Based on the Theory of Planned Behavior [
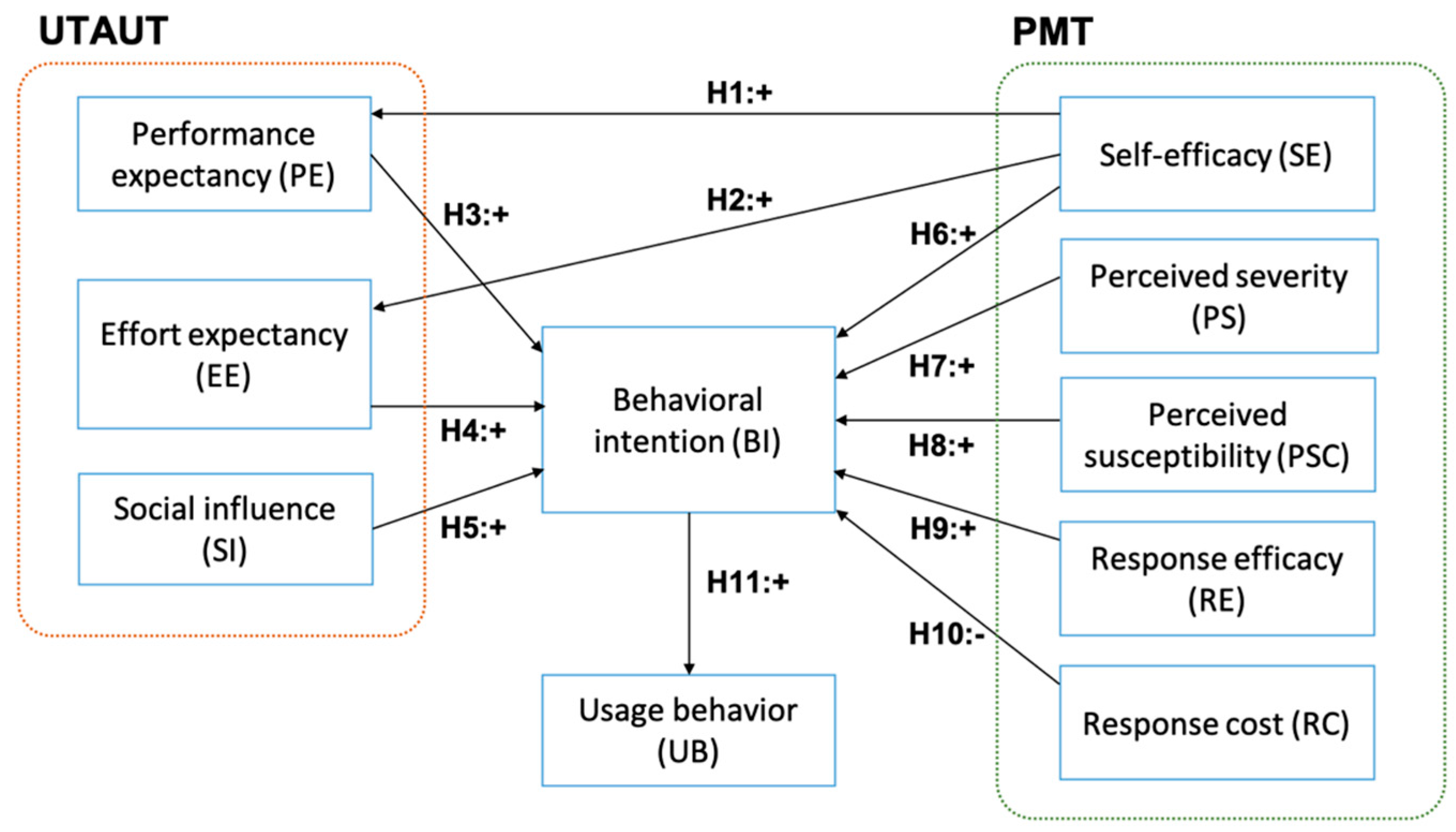
29], intention captures the motivational aspects that influence the actual behavior. The stronger the intention to carry out a specific behavior, the more likely the undertaking will be. Consumers’ intention to modify or take up a specific behavior (e.g., participating in online health communities, searching and sharing health information, and having an online consultation with medical professionals) precedes and shapes the actual behavior. Accordingly, consumers’ behavior in this study refers to the intention that precedes the actual participations, which include all activities associated with e-patient and health communication on social media, and the cognitive and social processes that precede and follow these activities. The integration of UTAUT and PMT is viable to analyze and to interpret consumers’ behavior in using social media for optimum online health communication.
