Racial/Ethnic Differences in Physiological Stress and Relapse among Treatment Seeking Tobacco Smokers
Abstract
1. Introduction
The Present Study
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Intervention
2.5. Measures
2.5.1. Demographics
2.5.2. Nicotine Dependence
2.5.3. Sleep
2.5.4. Physiological Stress
2.5.5. Smoking Relapse
2.6. Statistical Analyses
3. Results
3.1. Participant Characteristics by Race/Ethnicity
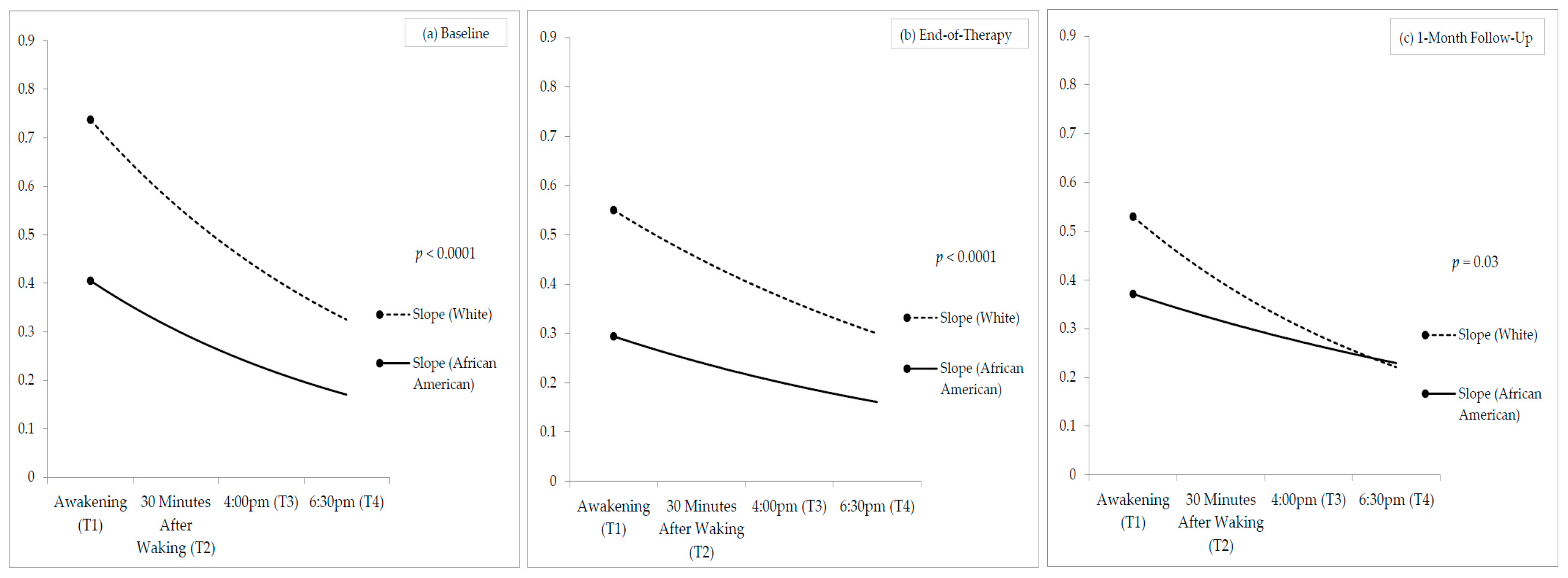
3.2. Physiological Stress Overall and by Race/Ethnicity
3.3. Smoking Relapse
4. Discussion
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- American Cancer Society. Cancer Facts & Figures for African Americans 2016–2018; American Cancer Society: Atlanta, GA, USA, 2016. [Google Scholar]
- U.S. Department of Health and Human Services. Tobacco Use Among U.S. Racial/ethnic Minority Groups — African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A Report of the Surgeon General; Department of Health and Human Services: Washington, DC, USA; Centers for Disease Control and Prevention: Atlanta, GA, USA, 1998.
