; Wells, A.U. Comorbidities in interstitial lung diseases. Eur. Respir. Rev. 2017, 26, 160027. [Google Scholar] [CrossRef]
- Shoup, R.; Dalsky, G.; Warner, S.; Davies, M.; Connors, M.; Khan, M.; Khan, F.; ZuWallack, R. Body composition and health-related quality of life in patients with obstructive airways disease. Eur. Respir. J. 1997, 10, 1576–1580. [Google Scholar] [CrossRef]
- O’Donnell, D.E.; Laveneziana, P. Dyspnea and activity limitation in COPD: Mechanical factors. COPD J. Chronic Obstr. Pulm. Dis. 2009, 4, 225–236. [Google Scholar] [CrossRef]
- Kwon, H.; Kim, E. Factors contributing to quality of life in COPD patients in South Korea. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 103. [Google Scholar] [CrossRef]
| Total | Lung Function | p Value | ||
|---|---|---|---|---|
| Normal Lung Function † | Poor Lung Function ‡ | |||
| N | 8398 | 5197 | 3201 | |
| Sex (Male, N, %) | 3561 (42.40) | 1903 (36.62) | 1658 (51.80) | <0.0001 * |
| Age (y, mean ± SD) | 63.51 ± 8.06 | 62.11 ± 7.74 | 65.79 ± 8.07 | <0.0001 * |
| BMI (kg/m2, mean ± SD) | 24.08 ± 3.22 | 24.13 ± 3.10 | 24.00 ± 3.41 | 0.0591 |
| Marriage (N, %) | 7459 (88.82) | 4676 (89.97) | 2783 (86.94) | <0.0001 * |
| Education | <0.0001 * | |||
| <9y (N, %) | 4820 (57.39) | 2793 (53.740) | 2027 (63.32) | |
| 9–12y (N, %) | 2532 (30.15) | 1693 (32.58) | 839 (26.21) | |
| >12y (N, %) | 1046 (12.46) | 711 (13.68) | 335 (10.47) | |
| Smoking | <0.0001 * | |||
| No smoking (N, %) | 6176 (73.54) | 4070 (78.31) | 2106 (65.79) | |
| Current smoking (N, %) | 1331 (15.85) | 677 (13.03) | 654 (20.43) | |
| Quit smoking (N, %) | 891 (10.61) | 450 (8.66) | 441 (13.78) | |
| Passive smoking (N, %) | 2495 (29.71) | 1629 (31.35) | 866 (27.05) | <0.0001 * |
| Drinking | <0.0001 * | |||
| No drinking (N, %) | 5846 (69.61) | 3705 (71.29) | 2141 (66.89) | |
| Current drinking (N, %) | 2178 (25.93) | 1312 (25.25) | 866 (27.05) | |
| Quit drinking (N, %) | 374 (4.45) | 180 (3.46) | 194 (6.06) | |
| Exercise (N, %) | 7606 (90.57) | 4718 (90.78) | 2888 (90.22) | 0.3926 |
| Hypertension (N, %) | 2771 (33.00) | 1576 (30.33) | 1195 (37.33) | <0.0001 * |
| Hyperlipemia (N, %) | 1549 (18.44) | 961 (18.49) | 588 (18.37) | 0.8885 |
| Diabetes (N, %) | 943 (11.23) | 530 (10.20) | 413 (12.90) | 0.0001 * |
| Total | Lung Function | p Value | ||
|---|---|---|---|---|
| Normal Lung Function † | Poor Lung Function ‡ | |||
| N | 8398 | 5197 | 3201 | |
| FVC (L) | 2.44 ± 0.70 | 2.75 ± 0.58 | 1.93 ± 0.56 | <0.0001 * |
| FEV1 (L) | 2.10 ± 0.60 | 2.37 ± 0.49 | 1.66 ± 0.48 | <0.0001 * |
| FEV1/FVC (%) | 86.45 ± 10.79 | 86.64 ± 7.95 | 86.13 ± 14.23 | <0.0001 * |
| MMF (L/s) | 2.64 ± 1.01 | 2.87 ± 0.85 | 2.27 ± 1.13 | <0.0001 * |
| PEF (L/s) | 4.38 ± 1.90 | 4.81 ± 1.85 | 3.69 ± 1.78 | <0.0001 * |
