Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma
Abstract
1. Introduction
1.1. Problem of Interest
1.2. Lessons Learned from Prior Review
- (1)
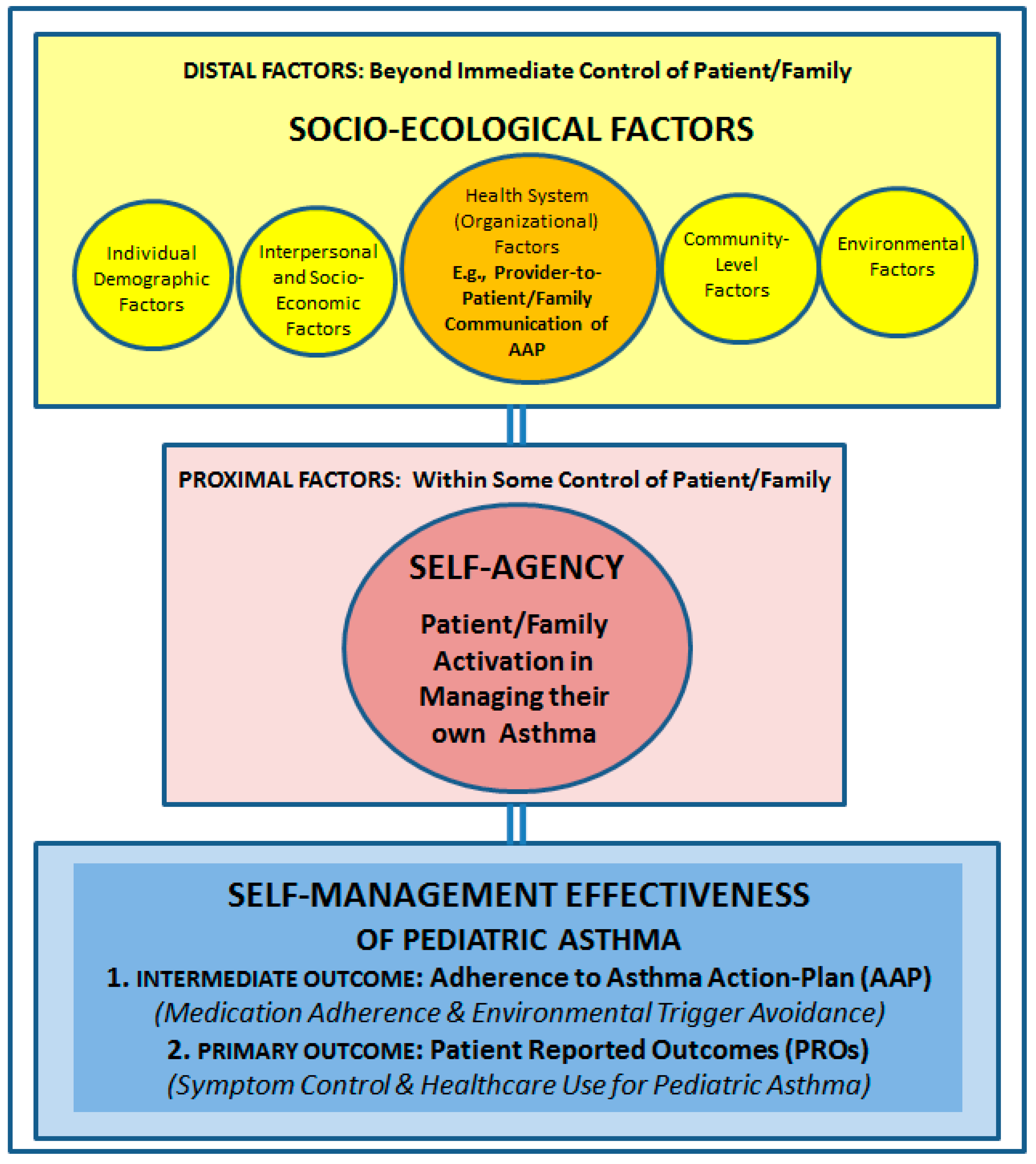
- Distal factors that are beyond the immediate control of the patient/family, and would include socio-ecological factors at various levels, e.g., individual factors (demographic & biologic characteristics, asthma severity-of-illness; health literacy); socio-economic factors (insurance coverage for asthma controller medications); community-level factors (support for self-management education in schools), etc.; and
- (2)
- Proximal factors that are within some control of the patient/family, and would include self-agency or patient/family activation in asthma management. The latter, in turn, would include behaviors and actions taken by the patient/family toward asthma management and control (e.g., regularly refilling prescription medications or refraining from exposure to tobacco smoke, to control irritant environmental triggers).