- Sheffer, C.E.; Stitzer, M.; Landes, R.; Brackman, S.L.; Munn, T.; Moore, P. Socioeconomic disparities in community-based treatment of tobacco dependence. Am. J. Public Health 2012, 102, e8–e16. [Google Scholar] [CrossRef] [PubMed]
- Covey, L.S.; Botello-Harbaum, M.; Glassman, A.H.; Masmela, J.; LoDuca, C.; Salzman, V.; Fried, J. Smokers’ Response to Combination Bupropion, Nicotine Patch, and Counseling Treatment by Race/Ethnicity. Ethn. Dis. 2008, 18, 59–64. [Google Scholar] [PubMed]
- Honda, K. Psychosocial correlates of smoking cessation among elderly ever-smokers in the United States. Addict. Behav. 2005, 30, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Kassel, J.D.; Stroud, L.R.; Paronis, C.A. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychol. Bull. 2003, 129, 270–304. [Google Scholar] [CrossRef] [PubMed]
- Berg, C.J.; Wen, H.; Cummings, J.R.; Ahluwalia, J.S.; Druss, B.G. Depression and substance abuse and dependency in relation to current smoking status and frequency of smoking among nondaily and daily smokers. Am. J. Addict. 2013, 22, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, R.; Shen, C.; Sambamoorthi, U. Excess risk of chronic physical conditions associated with depression and anxiety. BMC Psychiatry 2014, 14, 10. [Google Scholar] [CrossRef] [PubMed]
- Colby, J.P.; Linsky, A.S.; Straus, M.A. Social Stress and State-to-State Differences in Smoking and Smoking-Related Mortality in the United-States. Soc. Sci. Med. 1994, 38, 373–381. [Google Scholar] [CrossRef]
- Geronimus, A.T.; Thompson, J.P. To denigrate, ignore, or disrupt: Racial inequality in health and the impact of a policy-induced breakdown of African American communities. Du Bois Rev. Soc. Sci. Res. Race 2004, 1, 247–279. [Google Scholar] [CrossRef]
- Romano, P.S.; Bloom, J.; Syme, S.L. Smoking, social support, and hassles in an urban African-American community. Am. J. Public Health 1991, 81, 1415–1422. [Google Scholar] [CrossRef]
- Slopen, N.; Dutra, L.M.; Williams, D.R.; Mujahid, M.S.; Lewis, T.T.; Bennett, G.G.; Ryff, C.D.; Albert, M.A. Psychosocial stressors and cigarette smoking among African American adults in midlife. Nicot. Tob. Res. 2012, 14, 1161–1169. [Google Scholar] [CrossRef]
- Webb, M.S.; Carey, M.P. Tobacco smoking among low-income Black women: Demographic and psychosocial correlates in a community sample. Nicot. Tob. Res. 2008, 10, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Slopen, N.; Kontos, E.Z.; Ryff, C.D.; Ayanian, J.Z.; Albert, M.A.; Williams, D.R. Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9-10 years: A prospective study of middle-aged adults in the United States. Cancer Causes Control 2013, 24, 1849–1863. [Google Scholar] [CrossRef] [PubMed]
- Mulder, B.C.; de Bruin, M.; Schreurs, H.; van Ameijden, E.J.; van Woerkum, C.M. Stressors and resources mediate the association of socioeconomic position with health behaviours. BMC Public Health 2011, 11, 798. [Google Scholar] [CrossRef] [PubMed]
- Flint, A.J.; Novotny, T.E. Poverty status and trends in smoking prevalence and cessation in the United States, 1983-1992. Circulation 1996, 93, 20. [Google Scholar]
- Winkleby, M.A.; Jatulis, D.E.; Frank, E.; Fortmann, S.P. Socioeconomic-Status and Health—How Education, Income, and Occupation Contribute to Risk-Factors for Cardiovascular-Disease. Am. J. Public Health 1992, 82, 816–820. [Google Scholar] [CrossRef]
- Barbeau, E.M.; Krieger, N.; Soobader, M.J. Working class matters: Socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am. J. Public Health 2004, 94, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.J.; Avison, W.R. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. J. Health Soc. Behav. 2003, 44, 488–505. [Google Scholar] [CrossRef]
- Berg, C.J.; Thomas, J.L.; Guo, H.; An, L.C.; Okuyemi, K.S.; Collins, T.C.; Ahluwalia, J.S. Predictors of smoking reduction among Blacks. Nicot. Tob. Res. 2010, 12, 423–431. [Google Scholar] [CrossRef]
