Adolescents’ and Parents’ Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Protocol
2.3. Evaluation of the rPSMF
2.4. Analysis
3. Results
3.1. Adherence and Anthropometric Outcomes
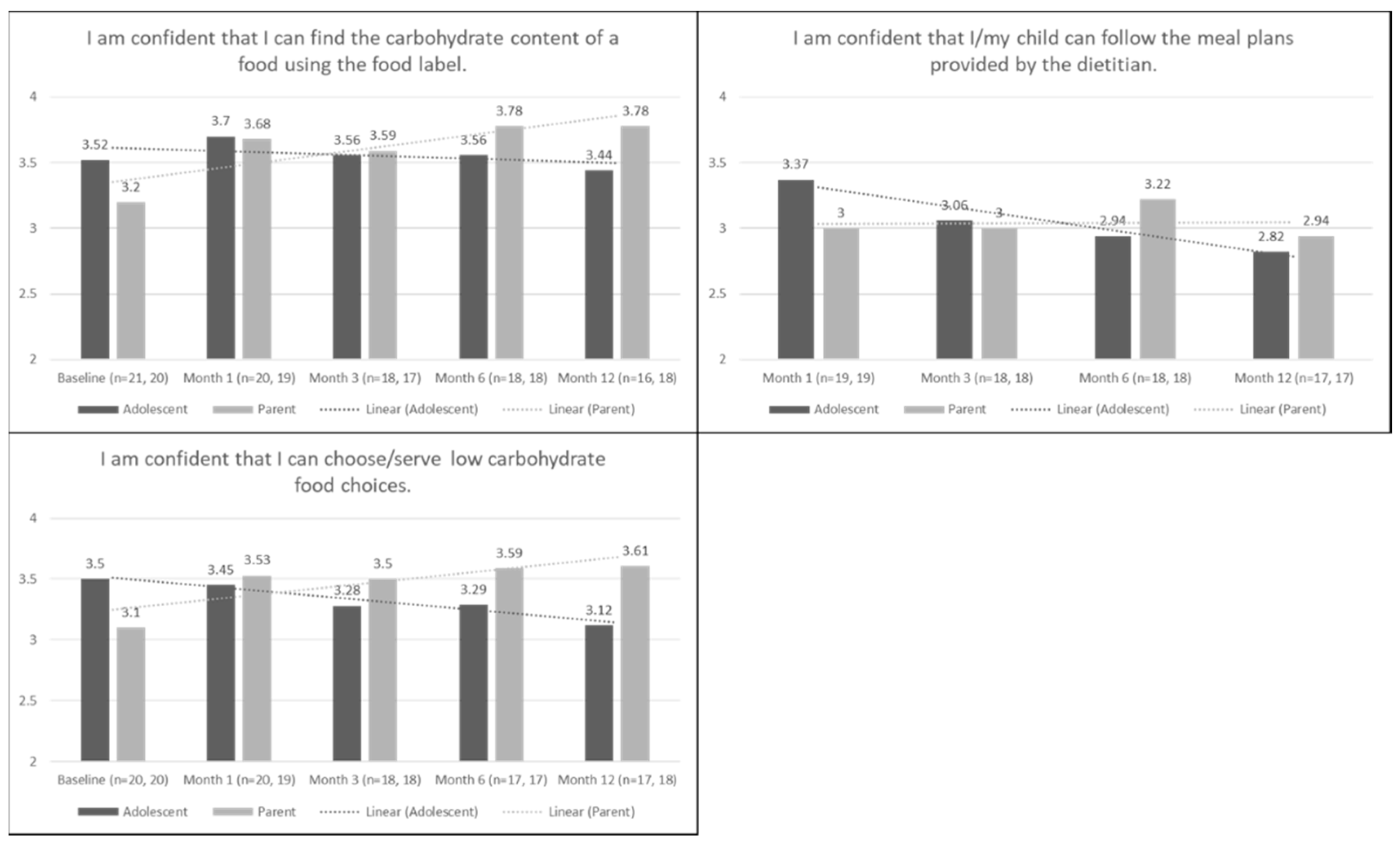
3.2. Confidence
3.3. Confidence Based on Adherence and Response (Weight Loss) to the rPSMF
- (a)
- One month: There were no significant differences in confidence ratings based on adolescent adherence to the rPSMF at one month, though there was a significant difference in confidence rating based on response to the rPSMF at one month. Adolescents who lost weight on the rPSMF from baseline to 1 month (n = 17, Mean (M) = 3.47, Standard Deviation (SD) = 0.51) reported higher confidence in following the meal plans provided by the dietitian as compared to adolescents who did not lose weight (n = 2, M = 2.50, SD = 0.71; t(17) = 2.46, p = 0.025).