1.3. Need for the Current Review
1.4. Aims of This Paper
- 1)
- Conduct an integrative review of the literature to identify existing, validated measures of the key constructs and variables in the framework (summarized in Figure 1), with a view to operationalizing the framework.
- 2)
- Discuss implications of the operationalized framework for practice, policy, and research related to asthma management.
1.5. Special Relevance of the Holistic Framework to Pediatric Asthma
2. Methodology for the Integrative Review
- Literature on measures of provider-patient/family communication (stream #1);
- Literature on measures of patient/family activation (stream #2); and
- Literature on measures of self-management effectiveness of pediatric asthma (stream #3).
- Literature on measures of medication adherence (stream #3a);
- Literature on measures of environmental trigger avoidance (stream #3b); and
- Literature on measures of asthma symptom control (stream #3c).
2.1. Review Approach for Stream #1: Measures of Provider-Patient Communication
2.2. Review Approach for Stream #2: Measures of Patient Activation
2.3. Review Approach for Stream #3a: Measures of Medication Adherence
2.4. Review Approach for Stream #3b: Measures of Environmental Trigger Avoidance
2.5. Review Approach for Stream #3c: Measures of Asthma Symptom Control
3. Key Findings from the Integrative Review
3.1. Findings from Review of Measures of Provider-Patient Communication (Stream #1)
3.2. Findings from Review of Measures of Patient/Family Activation (Stream #2)
3.3. Findings from Review of Measures of Self-Management Effectiveness (Streams #3a, #3b, and #3c)
3.3.1. Intermediate Outcomes
3.3.2. Primary (Health) Outcomes
- Total number of encounters for pediatric asthma care, i.e., aggregate of outpatient visits (routine and sick), inpatient admissions (general admission and PICU), ED and urgent care visits for pediatric asthma care over a period of time, adjusted by the patient’s severity of illness.
- Total number of “non-revisits” for pediatric asthma outpatient care i.e., patient/families who do not return even once for outpatient care, over a six-month period following an initial visit, adjusted by the patient’s severity of illness.
- Total number of “no-shows” for pediatric asthma outpatient care, i.e., patient/families who do not show up for scheduled appointments for pediatric asthma outpatient care, adjusted by the patient’s severity of illness.
3.4. Drawing upon Established Measures for Other Socio-Ecological (Control) Variables in the Framework
- ○
- Individual demographic characteristics (e.g., age, gender, race, school attended and grade level, names of pharmacy and primary care physician, family history of asthma) and primary caregiver’s demographic characteristics (age, race, income, employment, insurance status, tobacco use, zip code, etc.) could be captured through patient surveys, and further supplemented/verified through medical record review in any research endeavor. Similarly, the health literacy of children with asthma and their families could be assessed using widely-used existing validated instruments: (1) Rapid Estimate of Adult Literacy in Medicine (REALM) or (Rapid Estimate of Adolescent Literacy in Medicine (REALM-Teen), (2) Single Item Literacy Screener (SILS), and (3) Newest Vital Sign (NVS) [68,69,70,71,72].
- ○
- Individual biological variables, such as asthma severity, could be defined using the EPR-3 asthma severity categorization framework, which, in turn, could be captured through patient surveys, and further verified through medical record review in any research endeavor [5].
- ○
- Interpersonal and socio-economic variables would be assessed using validated instruments like the Cohen Social Support Index and Holmes and Rahe Stress Scale; in addition to fact- based questions for families, e.g.: Has your insurance company denied coverage for your child’s asthma control or relief medications? Does your child live in: (1) one home; or (2) more than one home? [73,74,75].
- ○
- Health system variables. In addition to the QQPPI measures of physician-patient communication, health system (organizational) factors influencing asthma management could be assessed using validated National Asthma Survey (NAS) questions on Self-Management Education Received from Providers [63]. Examples from this survey include: Has your child’s primary care (or clinic doctor) ever: (1) shown you how to use your child’s inhaler? (2) taught you how to use your child’s peak flow meter to adjust his/her daily medications?
