Health-Related Participatory Research in American Indian and Alaska Native Communities: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview of Scoping Review Methodology
2.2. Research Team
2.3. Research Question and Purpose
- RQ1: What is the character and extent of community engagement in research in health-related PR involving AIAN communities?
- RQ2: What tools for guiding and regulating research at the community level are employed in health-related PR involving AIAN communities?
- RQ3: How is cultural adaptation employed in health-related PR involving AIAN communities?
- RQ4: What activities related to development of community research capacity are undertaken in health-related PR involving AIAN communities?
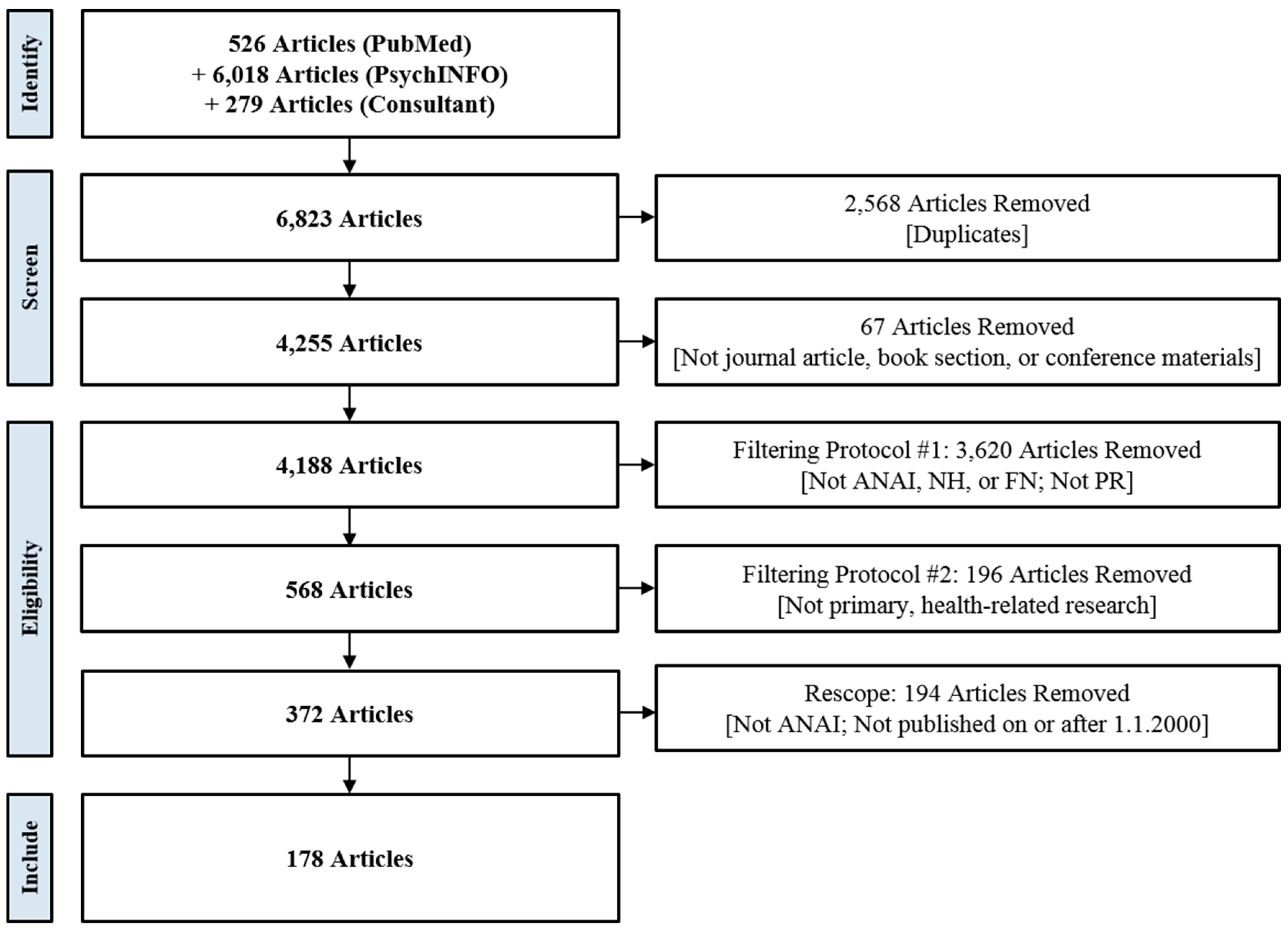
2.4. Search Strategy
2.5. Article Selection
2.6. Data Extraction
2.7. Consultation
3. Results
3.1. Overview of Health-Related PR in AIAN Communities
3.2. Community Engagement in the Research Process
3.2.1. Initiation
3.2.2. Funding
3.2.3. Research Question and Study Aims
3.2.4. Administration
3.2.5. Design, Methods, and Approach
3.2.6. Protocols
3.2.7. Meetings and Events
3.2.8. Data Collection and Analysis
3.2.9. Intervention
3.2.10. Dissemination
3.3. Community Guidance and Tribal Regulation of Research
3.3.1. Community Advisory Groups
3.3.2. Tribal Mechanisms for Regulating Research
3.4. Cultural Adaptation
3.4.1. Study Design
3.4.2. Study Protocols
3.4.3. Interventions
3.4.4. Dissemination Methods and Products
3.5. Capacity Building and Co-learning
3.5.1. Developing Community Capacity to Regulate Research
3.5.2. Developing Community Capacity to Conduct Research
3.5.3. Paid Employment
3.5.4. Researcher Co-learning
4. Discussion
4.1. Research Recommendations
- How do community values and norms, as well as community resources and infrastructure, affect the acceptability and feasibility of different study designs and objectives?
- Do various PR approaches differentially affect project timelines and costs, participation and retention rates, or the effectiveness of an intervention?
- How do different strategies for adapting PR approaches and evidence-based interventions to the needs of individual communities compare to one another in terms of ease of application and impact on outcomes?