- (b)
- Three months: There were no significant differences in adolescent reports or parent reports on the confidence questions based on whether the adolescent was adherent with the rPSMF approach at 3 months, and there was not a large enough sample (weight loss n = 15, weight gain/stayed the same n = 1) at three months to conduct analyses based on response to the diet.
- (c)
- Six months: Adolescents who were adherent (n = 3, M = 4.00, SD = 0.00) had greater confidence in reading food labels than adolescents who were not adherent (n = 12, M = 3.58, SD = 0.67; t(11) = −2.16, p = 0.054). There were no significant differences for adolescent and parent responses on the confidence questions based on whether adolescents lost weight or gained weight/stayed the same.
- (d)
- Twelve months: Parents of adolescents who were adherent (n = 2, M = 4.00, SD = 0.00) had greater confidence in reading food labels than parents of adolescents who were not adherent (n = 9, M = 3.56, SD = 0.53, t(8) = −2.53, p = 0.035). Parents of adolescents who were adherent (n = 2, M = 4.00, SD = 0.00) also reported greater confidence in serving low carbohydrate food choices than parents of adolescents who were not adherent (n = 9, M = 3.56, SD = 0.53; t(8) = −2.53, p = 0.035). Parents of adolescents who were adherent (n = 2, M = 4.00, SD = 0.00) reported greater confidence that their child could follow the meal plans provided by the dietitian compared to parents of adolescents who were not adherent (n = 8, M = 2.88, SD = 0.35; t(8) = −4.30, p = 0.003). There were no significant differences for adolescent and parents’ reports of confidence based on adolescents who lost weight or gained weight/stayed the same.
3.4. Satisfaction
- (a)
- Adolescent and Parent Changes over Time: There was a significant difference in response from 1 month to 12 months for adolescents (n = 16) and parents (n = 17) to the question “How much do you feel that the low-carbohydrate, high-protein diet has helped you/your child lose weight?” Adolescents at 1 month (M = 84.75, SD = 15.18) felt that the rPSMF approach helped them to lose weight more than they reported at 12 months (M = 65.44, SD = 21.26; t(15) = 2.90, p = 0.011). Parents also had higher reports at 1 month (M = 86.06, SD = 22.30) than 12 months (M = 63.24, SD = 29.56; t(16) = 3.64, p = 0.002).
- (b)
- Adolescent-Parent Comparisons over Time: See Table 4 for comparisons between adolescents’ and parents’ mean scores on the satisfaction questions at each time point. Overall, on the question, “How much do you feel that the low-carbohydrate, high-protein diet has helped you/your child lose weight?”, parents had higher satisfaction with weight loss at each follow-up time point than adolescents. However, the difference between adolescents and parents scores became smaller over time, meaning they became more congruent in their perceptions; 1 month mean difference = 9.00 (SD = 21.11) vs. 12 months mean difference = −1.29 (SD = 25.73). There was a significant difference at 3 months between adolescents (M = 73.00, SD = 21.98) and parents (M = 82.53, SD = 25.53), where parents significantly endorsed that the rPSMF approach helped their child lose weight (t(16) = −2.61, p = 0.016) compared to adolescents.
3.5. Satisfaction Based on Adherence and Response to the rPSMF
- (a)
- Three months: Adolescents who were adherent (n = 8, M = 86.50, SD = 10.89) endorsed that the rPSMF helped them lose weight more than adolescents who were not adherent (n = 8, M = 59.63, SD = 23.94; t(14) = −2.89, p = 0.012). Adolescents who were adherent (n = 8, M = 68.50, SD = 15.13) were also more satisfied with their weight changes than adolescents who were not adherent (n = 7, M = 46.86, SD = 18.18; t(13) = −2.52, p = 0.026). Parents of adolescents who were adherent (n = 8, M = 94.50, SD = 5.63) also endorsed that the rPSMF helped their child lose weight more than parents of adolescents who were not adherent (n = 8, M = 68.50, SD = 32.10; t(7.43) = −2.26, p = 0.057).