- ○
- Community-level variables, such as school support for asthma, could be assessed using validated questions from the CDC Healthy Schools initiative [76]. For example: (1) Does your school/daycare have a copy of your child’s AAP? (2) Does someone in your school/daycare give your child his/her controller medication?
- ○
- Environmental variables in turn, could be assessed using the “Environment Section” of the validated National Asthma Survey (NAS) [63]. A key relevant feature of this section within the NAS, is that it includes questions to distinguish between “environmental risk factors” beyond the control of patient/family (e.g., how old is your home?); and “environmental trigger control,” or actions within the control of patient/family (e.g., does anyone in your household smoke?).
3.5. Operationalizing the Holistic Framework
4. Discussion
4.1. Implications for Future Research
4.2. Implications for Practice and Policy
4.3. Limitations of the Review
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Asthma self-management education and environmental management: Approaches to enhancing reimbursement. In National Asthma Control Program; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2013. [Google Scholar]
- Akinbami, L. Asthma Prevalence, Health Care Use and Mortality: United States (2003–2005); CDC National Center for Health Statistics: Hyattsville, MD, USA, 2011.
- Young, H.N.; Larson, T.L.; Cox, E.D.; Moreno, M.A.; Thorpe, J.M.; MacKinnon, N.J. The Active Patient Role and Asthma Outcomes in an Underserved Rural Community. J. Rural Health 2014, 30, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Pinnock, H.; Epiphaniou, E.; Pearce, G.; Parke, H.; Greenhalgh, T.; Sheikh, A.; Griffiths, C.J.; Taylor, S.J. Implementing supported self-management for asthma: A systematic review and suggested hierarchy of evidence of implementation studies. BMC Med. 2015, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- NIH National Asthma Education & Prevention Program. Guidelines for the Diagnosis and Management of Asthma. Expert Panel Report 3; United States Department of Health and Human Services: Washington, DC, USA, 2007.
- The Joint Commission. Specification Manual for National Inpatient Quality Measures; The Joint Commission: Oakbrook Terrace, IL, USA, 2012. [Google Scholar]
- Sleath, B.; Carpenter, D.M.; Beard, A.; Gillette, C.; Williams, D.; Tudor, G.; Ayala, G.X. Child and caregiver reported problems in using asthma medications and question-asking during pediatric asthma visits. Int. J. Pharm. Pract. 2014, 22, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Young, H.N.; Kanchanasuwan, S.; Cox, E.D.; Moreno, M.M.; Havican, N.S. Barriers to medication use in rural underserved patients with asthma. Res. Soc. Adm. Pharm. 2015, 11, 909–914. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Unni, E.; Farris, K.B. Determinants of different types of medication non-adherence in cholesterol lowering and asthma maintenance medications: A theoretical approach. Patient Educ. Couns. 2011, 83, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Rangachari, P. A framework for measuring self-management effectiveness and healthcare use among pediatric asthma patients & families. J. Asthma Allergy 2017, 10, 111–122. [Google Scholar] [PubMed]
- Bender, B.; Milgrom, H. Non-adherence in asthmatic patients: Is there a solution to the problem? Asthma Immunol. 1997, 79, 177–185. [Google Scholar] [CrossRef]
- Brown, R. Behavioral issues in asthma management. Allergy Asthma Proced. 2001, 22, 67–69. [Google Scholar] [CrossRef]
- Conway, A. Adherence and compliance in the management of asthma. Br. J. Nurs. 1998, 7, 1313–1315. [Google Scholar] [CrossRef]
- Fish, L.; Lung, C.L. Adherence to asthma therapy annals of allergy. Ann. Allerg. Asthma Immunol. 2001, 86 (Suppl. 1), 24–30. [Google Scholar] [CrossRef]
- Trueman, J.K. Non-adherence to medication in asthma. Prof. Nurse 2000, 15, 583–586. [Google Scholar] [PubMed]
- Kolbe, J. The influence of socio-economic and psychological factors on patient adherence to self-management strategies: Lessons learned in asthma. Dis. Manag. Health Outcomes 2002, 10, 551–570. [Google Scholar] [CrossRef]