- What is the perspective of community stakeholders on the costs and benefits of different PR approaches and the relative importance of the various components of those approaches?
4.2. Practice Recommendations
4.3. Policy Recommendations
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cargo, M.; Mercer, S.L. The value and challenges of participatory research: Strengthening its practice. Annu. Rev. Public Health 2008, 29, 325–350. [Google Scholar] [CrossRef] [PubMed]
- Macaulay, A.C. Participatory research: What is the history? Has the purpose changed? Fam. Pract. 2016, 34, 256–258. [Google Scholar] [CrossRef] [PubMed]
- Baum, F.; MacDougall, C.; Smith, D. Participatory action research. J. Epidemiol. Community Health 2006, 60, 854–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Educ. Health 2001, 14, 182–197. [Google Scholar]
- Wallerstein, N.; Duran, B.; Oetzel, J.; Minkler, M. Community-Based Participatory Research for Health: Advancing Social and Health Equity; John Wiley & Sons: Hoboken, NJ, USA, 2017. [Google Scholar]
- Fisher, P.A.; Ball, T.J. Tribal participatory research: Mechanisms of a collaborative model. Am. J. Community Psychol. 2003, 32, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Letiecq, B.L.; Bailey, S.J. Evaluating from the outside: Conducting Cross-Cultural Evaluation Research on an American Indian Reservation. Eval. Rev. 2004, 28, 342–357. [Google Scholar] [CrossRef] [PubMed]
- Mariella, P.; Brown, E.; Carter, M.; Verri, V. Tribally-Driven Participatory Research: State of the practice and potential strategies for the future. J. Health Disparities Res. Pract. 2009, 3, 41–58. [Google Scholar]
- DOI Bureau of Indian Affairs-Frequently Asked Questions. Available online: https://www.bia.gov/frequently-asked-questions (accessed on 22 July 2019).
- Department of Justice. Department of Justice Policy on Indian Sovereignty and Government-To-Government Relations with Indian Tribes. 1995. Available online: https://www.hsdl.org/?abstract&did=468520 (accessed on 16 August 2019).
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing Partnership Approaches to Improve Public Health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef]
- Foulks, E.F. Misalliances in the Barrow Alcohol Study. Am. Indian Alsk. Native Ment. Health Res. (Online) 1989, 2, 7–17. [Google Scholar] [CrossRef]
- Mello, M.M.; Wolf, L.E. The Havasupai Indian tribe case—lessons for research involving stored biologic samples. New Engl. J. Med. 2010, 363, 204–207. [Google Scholar] [CrossRef]
- Goins, R.T.; Garroutte, E.M.; Fox, S.L.; Dee Geiger, S.; Manson, S.M. Theory and practice in participatory research: Lessons from the Native Elder Care Study. Gerontologist. 2011, 51, 285–294. [Google Scholar] [CrossRef]
- Davis, S.M.; Reid, R. Practicing participatory research in American Indian communities. Am. J. Clin. Nutr. 1999, 69, 755–759. [Google Scholar] [CrossRef]
- Jernigan, V.B. Community-based participatory research with Native American communities: The Chronic Disease Self-Management Program. Health Promot. Pract. 2010, 11, 888–899. [Google Scholar] [CrossRef]
- Roberts, E.B.; Jette, S.L. Implementing participatory research with an urban American Indian community: Lessons learned. Health Educ. J. 2016, 75, 158–169. [Google Scholar] [CrossRef]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. Bmc Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- NIH Report. Project Information: Center on American Indian and Alaska Native Genomic Research. Available online: https://projectreporter.nih.gov/project_info_description.cfm?aid=9274374&icde=38507418&ddparam=&ddvalue=&ddsub=&cr=3&csb=default&cs=ASC&pball. (accessed on March 9th 2019).
- Hiratsuka, V.Y.; Beans, J.A.; Reedy, J.; Yracheta, J.M.; Peercy, M.T.; Saunkeah, B.R.; Woodbury, R.B.; O’Leary, M.; Spicer, P. Fostering Ethical, Legal, and Social Implications Research in Tribal Communities – The Center for the Ethics of Indigenous Genomic Research. J. Empir. Res. Human Res. Ethics. Forthcoming.