2.1. Hypotheses Development
The UTAUT provides a lens to examine users’ intentions to use information technology and their actual behavior, based on four construct variables, i.e., performance expectancy, effort expectancy, social influence, and facilitating condition [
27]. The UTAUT model has been widely tested in real world applications, including healthcare technologies, to investigate the factors that influence the use and acceptance of e-health in a specific region [
30,
31]; consumers’ intention to adopt wearable healthcare technologies [
32] and mobile health systems [
33,
34,
35]; and healthcare professionals’ intention to adopt the mobile electronic medical record (EMR) [
35]. A review in [
33] suggests that perceived ease of use, perceived usefulness, and facilitating qualities influence and increase consumers’ adoption of mobile technologies. A study in [
35] shows how performance expectancy affect users’ intention to use the mobile EMR and suggests that the most beneficial functions that could increase users’ performance should be optimized. A study in [
34] reported that social influence was one of the significant factors that contributed to the adoption of m-health by elderly users in a developing country. The study also suggests that socio-economic and local culture might have confounded the results of their study because parts of them appeared to be inconsistent with what had been documented in the literature.
The PMT postulates that threats and coping appraisal motivate an individual to undertake self-protective behavior [
25]. The PMT model has been applied to examine health-related intention and behavior, for example, the way to change attitude in embracing healthier living [
36], the adoption of mobile health services [
26,
37], and compliance with electronic medical record privacy policies [
38]. Babazadeh et al. [
36] conducted a study to explore the factors that shaped skin cancer preventive behaviors (SCPB) in rural areas and suggested that it was the perceived susceptibility that influenced preventive behaviors among farmers. In another study, Guo et al. [
37] reported that threat appraisal factors (perceived vulnerability and perceived severity) and coping appraisal factors (response efficacy and self-efficacy), along with the attitude specific to gender and age, affected the intention to adopt m-health. The threat appraisal factors had higher impacts on attitude among women and the elderly, while coping appraisal factors had more significant effects on attitude among men and the youth. Despite its wide application in health behavior interpretation or social media usage, the use of PMT model on social media for health communication is rather limited.
The first hypotheses set considers the consumer’s self-efficacy and the key attributes of technology acceptance, i.e., performance expectancy (PE) and effort expectancy (EE). Self-efficacy refers to the sense of confidence in one’s ability to accomplish a task successfully. The task in this study encompasses all activities of using social media for e-patient and health-related purposes. Confident and skillful users accomplish a task more frequently, thus, they perceive more benefits from using a system. Performance expectancy encompasses perceived usefulness (Technology Acceptance Model, TAM) and other constructs that are associated with the usefulness of a technology/system to assist one’s job or to improve performance. Effort expectancy is defined as the degree of ease of use of a technology/system, which includes the perceived ease of use and complexity constructs. Previous studies have demonstrated that self-efficacy positively influences PE and EE [
39,
40,
41]. The first hypotheses set, thus, comprise:
Hypothesis 1 (H1). Self-efficacy has a positive impact on performance expectancy.
Hypothesis 2 (H2). Self-efficacy has a positive impact on effort expectancy.
According to the UTAUT framework, PE and EE influence the intention to use a technology, including Health Information Technology (HIT). Prior studies have demonstrated that PE and EE are positively correlated with behavioral intention, such as HIT acceptance in a specific region [
30], the acceptance of wearable technology in health care [
32], and the adoption of mobile technologies [
34,
35]. Similarly, social influence also impacts the intention to use a technology [
26,
42,
43]. Social influence considers the social norms where an individual uses a technology/system and the influence of important others relating to the use of a technology/system [
27]. Thus, the formulated hypotheses are as follows:
Hypothesis 3 (H3). Performance expectancy has a positive impact on behavioral intention to use social media for e-patient activities.
Hypothesis 4 (H4). Effort expectancy has a positive impact on behavioral intention to use social media for e-patient activities.
Hypothesis 5 (H5). Social influence have a positive impact on behavioral intention to use social media for e-patient activities.
Previous studies in PMT indicate that the threat appraisal factors, i.e., perceived severity and perceived susceptibility, positively impact the intention to use a system [
32,
44]. Perceived susceptibility refers to how vulnerable an individual to a health threat, while perceived severity is defined as the degree of an individual’s belief that he/she would suffer from a health threat from unhealthy lifestyle [
45,
46]. When facing a relatively unknown or a significant threat, users tend to develop a positive attitude in taking a preventive action or in minimizing the risks. Hence, we propose the following hypotheses:
Hypothesis 6 (H6). Perceived severity has a positive impact on behavioral intention to use social media for e-patient activities.