- (b)
- Six months: Adolescents who were adherent (n = 3, M = 94.67, SD = 3.51) endorsed that the rPSMF helped them lose weight more than adolescents who were not adherent (n = 12, M = 64.25, SD = 29.35; t(12.08) = −3.49, p = 0.004). Parents of adolescents who lost weight (n = 13, M = 72.38, SD = 21.68) reported more satisfaction with weight changes compared to parents of adolescents who gained weight/stayed the same weight (n = 2, M = 31.50, SD = 9.19; t(13) = 2.56, p = 0.024).
- (c)
- Twelve months: Adolescents who were not adherent (n = 9, M = 70.44, SD = 19.37) believed that the rPSMF was more difficult to follow than adolescents who were adherent (n = 2, M = 31.00, SD = 25.46; t(9) = 2.51, p = 0.034). Similarly, parents of adolescents who were not adherent (n = 8, M = 73.25, SD = 17.50) believed that the rPSMF was more difficult to follow than parents of adolescents who were adherent (n = 2, M = 25.00, SD = 35.36; t(8) = 2.96, p = 0.018). Adolescents who lost weight (n = 7, M = 58.86, SD = 27.38) reported more satisfaction with weight changes compared to adolescents who gained weight/stayed the same weight (n = 4, M = 21.50, SD = 16.09; t(9) = 2.46, p = 0.036). Parents of adolescents who lost weight (n = 7, M = 82.14, SD = 21.05) endorsed that the rPSMF helped their child lose weight more than parents of adolescents who gained weight/stayed the same weight (n = 4, M = 32.50, SD = 16.62; t(9) = 4.02, p = 0.003).
3.6. Open-Ended Questions
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.E.; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120 (Suppl. 4), S164–S192. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, E.A.; Evans, C.V.; Burda, B.U.; Walsh, E.S.; Eder, M.; Lozano, P. Screening for Obesity and Interventions for Weight Management in Children and Adolescents: A Systematic Evidence Review for the U.S. Preventive Services Task Force; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2017.
- Hipsky, J.; Kirk, S. HealthWorks! Weight management program for children and adolescents. J. Am. Diet. Assoc. 2002, 102 (Suppl. 3), S64–S67. [Google Scholar] [CrossRef]
- Savoye, M.; Shaw, M.; Dziura, J.; Tamborlane, W.V.; Rose, P.; Guandalini, C.; Goldberg-Gell, R.; Burgert, T.; Cali, A.M.G.; Weiss, R.; et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA 2007, 297, 2697–2704. [Google Scholar] [CrossRef] [PubMed]
- Sothern, M.S.; Schumacher, H.; von Almen, T.K.; Carlisle, L.K.; Udall, J.N. Committed to kids: An integrated, 4-level team approach to weight management in adolescents. J. Am. Diet. Assoc. 2002, 102 (Suppl. 3), S81–S85. [Google Scholar] [CrossRef]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe obesity in children and adolescents: Identification, associated health risks, and treatment approaches: A scientific statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.A.; Tyler, C.; Palcic, J.L.; Stansberry, S.A.; Gallagher, M.R.; Foreyt, J.P. Smaller weight changes in standardized body mass index in response to treatment as weight classification increases. J. Pediatr. 2011, 158, 624–627. [Google Scholar] [CrossRef]
- Schilling, P.L.; Davis, M.M.; Albanese, C.T.; Dutta, S.; Morton, J. National trends in adolescent bariatric surgical procedures and implications for surgical centers of excellence. J. Am. Coll. Surg. 2008, 206, 1–12. [Google Scholar] [CrossRef]
- Black, J.A.; White, B.; Viner, R.M.; Simmons, R.K. Bariatric surgery for obese children and adolescents: A systematic review and meta-analysis. Obes. Rev. 2013, 14, 634–644. [Google Scholar] [CrossRef]
- Stallings, V.A.; Archibald, E.H.; Pencharz, P.B.; Harrison, J.E.; Bell, L.E. One-year follow-up of weight, total body potassium, and total body nitrogen in obese adolescents treated with the protein-sparing modified fast. Am. J. Clin. Nutr. 1988, 48, 91–94. [Google Scholar] [CrossRef]