- Rink, E.; FourStar, K.; Elk, J.M.; Dick, R.; Jewett, L.; Gesink, D. Pregnancy prevention among American Indian men ages 18-24: The role of mental health and intervention to use birth control. Am. Indian Alsk. Native Ment. Health Res. 2012, 19, 57–75. [Google Scholar] [CrossRef]
- Daley, C.M.; James, A.S.; Ulrey, E.; Joseph, S.; Talawyma, A.; Choi, W.S.; Greiner, K.A.; Coe, M.K. Using focus groups in community-based participatory research: Challenges and resolutions. Qual. Health Res. 2010, 20, 697–706. [Google Scholar] [CrossRef]
- Margalit, R.; Watanabe-Galloway, S.; Kennedy, F.; Lacy, N.; Red Shirt, K.; Vinson, L.; Kills Small, J. Lakota elders’ views on traditional versus commercial/addictive tobacco use; oral history depicting a fundamental distinction. J. Community Health 2013, 38, 538–545. [Google Scholar] [CrossRef]
- Komro, K.A.; Wagenaar, A.C.; Boyd, M.; Boyd, B.J.; Kominsky, T.; Pettigrew, D.; Tobler, A.L.; Lynne-Landsman, S.D.; Livingston, M.D.; Livingston, B.; et al. Prevention trial in the Cherokee Nation: Design of a randomized community trial. Prev. Sci. 2015, 16, 291–300. [Google Scholar] [CrossRef]
- Tingey, L.; Strom, R.; Hastings, R.; Parker, A.; Barlow, A.; Rompalo, A.; Gaydos, C. Self-administered sample collection for screening of sexually transmitted infection among reservation-based American Indian youth. Int. J. Std Aids 2015, 26, 661–666. [Google Scholar] [CrossRef]
- Johnson, C.V.; Bartgis, J.; Worley, J.A.; Hellman, C.M.; Burkhart, R. Urban Indian voices: A community-based participatory research health and needs assessment. Am. Indian Alsk. Native Ment. Health Res. 2010, 17, 49–70. [Google Scholar] [CrossRef]
- Simonds, V.W.; Christopher, S.; Sequist, T.D.; Colditz, G.A.; Rudd, R.E. Exploring patient-provider interactions in a Native American community. J. Health Care Poor Underserved 2011, 22, 836–852. [Google Scholar] [CrossRef]
- Newman, S.; Cheng, T.; Ghahate, D.M.; Bobelu, J.; Sandy, P.; Faber, T.; Shah, V.O. Assessing knowledge and attitudes of diabetes in Zuni Indians using a culture-centered approach. PLoS ONE 2014, 9, e99614. [Google Scholar] [CrossRef]
- Filippi, M.K.; James, A.S.; Brokenleg, S.; Talawyma, M.; Perdue, D.G.; Choi, W.S.; Greiner, K.A.; Daley, C.M. Views, barriers, and suggestions for colorectal cancer screening among american Indian women older than 50 years in the midwest. J. Prim. Care Community Health 2013, 4, 160–166. [Google Scholar] [CrossRef]
- Fahrenwald, N.L.; Belitz, C.; Keckler, A. Outcome evaluation of ‘sharing the gift of life’: An organ and tissue donation educational program for American Indians. Am. J. Transplant. 2010, 10, 1453–1459. [Google Scholar] [CrossRef]
- Adams, A.K.; Scott, J.R.; Prince, R.; Williamson, A. Using community advisory boards to reduce environmental barriers to health in American Indian communities, Wisconsin, 2007–2012. Prev. Chronic Dis. 2014, 11, E160. [Google Scholar] [CrossRef]
- Gilder, D.A.; Luna, J.A.; Roberts, J.; Calac, D.; Grube, J.W.; Moore, R.S.; Ehlers, C.L. Usefulness of a survey on underage drinking in a rural American Indian community health clinic. Am. Indian Alsk. Native Ment. Health Res. 2013, 20, 1–26. [Google Scholar] [CrossRef]
- English, K.C.; Wallerstein, N.; Chino, M.; Finster, C.E.; Rafelito, A.; Adeky, S.; Kennedy, M. Intermediate outcomes of a tribal community public health infrastructure assessment. Ethn. Dis. 2004, 14, S61–S69. [Google Scholar]
- Johansson, P.; Knox-Nicola, P.; Schmid, K. The Waponahki Tribal Health Assessment: Successfully using CBRP to conduct a comprehensive and baseline health assessment of Waponahki tribal members. J. Health Care Poor Underserved 2015, 26, 889–907. [Google Scholar] [CrossRef]
- Mohammed, S.A.; Walters, K.L.; LaMarr, J.; Evans-Campbell, T.; Fryberg, S. Finding middle ground: Negotiating university and tribal community interests in community-based participatory research. Nurs. Inq. 2012, 19, 116–127. [Google Scholar] [CrossRef]
- Piontkowski, S.R.; Peabody, J.S.; Reede, C.; Velascosoltero, J.; Tsatoke, G., Jr.; Shelhamer, T.; Hicks, K.R. Reducing Motor Vehicle-Related Injuries at an Arizona Indian Reservation: Ten Years of Application of Evidence-Based Strategies. Glob. Healthscience Pract. 2015, 3, 619–629. [Google Scholar] [CrossRef] [Green Version]
- Redwood, D.; Lanier, A.; Kemberling, M.; Klejka, J.; Sylvester, I.; Lundgren, K. Community-based participatory research in a large cohort study of chronic diseases among Alaska native adults. Prog. Community Health Partnersh. 2010, 4, 325–330. [Google Scholar]
- Thurman, P.J.; Allen, J.; Deters, P.B. The circles of care: Doing participatory evaluation with American Indian and Alaska Native communities. Am. Indian Alsk. Native Ment. Health Res. 2004, 11, 139–154. [Google Scholar] [CrossRef]
- Richards, J.; Mousseau, A. Community-based participatory research to improve preconception health among Northern Plains American Indian adolescent women. Am. Indian Alsk. Native Ment. Health Res. 2012, 19, 154–185. [Google Scholar] [CrossRef]
- Richmond, L.S.; Peterson, D.J.; Betts, S.C. The evolution of an evaluation: A case study using the tribal participatory research model. Health Promot. Pract. 2008, 9, 368–377. [Google Scholar] [CrossRef]
