Communicating Risk for a Climate-Sensitive Disease: A Case Study of Valley Fever in Central California
Abstract
1. Introduction
Climate Change and Epidemiology of Valley Fever
2. Materials and Methods
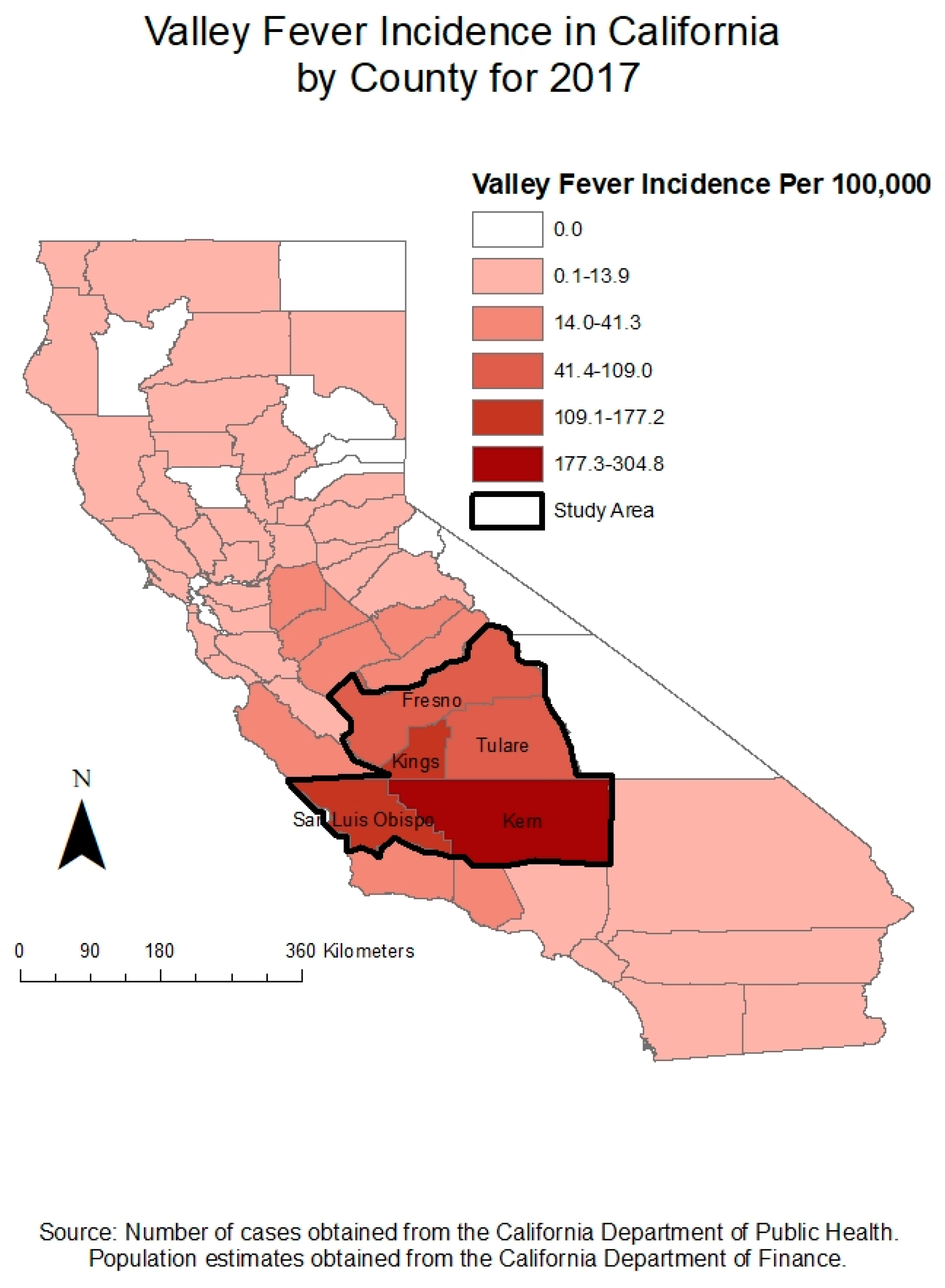
2.1. Study Location
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Research Question 1: How do Central Californian Public Health Agencies Currently Communicate Valley Fever Prevention to their Communities?