- Nuss, H.J.; Hester, L.L.; Perry, M.A.; Stewart-Briley, C.; Reagon, V.M.; Collins, P. Applying the social ecological model to creating asthma-friendly schools. J. Sch. Health 2016, 86, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Kralik, D.; Koch, T.; Price, K.; Howard, N. Chronic illness self-management: Taking action to create order. J. Clin. Nurs. 2004, 13, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, M.; Ekstrom, T.; Moller, M.; Ahlner, J. Asthma care and factors affecting medication compliance: The patients’ point of view. Int. J. Qual. Health Care 2001, 13, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, I. Patients are experts in their own field. BMJ 2003, 326, 1276. [Google Scholar] [CrossRef]
- Street, R.L., Jr.; Makoul, G.; Arora, N.K.; Epstein, R.M. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ. Couns. 2009, 74, 295–301. [Google Scholar] [CrossRef]
- Bender, B. Physician-patient communication as a tool that can change adherence. Ann. Allergy Asthma Immunol. 2009, 103, 1–2. [Google Scholar] [CrossRef]
- DiMatteo, M.R.; Sherbourne, C.D.; Hays, R.D.; Ordway, L.; Kravitz, R.L.; McGlynn, E.A.; Kaplan, S.; Rogers, W.H. Physicians characteristics influence patients adherence to medical treatment: Results from the medical outcomes study. Health Psychol. 1993, 12, 93–102. [Google Scholar] [CrossRef]
- Zolnierek, K.B.H.; DiMatteo, M.R. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009, 47, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Zandbelt, L.C.; Smets, E.M.; Oort, F.J.; Godfried, M.H.; Haes, H.C. Medical specialists’ patient-centered communication and patient-reported outcomes. Med. Care 2007, 45, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.W.; Head, A.J.; Rene, J. Patient decision-making related to anti-rheumatic drugs in rheumatoid arthritis: The importance of patient trust of physician. J. Rheumatol. 2008, 35, 618–624. [Google Scholar] [PubMed]
- Farber, H.J.; Capra, A.M.; Finkelstein, J.A. Misunderstanding of asthma controller medications: Association with non-adherence. J. Asthma 2003, 40, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Howell, G. Non-adherence to medical therapy in asthma: Risk factors, barriers, and strategies for improving. J. Asthma 2008, 45, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.R.; Strub, P.; Buist, A.S. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am. J. Respir. Crit. Care Med. 2010, 181, 566–577. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv. Res. 2004, 39, 1004–1026. [Google Scholar] [CrossRef] [PubMed]
- Day, J.; Bodmer, C.W.; Dunn, O.M. Development of a Questionnaire Identifying Factors Responsible for Successful Self-management of Insulin-Treated Diabetes. Diabet. Med. 1996, 13, 564–573. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Funnell, M.M.; Bonomi, A.E. Self-management Aspects of the Improving Chronic Illness Care Breakthrough Series: Implementation with Diabetes and Heart Failure Teams. Ann. Behav. Med. 2002, 24, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Boon, H.; Stewart, M. Patient-physician communication assessment instruments: 1986 to 1996 in review. Patient Educ. Couns. 1998, 35, 161–176. [Google Scholar] [CrossRef]
- Ong, L.M.; de Haes, J.C.; Hoos, A.M.; Lammes, F.B. Doctor-patient communication: A review of the literature. Soc. Sci. Med. 1995, 40, 903–918. [Google Scholar] [CrossRef]
- Zill, J.M.; Christalle, E.; Müller, E.; Härter, M.; Dirmaier, J.; Scholl, I. Measurement of Physician-Patient Communication—A Systematic Review. PLoS ONE 2014, 9, e112637. [Google Scholar] [CrossRef] [PubMed]
- DeCamp, L.R.; Showell, N.; Godage, S.K.; Leifheit, K.M.; Valenzuela-Araujo, D.; Shah, H.; Polk, S. Parent activation and pediatric primary care outcomes for vulnerable children: A mixed methods study. Patient Educ. Couns. 2019. [Google Scholar] [CrossRef] [PubMed]
- Prey, J.E.; Qian, M.; Restaino, S.; Hibbard, J.; Bakken, S.; Schnall, R.; Rothenberg, G.; Vawdrey, D.K.; Creber, R.M. Reliability and validity of the patient activation measure in hospitalized patients. Patient Educ. Couns. 2016, 99, 2026–2033. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef] [PubMed]
- Pearce, C.J.; Fleming, L. Adherence to medication in children and adolescents with asthma: Methods for monitoring and intervention. Expert Rev. Clin. Immunol. 2018, 14, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Downes, M.J.; Wisnivesky, J.P. Comprehensive environmental management of asthma and pediatric preventive care. Pediatric Allergy Immunol. 2011, 22, 277–282. [Google Scholar] [CrossRef]