- Manson, S.M.; Garroutte, E.; Goins, R.T.; Henderson, P.N. Access, relevance, and control in the research process: Lessons from Indian country. J. Aging Health 2004, 16, 58S–77S. [Google Scholar] [CrossRef]
- Petersen, D.M.; Minkler, M.; Vasquez, V.B.; Kegler, M.C.; Malcoe, L.H.; Whitecrow, S. Using community-based participatory research to shape policy and prevent lead exposure among Native American children. Prog. Community Health Partnersh. 2007, 1, 249–256. [Google Scholar] [CrossRef]
- Daley, C.M.; Greiner, K.A.; Nazir, N.; Daley, S.M.; Solomon, C.L.; Braiuca, S.L.; Smith, T.E.; Choi, W.S. All Nations Breath of Life: Using community-based participatory research to address health disparities in cigarette smoking among American Indians. Ethn. Dis. 2010, 20, 334–338. [Google Scholar]
- Christopher, S.; Watts, V.; McCormick, A.K.; Young, S. Building and maintaining trust in a community-based participatory research partnership. Am. J. Public Health 2008, 98, 1398–1406. [Google Scholar] [CrossRef]
- Mullany, B.; Barlow, A.; Neault, N.; Billy, T.; Jones, T.; Tortice, I.; Lorenzo, S.; Powers, J.; Lake, K.; Reid, R.; et al. The Family Spirit Trial for American Indian teen mothers and their children: CBPR rationale, design, methods and baseline characteristics. Prev. Sci. 2012, 13, 504–518. [Google Scholar] [CrossRef]
- Rasmus, S.; Allen, J.; Connor, W.; Freeman, W.; Skewes, M. Native Transformations in the Pacific Northwest: A strength-based model of protection against substance use disorder. Am. Indian Alsk. Native Ment. Health Res. 2016, 23, 158–186. [Google Scholar] [CrossRef]
- Whitesell, N.R.; Sarche, M.; Trucksess, C. The survey of well-being of young children: Results of a feasibility study with American Indian and Alaska Native communities. Infant Ment. Health J. 2015, 36, 483–505. [Google Scholar] [CrossRef]
- Coe, K.; Wilson, C.; Eisenberg, M.; Attakai, A.; Lobell, M. Creating the environment for a successful community partnership. Cancer 2006, 107, 1980–1986. [Google Scholar] [CrossRef]
- Verney, S.P.; Avila, M.; Espinosa, P.R.; Cholka, C.B.; Benson, J.G.; Baloo, A.; Pozernick, C.D. Culturally sensitive assessments as a strength-based approach to wellness in Native communities: A community-based participatory research project. Am. Indian Alsk. Native. Ment. Health Res. 2016, 23, 271–292. [Google Scholar] [CrossRef]
- Berns, R.M.; Tomayko, E.J.; Cronin, K.A.; Prince, R.J.; Parker, T.; Adams, A.K. Development of a culturally informed child safety curriculum for American Indian families. J. Prim. Prev. 2017, 38, 195–205. [Google Scholar] [CrossRef]
- Cruz, T.H.; Davis, S.M.; FitzGerald, C.A.; Canaca, G.F.; Keane, P.C. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in rural American Indian and Hispanic children. J. Prim. Prev. 2014, 35, 135–149. [Google Scholar] [CrossRef]
- Stiffman, A.; Brown, E.; Striley, C.W.; Ostmann, E.; Chowa, G. Cultural and ethical issues concerning research on American Indian youth. Ethics Behav. 2005, 15, 1–14. [Google Scholar] [CrossRef]
- Allen, J.; Mohatt, G.V.; Rasmus, S.M.; Hazel, K.L.; Thomas, L.; Lindley, S. The tools to understand: Community as co-researcher on culture-specific protective factors for Alaska Natives. J. Prev. Interv. Community 2006, 32, 41–59. [Google Scholar] [CrossRef]
- Armstrong, D.L. A community diabetes education and gardening project to improve diabetes care in a Northwest American Indian tribe. Diabetes Educ. 2000, 26, 113–120. [Google Scholar] [CrossRef]
- Bastida, E.M.; Tseng, T.-S.; McKeever, C.; Jack, L. Ethics and community-based participatory research: Perspectives from the field. Health Promot. Pract. 2010, 11, 16–20. [Google Scholar] [CrossRef]
- Burhansstipanov, L.; Krebs, L.U.; Harjo, L.; Watanabe-Galloway, S.; Pingatore, N.; Isham, D.; Duran, F.T.; Denny, L.; Lindstrom, D.; Crawford, K. Providing community education: Lessons learned from Native Patient Navigators. J. Cancer Educ. 2014, 29, 596–606. [Google Scholar] [CrossRef]
- Montgomery, M.; Manuelito, B.; Nass, C.; Chock, T.; Buchwald, D. The Native Comic Book Project: Native youth making comics and healthy decisions. J. Cancer Educ. 2012, 27, S41–S46. [Google Scholar] [CrossRef]
- Cueva, M.; Kuhnley, R.; Revels, L.; Schoenberg, N.E.; Dignan, M. Digital storytelling: A tool for health promotion and cancer awareness in rural Alaskan communities. Int. J. Circumpolar Health 2015, 74. [Google Scholar] [CrossRef]
- Kegler, M.C.; Malcoe, L.H.; Fedirko, V. Primary prevention of lead poisoning in rural Native American children: Behavioral outcomes from a community-based intervention in a former mining region. Fam. Community Health 2010, 33, 32–43. [Google Scholar] [CrossRef]
- Brown, B.D.; Harris, K.J.; Harris, J.L.; Parker, M.; Ricci, C.; Noonan, C. Translating the diabetes prevention program for Northern Plains Indian youth through community-based participatory research methods. Diabetes Educ. 2010, 36, 924–935. [Google Scholar] [CrossRef]
- Beals, J.; Manson, S.M.; Mitchell, C.M.; Spicer, P.; Team, A.-S. Cultural specificity and comparison in psychiatric epidemiology: Walking the tightrope in American Indian research. Cult. Med. Psychiatry 2003, 27, 259–289. [Google Scholar] [CrossRef]