3.1.1. “Get Tested” Valley Fever Prevention Messages
3.1.2. Aligning Dissemination of Valley Fever Risk Campaigns with Peak Seasonal Onset
3.1.3. Targeted Messaging for At-Risk Groups
Valley Fever Messaging for Construction Workers and Sites
Valley Fever Messaging for Farmers
Valley Fever Messaging for the Prison Population
3.1.4. Absence of Explicit Discussion about Valley Fever as a Climate-Sensitive Disease
3.1.5. Climate Influences on Valley Fever Discussed as Wind Messages
3.2. Research Question 2: How Would these Agencies Like toSsee Climate Communication in Relation to Valley Fever?
3.2.1. Comparisons with Public Health Risk Messages Already Familiar to the Public
3.2.2. Analogies with Health Conditions Familiar to the Public
3.2.3. Valley Fever Risk Message Fatigue
3.3. Research Question 3: What Limitations/Challenges do Public Health Agencies See with Communicating Climate Risk to their Local Communities?
3.3.1. Uncertainty Inherent to Valley Fever Diagnosis Presents Prevention Challenge
3.3.2. Political Considerations in Valley Fever Messaging to Farmers
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moser, S. Communicating Climate Change Adaptation and Resilience. Oxf. Res. Encycl. Clim. Sci. 2017. [Google Scholar] [CrossRef]
- Burton, I. Vulnerability and Adaptive Response in the Context of Climate and Climate Change. Clim. Change 1997, 26, 185–196. [Google Scholar] [CrossRef]
- Frumkin, H.; McMichael, A. Climate Change and Public Health: Thinking, Communicating, Acting. Am. J. Prev. Med. 2008, 35, 403–410. [Google Scholar] [CrossRef]
- Hornik, R. Communicating to Advance the Public’s Health: Workshop Summary; National Academic Press: Washington, DC, USA; Roundtable on Population Health Improvement: Washington, DC, USA; Board on Population Health and Public Health Practice: Washington, DC, USA; Institute of Medicine: Bational Academic Press, 2015. [Google Scholar] [CrossRef]
- Lundgren, R.; McMakin, A. Risk Communication: A Handbook for Communicating Environmental, Safety, and Health Risks, 5th ed.; Battelle Press: Columbus, OH, USA, 2013. [Google Scholar]
- Levine, A.; Kline, R. A new approach for evaluating climate change communication. Clim. Change 2017, 142, 301–309. [Google Scholar] [CrossRef]
- Fischhoff, B. Risk Perception and Communication Unplugged: Twenty Years of Process. Risk Anal. 1995, 15, 137–145. [Google Scholar] [CrossRef]
- Ockwell, O.; Whitmarsh, L.; O’Neill, S. Reorienting Climate Change Communication for Effective Mitigation: Forcing People to be Green or Fostering Grass-Roots Engagement? Sci. Commun. Sage 2009, 30, 3. [Google Scholar] [CrossRef]
- Adger, W.; Dessai, S.; Goulden, M.; Hulme, M.; Lorenzoni, I.; Nelson, D.; Naess, L.; Wolf, J.; Wreford, A. Are there social limits to adaptation to climate change? Clim. Change 2008, 93, 335–354. [Google Scholar] [CrossRef]
- Communicating for Health. Available online: https://www.who.int/communicating-for-health/principles/en/ (accessed on 14 July 2019).
- Parrott, R.; Monahan, J.; Ainsworth, S.; Steiner, C. Communicating to Farmers about Skin Cancer the Behavior Adaptation Model. Hum. Commun. Res. 1988, 23, 386–409. [Google Scholar] [CrossRef]
- Barr, S.; Woodley, E. Enabling communities for a changing climate: Re-configuing spaces of hazard governance. Geoforum 2019, 100, 116–127. [Google Scholar] [CrossRef]
- Slovic, P. Perceived Risk, Trust, and Democracy. Risk Anal. 1993, 13, 675–682. [Google Scholar] [CrossRef]
- Kasperson, R. Four questions for risk communication. J. Risk Res. 2014, 17, 1233–1239. [Google Scholar] [CrossRef]
- Peiffer, R.; O’Connor, M.; Horwitz, P. Nowhere to hide: Awareness and perceptions of environmental changes, and their influence on relationships with place. J. Environ. Psychol. 2005, 25, 147–158. [Google Scholar] [CrossRef]
- CDC-NIOSH Publications and Products-NIOSH Fast Facts: Protecting Yourself from Sun Exposure (2010-116). Available online: https://www.cdc.gov/niosh/docs/2010-116/ (accessed on 15 June 2019).