- Alzahrani, Y.A.; Becker, E.A. Asthma control assessment tools. Respir. Care 2016, 61, 106–116. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; De Vet, H.C. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.; Bouter, L.M.; de Vet, H.C. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2012, 21, 651–657. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Zandbelt, L.C.; Smets, E.M.A.; Oort, F.J.; De Haes, H.C.J.M. Coding patient-centered behavior in the medical encounter. Soc. Sci. Med. 2005, 61, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Makoul, G. The SEGUE framework for teaching and assessing communication skills. Patient Educ. Couns. 2001, 45, 23–34. [Google Scholar] [CrossRef]
- Bieber, C.; Muller, K.G.; Nicolai, J.; Hartmann, M.; Eich, W. How does your doctor talk with you? Preliminary validation of a brief patient self-report questionnaire on the quality of physician-patient interaction. J. Clin. Psychol. Med. Settings 2010, 17, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Bieber, C.; Muller, K.G.; Blumenstiel, K. A shared decision-making communication training program for physicians treating fibromyalgia patients: Effects of a randomized controlled trial. J. Psychosom. Res. 2008, 64, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Bieber, C.; Muller, K.G.; Blumenstiel, K. Long-term effects of a shared decision making intervention on physician–patient interaction and outcome in fibromyalgia. A qualitative and quantitative one year follow-up of a randomized controlled trial. Patient Educ. Couns. 2006, 63, 357–366. [Google Scholar] [CrossRef]
- Mancuso, C.A.; Sayles, W.; Allegrante, J.P. Development and testing of the asthma self-management questionnaire. Ann. Allergy Asthma Immunol. 2009, 102, 294–302. [Google Scholar] [CrossRef]
- Staiger, J.G.; Jarvik, R.A.; Deyo, B. Brief report: Patient-physician agreement as a predictor of outcomes in patients with back pain. J. Gen. Intern. Med. 2005, 20, 935–937. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.A.; Dedrick, R.F. Development of the trust in physician scale—A measure to assess interpersonal trust in patient-physician relationships. Psychol. Rep. 1990, 67, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Riekert, K.A.; Borrelli, B.; Bilderback, A. The development of a motivational interviewing intervention to promote medication adherence among inner-city, African-American adolescents with asthma. Patient Educ. Couns. 2011, 82, 117–122. [Google Scholar] [CrossRef]
- Lerman, C.E.; Brody, D.S.; Caputo, G.C.; Smith, D.G.; Lazaro, C.G.; Wolfson, H.G. Patients’ Perceived Involvement in Care Scale: Relationship to attitudes about illness and medical care. J. Gen. Intern. Med. 1990, 5, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Wallston, K.A.; Stein, M.J.; Smith, C.A. Form C of the MHLC scales: A condition-specific measure of locus of control. J. Personal. Assess. 1994, 63, 534–553. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Mazonson, P.D.; Holman, H.R. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheumatol. 1993, 36, 439–446. [Google Scholar] [CrossRef] [PubMed]
- DiClemente, C.C. Motivational interviewing and the stages of change. In Motivational Interviewing: Preparing People to Change Addictive Behavior; Miller, W.R., Rollnick, S., Eds.; Guilford Press: New York, NY, USA, 1991; pp. 191–202. [Google Scholar]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.L.; Mann, D.M.; Wisnivesky, J.P.; Horne, R.; Leventhal, H.; Musumeci-Szabó, T.J.; Halm, E.A. Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: The medication adherence report scale for asthma. Ann. Allergy Asthma Immunol. 2009, 103, 325–331. [Google Scholar] [CrossRef]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M.; Ward, H.J. Predictive validity of a medication adherence measure in an outpatient setting. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef]
- National Center for Health Statistics State and Local Area Integrated Telephone Survey (SLAITS) National Asthma Survey. National Sample Specifications. Available online: https://www.cdc.gov/nchs/data/slaits/revised_nas2003_national_specs.pdf (accessed on 31 May 2014).
