3.4.2. Conditional Variables
Conditional variables include resource heterogeneity, governance structure and normative effectiveness. Specifically, resource heterogeneity is defined by the heterogeneity of service resources and technical resources. Governance structure is analyzed based on the balance between governmental control and internal control, as well as the balance between centralization and decentralization. Normative effectiveness is used to characterize the degree of normality of policy documents. The specific definition criteria are as follows:
Resource Heterogeneity
As shown in
Table 4, this study depicts resource heterogeneity based on the number of practitioners (including assistant practitioners), open sick beds, and available medical equipment. In the first place, we measure the heterogeneity of technical resources based on the configuration of medical equipment in an IHC, and this equipment will include ambulances, biochemical instruments, electrocardiograms, B-ultrasounds, color ultrasounds, X-ray machines, DR/CR, CT and MRI, etc. With reference to the previous research carried out by Teachman (1980) [
39] and Meyer and Goes (1988) [
40], the specific calculation formula is as follows:
Specifically, j represents medical devices owned by the ith hospital, Pij indicates the proportion of medical devices located in the ith hospital; LnI indicates the theoretical maximum value of entropy. According to the definition of entropy, which indicates the degree of internal chaos in a system, the more chaotic a system is, the more even its distribution. In other words, the smaller the value of entropy_techi, the greater the heterogeneity of technical resources.
In addition, this study measures heterogeneity of service resources based on the number of licensed physicians (including assistant practitioners) and open sick beds in the calculation formula described above. Then, Principal Component Analysis (PCA) is used to determine the variable of resource heterogeneity. This comprehensive indicator of resource heterogeneity is determined in order to achieve the required balance between the number of cases and the number of conditions [
38].
Subsequently, we calibrated the calculated value, which is a continuous value from 0 to 1, and set the full membership, the crossover point and the full non-membership threshold as 0.83, 0.73 and 0.57, respectively, after many attempts.
Governance Structure
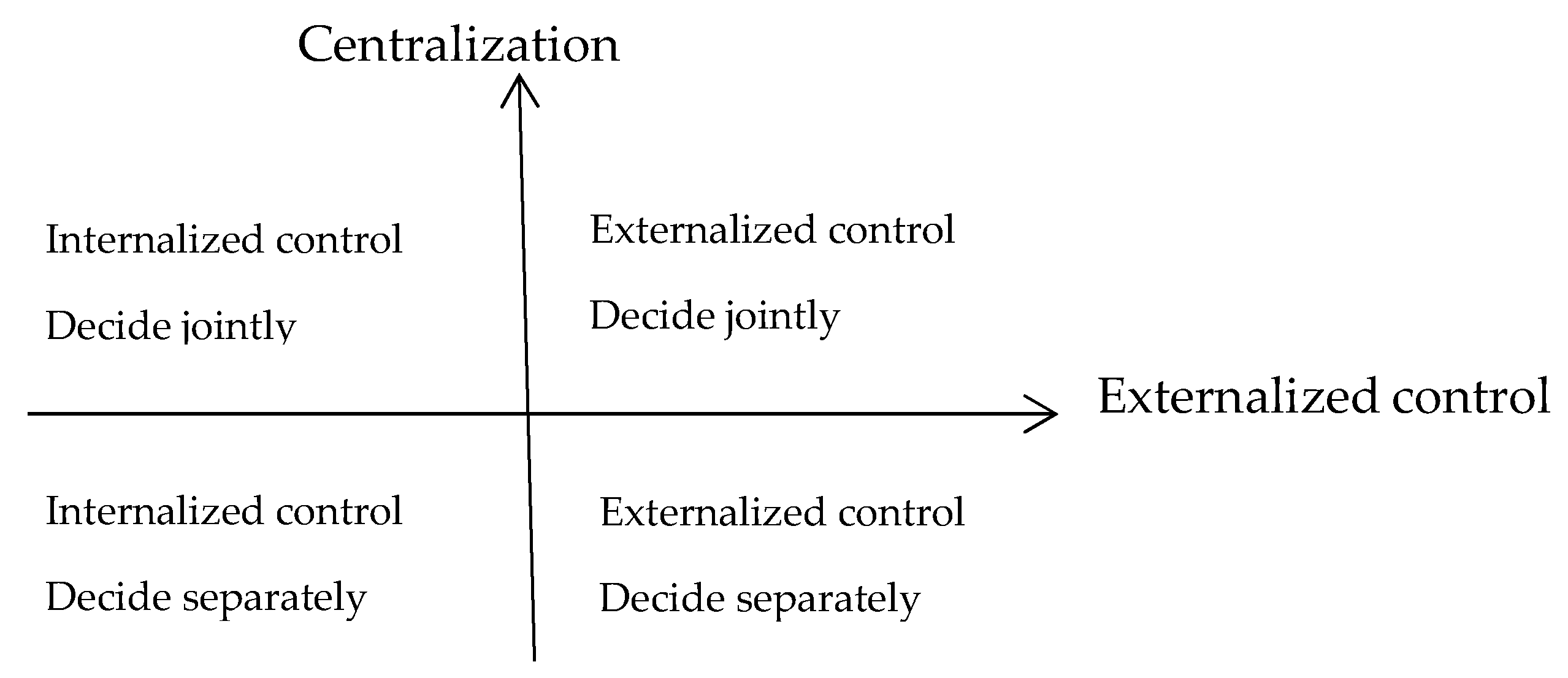
In this research, governance structure is defined in terms of the dimensions of governmental control and centralization. On the one hand, governmental control is primarily used to describe the manner in which local government affects the IHC at an organizational and fiscal level, and the extent of this intervention. In the context of a bureaucratic health system, health system reform is promoted by the health department and exhibits governmental control to some extent. In general, voluntary cooperative networks that are established among health service providers in a county are able to receive little if anything in the way of governmental support, and the governmental control over them is quite low. Actually, health system reform involves cooperation between the health department and related departments, such as the finance department and the human resources and social security department, and the administrative power of the health department is relatively limited. The administrative power of working groups led by main government officials (often referred to as the permanent member of a committee in China) is significantly stronger than that of the single health department. In addition, working groups led by the heads of county-level government have the strongest administrative power and are more likely to receive organizational and financial support. Therefore, a quartering method (“1/0.67/0.33/0”) is employed to portray the degree of governmental control.