- Suskind, R.M.; Blecker, U.; Udall, J.N., Jr.; Von Almen, T.K.; Schumacher, H.D.; Carlisle, L.; Sothern, M.S. Recent advances in the treatment of childhood obesity. Pediatr. Diabetes 2000, 1, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Bakhach, M.; Shah, V.; Harwood, T.; Lappe, S.; Bhesania, N.; Mansoor, S.; Alkhouri, N. The Protein-Sparing Modified Fast Diet.: An. Effective and Safe. Approach to Induce Rapid Weight Loss in Severely Obese Adolescents. Glob. Pediatr. Health 2016, 3, 2333794X15623245. [Google Scholar] [CrossRef] [PubMed]
- Merritt, R.J.; Bistrian, B.R.; Blackburn, G.L.; Suskind, R.M. Consequences of modified fasting in obese pediatric and adolescent patients. I. Protein-sparing modified fast. J. Pediatr. 1980, 96, 13–19. [Google Scholar] [CrossRef]
- Koeck, E.; Davenport, K.; Barefoot, L.C.; Qureshi, F.G.; Davidow, D.; Nadler, E.P. Inpatient weight loss as a precursor to bariatric surgery for adolescents with extreme obesity: Optimizing bariatric surgery. Clin. Pediatr. Phila 2013, 52, 608–611. [Google Scholar] [CrossRef] [PubMed]
- Figueroa-Colon, R.; Franklin, F.A.; Lee, J.Y.; Von Almen, T.K.; Suskind, R.M. Feasibility of a clinic-based hypocaloric dietary intervention implemented in a school setting for obese children. Obes. Res. 1996, 4, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Escobar, O.; Mizuma, H.; Sothern, M.S.; Blecker, U.; Udall, J.N., Jr.; Suskind, R.M.; Hilton, C.; Vargas, A. Hepatic insulin clearance increases after weight loss in obese children and adolescents. Am. J. Med. Sci. 1999, 317, 282–286. [Google Scholar] [CrossRef]
- Bravata, D.M.; Sanders, L.; Huang, J.; Krumholz, H.M.; Olkin, I.; Gardner, C.D.; Bravata, D.M. Efficacy and safety of low-carbohydrate diets: A systematic review. JAMA 2003, 289, 1837–1850. [Google Scholar] [CrossRef]
- Krebs, N.F.; Gao, D.; Gralla, J.; Collins, J.S.; Johnson, S.L. Efficacy and safety of a high protein, low carbohydrate diet for weight loss in severely obese adolescents. J. Pediatr. 2010, 157, 252–258. [Google Scholar] [CrossRef]
- Chang, J.; Kashyap, S.R. The protein-sparing modified fast for obese patients with type 2 diabetes: What to expect. Clevel. Clin. J. Med. 2014, 81, 557–565. [Google Scholar] [CrossRef]
- Sumithran, P.; Prendergast, L.A.; Delbridge, E.; Purcell, K.; Shulkes, A.; Kriketos, A.; Proietto, J. Ketosis and appetite-mediating nutrients and hormones after weight loss. Eur. J. Clin. Nutr. 2013, 67, 759–764. [Google Scholar] [CrossRef]
- Cummings, D.E.; Weigle, D.S.; Frayo, R.S.; Breen, P.A.; Ma, M.K.; Dellinger, E.P.; Purnell, J.Q. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 2002, 346, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Geldszus, R.; Mayr, B.; Horn, R.; Geisthövel, F.; Von Zur Mühlen, A.; Brabant, G. Serum leptin and weight reduction in female obesity. Eur. J. Endocrinol. 1996, 135, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Eneli, I.U.; Watowicz, R.P.; Xu, J.; Tindall, A.; Walston, M.; Tanner, K.; Pratt, K. Rationale and design of a pilot study to evaluate the acceptability and effectiveness of a revised protein sparing modified fast (rPSMF) for severe obesity in a pediatric tertiary care weight management clinic. Contemp. Clin. Trials Commun. 2019, 15, 100388. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.G.; Carter, R.E.; Nietert, P.J.; Stewart, P.W. Recommendations for planning pilot studies in clinical and translational research. Clin. Transl. Sci. 2011, 4, 332–334. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R.; Mei, Z.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC growth charts: United States. Adv. Data 2000, 314, 1–27. [Google Scholar]