- Manning, B.K.; Catley, D.; Harris, K.J.; Mayo, M.S.; Ahluwalia, J.S. Stress and quitting among African American smokers. J. Behav. Med. 2005, 28, 325–333. [Google Scholar] [CrossRef]
- Knight, J.M.; Avery, E.F.; Janssen, I.; Powell, L.H. Cortisol and Depressive Symptoms in a Population-Based Cohort of Midlife Women. Psychosom. Med. 2010, 72, 855–861. [Google Scholar] [CrossRef]
- Bonfiglio, J.J.; Inda, C.; Refojo, D.; Holsboer, F.; Arzt, E.; Silberstein, S. The corticotropin-releasing hormone network and the hypothalamic-pituitary-adrenal axis: Molecular and cellular mechanisms involved. Neuroendocrinology 2011, 94, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Dallman, M.F. Stress update Adaptation of the hypothalamic-pituitary-adrenal axis to chronic stress. Trends Endocrinol. Metab. 1993, 4, 62–69. [Google Scholar] [CrossRef]
- Chan, S.; Debono, M. Replication of cortisol circadian rhythm: New advances in hydrocortisone replacement therapy. Ther. Adv. Endocrinol. Metab. 2010, 1, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Skinner, M.L.; Shirtcliff, E.A.; Haggerty, K.P.; Coe, C.L.; Catalano, R.F. Allostasis model facilitates understanding race differences in the diurnal cortisol rhythm. Dev. Psychopathol. 2011, 23, 1167–1186. [Google Scholar] [CrossRef] [PubMed]
- Kristenson, M.; Eriksen, H.R.; Sluiter, J.K.; Starke, D.; Ursin, H. Psychobiological mechanisms of socioeconomic differences in health. Soc. Sci. Med. 2004, 58, 1511–1522. [Google Scholar] [CrossRef]
- Targovnik, J.H. Nicotine, corticotropin, and smoking withdrawal symptoms: Literature review and implications for successful control of nicotine addiction. Clin. Ther. 1989, 11, 846–853. [Google Scholar] [PubMed]
- Badrick, E.; Kirschbaum, C.; Kumari, M. The relationship between smoking status and cortisol secretion. J. Clin. Endocrinol. Metab. 2007, 92, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Koob, G.F.; Le Moal, M. Drug abuse: Hedonic homeostatic dysregulation. Science 1997, 278, 52–58. [Google Scholar] [CrossRef]
- Piazza, P.V.; Le Moal, M. The role of stress in drug self-administration. Trends Pharmacol. Sci. 1998, 19, 67–74. [Google Scholar] [CrossRef]
- al’Absi, M.; Hatsukami, D.; Davis, G.L. Attenuated adrenocorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology 2005, 181, 107–117. [Google Scholar] [CrossRef]
- Chong, R.Y.; Uhart, M.; McCaul, M.E.; Johnson, E.; Wand, G.S. Whites have a more robust hypothalamic–pituitary–adrenal axis response to a psychological stressor than blacks. Psychoneuroendocrinology 2008, 33, 246–254. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suglia, S.F.; Staudenmayer, J.; Cohen, S.; Enlow, M.B.; Rich-Edwards, J.W.; Wright, R.J. Cumulative Stress and Cortisol Disruption among Black and Hispanic Pregnant Women in an Urban Cohort. Psychol. Trauma 2010, 2, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Rosmond, R.; Bjorntorp, P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J. Int. Med. 2000, 247, 188–197. [Google Scholar] [CrossRef]
- Kolar, S.K.; Webb Hooper, M. Self-reported time-to-relapse following smoking cessation: Comparison by operationalization of initial abstinence classification. Addict. Res. Theory 2016, 24, 25–31. [Google Scholar] [CrossRef]
- Webb, M.S.; de Ybarra, D.R.; Baker, E.A.; Reis, I.M.; Carey, M.P. Cognitive-behavioral therapy to promote smoking cessation among African American smokers: A randomized clinical trial. J. Consult. Clin. Psychol. 2010, 78, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Webb Hooper, M.; Kolar, S.K. Distress, race/ethnicity and smoking cessation in treatment-seekers: Implications for disparity elimination. Addiction 2015, 110, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Brandon, T.H.; Zelman, D.C.; Baker, T.B. Effects of Maintenance Sessions on Smoking Relapse - Delaying the Inevitable. J. Consult. Clin. Psychol. 1987, 55, 780–782. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerstrom Test for Nicotine Dependence—A Revision of the Fagerstrom Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Fries, E.; Dettenborn, L.; Kirschbaum, C. The cortisol awakening response (CAR): Facts and future directions. Int. J. Psychophysiol. 2009, 72, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Minkel, J.; Moreta, M.; Muto, J.; Htaik, O.; Jones, C.; Basner, M.; Dinges, D. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. 2014, 33, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Perkins, K.A.; Karelitz, J.L.; Jao, N.C. Optimal carbon monoxide criteria to confirm 24-hr smoking abstinence. Nicot. Tob. Res. 2013, 15, 978–982. [Google Scholar] [CrossRef] [PubMed]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicot. Tob. Res. 2002, 4, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Pfister, R.; Schwarz, K.; Carson, R.; Jancyzk, M. Easy methods for extracting individual regression slopes: Comparing SPSS, R, and Excel. Tutor. Quant. Methods Psychol. 2013, 9, 72–78. [Google Scholar] [CrossRef]
- Cohen, S.; Schwartz, J.E.; Epel, E.; Kirschbaum, C.; Sidney, S.; Seeman, T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom. Med. 2006, 68, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Fuller-Rowell, T.E.; Doan, S.N.; Eccles, J.S. Differential effects of perceived discrimination on the diurnal cortisol rhythm of African Americans and Whites. Psychoneuroendocrinology 2012, 37, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.A.; Pickworth, W.B.; Waters, A.J.; al’Absi, M.; Leventhal, A.M. Cortisol levels decrease after acute tobacco abstinence in regular smokers. Hum. Psychopharmacol. 2014, 29, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Dallman, M.F.; Viau, V.G.; Bhatnagar, S.; Gomez, F.; Laugero, K.; Bell, M.E. Corticotropin-Releasing Factor, Corticosteroids, Stress, and SugarEnergy Balance, the Brain, and Behavior; Academic Press: San Diego, CA, USA, 2002; pp. 571–631. [Google Scholar]
- Steptoe, A.; Serwinski, B. Chapter 34—Cortisol Awakening Response, in Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: San Diego, CA, USA, 2016; pp. 277–283. [Google Scholar]
- Antoni, M.H.; Lechner, S.; Diaz, A.; Vargas, S.; Holley, H.; Phillips, K.; McGregor, B.; Carver, C.S.; Blomberg, B. Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain Behav. Immun. 2009, 23, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R. Effects of abstinence from tobacco: Valid symptoms and time course. Nicot. Tob. Res. 2007, 9, 315–327. [Google Scholar] [CrossRef] [PubMed]
- al’Absi, M.; Hatsukami, D.; Davis, G.L.; Wittmers, L.E. Prospective examination of effects of smoking abstinence on cortisol and withdrawal symptoms as predictors of early smoking relapse. Drug Alcohol. Depend. 2004, 73, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Novotny, T.E.; Warner, K.E.; Kendrick, J.S.; Remington, P.L. Smoking by Blacks and Whites—Socioeconomic and Demographic Differences. Am. J. Public Health 1988, 78, 1187–1189. [Google Scholar] [CrossRef]
- U.S. National Cancer Institute. A Socioecological Approach to Address Tobacco-Related Health Disparities; U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute: Bethesda, MD, USA, 2017.
- Howard, J.T.; Sparks, P.J. The Effects of Allostatic Load on Racial/Ethnic Mortality Differences in the United States. Popul. Res. Policy Rev. 2016, 35, 421–443. [Google Scholar] [CrossRef]
- McEwen, B.S. Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998, 840, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Lantz, P.M.; House, J.S.; Mero, R.P.; Williams, D.R. Stress, life events, and socioeconomic disparities in health: Results from the Americans’ changing lives study. J. Health Soc. Behav. 2005, 46, 274–288. [Google Scholar] [CrossRef] [PubMed]
- Prelow, H.M.; Danoff-Burg, S.; Swenson, R.R.; Pulgiano, D. The impact of ecological risk and perceived discrimination on the psychological adjustment of African American and European American youth. J. Community Psychol. 2004, 32, 375–389. [Google Scholar]