On the other hand, centralization is inferred on the basis of the authority exercised by the leading hospital over the member organizations in terms of the allocation of human, financial and other resources. According to the “Guiding Opinions on Promoting the Construction of Grading Diagnosis and Treatment System”, the “Guiding Opinions on Promoting the Construction and Development of Integrated Healthcare” and related implementation plans that have been publicly released, most health service providers in IHCs have maintained their previous functions and responsibilities, and explored establishing cooperative relationships with medical businesses, management or interests. In fact, the power of management of human, financial and material resources over health service providers is limited. For instance, although the health authorities at the county level having explored the trasnferral of power over personnel to county-level hospitals (i.e., recommendation and recruitment power), some of them have retained the power to inspect and appoint the heads of the health service providers. In this case, the appointment power of the leading hospital over the health service providers is limited. Therefore, this research focuses on the analysis of the limited power to allocate and distribute human, financial and material resources among health service providers. Undoubtedly, the authority of the leading hospital over the member organizations varies by region and time. As shown in
Table 5, we also use the quartering method (“1/0.67/0.33/0”) to visualize the value of centralization within a specific time frame (
Table 5).
In terms of value, we see that governmental control of the working group led by the head of a county-level government presents greater effectiveness than the other two working groups, and governmental control in a voluntary cooperative network is the least effective. Therefore, governmental control of the working group led by the head of county-level government is scored as “1”, the control in a voluntary cooperative network is scored as “0”, and control such as in the other two working groups are scored as “0.67” and “0.33”, respectively. The scoring of Centralization is identical to that of Governmental Control.
Normative Effectiveness
According to institutional theory, regularity, normality and cultural cognition constitute the three basic elements of normative effectiveness, which affects to a large extent the selection of organizational mode; furthermore, the normative effectiveness of policy documents can be analyzed based on policy texts. In accordance with the “Notice of the General Office of the Chinese State Council on Strengthening the Formulation, Supervision and Management of Administrative Normative Documents” (State Council 2018, No. 37), internal institutions of governmental departments are not allowed to issue normative documents, and administrative normative documents that have not been publicly released shall not be used as the basis on which to enforce administrative law. To this end, this article analyzes the normative effectiveness via a text analysis of the health policy documents issued by county-level governments, and we ensured that the selected documents had been publicly issued. (Although policy texts in XCS/XNX/XLY/XTJ are issued by the health departments, these are publicly issued policy documents. In addition, because of the lack of policy texts issued by the county-level government, the analysis of these documents is regarded as acceptable.)
The existing literature studying the effectiveness of policy texts generally analyzes the normative effectiveness of policy documents by calculating the occurrence of specified restrictive words, such as prohibition (forbidden), necessity, no, should, norms, regulations, standards, etc. [
41]. In the coding phase, we adopted the above-mentioned method and tried to ascertain the membership of the selected samples on the basis of the proportion of regulatory elements, normative elements and cultural-cognitive elements in the institutional elements. Based on this textual analysis, we found that most implementation plans are led by regulatory and normative elements, and that the occurrence of these elements varies from county to county. Therefore, this study defines the degree of normativity of sample cases with reference to the occurrence of regulatory and normative elements in the policy text, setting thresholds for normative effectiveness based on many attempts and with reference to an extensive database of our related research. The normative effectiveness of the sample case is calibrated by the occurrence of specified restrictive words. Specifically, when the occurrence is no less than 22, it will be calibrated as “1”, signaling full membership, and when the occurrence is below 8, it will be calibrated as “0”, denoting full non-membership. Furthermore, the crossover point is set as 15 in order to ascertain the sample cases’ normative effectiveness.
In conclusion, in accordance with the analytical requirements of fsQCA, the selected 15 IHC samples are measured (see
Table 4 and
Table 5), and the resulting data matrix (in light of the definition of entropy, the greater the RH value, the lower the degree of resource heterogeneity; by this logic, the greater the calibrated RH value, the lower the degree of resource heterogeneity) is shown in
Appendix B.