| FEF25 (L/s) | 3.44 ± 1.98 | 3.68 ± 2.04 | 3.04 ± 1.82 | <0.0001 * |
| FEF50 (L/s) | 2.97 ± 1.25 | 3.28 ± 1.09 | 2.47 ± 1.33 | <0.0001 * |
| FEF75 (L/s) | 2.02 ± 1.49 | 2.30 ± 1.62 | 1.57 ± 1.11 | <0.0001 * |
| Total scores | 75.40 ± 10.51 | 75.88 ± 10.44 | 74.63 ± 10.57 | <0.0001 * |
| Physical health domain score | 75.37 ± 17.05 | 76.35 ± 16.68 | 73.78 ± 17.52 | <0.0001 * |
| Psychological state domain score | 73.58 ± 13.07 | 73.89 ± 13.15 | 73.08 ± 12.92 | <0.0001 * |
| Social relationships domain score | 74.50 ± 12.75 | 74.95 ± 12.70 | 73.77 ± 12.79 | <0.0001 * |
| Environment domain score | 78.15 ± 12.27 | 78.32 ± 12.35 | 77.88 ± 12.14 | 0.8377 |
| Estimated Changes (95% CI) by Continuous FVC | Estimated Changes (95% CI) by Tertile of FVC | ||||||
|---|---|---|---|---|---|---|---|
| β | p Value | T1 (<2.12 L) | T2 (2.12–2.69 L) | T3 (≥2.69 L) | p Trend | ||
| N | 2767 | 2807 | 2824 | ||||
| Median (L) | 1.78 | 2.39 | 3.08 | ||||
| Total score | Univariate model | 1.36 (1.04,1.69) | <0.0001 * | 0 (reference) | 1.43 (0.88,1.98) * | 2.12 (1.57,2.67) * | <0.0001 * |
| Model 1 † | 0.83 (0.46,1.20) | <0.0001 * | 0 (reference) | 0.73 (0.17,1.30) * | 1.18 (0.56,1.80) * | 0.0002 * | |
| Model 2 ‡ | 0.84 (0.47,1.21) | <0.0001 * | 0 (reference) | 0.75 (0.19,1.32) * | 1.20 (0.58,1.82) * | 0.0002 * | |
| Model 3 § | 0.63 (0.26,1.00) | 0.0010 * | 0 (reference) | 0.61 (0.04,1.17) * | 0.89 (0.27,1.51) * | 0.0056 * | |
| Physical health domain score | Univariate model | 2.90 (2.38,3.42) | <0.0001 * | 0 (reference) | 2.33 (1.44,3.22) * | 4.27 (3.38,5.16) * | <0.0001 * |
| Model 1 † | 1.85 (1.25,2.45) | <0.0001 * | 0 (reference) | 0.98 (0.07,1.89) * | 2.36 (1.36,3.36) * | <0.0001 * | |
| Model 2 ‡ | 1.88 (1.29,2.48) | <0.0001 * | 0 (reference) | 1.03 (0.11,1.94) * | 2.41 (1.41,3.41) * | <0.0001 * | |
| Model 3 § | 1.67 (1.07,2.28) | <0.0001 * | 0 (reference) | 0.89 (−0.02,1.80) | 2.08 (1.07,3.08) * | <0.0001 * | |
| Psychological state domain score | Univariate model | 1.27 (0.87,1.67) | <0.0001 * | 0 (reference) | 1.58 (0.90,2.27) * | 2.12 (1.44,2.81) * | <0.0001 * |
| Model 1 † | 0.50 (0.04,0.96) | 0.0343 * | 0 (reference) | 0.82 (0.11,1.52) * | 0.88 (0.10,1.65) * | 0.0294 * | |
| Model 2 ‡ | 0.51 (0.05,0.97) | 0.0309 * | 0 (reference) | 0.83 (0.13,1.54) * | 0.89 (0.12,1.67) * | 0.0266 * | |
| Model 3 § | 0.25 (−0.21,0.72) | 0.2850 | 0 (reference) | 0.64 (−0.06,1.35) | 0.54 (−0.24,1.32) | 0.1864 | |
| Social relationships domain score | Univariate model | 0.80 (0.41,1.19) | <0.0001 * | 0 (reference) | 1.09 (0.42,1.76) * | 1.24 (0.58,1.91) * | 0.0003 * |
| Model 1 † | 0.71 (0.26,1.16) | 0.0021 * | 0 (reference) | 0.77 (0.08,1.46) * | 1.05 (0.29,1.80) * | 0.0074 * | |
| Model 2 ‡ | 0.72 (0.27,1.17) | 0.0018 * | 0 (reference) | 0.78 (0.09,1.47) * | 1.06 (0.30,1.82) * | 0.0066 * | |