| Mean (SD) | White | African American | p-Value |
|---|---|---|---|
| (n = 43) | (n = 72) | ||
| Age (years) | 46.2 (13.2) | 49.5 (8.2) | 0.09 |
| Cigarettes per day | 20.19 (10.6) | 17.6 (10.2) | 0.1 |
| Years of smoking | 29.1 (12.9) | 27.8 (11.0) | 0.56 |
| Nicotine dependence (FTND) | 5.9 (2.2) | 5.6 (2.2) | 0.41 |
| Hours of Sleep | 6.89 (3.2) | 6.0 (2.4) | 0.09 |
| % (n) | |||
| Sex | 0.51 | ||
| Male | 61% (26) | 54% (39) | |
| Female | 40% (17) | 46% (33) | |
| Total annual household income | <0.01 | ||
| Under $10,000 | 43% (18) | 63% (45) | |
| $10,000 to $20,000 | 17% (7) | 10% (16) | |
| $20,001 to $40,000 | 17% (7) | 14% (10) | |
| > $40,000 | 26% (11) | 1% (1) | |
| Marital status | 0.41 | ||
| Single | 42% (18) | 58% (42) | |
| Married | 13% (9) | 13% (9) | |
| Separated/Divorced/Widowed | 37% (16) | 29% (21) | |
| Education | 0.04 | ||
| Less than high school | 16% (7) | 21% (15) | |
| High school | 26% (11) | 38% (27) | |
| Business or technical training | 2% (1) | 10% (7) | |
| Some college, no degree | 28% (12) | 26% (19) | |
| College degree | 28% (12) | 6% (4) | |
| Sleep | |||
| Overnight Bedtime | 85% (37) | 80% (58) | 0.45 |
| Day Bedtime | 15% (6) | 20% (14) | |
| Baseline (Session 1) | Overall | White | African American | p-Value |
|---|---|---|---|---|
| Mean μg/dL (SD) | ||||
| Awakening (T1) | 0.45 (0.41) | 0.66 (0.55) | 0.37 (0.30) | 0.01 |
| 30 Minutes After Waking (T2) | 0.48 (0.60) | 0.71 (0.97) | 0.37 (0.29) | 0.03 |
| 4:00 pm (T3) | 0.26 (0.24) | 0.39 (0.29) | 0.21 (0.21) | 0.04 |
| 6:30 pm (T4) | 0.21 (0.23) | 0.31 (0.30) | 0.17 (0.19) | 0.01 |
| End-of-Therapy | ||||
| Awakening (T1) | 0.36 (0.31) | 0.51 (0.40) | 0.27 (0.18) | < 0.01 |
| 30 Minutes After Waking (T2) | 0.38 (0.28) | 0.49 (0.35) | 0.31 (0.20) | < 0.01 |
| 4:00 pm (T3) | 0.24 (0.28) | 0.39 (0.40) | 0.16 (0.12) | < 0.01 |
| 6:30 pm (T4) | 0.21 (0.29) | 0.24 (0.40) | 0.17 (0.19) | 0.04 |
| 1-Month Follow-up | ||||
| Awakening (T1) | 0.40 (0.22) | 0.48 (0.25) | 0.35 (0.19) | 0.04 |
| 30 Minutes After Waking (T2) | 0.41 (0.25) | 0.47 (0.28) | 0.36 (0.21) | 0.07 |
| 4:00 pm (T3) | 0.27 (0.20) | 0.28 (0.20) | 0.26 (0.20) | 0.99 |
| 6:30 pm (T4) | 0.22 (0.16) | 0.22 (0.16) | 0.23 (0.16) | 0.79 |
| Characteristic | Session 1 to EOT (n = 107) | Session 1 to EOT | Session 1 to 1-Month Follow-Up (n = 109) | Session 1 to 1-Month Follow-Up |
|---|---|---|---|---|
| AOR 1 (95% CI) | AOR 2 (95% CI) | AOR 1 (95% CI) | AOR 2 (95% CI) | |
| Race/Ethnicity | ||||
| White | Ref | Ref | Ref | Ref |
| African American | 3.89 (1.10–13.78) | 3.60 (0.98–13.24) | 2.73 (1.08–6.91) | 3.81 (1.36–10.64) |
| Education | 1.11 (0.79–1.55) | 1.10 (0.77–1.58) | 1.17 (0.87–1.56) | 1.20 (0.87–1.65) |
| Household Income | 1.17 (0.91–1.51) | 1.18 (0.87–1.60) | 1.02 (0.81–1.27) | 1.09 (0.83–1.42) |
| Baseline Cortisol Slope | 0.54 (0.60–4.87) | 0.97 (0.12–7.91) |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Webb Hooper, M. Racial/Ethnic Differences in Physiological Stress and Relapse among Treatment Seeking Tobacco Smokers. Int. J. Environ. Res. Public Health 2019, 16, 3090. https://doi.org/10.3390/ijerph16173090
Webb Hooper M. Racial/Ethnic Differences in Physiological Stress and Relapse among Treatment Seeking Tobacco Smokers. International Journal of Environmental Research and Public Health. 2019; 16(17):3090. https://doi.org/10.3390/ijerph16173090
Chicago/Turabian StyleWebb Hooper, Monica. 2019. "Racial/Ethnic Differences in Physiological Stress and Relapse among Treatment Seeking Tobacco Smokers" International Journal of Environmental Research and Public Health 16, no. 17: 3090. https://doi.org/10.3390/ijerph16173090
APA StyleWebb Hooper, M. (2019). Racial/Ethnic Differences in Physiological Stress and Relapse among Treatment Seeking Tobacco Smokers. International Journal of Environmental Research and Public Health, 16(17), 3090. https://doi.org/10.3390/ijerph16173090