- Maibach, E. Increasing Public Awareness and Facilitating Behavior Change: Two Guiding Heuristics, Climate Change and Biodiversity, 2nd ed.; Yale University Press: London, UK, 2017. [Google Scholar]
- Extremely High Levels of PM2.5: Steps to Reduce Your Exposure. Available online: https://airnow.gov/aqi/aqi-basics/extremely-high-levels-of-pm25 (accessed on 15 June 2019).
- Nerlich, B.; Koteyko, N.; Brown, B. Theory and language of climate change communication. WIREs Clim. Change 2009, 1, 97–110. [Google Scholar] [CrossRef]
- Berkhout, F. Adaptation to climate change by organizations. WIREs Clim. Change 2011, 3, 91–106. [Google Scholar] [CrossRef]
- Fischhoff, B.; Davis, A. Communicating scientific uncertainty. PNAS 2014, 111, 13664–13671. [Google Scholar] [CrossRef] [PubMed]
- Galgiani, J. Coccidioidomycosis: A regional disease of national importance. Rethinking approaches for control. Ann. Int. 1999, 130, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Sondermeyer Cooksey, G.; Nguyen, A.; Knutson, K.; Tabnak, F.; Benedict, K.; McCotter, O.; Jain, S.; Vugia, D. Notes from the Field: Increase in Coccidioidomycosis–California. Morb. Mortal. Wkly. Report 2017, 66, 833–834. [Google Scholar] [CrossRef]
- Nguyen, C.; Barker, B.; Hoover, S.; Nix, D.; Ampel, N.; Frelinger, J.; Orbach, M.; Galgiani, J. Recent advances in our understanding of the environmental, epidemiological, immunological, and clinical dimensions of coccidioidomycosis. Clin. Microbiol. Rev. 2013, 26, 505–525. [Google Scholar] [CrossRef]
- Coccidioidomycosis. Available online: https://www.cdc.gov/fungal/diseases/coccidioidomycosis/index.html (accessed on 30 May 2019).
- Filip, D.; Filip, S. Valley Fever Epidemic; Golden Phoenix Books: Beijing China, 2008. [Google Scholar]
- Huang, J.; Bristow, B.; Shafir, S.; Sorvillo, F. Coccidioidomycosis-associated Deaths, United States, 1990–2008. Emerg. Infect. Dis. 2012, 18, 1723–17238. [Google Scholar] [CrossRef]
- Lawrence, R.; Hoeprich, P. Comparison of amphotericin B and amphotericin B methyl ester: Efficacy in murine coccidioidomycosis and toxicity. J. Infect. Dis. 1976, 133, 168–174. [Google Scholar] [CrossRef]
- Converse, J.; Reed, R. Experimental epidemiology of coccidioidomycosis. Bacteriol. Rev. 1966, 30, 678. [Google Scholar]
- Ampel, N.; Mosley, D.; England, B.; Vertz, P.; Komatsu, K.; Hajjeh, R. Coccidioidomycosis in Arizona: Increase in incidence from 1990 to 1995. Clin. Infect. Dis. 1998, 27, 1528–1530. [Google Scholar] [CrossRef] [PubMed]
- Egeberg, R.; Ely, A. Coccidioides Immitis in the soil of the southern San Joaquin Valley. Am. J. Med. Sci. 1956, 231, 151–154. [Google Scholar] [CrossRef]
- Hugenholtz, P. Climate and coccidioidomycosis. In Proceedings of the Symposium on Coccidioidomycosis, Phoenix, AZ, USA, 1957; Public Health Services: Washington, DC, USA, 1957; Publication 575; pp. 136–143. [Google Scholar]
- Maddy, K. Observations on Coccidioides immitis found growing naturally in soil. Ariz. Med. 1965, 22, 281–288. [Google Scholar] [PubMed]