Hypothesis 7 (H7). Perceived susceptibility has a positive impact on behavioral intention to use social media for e-patient activities.
Similarly, the coping factors, i.e., self-efficacy and response efficacy, also significantly influence behavioral intention [
47,
48]. Response efficacy refers to an individual’s belief that health threats could be reduced by adopting a specific coping response [
47]. When a user decides to adopt a technology or a system, he/she considers the effort and time to learn how to use the system and how to achieve satisfactory productivity, i.e., the response cost. Therefore, a high response cost hinders technology/system adoption [
44,
48]. Considering the results of the PMT applications, the hypotheses are formulated as follows:
Hypothesis 8 (H8). Self-efficacy has a positive impact on behavioral intention to use social media for e-patient activities.
Hypothesis 9 (H9). Response-efficacy has a positive impact on behavioral intention to use social media for e-patient activities.
Hypothesis 10 (H10). Response-cost has a negative impact on behavioral intention to use social media for e-patient activities.
Lastly, behavioral intention indicates the motivational assertion pertaining to engaging in a specific behavior that shapes the actual behavior. Drawing on the UTAUT framework, the intention to use a specific system/technology affects the actual usage [
27,
49], thus, we propose the following hypothesis:
Hypothesis 11 (H11). Behavioral intention has a positive impact on usage behavior.
Figure 1 shows the research model of this study.
2.2. Data Collection
We conducted a purposive sampling to recruit the study participants from all over Indonesia. The recruited participants were non-medical professionals with a minimum age of 18 years, Indonesian citizens or have been living in Indonesia for at least one year, was on social media, at least on one platform, e.g., Twitter, Facebook, Instagram, YouTube, Blogger, etc., and had the experience in using social media for e-patient activities. The participants consisted of undergraduate and graduate students, professionals (a person engaged or qualified in a profession, i.e., lawyer, academic professor, language tutor, software engineer, and psychologist), entrepreneurs, and homemakers.
The data was collected using paper-based and web-based questionnaires that consisted of demographic profile and behavioral questions. Both questionnaires were identical. The paper-based questionnaire was given to the participants who lived in Surabaya, Jakarta, and Bandung (Indonesia), while the web-based questionnaire was sent to participants who lived outside these cities. The purpose of using the two media was to increase the distribution of the participants’ domiciles so that they adequately represented the geographical areas in Indonesia. Each questionnaire was written in two languages: English and Bahasa Indonesia. A certified translator translated the questions and all participants’ responses from Bahasa Indonesia into English. The questions relating to UTAUT were adapted from [
27], while the questions pertaining to PMT were adapted from [
23,
50,
51].
Before the data collection, one public health practitioner (Expert 1) and one health informatics expert (Expert 2) assessed the face validity (i.e., readability, feasibility, and clarity of wording) and the content validity of the questionnaire. The evaluation of the questionnaire validity followed the average congruency percentage (ACP) method [
52]. Expert 1 assessed that 28 out of 29 questions were relevant, while Expert 2 agreed on 27 out of 29 questions, yielding an ACP score of 94.83%. Since the score was higher than 90%, the questionnaire was considered valid [
52]. We revised the questionnaire according to the experts’ feedback on the clarity of wording and conducted a pilot readability test to 20 selected participants. Subsequently, we submitted the data collection protocol to Health Research Ethical Committee of Faculty of Public Health, Universitas Airlangga. After the ethical review approval (certificate number 50/EA/KEPK/2019), the questionnaire was distributed to the participants. The participants for paper-based questionnaire were recruited by phone, email, and via university bulletin board, while participants for the web-based questionnaire were recruited by email, messaging apps (i.e., WhatsApp and Line), and via invitation sent to Indonesian health community social media. The indicator and the corresponding question are presented in
Appendix A and the full English questionnaire is provided in
Supplementary Material File S1.