- Chadwick, J.Q.; Copeland, K.C.; Daniel, M.R.; Erb-Alvarez, J.A.; Felton, B.A.; Khan, S.I.; Saunkeah, B.R.; Wharton, D.F.; Payan, M.L. Partnering in research: A national research trial exemplifying effective collaboration with American Indian Nations and the Indian Health Service. Am. J. Epidemiol. 2014, 180, 1202–1207. [Google Scholar] [CrossRef]
- Garwick, A.W.; Auger, S. Participatory action research: The Indian Family Stories Project. Nurs. Outlook 2003, 51, 261–266. [Google Scholar] [CrossRef]
- Belkora, J.; Franklin, L.; O’Donnell, S.; Ohnemus, J.; Stacey, D. Adaptation of consultation planning for Native American and Latina women with breast cancer. J. Rural Health 2009, 25, 384–387. [Google Scholar] [CrossRef]
- Ravenscroft, J.; Schell, L.M.; Cole, T. Applying the community partnership approach to human biology research. Am. J. Hum. Biol. 2015, 27, 6–15. [Google Scholar] [CrossRef]
- Katz, J.R.; Martinez, T.; Paul, R. Community-based participatory research and American Indian/Alaska native nurse practitioners: A partnership to promote adolescent health. J. Am. Acad. Nurse Pract. 2011, 23, 298–304. [Google Scholar] [CrossRef]
- Schmidt-Grimminger, D.; Frerichs, L.; Black Bird, A.E.; Workman, K.; Dobberpuhl, M.; Watanabe-Galloway, S. HPV knowledge, attitudes, and beliefs among Northern Plains American Indian adolescents, parents, young adults, and health professionals. J. Cancer Educ. 2013, 28, 357–366. [Google Scholar] [CrossRef]
- Horn, K.; McCracken, L.; Dino, G.; Brayboy, M. Applying community-based participatory research principles to the development of a smoking-cessation program for American Indian teens: “Telling our story”. Health Educ. Behav. 2008, 35, 44–69. [Google Scholar] [CrossRef]
- Goodkind, J.R.; Gorman, B.; Hess, J.M.; Parker, D.P.; Hough, R.L. Reconsidering culturally competent approaches to American Indian healing and well-being. Qual. Health Res. 2015, 25, 486–499. [Google Scholar] [CrossRef]
- Tingey, L.; Cwik, M.F.; Goklish, N.; Larzelere-Hinton, F.; Lee, A.; Suttle, R.; Walkup, J.T.; Barlow, A. Risk pathways for suicide among Native American adolescents. Qual. Health Res. 2014, 24, 1518–1526. [Google Scholar] [CrossRef]
- Weidmer-Ocampo, B.; Johansson, P.; Dalpoas, D.; Wharton, D.; Darby, C.; Hays, R.D. Adapting CAHPS for an American Indian population. J. Health Care Poor Underserved 2009, 20, 695–712. [Google Scholar] [CrossRef]
- Weiner, D.; Canales, M. “It Is Not Just Diabetes”: Engaging Ethnographic Voices to Develop Culturally Appropriate Health Promotion Efforts. Am. Indian Cult. Res. J. 2014, 38, 73–100. [Google Scholar]
- Allen, J.; Mohatt, G.V.; Fok, C.C.T.; Henry, D.; Burkett, R. A protective factors model for alcohol abuse and suicide prevention among Alaska Native youth. Am. J. Community Psychol. 2014, 54, 125–139. [Google Scholar] [CrossRef]
- Radin, S.M.; Kutz, S.H.; Lamarr, J.; Vendiola, D.; Vendiola, M.; Wilbur, B.; Thomas, L.R.; Donovan, D.M. Community perspectives on drug/alcohol use, concerns, needs, and resources in four Washington State Tribal communities. J. Ethn. Subst. Abuse 2015, 14, 29–58. [Google Scholar] [CrossRef]
- Kaufman, C.E.; Whitesell, N.R.; Keane, E.M.; Desserich, J.A.; Giago, C.; Sam, A.; Mitchell, C.M. Effectiveness of Circle of Life, an HIV-preventive intervention for American Indian middle school youths: A group randomized trial in a Northern Plains tribe. Am. J. Public Health 2014, 104, e106–e112. [Google Scholar] [CrossRef]
- Fleischhacker, S.; Vu, M.; Ries, A.; McPhail, A. Engaging tribal leaders in an American Indian healthy eating project through modified talking circles. Fam. Community Health: J. Health Promot. Maint. 2011, 34, 202–210. [Google Scholar] [CrossRef]
- Gibson, G.; Martin, J.; Zoe, J.B.; Edwards, K.; Gibson, N. Setting our minds to it: Community-centred research for health policy development in Northern Canada. Pimatisiwin: A J. Aborig. Indig. Community Health 2007, 5. [Google Scholar]
- English, K.C.; Fairbanks, J.; Finster, C.E.; Rafelito, A.; Luna, J.; Kennedy, M. A socioecological approach to improving mammography rates in a tribal community. Health Educ. Behav. 2008, 35, 396–409. [Google Scholar] [CrossRef]
- Rink, E.; FourStar, K.; Elk, J.M.; Dick, R.; Jewett, L.; Gesink, D. Young Native American men and their intention to use family planning services. Am. J. Men’s Health 2012, 6, 324–330. [Google Scholar] [CrossRef]
- Smith, A.; Christopher, S.; McCormick, A.K. Development and implementation of a culturally sensitive cervical health survey: A community-based participatory approach. Women Health 2004, 40, 67–86. [Google Scholar] [CrossRef]
- Getrich, C.M.; Sussman, A.L.; Campbell-Voytal, K.; Tsoh, J.Y.; Williams, R.L.; Brown, A.E.; Potter, M.B.; Spears, W.; Weller, N.; Pascoe, J.; et al. Cultivating a cycle of trust with diverse communities in practice-based research: A report from PRIME net. Ann. Fam. Med. 2013, 11, 550–558. [Google Scholar] [CrossRef]
- Pearson, C.R.; Parker, M.; Fisher, C.B.; Moreno, C. Capacity building from the inside out: Development and evaluation of a CITI ethics certification training module for American Indian and Alaska Native community researchers. J. Empir. Res. Hum. Res. Ethics 2014, 9, 46–57. [Google Scholar] [CrossRef]
- Stoddart, M.L.; Jarvis, B.; Blake, B.; Fabsitz, R.R. Recruitment of American Indians in epidemiologic research: The strong heart study. Am. Indian Alsk. Nativ. Ment. Health Res. 2000, 9, 20. [Google Scholar] [CrossRef]