- Jinadu, B. Valley Fever Task Force Report on the Control of Coccidioides Immitis, Kern County; Kern County Health Department: Bakersfield, CA, USA, 1995. [Google Scholar]
- Stevens, D. Coccioioidomycosis. N. Engl. J. Med. 1995, 322, 1077–1082. [Google Scholar] [CrossRef]
- Maddy, K. Ecological Factors possibly relating to the geographic distribution of Coccidioides immitis. In Proceedings of the Symposium on Coccidioidomycosis, Phoenix, AZ, USA, 11–13 February1957; Public Health Service: Washington, DC, USA; pp. 144–157. [Google Scholar]
- Kolivras, K.; Comrie, A. Modeling valley fever (coccidioidomycosis) incidence on the basis of climate conditions. Int. J. Biometeorol. 2003, 47, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Sigel, K.; Vaz, V.; Komatsu, K.; McRill, C.; Phelan, M.; Colman, T.; Comrie, A.; Warnock, D.; Galgiani, J.; et al. An epidemic of coccidioidomycosis in Arizona associated with climatic changes, 1998–2001. J. Infect. Dis. 2005, 191, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Comrie, A. Climate factors influencing coccidioidomycosis seasonality and outbreaks. Environ. Health Perspect. 2005, 113, 688–692. [Google Scholar] [CrossRef]
- Comrie, A.; Glueck, M. Assessment of climate-coccidioidomycosis model: Model sensitivity for assessing climatologic effects on the risk of acquiring coccidioidomycosis. Ann. N.Y. Acad. Sci. 2007, 1111, 83–95. [Google Scholar] [CrossRef]
- Zender, C.; Talamantes, J. Climate controls on valley fever incidence in Kern County, California. Int. J. Biometeorol. 2006, 50, 174–182. [Google Scholar] [CrossRef]
- Talamantes, J.; Behseta, S.; Zender, C. Statistical modeling of valley fever data in Kern County, California. Int. J. Biometeorol. 2007, 51, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Stacy, P.; Comrie, A.; Yool, S. Modeling valley fever incidence in Arizona using a satellite-derived soil moisture proxy. GISci. Remote Sens. 2012, 49, 299–316. [Google Scholar] [CrossRef]
- Sprigg, W.; Nickovic, S.; Galgiani, J.; Pejanovic, G.; Petkovic, S.; Vujadinovic, M.; Vukovic, A.; Dacic, M.; DiBiase, S.; Prasad, A. Regional dust storm modeling for health services: The case of valley fever. Aeolian Res. 2014, 14, 53–73. [Google Scholar] [CrossRef]
- Gorris, M.; Cat, L.; Zender, C.; Treseder, K.; Randerson, J. Coccidioidomycosis Dynamics in Relation to Climate in the Southwestern United States. GeoHealth 2018, 2, 6–24. [Google Scholar] [CrossRef]
- Tracy, S.J. Qualitative Research Methods: Collecting Evidence, Crafting Analysis, Communicating Impact; Wiley-Blackwell: Oxford, UK, 2013. [Google Scholar]
- Morse, J.M. Data were saturated. Qual. Health Res. 2015, 25, 587–588. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage: Beijing, China, 1985. [Google Scholar]
- Tracy, S.J. Qualitative quality: Eight big tent criteria for excellent qualitative research. Qual. Inq. 2010, 16, 837–851. [Google Scholar] [CrossRef]
- Innes, S.; Pierce, H. States Skimp on Valley Fever Awareness. Center for Health Journalism Collaborative. 2017. Available online: https://www.centerforhealthjournalism.org/valleyfever/states-skimp-valley-fever-awareness (accessed on 13 July 2019).