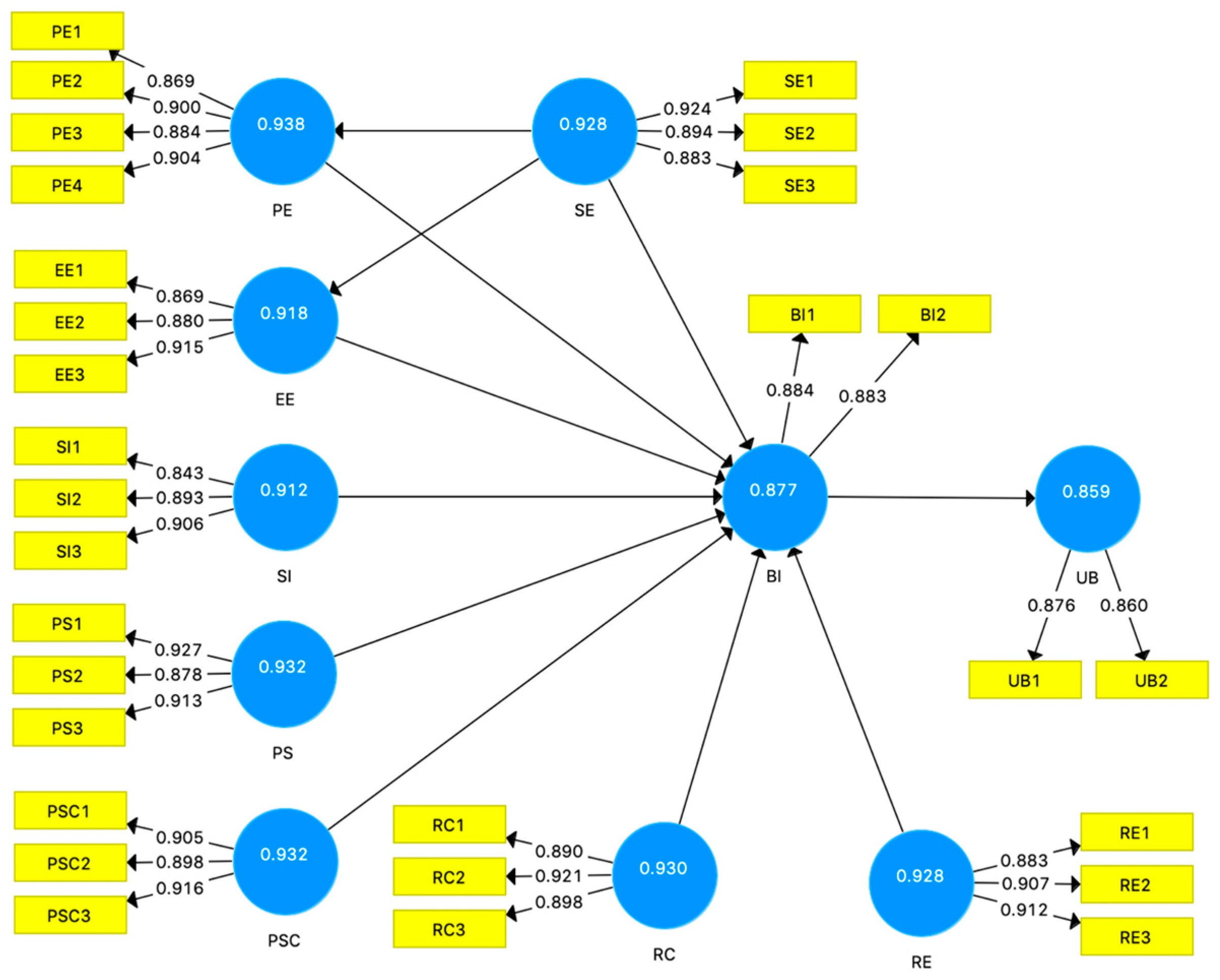
2.3. Data Model and Analysis
The data collected from the participants was tabulated using descriptive statistical analysis that covered all the demographic profiles and answers. To describe the users’ behavior in using social media for online health communication, we developed a model based on partial least square structural equation modeling (PLS-SEM). The PLS-SEM was selected because the proposed model comprised many indicators, the data collected was non-normally distributed, and one of the study purposes was to identify the driver constructs [
53,
54]. The evaluation of the proposed model consisted of the measurement model assessment and the structural model analysis.
The measurement model examines the indicator loadings, the internal consistency reliability, the convergent validity, and the discriminant validity [
54]. The recommended indicator loadings value is above 0.708. The internal consistency can be assessed using the composite reliability (CR) and the threshold CR value is above 0.7 [
55]. The convergent validity tests whether the expected related constructs shared a high proportion of the variance in the average variance extracted (AVE) metric. The recommended AVE value is higher than 0.6 [
54]. Lastly, the discriminant validity tests the degree of a single construct and whether it is distinct from other constructs in the model. The discriminant validity of the construct is satisfied if the correlation between latent constructs was greater than
[
55].