- Filippi, M.K.; McCloskey, C.; Williams, C.; Bull, J.W.; Choi, W.S.; Greiner, K.A.; Daley, C.M. Perceptions, barriers, and suggestions for creation of a tobacco and health website among American Indian/Alaska Native college students. J. Community Health: Publ. Health Promot. Dis. Prev. 2013, 38, 486–491. [Google Scholar] [CrossRef]
- Friesen, B.J.; Cross, T.L.; Jivanjee, P.; Thirstrup, A.; Bandurraga, A.; Gowen, L.K.; Rountree, J. Meeting the transition needs of urban American Indian/Alaska Native youth through culturally based services. J. Behav. Health Serv. Res. 2015, 42, 191–205. [Google Scholar] [CrossRef]
- Rivkin, I.; Trimble, J.; Lopez, E.D.; Johnson, S.; Orr, E.; Allen, J. Disseminating research in rural Yup’ik communities: Challenges and ethical considerations in moving from discovery to intervention development. Int J Circumpolar Health 2013, 72. [Google Scholar] [CrossRef]
- Lowe, J.; Liang, H.; Riggs, C.; Henson, J.; Elder, T. Community partnership to affect substance abuse among Native American adolescents. Am. J. Drug Alcohol Abus. 2012, 38, 450–455. [Google Scholar] [CrossRef]
- Markus, S.F. Photovoice for healthy relationships: Community-based participatory HIV prevention in a rural American Indian community. Am. Indian Alsk. Native Ment. Health Res. 2012, 19, 102–123. [Google Scholar] [CrossRef]
- Rasmus, S.M.; Charles, B.; Mohatt, G.V. Creating Qungasvik (a Yup’ik intervention “toolbox”): Case examples from a community-developed and culturally-driven intervention. Am. J. Community Psychol. 2014, 54, 140–152. [Google Scholar] [CrossRef]
- Cordova, F.M.; Joshweseoma, L.; Teufel-Shone, N.I.; Coe, K. Using a Community-Based Participatory Research Approach to Collect Hopi Breast Cancer Survivors’ Stories. Am. Indian Cult. Res. J. 2015, 39, 97–109. [Google Scholar] [CrossRef]
- Gittelsohn, J.; Davis, S.M.; Steckler, A.; Ethelbah, B.; Clay, T.; Metcalfe, L.; Rock, B.H. Pathways: Lessons learned and future directions for school-based interventions among American Indians. Prev. Med. 2003, 37, S107–S112. [Google Scholar] [CrossRef]
- Helm, S.; Lee, W.; Hanakahi, V.; Gleason, K.; McCarthy, K.; Haumana. Using photovoice with youth to develop a drug prevention program in a rural Hawaiian community. Am. Indian Alsk. Native Ment. Health Res. 2015, 22, 1–26. [Google Scholar] [CrossRef]
- Adams, A.K.; LaRowe, T.L.; Cronin, K.A.; Prince, R.J.; Wubben, D.P.; Parker, T.; Jobe, J.B. The Healthy Children, Strong Families intervention: Design and community participation. J. Prim. Prev. 2012, 33, 175–185. [Google Scholar] [CrossRef]
- Hiratsuka, V.Y.; Brown, J.K.; Hoeft, T.J.; Dillard, D.A. Alaska Native people’s perceptions, understandings, and expectations for research involving biological specimens. Int. J. Circumpolar Health 2012, 71. [Google Scholar] [CrossRef]
- Heckert, W.; Eisenhauer, C. A case report of historical trauma among American Indians on a rural Northern Plains Reservation. J. Forensic Nurs. 2014, 10, 106–109. [Google Scholar] [CrossRef]
- Perry, C.; Hoffman, B. Assessing tribal youth physical activity and programming using a community-based participatory research approach. Public Health Nurs. 2010, 27, 104–114. [Google Scholar] [CrossRef]
- Schell, L.M.; Ravenscroft, J.; Cole, M.; Jacobs, A.; Newman, J. Health disparities and toxicant exposure of Akwesasne Mohawk young adults: A partnership approach to research. Environ. Health Perspect. 2005, 113, 1826–1832. [Google Scholar] [CrossRef]
- Walters, K.L.; LaMarr, J.; Levy, R.L.; Pearson, C.; Maresca, T.; Mohammed, S.A.; Simoni, J.M.; Evans-Campbell, T.; Fredriksen-Goldsen, K.; Fryberg, S.; et al. Project həli?dxw/Healthy Hearts Across Generations: Development and evaluation design of a tribally based cardiovascular disease prevention intervention for American Indian families. J. Prim. Prev. 2012, 33, 197–207. [Google Scholar] [CrossRef]
- Hodge, C.E.; Hodge, F.S.; Palacios, J.F. Tribal-Based Participatory Research: The Wellness Circles Project. In Health Promotion in Multicultural Populations: A Handbook for Practitioners and Students; Huff, R.M., Kline, M.V., Peterson, D.V., Eds.; SAGE Publications, Inc.: Thousand Oaks, CA, 2015; Volume 3. [Google Scholar]
- Schell, L.M.; Ravenscroft, J.; Gallo, M.; Denham, M. Advancing biocultural models by working with communities: A partnership approach. Am. J. Hum. Biol. 2007, 19, 511–524. [Google Scholar] [CrossRef]
- Krebs, L.U.; Burhansstipanov, L.; Watanabe-Galloway, S.; Pingatore, N.L.; Petereit, D.G.; Isham, D. Navigation as an intervention to eliminate disparities in American Indian communities. Semin. Oncol. Nurs. 2013, 29, 118–127. [Google Scholar] [CrossRef]
- Wendt, D.C.; Gone, J.P. Urban-indigenous therapeutic landscapes: A case study of an urban American Indian health organization. Health Place 2012, 18, 1025–1033. [Google Scholar] [CrossRef]
- Brown, S.R.; Joshweseoma, L.; Flood, T.; Coe, K. Process for determining the cancer burden of the Hopi Tribe. Public health reports 2010, 125, 793–800. [Google Scholar] [CrossRef]
- Wallerstein, N.; Oetzel, J.; Duran, B.; Tafoya, G.; Belone, L.; Rae, R. What predicts outcomes in CBPR. Community-Based Particip. Res. Health: Process Outcomes 2008, 2, 371–392. [Google Scholar]