- Bloom, B.; Cohen, R.A. Summary health statistics for U.S. children: National Health Interview Survey, 2007. Vital Health Stat. 2007, 239, 1–80. [Google Scholar]
- Revicki, D.; Weiss, K. Clinical assessment of asthma symptom control: Review of current assessment instruments. J. Asthma 2006, 43, 481–487. [Google Scholar] [CrossRef]
- Nathan, R.A.; Sorkness, C.A.; Kosinski, M.; Schatz, M.; Li, J.T.; Marcus, P.; Murray, J.J.; Pendergraft, T.B. Development of the Asthma Control Test: A survey for assessing asthma control. J. Allergy Clin. Immunol. 2004, 113, 59–65. [Google Scholar] [CrossRef]
- Liu, A.H.; Zeiger, R.; Sorkness, C.; Mahr, T.; Ostrom, N.; Burgess, S.; Rosenzweig, J.C.; Manjunath, R. Development and cross-sectional validation of the Childhood Asthma Control Test. J. Allergy Clin. Immunol. 2007, 119, 817–825. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Roundtable on Health Literacy. An overview of measures of health literacy. In Measures of Health Literacy: Workshop Summary; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Murphy, P.W.; Davis, T.C.; Long, S.W.; Jackson, R.H.; Decker, B.C. Rapid Estimate of Adult Literacy in Medicine (REALM): A Quick Reading Test for Patients. J. Read. 1993, 37, 124–130. [Google Scholar]
- Davis, T.C.; Wolf, M.S.; Arnold, C.L. Development and Validation of the Rapid Estimate of Adolescent Literacy in Medicine (REALM-Teen): A Tool to Screen Adolescents for Below-Grade Reading in Health Care Settings. Pediatrics 2006, 118, e1707. [Google Scholar] [CrossRef] [PubMed]
- Morris, N.S.; MacLean, C.D.; Chew, L.D.; Littenberg, B. The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Fam. Pract. 2006, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick Assessment of Literacy in Primary Care: The Newest Vital Sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Cyranowski, J.M.; Zill, N.; Bode, R.; Butt, Z.; Kelly, M.A.; Pilkonis, P.A.; Salsman, J.M.; Cella, D. Assessing Social Support, Companionship, and Distress: NIH Toolbox Adult Social Relationship Scales. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2013, 32, 293–301. [Google Scholar] [CrossRef]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention Healthy Schools Initiative. Available online: https://www.cdc.gov/healthyschools/asthma/ (accessed on 20 October 2017).
- Young, H.N.; Rios, M.L.; Brown, R. How Does Patient-Provider Communication Influence Adherence to Asthma Medications? Patient Educ. Couns. 2017, 100, 696–702. [Google Scholar] [CrossRef]
| Stream # | Stream Name | Review Approach | Description |
|---|---|---|---|
| Stream #1 | Measures of Provider-Patient/Family Communication | Review of Systematic Reviews. | Review of all existing “systematic reviews” of “measures of physician-patient communication,” to identify existing validated measures for recommendation. Details of the review process are described in Section 2.1. |
| Stream #2 | Measures of Patient/Family Activation | Keyword search of stream #2 literature. | Keyword search of PubMed archives with inclusion/exclusion criteria to identify a final set of articles for review. Articles are reviewed with a view to identifying existing validated measures for recommendation. Details of the review process are described in Section 2.2. |
| Stream #3a | Measures of Medication Adherence | Keyword search of stream #3a literature. | Keyword search of PubMed archives with inclusion/exclusion criteria to identify a final set of articles for review. Articles are reviewed with a view to identifying existing validated measures for recommendation. Details of the review process are described in Section 2.3. |
| Stream #3b | Measures of Environmental Trigger Avoidance | Keyword search of stream #3b literature. | Keyword search of PubMed archives with inclusion/exclusion criteria to identify a final set of articles for review. Articles are reviewed with a view to identifying existing validated measures for recommendation. Details of the review process are described in Section 2.4. |