| Model 3 § | 0.49 (0.03,0.95) | 0.0356 * | 0 (reference) | 0.62 (−0.08,1.31) | 0.72 (−0.04,1.49) | 0.0670 | |
| Environment domain score | Univariate model | 0.49 (0.12,0.87) | 0.0103 * | 0 (reference) | 0.73 (0.08,1.37) * | 0.84 (0.19,1.48) * | 0.0214 * |
| Model 1 † | 0.25 (−0.19,0.69) | 0.2601 | 0 (reference) | 0.37 (−0.29,1.04) | 0.44 (−0.29,1.17) | 0.2444 | |
| Model 2 ‡ | 0.26 (−0.18,0.69) | 0.2469 | 0 (reference) | 0.38 (−0.28,1.05) | 0.45 (−0.28,1.18) | 0.2324 | |
| Model 3 § | 0.09 (−0.35,0.54) | 0.6739 | 0 (reference) | 0.27 (−0.40,0.94) | 0.22 (−0.52,0.95) | 0.5796 | |
| Estimated Changes (95% CI) by Continuous FEV1 | Estimated Changes (95% CI) by Tertile of FEV1 | p Trend | |||||
|---|---|---|---|---|---|---|---|
| β | p Value | T1 (<1.86 L) | T2 (1.86–2.33 L) | T3 (≥2.33 L) | |||
| N | 2797 | 2769 | 2832 | ||||
| Median (L) | 1.55 | 2.09 | 2.64 | ||||
| Total score | Univariate model | 1.54 (1.17,1.92) | <0.0001 * | 0 (reference) | 1.53 (0.98,2.08) * | 2.09 (1.54,2.64) * | <0.0001 * |
| Model 1 † | 0.73 (0.29,1.16) | 0.0011 * | 0 (reference) | 0.76 (0.19,1.33) * | 0.93 (0.31,1.56) * | 0.0031 * | |
| Model 2 ‡ | 0.76 (0.33,1.20) | 0.0006 * | 0 (reference) | 0.78 (0.22,1.35) * | 0.97 (0.35,1.60) * | 0.0021 * | |
| Model 3 § | 0.53 (0.09,0.97) | 0.0175 * | 0 (reference) | 0.61 (0.04,1.17) * | 0.69 (0.07,1.32) * | 0.0287 * | |
| Physical health domain score | Univariate model | 3.21 (2.60,3.82) | <0.0001 * | 0 (reference) | 3.01 (2.12,3.90) * | 3.88 (2.99,4.77) * | <0.0001 * |
| Model 1 † | 1.62 (0.92,2.33) | <0.0001 * | 0 (reference) | 1.51 (0.59,2.42) * | 1.47 (0.46,2.47) * | 0.0040 * | |
| Model 2 ‡ | 1.71 (1.00,2.41) | <0.0001 * | 0 (reference) | 1.56 (0.65,2.47) * | 1.55 (0.55,2.56) * | 0.0022 * | |
| Model 3 § | 1.46 (0.75,2.17) | <0.0001 * | 0 (reference) | 1.38 (0.47,2.30) * | 1.25 (0.24,2.27) * | 0.0142 * | |
| Psychological state domain score | Univariate model | 1.50 (1.03,1.97) | <0.0001 * | 0 (reference) | 1.43 (0.74,2.11) * | 2.19 (1.51,2.87) * | <0.0001 * |
| Model 1 † | 0.47 (−0.07,1.02) | 0.0890 | 0 (reference) | 0.64 (−0.06,1.35) | 0.80 (0.02,1.58) * | 0.0421 * | |
| Model 2 ‡ | 0.50 (−0.05,1.04) | 0.0732 | 0 (reference) | 0.66 (−0.05,1.37) | 0.83 (0.05,1.61) * | 0.0357 * | |
| Model 3 § | 0.22 (−0.33,0.77) | 0.4258 | 0 (reference) | 0.45 (−0.25,1.16) | 0.51 (−0.27,1.16) | 0.1979 | |
| Social relationships domain score | Univariate model | 0.92 (0.46,1.38) | <0.0001 * | 0 (reference) | 1.03 (0.36,1.69) * | 1.31 (0.65,1.98) * | 0.0001 * |
| Model 1 † | 0.68 (0.14,1.21) | 0.0130 * | 0 (reference) | 0.62 (−0.07,1.31) | 0.98 (0.22,1.74) * | 0.0116 * | |
| Model 2 ‡ | 0.70 (0.17,1.23) | 0.0100 * | 0 (reference) | 0.64 (−0.06,1.33) | 1.00 (0.24,1.76) * | 0.0096 ** | |