- Oetzel, J.G.; Wallerstein, N.; Duran, B.; Sanchez-Youngman, S.; Nguyen, T.; Woo, K.; Wang, J.; Schulz, A.; Keawe’aimoku Kaholokula, J.; Israel, B.; et al. Impact of Participatory Health Research: A Test of the Community-Based Participatory Research Conceptual Model. Biomed Res. Int. 2018, 2018, 7281405. [Google Scholar] [CrossRef]
- Simera, I.; Moher, D.; Hoey, J.; Schulz, K.F.; Altman, D.G. A catalogue of reporting guidelines for health research. Eur. J. Clin. Investig. 2010, 40, 35–53. [Google Scholar] [CrossRef]
- Chalmers, I.; Glasziou, P. Avoidable waste in the production and reporting of research evidence. Lancet 2009, 374, 86–89. [Google Scholar] [CrossRef]
- Simera, I.; Altman, D.G. Writing a research article that is “fit for purpose”: Equator Network and reporting guidelines. Evid.- Based Med. 2009, 14, 132–134. [Google Scholar] [CrossRef]
- Israel, B.A.; Eng, E.; Schulz, A.J.; Parker, E.A. Methods for Community-Based Participatory Research for Health; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Minkler, M.; Wallerstein, N. Community-Based Participatory Research for Health: From Process to Outcomes; Wiley: Hoboken, NJ, USA, 2011. [Google Scholar]
- National Congress of American Indians (NCAI) Policy Research Center, Center for Native Health Partnerships. Walk Softly and Listen Carefully: Building Research Relationships with Tribal Communities; National Congress of American Indians (NCAI) Policy Research Center: Washington, DC, USA; Bozeman, MT, USA, 2012. [Google Scholar]
- Native American Center for Excellence. Steps for Conducting Research and Evaluation in Native Communities; Native American Center for Excellence: Houston, TX, USA; Available online: http://localcontexts.org/project/nace-steps-conducting-research-evaluation-native-communities/ (accessed on August 16th 2019).
- Langdon, S.E.; Golden, S.L.; Arnold, E.M.; Maynor, R.F.; Bryant, A.; Freeman, V.K.; Bell, R.A. Lessons learned from a community-based participatory research mental health promotion program for American Indian youth. Health Promot. Pract. 2016, 17, 457–463. [Google Scholar] [CrossRef]
- Matloub, J.; Creswell, P.D.; Strickland, R.; Pierce, K.; Stephenson, L.; Waukau, J.; Kaur, J.S.; Remington, P. Lessons learned from a community-based participatory research project to improve American Indian cancer surveillance. Prog. Community Health Partnersh. 2009, 3, 47–52. [Google Scholar] [CrossRef]
- Schell, L.M.; Tarbell, A.M. A partnership study of PCBs and the health of Mohawk youth: Lessons from our past and guidelines for our future. Environ. Health Perspect. 1998, 106, 833–840. [Google Scholar]
- Thomas, L.R.; Rosa, C.; Forcehimes, A.; Donovan, D.M. Research partnerships between academic institutions and American Indian and Alaska Native Tribes and organizations: Effective strategies and lessons learned in a multisite CTN study. Am. J. Drug Alcohol Abus. 2011, 37, 333–338. [Google Scholar] [CrossRef]
- Bordeaux, B.C.; Wiley, C.; Tandon, S.D.; Horowitz, C.R.; Brown, P.B.; Bass, E.B. Guidelines for writing manuscripts about community-based participatory research for peer-reviewed journals. Prog. Community Health Partnersh. 2007, 1, 281–288. [Google Scholar] [CrossRef]
- Grieb, S.D.; Eder, M.M.; Smith, K.C.; Calhoun, K.; Tandon, D. Qualitative Research and Community-Based Participatory Research: Considerations for Effective Dissemination in the Peer-Reviewed Literature. Prog. Community Health Partnersh. 2015, 9, 275–282. [Google Scholar] [CrossRef]
- Smith, L.; Rosenzweig, L.; Schmidt, M. Best Practices in the Reporting of Participatory Action Research: Embracing Both the Forest and the Trees 1Ψ7. Couns. Psychol. 2010, 38, 1115–1138. [Google Scholar] [CrossRef]
- Horowitz, C.R.; Robinson, M.; Seifer, S. Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation 2009, 119, 2633–2642. [Google Scholar] [CrossRef]
- Institute of Medicine. Who Will Keep the Public Healthy? Educating Public Health Professionals for the 21st Century; The National Academies Press: Washington, DC, USA, 2003. [Google Scholar]

| Health Conditions/Issues or Topics of Interest | Articles n (%) |
|---|---|
| Any Cancer | 33 (18) |
| Breast Cancer 1 | 13 (7) |
| Cervical Cancer 2 | 6 (3) |
| Colorectal Cancer | 2 (1) |
| Cancer (General/Other) 3 | 15 (8) |
| Any Mental/Behavioral Health | 24 (13) |
| Historical Trauma | 3 (2) |
| Suicide | 13 (7) |
| Mental/Behavioral Health (General) | 9 (5) |
| Any Substance Use/Misuse | 34 (19) |
| Alcohol Misuse | 13 (7) |
| Tobacco Use 4 | 8 (4) |
| Substance Misuse (General/Other) | 16 (9) |
| CVD | 4 (2) |
| Diabetes/Obesity | 18 (10) |
| Elder Care | 6 (3) |
| Environmental Health | 8 (4) |
| Exercise/Diet | 14 (8) |
| Family Wellness | 9 (5) |
| Sexual Health 5 | 14 (8) |
| Evaluating/Developing Health Research Systems and Approaches | 23 (13) |
| Evaluating/Developing Health Care and Public Health Systems | 18 (10) |
| Other | 21 (12) |
| Study Component | Example Activity | Y (%) | N (%) | NR (%) | NA (%) |
|---|---|---|---|---|---|
| Initiation | Ft. Peck Tribes invited Montana State University Staff to Ft. Peck Reservation to discuss potential research project on the community’s sexual and reproductive health needs [23]. | 49 (27) | 20 (11) | 110 (61) | 1 (1) |