- Fischhoff, B. Strategies for Risk Communication. Appendix, C. In National Research Council: Improving Risk Communication; National Academy Press: Washington, DC, USA, 1995; pp. 282–320. [Google Scholar]
- Smit, B.; McNabb, D.; Smithers, J. Agricultural adaptation to climatic variation. Clim. Change 1996, 33, 7–29. [Google Scholar] [CrossRef]
- Holloway, L. Understanding Climate Change and Farming: Scientific and Farmers’ Constructions of Global Warming in Relation to Agriculture. Sage 1999, 31, 2017–2032. [Google Scholar] [CrossRef]
- Gbetibouo, G. Understanding Farmer’s Perceptions and Adaptations to Climate Change and Vulnerability. The case of the Limpopo Basin, South Africa; International Food Policy Research Institute: Washington, DC, USA, 2009. [Google Scholar]
- Geoghegan, H.; Leyson, C. On climate change and cultural geography: Farming on the Lizard Peninsula, Cornwall, UK. Clim. Change 2012, 113, 55–66. [Google Scholar] [CrossRef]
- Seo, S. Modeling farmer adaptations to climate change in South America: A micro-behavioral economic perspective. Environ. Ecol. Stat. 2016, 23, 1–21. [Google Scholar] [CrossRef]
- Mase, A.; Gramig, B.; Prokopy, L. Climate change beliefs, risk perceptions, and adaptation behavior among Midwestern, U.S. crop farmers. Clim. Risk Manag. 2017, 15, 8–17. [Google Scholar] [CrossRef]
- Prokopy, L.; Carlton, S.; Haigh, T.; Lemos, M.; Mase, A.; Widhalm, M. Useful to Usable: Developing usable climate science for agriculture. Clim. Risk Manag. 2017, 15, 1–7. [Google Scholar] [CrossRef]
- Truelove, H.; Carrico, A.; Thabrew, L. A scoio-psychological model for analyzing climate change adaptation: A case study of Sri Lankan paddy farmers. Glob. Environ. Change 2015, 31, 85–97. [Google Scholar] [CrossRef]
- Morton, L.; McGuire, J.; Cast, A. A good farmer pays attention to weather. Clim. Risk Manag. 2017, 17, 18–31. [Google Scholar] [CrossRef]
- Lubell, M.; Vedlitz, A.; Zahran, S. Collective Action, Environmental Activism, and Air Quality Policy. Political Res. Q. 2006, 59, 149–160. [Google Scholar] [CrossRef]
- Oltra, C.; Sala, R. Perception of risk from air pollution and reported behaviors: A cross-sectional survey study in four cities. J. Risk Res. 2015, 21, 869–884. [Google Scholar] [CrossRef]
- Beaumont, R.; Hamilton, R.; Machin, N.; Perks, J.; Williams, I. Social awareness of air quality information. Sci. Total Environ. 1999, 235, 319–329. [Google Scholar] [CrossRef]
- Bickerstaff, K.; Walker, G. Clearing the Smog? Public responses to air-quality information. Local Environ. 2007, 4, 279–294. [Google Scholar] [CrossRef]
- Davis, L. The Effect of Driving Restrictions on Air Quality in Mexico City. J. Political Econ. 2008, 116, 38–81. [Google Scholar] [CrossRef]
- Hendel, M.; Azos-Diaz, K.; Tremeac, B. Behavioral adaptation to heat-related health risks in cities. Energy Build. 2017, 152, 823–829. [Google Scholar] [CrossRef]
- Kates, R.; Travis, W.; Wilbanks, T. Transformational adaptation when incremental adaptations to climate change are insufficient. PNAS 2012, 109, 7156–7161. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matlock, M.; Hopfer, S.; Ogunseitan, O.A. Communicating Risk for a Climate-Sensitive Disease: A Case Study of Valley Fever in Central California. Int. J. Environ. Res. Public Health 2019, 16, 3254. https://doi.org/10.3390/ijerph16183254
Matlock M, Hopfer S, Ogunseitan OA. Communicating Risk for a Climate-Sensitive Disease: A Case Study of Valley Fever in Central California. International Journal of Environmental Research and Public Health. 2019; 16(18):3254. https://doi.org/10.3390/ijerph16183254
Chicago/Turabian StyleMatlock, Melissa, Suellen Hopfer, and Oladele A. Ogunseitan. 2019. "Communicating Risk for a Climate-Sensitive Disease: A Case Study of Valley Fever in Central California" International Journal of Environmental Research and Public Health 16, no. 18: 3254. https://doi.org/10.3390/ijerph16183254
APA StyleMatlock, M., Hopfer, S., & Ogunseitan, O. A. (2019). Communicating Risk for a Climate-Sensitive Disease: A Case Study of Valley Fever in Central California. International Journal of Environmental Research and Public Health, 16(18), 3254. https://doi.org/10.3390/ijerph16183254