| Stream #3c | Measures of Asthma Symptom Control | Keyword search of stream #3c literature. | Keyword search of PubMed archives with inclusion/exclusion criteria to identify a final set of articles for review. Articles are reviewed with a view to identifying existing validated measures for recommendation. Details of the review process are described in Section 2.5. |
| Construct | Sub-Construct | Variable | Recommended Existing Validated Measure(s)/Instrument(s)/Question(s) |
|---|---|---|---|
| Socio-Ecological Factors | Individual Biologic & Demographic Characteristics | Asthma Severity | EPR-3 Asthma Severity Classification (1-Intermittent; 2-Mild-Persistent; 3-Moderate-Persistent; 4-Severe-Persistent) |
| Health Literacy | Rapid Estimate of Adult Literacy in Medicine (REALM) | ||
| REALM Teen | |||
| Single-Item Literacy Screener (SILS) | |||
| Newest Vital Sign (NVS) | |||
| Other Demographic characteristics | Miscellaneous validated questions to ascertain demographic characteristics | ||
| Socio-Ecological Factors | Interpersonal and Socio-economic Risk Factors | Social Support | Cohen Social Support Index |
| Stress | Holmes and Rahe Stress Assessment Instrument | ||
| Socio-Ecological Factors | Health System (Organizational Factors) | Provider-Patient/Family Communication | Questionnaire on Quality of Physician-Patient Communication (QQPPI) |
| Provider-Patient/Family Communication of Asthma Action Plan (AAP) | National Asthma Survey (NAS) questions related to asthma self-management education by providers | ||
| Immediate Outcomes of Provider-Patient/Family Communication | Asthma Self-Management Questionnaire (ASMQ); Trust in Provider Scale (TPS); Steigers’s Agreement Instrument; Perceived Involvement in Care Scale (PICS); Riekert Motivation Scale. | ||
| Socio-Ecological Factors | Community-Level Factors | School Support for Asthma Management | Centers for Disease Control and Prevention (CDC) Healthy Schools Questionnaire |
| Socio-Ecological Factors | Environmental-Level Factors | Indoor Environmental Air Quality | National Asthma Survey (NAS) section on Environmental Risk Factors |
| Self-Agency | Patient Activation | Patient/Family Activation in Asthma Management | Patient Activation Measure (PAM) |
| Self-Management Effectiveness of Pediatric Asthma | Asthma-Action Plan (AAP) Adherence | Adherence to Medication (Intermediate Outcome) | Morisky Medication Adherence Scale (MMAS) |
| Adherence to Environmental Trigger Controls (Intermediate Outcome) | National Asthma Survey (NAS) section on Environmental Trigger Control | ||
| Asthma Control | Asthma Symptom Control (Primary Outcome) | Child Asthma Control Test (CACT) | |
| Healthcare Use | Healthcare Visits for Pediatric Asthma (Primary Outcome) | Type of Visit for Pediatric Asthma Care:
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rangachari, P.; May, K.R.; Stepleman, L.M.; Tingen, M.S.; Looney, S.; Liang, Y.; Rockich-Winston, N.; Rethemeyer, R.K. Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma. Int. J. Environ. Res. Public Health 2019, 16, 3060. https://doi.org/10.3390/ijerph16173060
Rangachari P, May KR, Stepleman LM, Tingen MS, Looney S, Liang Y, Rockich-Winston N, Rethemeyer RK. Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma. International Journal of Environmental Research and Public Health. 2019; 16(17):3060. https://doi.org/10.3390/ijerph16173060
Chicago/Turabian StyleRangachari, Pavani, Kathleen R. May, Lara M. Stepleman, Martha S. Tingen, Stephen Looney, Yan Liang, Nicole Rockich-Winston, and R. Karl Rethemeyer. 2019. "Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma" International Journal of Environmental Research and Public Health 16, no. 17: 3060. https://doi.org/10.3390/ijerph16173060
APA StyleRangachari, P., May, K. R., Stepleman, L. M., Tingen, M. S., Looney, S., Liang, Y., Rockich-Winston, N., & Rethemeyer, R. K. (2019). Measurement of Key Constructs in a Holistic Framework for Assessing Self-Management Effectiveness of Pediatric Asthma. International Journal of Environmental Research and Public Health, 16(17), 3060. https://doi.org/10.3390/ijerph16173060