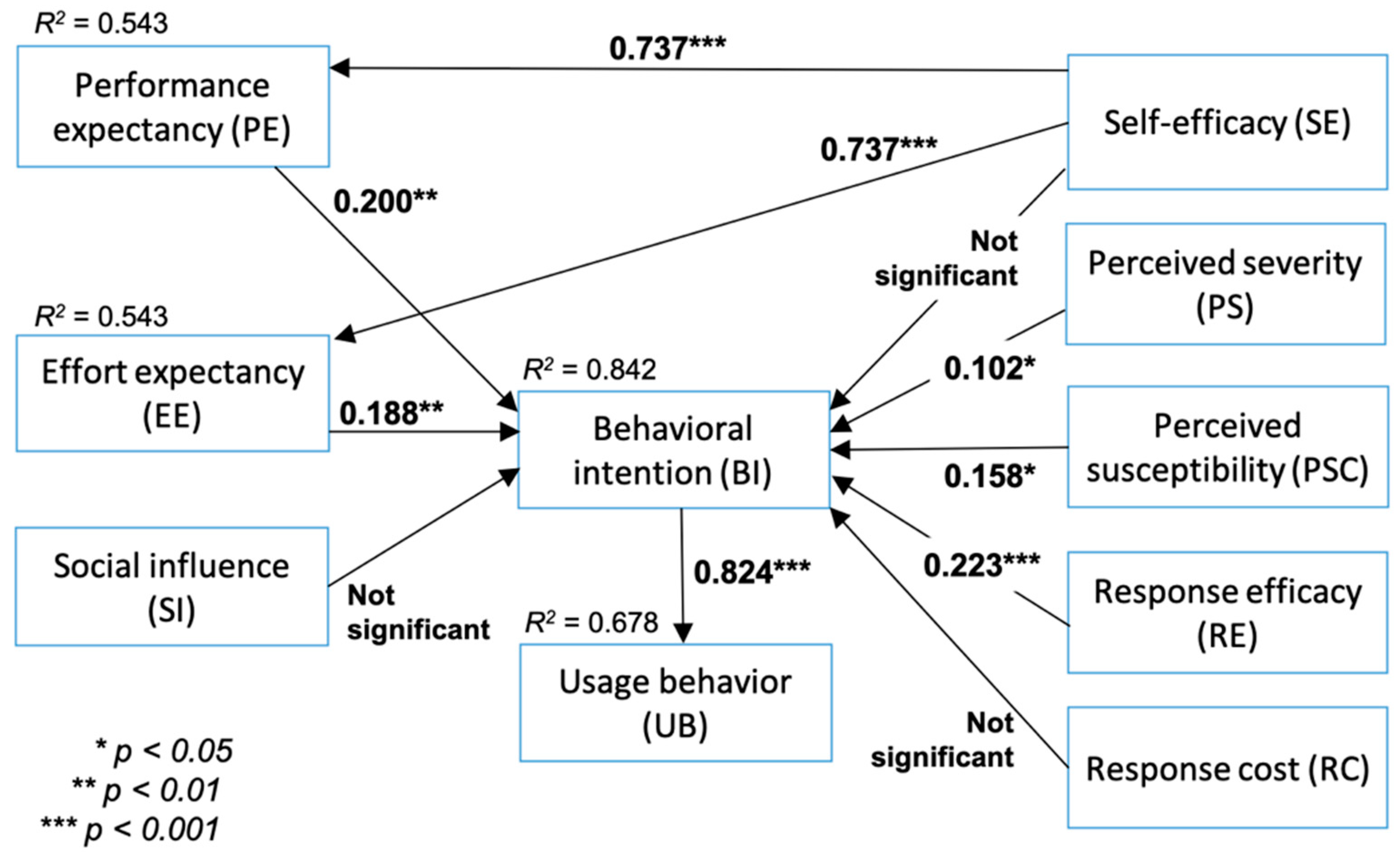
Provided that all measurement model results were satisfactory, the next step was evaluating the structural model. The structural model assessment criteria included the coefficient of determination (
R2), cross-validated redundancy (Q
2), and path coefficients [
54]. The
R2 measures the model explanatory power within the range of 0–1, with the higher value denoting a higher explanatory power [
56]. The Q
2 assesses the model’s predictive accuracy by employing a blindfolding technique. As a guideline, the Q
2 value should be larger than zero, with values higher than 0, 0.25, and 0.5 exhibiting small, medium, and large PLS model predictive relevance [
54]. Other criteria that can be used to evaluate the structural model are the standardized root mean square residual (SRMR) and normed fit index (NFI) [
57]. SRMR can be used to avoid model misspecification by measuring the difference between the observed correlation and the model implied correlation matrix [
57]. The SRMR recommended value is below 0.1 or of 0.08 [
58]. NFI compares the discrepancy between the χ
2 value of the proposed model and the χ
2 value of the null model. The general cut-off for a good fit of NFI is larger than 0.90. Finally, the last step was examining the relationships among hypothesized latent constructs and observable variables based on the statistical significance and the relevance of the path coefficients.