- Dinsdale, H.; Ridler, C.; Ells, L. A Simple Guide to Classifying Body Mass Index in Children; University of Oxford, National Obesity Observatory: Oxford, UK, 2011. [Google Scholar]
- Eneli, I.; Tindall, A.; Watowicz, R.; Worthington, J.; Tanner, K.; Pratt, K.J.; Walston, M. Using a Revised Protein Sparing Modified Fast (rPSMF) for Children and Adolescents with Severe Obesity: A Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 3061. [Google Scholar] [CrossRef] [PubMed]
- Skelton, J.A.; Irby, M.B.; Geiger, A.M. A systematic review of satisfaction and pediatric obesity treatment: New avenues for addressing attrition. J. Healthc. Qual. 2014, 36, 5–22. [Google Scholar] [CrossRef]
- Skelton, J.A.; Martin, S.; Irby, M.B. Satisfaction and attrition in paediatric weight management. Clin. Obes. 2016, 6, 143–153. [Google Scholar] [CrossRef]
- Pratt, K.J.; Lazorick, S.; Lamson, A.L.; Ivanescu, A.; Collier, D.N. Quality of life and BMI changes in youth participating in an integrated pediatric obesity treatment program. Health Qual. Life Outcomes 2013, 11, 116. [Google Scholar] [CrossRef]
- Pratt, K.J.; Lamson, A.L.; Swanson, M.S.; Lazorick, S.; Collier, D.N. The importance of assessing for depression with HRQOL in treatment seeking obese youth and their caregivers. Qual. Life Res. 2012, 21, 1367–1377. [Google Scholar] [CrossRef]
- Unick, J.L.; Neiberg, R.H.; Hogan, P.E.; Cheskin, L.J.; Dutton, G.R.; Jeffery, R.; Nelson, J.A.; Pi-Sunyer, X.; West, D.S.; Wing, R.R.; et al. Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity 2015, 23, 1353–1356. [Google Scholar] [CrossRef] [PubMed]
- Theim, K.R.; Sinton, M.M.; Goldschmidt, A.B.; Van Buren, D.J.; Doyle, A.C.; Saelens, B.E.; Stein, R.I.; Epstein, L.H.; Wilfley, D.E. Adherence to behavioral targets and treatment attendance during a pediatric weight control trial. Obesity 2013, 21, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Sitzia, J.; Wood, N. Patient satisfaction: A review of issues and concepts. Soc. Sci. Med. 1997, 45, 1829–1843. [Google Scholar] [CrossRef]
- Martin, K.A.; Bowen, D.J.; Dunbar-Jacob, J.; Perri, M.G. Who will adhere? Key issues in the study and prediction of adherence in randomized controlled trials. Control Clin. Trials 2000, 21 (Suppl. 5), 195S–199S. [Google Scholar] [CrossRef]
| 11–13 Age Group | 14+ Age Group | |
|---|---|---|
| Comorbidity | Must have severe co-morbidity: Obstructive Sleep Apnea, Diabetes (type II), Fatty Liver, Slipped Capital Femoral Epiphysis (SCFE), Blount Disease, Pseudotumor Cerebri | Must have 1 severe co-morbidity OR 1 co-morbidity with sustained weight gain |
| Pubertal Maturity | Tanner Stage III, IV, V | Tanner Stage III, IV, V |
| BMI | Class II or III obesity | Class II or III obesity |
| Rapid Weight Gain | A weight increase of more than 5% compared with baseline during the treatment; Increase in BMI z-score of 0.5 SD or more at any point during the treatment to account for age- and sex-appropriate growth | A weight increase of more than 5% compared with baseline during the treatment; Increase in BMI z-score of 0.5 SD or more at any point during the treatment to account for age- and sex-appropriate growth |
| Question | Time Point | Who | Option Choices |
|---|---|---|---|
| Confidence Questions | |||
| I am confident that I can find the carbohydrate content of a food using the food label. | B * F/U * | Adolescent Parent | Strongly Agree, Agree, Disagree, Strongly Disagree |
| I am confident that I can choose/serve low carbohydrate food choices. | B F/U | Adolescent Parent | Strongly Agree, Agree, Disagree, Strongly Disagree |
| I am confident that I/my child can follow the meal plans provided by the dietitian. | F/U | Adolescent Parent | Strongly Agree, Agree, Disagree, Strongly Disagree |