| Model 3 § | 0.46 (−0.07,1.00) | 0.0914 | 0 (reference) | 0.45 (−0.25,1.14) | 0.71 (−0.06,1.47) | 0.0692 | |
| Environment domain score | Univariate model | 0.54 (0.10,0.98) | 0.0169 * | 0 (reference) | 0.66 (0.02,1.31) * | 0.97 (0.33,1.61) * | 0.0031 * |
| Model 1 † | 0.13 (−0.38,0.64) | 0.6221 | 0 (reference) | 0.27 (−0.40,0.93) | 0.49 (−0.25,1.22) | 0.1925 | |
| Model 2 ‡ | 0.15 (−0.37,0.66) | 0.5742 | 0 (reference) | 0.28 (−0.39,0.94) | 0.51 (−0.23,1.24) | 0.1755 | |
| Model 3 § | −0.02 (−0.54,0.50) | 0.9439 | 0 (reference) | 0.15 (−0.52,0.82) | 0.30 (−0.44,1.04) | 0.4218 | |
| Estimated Changes (95% CI) by Continuous FVC ‡ | Estimated Changes (95% CI) by Continuous FEV1 ‡ | ||||
|---|---|---|---|---|---|
| β | p Value | β | p Value | ||
| No comorbidities † (n = 3871) | Total score | 1.31 (0.76,1.85) | <0.0001 * | 1.06 (0.42,1.69) | 0.0011 * |
| Physical health domain score | 1.76 (0.94,2.59) | <0.0001 * | 1.64 (0.67,2.60) | 0.0009 * | |
| Psychological state domain score | 1.10 (0.42,1.78) | 0.0015 * | 0.76 (−0.04,1.56) | 0.0626 | |
| Social relationships domain score | 1.40 (0.73,2.06) | <0.0001 * | 1.21 (0.43,2.00) | 0.0024 * | |
| Environment domain score | 0.96 (0.32,1.60) | 0.0031 * | 0.61 (−0.13,1.36) | 0.1077 | |
| Comorbidities † (n = 4527) | Total score | −0.04 (−0.55,0.47) | 0.8781 | −0.04 (−0.64,0.57) | 0.9055 |
| Physical health domain score | 1.32 (0.48,2.16) | 0.0022 * | 0.97 (−0.02,1.97) | 0.0557 | |
| Psychological state domain score | −0.49 (−1.14,0.15) | 0.1303 | −0.27 (−1.03,0.49) | 0.4821 | |
| Social relationships domain score | −0.31 (−0.94,0.32) | 0.3346 | −0.22 (−0.97,0.52) | 0.5579 | |
| Environment domain score | −0.68 (−1.29,−0.06) | 0.0302 * | −0.63 (−1.35,0.10) | 0.0889 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wen, Y.; Wang, D.; Zhou, M.; Zhou, Y.; Guo, Y.; Chen, W. Potential Effects of Lung Function Reduction on Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2019, 16, 260. https://doi.org/10.3390/ijerph16020260
Wen Y, Wang D, Zhou M, Zhou Y, Guo Y, Chen W. Potential Effects of Lung Function Reduction on Health-Related Quality of Life. International Journal of Environmental Research and Public Health. 2019; 16(2):260. https://doi.org/10.3390/ijerph16020260
Chicago/Turabian StyleWen, Yuhan, Dongming Wang, Min Zhou, Yun Zhou, Yanjun Guo, and Weihong Chen. 2019. "Potential Effects of Lung Function Reduction on Health-Related Quality of Life" International Journal of Environmental Research and Public Health 16, no. 2: 260. https://doi.org/10.3390/ijerph16020260
APA StyleWen, Y., Wang, D., Zhou, M., Zhou, Y., Guo, Y., & Chen, W. (2019). Potential Effects of Lung Function Reduction on Health-Related Quality of Life. International Journal of Environmental Research and Public Health, 16(2), 260. https://doi.org/10.3390/ijerph16020260