| Funding | Community members helped review and provide feedback on grant proposals and assisted in drafting grant proposals [24]. | 46 (26) | 11 (6) | 120 (67) | 3 (2) |
| Research Question, Study Aims | Community elders, oral historian, and Lakota linguist involved in discussion that determined study goals [25]. | 118 (66) | 6 (3) | 55 (31) | 1 (1) |
| Administration | Community researchers participated in selection, interview, and hiring of community organizers [26]. | 96 (53) | 2 (1) | 81 (45) | 1 (1) |
| Design, Methods, Approach | Community input guided selection of screening methods and processes and targets related to adaptation of screening methods [27]. | 114 (63) | 3 (2) | 62 (34) | 1 (1) |
| Protocols | CAG 1, community-based project staff, and researchers co-developed telephone scripts and surveys with community member input [28]. | 129 (72) | 1 (1) | 47 (26) | 3 (2) |
| Meetings and Events | CAG meetings, open community meetings, executive board meetings, and monthly meetings between lay health advisors and project staff [29]. | 136 (76) | 0 (0) | 16 (9) | 28 (16) |
| Data Collection | Community health representatives moderated focus groups and took notes [30]. | 115 (64) | 7 (4) | 56 (31) | 2 (1) |
| Data Analysis | Community members helped develop codebook and were involved in coding and review of themes developed from codes [31]. | 83 (46) | 14 (8) | 77 (43) | 6 (3) |
| Intervention | CAG suggested cultural adaptations to educational materials to promote organ donation, including addition of storytelling components, emphasis on community values of generosity, and local photography [32]. | 111 (62) | 1 (1) | 29 (16) | 39 (22) |
| Dissemination | CAG members reviewed manuscripts draft and their comments were incorporated into final draft; CAG members also represented the project at national forums [33]. | 93 (52) | 1 (1) | 77 (43) | 9 (5) |
| Regulatory/Guidance Mechanism | Articles n (%) |
|---|---|
| Regulatory/Guidance Group CAG 1 | 125 (69) |
| Tribal Leader | 11 (6) |
| Tribal Liaison/Facilitator | 64 (36) |
| Community Leader | 4 (2) |
| Tribal Council | 45 (25) |
| Tribal Research Committee/Board | 14 (8) |
| Tribal Health Committee/Board | 18 (10) |
| Other Tribal Committee/Board | 26 (14) |
| Tribal IRB 2 | 18 (10) |
| Regulatory/Guidance Document | |
| Research Code/Agreement | 5 (3) |
| Memorandum of Agreement | 10 (6) |
| Tribal Resolution | 17 (9) |
| Data Sharing Agreement | 4 (2) |
| Total Regulatory/Guidance Groups and Documents per Study | |
| 0 Groups and Documents | 21 (12) |
| 1 Groups and Documents | 44 (24) |
| 2 Groups and Documents | 56 (31) |
| 3 Groups and Documents | 38 (21) |
| 4 Groups and Documents | 12 (7) |
| >4 Groups and Documents | 7 (4) |
| Cultural Adaptation | Articles n (%) |
|---|---|
| Type of Cultural Adaptation | |
| Culturally Adapted Study Design | 72 (40) |
| Culturally Adapted Study Protocols | 109 (61) |
| Culturally Adapted Interventions | 80 (44) |
| Dissemination Products and Methods | 35 (19) |
| Number of Culturally Adapted Study Components | |
| 0 Culturally Adapted Components | 32 (18) |
| 1 Culturally Adapted Components | 55 (31) |
| 2 Culturally Adapted Components | 50 (28) |
| 3 Culturally Adapted Components | 23 (13) |
| 4 Culturally Adapted Components | 18 (10) |
| Measures of Research Capacity or Co-learning | Y (%) | N (%) | NR (%) | NA (%) |
|---|---|---|---|---|
| Community members received research training | 93 (52) | 10 (6) | 76 (42) | 1 (1) |
| Community members received academic credit for research training | 4 (2) | 2 (1) | 87 (48) | 0 (0) |
| Community members were employed by researchers | 50 (28) | 7 (4) | 120 (67) | 3 (2) |
| Community had prior experience with research | 82 (46) | 1 (1) | 96 (53) | 1 (1) |
| Community members received training in PR | 43 (24) | 1 (1) | 135 (75) | 1 (1) |
| Researchers Received Training in Community Culture/History | 60 (33) | 0 (0) | 117 (65) | 3 (2) |
| Researchers had Prior Experience with Community | 89 (49) | 4 (2) | 85 (47) | 2 (1) |
| Researchers had or Received Training in PR | 47 (26) | 1 (1) | 131 (73) | 1 (1) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woodbury, R.B.; Ketchum, S.; Hiratsuka, V.Y.; Spicer, P. Health-Related Participatory Research in American Indian and Alaska Native Communities: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 16, 2969. https://doi.org/10.3390/ijerph16162969
Woodbury RB, Ketchum S, Hiratsuka VY, Spicer P. Health-Related Participatory Research in American Indian and Alaska Native Communities: A Scoping Review. International Journal of Environmental Research and Public Health. 2019; 16(16):2969. https://doi.org/10.3390/ijerph16162969
Chicago/Turabian StyleWoodbury, R. Brian, Scott Ketchum, Vanessa Y. Hiratsuka, and Paul Spicer. 2019. "Health-Related Participatory Research in American Indian and Alaska Native Communities: A Scoping Review" International Journal of Environmental Research and Public Health 16, no. 16: 2969. https://doi.org/10.3390/ijerph16162969
APA StyleWoodbury, R. B., Ketchum, S., Hiratsuka, V. Y., & Spicer, P. (2019). Health-Related Participatory Research in American Indian and Alaska Native Communities: A Scoping Review. International Journal of Environmental Research and Public Health, 16(16), 2969. https://doi.org/10.3390/ijerph16162969