| I am confident that I can buy a variety of lean protein food options for meals and snacks. | B F/U | Parent | Strongly Agree, Agree, Disagree, Strongly Disagree |
| Satisfaction Questions | |||
| How much do you feel that the low-carbohydrate, high-protein diet has helped you/your child lose weight? | F/U | Adolescent Parent | From 1 (low) to 100 (high) |
| How satisfied are you with your weight change so far? | F/U | Adolescent Parent | From 1 (low) to 100 (high) |
| How easy or difficult has this special diet been for you/your child to follow? | F/U | Adolescent Parent | From 1 (easy) to 100 (difficult) |
| Open-ended Questions | |||
| So far, what have you liked about the low-carbohydrate, high-protein diet? | F/U | Adolescent Parent | Open-ended |
| So far, what have you not liked about the low-carbohydrate, high-protein diet? | F/U | Adolescent Parent | Open-ended |
| Is there anything specific that has made it difficult for you to follow the diet? | F/U | Adolescent Parent | Open-ended |
| Since your child has been on this diet, have you changed the way you feed the rest of your family? | F/U | Parent | Open-ended |
| Adolescent (n = 21) n (%) or Mean (SD), Range | Parent (n = 20) n (%) or Mean (SD), Range | |
|---|---|---|
| Sex | ||
| Male | 5 (23.8%) | 0 |
| Female | 16 (76.2%) | 20 (100%) |
| Age | 16.3 (1.4), 13–18 | - |
| Race/Ethnicity | ||
| White/Caucasian | 11 (52.4%) | 11 (55%) |
| Black/African American | 9 (42.8%) | 7 (35%) |
| Other | 0 (0.0%) | 2 (10%) |
| Hispanic | 1 (4.8%) | 1 (5%) |
| Role to Adolescent | ||
| Mother | - | 19 (95%) |
| Grandmother | - | 1 (5%) |
| Baseline BMI | 42.0 (6.3), 33.3–59.8 | 34.2 (9.8), 18.2–59.2 |
| Baseline BMI z-score | 2.5 (.27), 2.1–3.3 | - |
| Weight Status | ||
| Healthy weight | 0 | 2 (10%) |
| Overweight | 0 | 7 (35%) |
| Obese | 21 (100%) | 11 (55%) * |
| Month 1 | Month 3 | Month 6 | Month 12 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Range | n | Mean (SD) | Range | n | Mean (SD) | Range | n | Mean (SD) | Range | |
| How much do you feel that the low-carbohydrate, high-protein diet has helped you/your child lose weight? | ||||||||||||
| Adolescent | 19 | 81.21 (19.68) | 26–100 | 18 | 73.00 (21.33) * | 5–98 | 18 | 70.72 (26.32) | 19–99 | 17 | 64.44 (20.97) | 12–100 |
| Parent | 19 | 87.16 (21.31) | 11–100 | 18 | 82.22 (24.80) | 5–100 | 18 | 76.83 (24.39) | 18–100 | 18 | 64.89 (29.52) | 13–100 |
| How satisfied are you with your weight change so far? | ||||||||||||
| Adolescent | 16 | 64.44 (26.72) | 9–100 | 17 | 58.88 (18.31) | 29–94 | 15 | 56.80 (24.46) * | 9–100 | 16 | 49.19 (25.83) * | 0–98 |
| Parent | 18 | 82.11 (21.27) | 17–100 | 18 | 71.61 (28.65) | 6–100 | 17 | 63.71 (25.16) | 25–100 | 18 | 60.72 (29.99) | 15–100 |
| How easy or difficult has this special diet been for you/your child to follow? | ||||||||||||
| Adolescent | 16 | 68.13 (17.84) | 19–92 | 17 | 56.18 (26.69) | 1–100 | 17 | 59.41 (26.70) | 2–95 | 17 | 62.00 (20.80) | 13–100 |
| Parent | 16 | 66.44 (18.57) | 31–100 | 18 | 61.72 (25.59) | 6–93 | 16 | 57.94 (28.24) | 0–92 | 17 | 69.35 (22.71) | 0–97 |
| n (%) | Theme | Quote | n (%) | Theme | Quote |
|---|---|---|---|---|---|
| Adolescent-Liked (n = 20) | Parent-Liked (n = 20) | ||||
| 11 (55.0) | Weight loss (teen) | “I like that I can see my weight loss.” | 12 (60.0) | Weight loss (teen) | “It has helped him lose weight in a structured setting.” |
| 8 (40.0) | Food taste | “The food and how good it tastes.” | 10 (50.0) | Easy to follow | “Easy and manageable.” |
| 6 (30.0) | Food variety | “It has a variety of good food options that the whole family likes.” | 7 (35.0) | Food variety | “I feel that there is a variety of foods for my child to eat.” |
| 6 (30.0) | Trying new foods | “I like the different things to try that are low carb.” | 6 (30.0) | Family involvement | “It’s making the whole family aware of what foods are good and bad for you.” |
| 6 (30.0) | Feel healthy | “It has helped me feel healthier, when I stick to it.” | 5 (25.0) | Meal planning/preparation | “East to prepare….” |
| 4 (20.0) | Easy to follow | “I don’t have to think a lot, I don’t have to count calories.” | 5 (25.0) | Nutrition education | “I like to be able to watch the nutrition content.” |
| 4 (20.0) | Protein | “Lots of meat.” | 5 (25.0) | Recipes | “Easy to find recipes that she enjoys.” |
| Adolescent-Disliked (n = 20) | Parent-Disliked (n = 20) | ||||
| 11 (55.0) | Not eating carbs | “How hard it is to not eat foods that I’m not allowed to eat.” | 8 (40.0) | Limiting carbs/finding low carb options | “Hard to find low carb options.” |
| 8 (40.0) | Hard to follow | “How hard it can be sometimes.” | 7 (35.0) | Nothing | |
| 7 (35.0) | Lack of food variety | “There is not a lot of big variety in foods you can eat.” | 5 (25.0) | Lack of food variety | “Constantly looking for more (food) items so she is not eating the same thing all the time.” |
| 6 (30.0) | Nothing | 5 (25.0) | Too restrictive | “My daughter found it to be to restrictive and decided to give it up.” | |
| 5 (25.0) | Time | “Challenging with a busy schedule.” | 5 (25.0) | Hard to follow | “Hard to stick to when we go through busy times.” |
| 3 (15.0) | Eating with peers | “I do not enjoy watching my peers eating carb-filled lunch and snacks.” | 5 (25.0) | Meal planning/preparation | “I need to learn how to make or get low carb meals to make ahead of time.” |
| Adolescent-Specifically made rPSMF difficult (n = 19) | Parent-Specifically made rPSMF difficult (n = 19) | ||||
| 9 (47.4) | Not eating carbs | “Not being able to eat certain foods while others in my family are.” | 9 (47.4) | Nothing | |
| 7 (36.8) | Eating with peers | “Friends eating whatever they want.” | 8 (42.1) | Food choices/variety | “The meal options are not customized to our exact preferences.” |
| 6 (31.6) | Nothing | 8 (42.1) | Time | “Time restraints.” | |
| 5 (26.3) | Food availability/variety | “Finding snack foods with low carbs.” | 5 (26.3) | Cost | “Money for groceries.” |
| 4 (21.1) | Time | “A busy scheduled makes the diet difficult to follow.” | 4 (21.1) | Meal planning/preparation | “The biggest obstacle has been having time to meal prep.” |
| 3 (15.8) | Special Events/Holidays/School | “I have a lot of special events.” | 4 (21.1) | Limiting carbs | “It’s difficult because she misses bread, potatoes, and pasta.” |
| 3 (15.8) | Peer pressure | “It’s hard when she goes out with friends or when there are parties.” | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pratt, K.; Cotto, J.; Xu, J.; Watowicz, R.; Walston, M.; Eneli, I. Adolescents’ and Parents’ Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity. Int. J. Environ. Res. Public Health 2019, 16, 3385. https://doi.org/10.3390/ijerph16183385
Pratt K, Cotto J, Xu J, Watowicz R, Walston M, Eneli I. Adolescents’ and Parents’ Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity. International Journal of Environmental Research and Public Health. 2019; 16(18):3385. https://doi.org/10.3390/ijerph16183385
Chicago/Turabian StylePratt, Keeley, Jennifer Cotto, Jinyu Xu, Rosanna Watowicz, Marnie Walston, and Ihuoma Eneli. 2019. "Adolescents’ and Parents’ Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity" International Journal of Environmental Research and Public Health 16, no. 18: 3385. https://doi.org/10.3390/ijerph16183385
APA StylePratt, K., Cotto, J., Xu, J., Watowicz, R., Walston, M., & Eneli, I. (2019). Adolescents’ and Parents’ Perspectives of a Revised Protein-Sparing Modified Fast (rPSMF) for Severe Obesity. International Journal of Environmental Research and Public Health, 16(18), 3385. https://doi.org/10.3390/ijerph16183385






