Cancer Incidence Among Air Transportation Industry Workers Using the National Cohort Study of Korea
Abstract
:1. Introduction
2. Methods
2.1. Data
2.2. Study Participants and Cohort
2.3. Cancers
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Approval of the Research Protocol
Informed Consent
References
- Hu, S.; Fruin, S.; Kozawa, K.; Mara, S.; Winer, A.M.; Paulson, S.E. Aircraft Emission Impacts in a Neighborhood Adjacent to a General Aviation Airport in Southern California. Environ. Sci. Technol. 2009, 43, 8039–8045. [Google Scholar] [CrossRef] [PubMed]
- Springston, J.P.; Esposito, W.A.; Cleversey, K.W. Baseline Indoor Air Quality Measurements Collected From 136 Metropolitan New York Region Commercial Office Buildings Between 1997–1999. AIHA J. 2002, 63, 354–360. [Google Scholar] [CrossRef]
- Takada, M.; Nunomiya, T.; Ishikura, T.; Nakamura, T.; Lewis, B.J.; Bennett, L.G.; Getley, I.L.; Bennett, B.H. Measuring cosmic-ray exposure in aircraft using real-time personal dosemeters. Radiat. Prot. Dosim. 2012, 149, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.J.; Abbott, S.M. Jet Lag and Shift Work Disorder. Sleep Med. Clin. 2015, 10, 523–535. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, R.F.; Powell, D.M. The occupational health and safety of flight attendants. Aviat. Space Environ. Med. 2012, 83, 514–521. [Google Scholar] [CrossRef]
- Band, P.R.; Spinelli, J.J.; Ng, V.T.; Moody, J.; Gallagher, R.P. Mortality and cancer incidence in a cohort of commercial airline pilots. Aviat. Space Environ. Med. 1990, 61, 299–302. [Google Scholar]
- A Salisbury, D.; Band, P.R.; Threlfall, W.J.; Gallagher, R.P. Mortality among British Columbia pilots. Aviat. Space Environ. Med. 1991, 62, 351–352. [Google Scholar]
- Irvine, D.; Davies, D.M. The mortality of British Airways pilots, 1966–1989: A proportional mortality study. Aviat. Space Environ. Med. 1992, 63, 276–279. [Google Scholar]
- Pukkala, E.; Aspholm, R.; Gundestrup, M.; Haldorsen, T.; Hammar, N.; Hrafnkelsson, J.; Kyyrönen, P.; Linnersjö, A.; Rafnsson, V.; Storm, H.; et al. Incidence of cancer among Nordic airline pilots over five decades: Occupational cohort study. BMJ 2002, 325, 567. [Google Scholar] [CrossRef]
- Rafnsson, V.; Hrafnkelsson, J.; Tulinius, H. Incidence of cancer among commercial airline pilots. Occup. Environ. Med. 2000, 57, 175–179. [Google Scholar] [CrossRef] [Green Version]
- Band, P.R.; Le, N.D.; Fang, R.; Deschamps, M.; Coldman, A.J.; Gallagher, R.P.; Moody, J. Cohort Study of Air Canada Pilots: Mortality, Cancer Incidence, and Leukemia Risk. Am. J. Epidemiol. 1996, 143, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Ballard, T.; Lagorio, S.; De Angelis, G.; Verdecchia, A. Cancer incidence and mortality among flight personnel: A meta-analysis. Aviat. Space Environ. Med. 2000, 71, 216–224. [Google Scholar] [PubMed]
- Buja, A.; Mastrangelo, G.; Perissinotto, E.; Grigoletto, F.; Frigo, A.C.; Rausa, G.; Marin, V.; Canova, C.; Dominici, F. Cancer Incidence among Female Flight Attendants: A Meta-Analysis of Published Data. J. Women’s Health 2006, 15, 98–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tokumaru, O.; Haruki, K.; Bacal, K.; Katagiri, T.; Yamamoto, T.; Sakurai, Y. Incidence of Cancer among Female Flight Attendants: A Meta-Analysis. J. Travel Med. 2006, 13, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Hammer, G.P.; Auvinen, A.; De Stavola, B.L.; Grajewski, B.; Gundestrup, M.; Haldorsen, T.; Hammar, N.; Lagorio, S.; Pinkerton, L.; Pukkala, E.; et al. Mortality from cancer and other causes in commercial airline crews: A joint analysis of cohorts from 10 countries. Occup. Environ. Med. 2014, 71, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S. Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy Plan. 2009, 24, 63–71. [Google Scholar] [CrossRef] [PubMed]
- United Nations Statistics Division (UNSD). International Standard Industrial Classification of All Economic Activities (ISIC); United Nations Publications: New York, NY, USA, 2008. [Google Scholar]
- Chun, C.B.; Kim, S.Y.; Lee, J.Y.; Lee, S.Y. Republic of Korea: Health system review. Health Syst. Transit. 2009, 11, 1–184. [Google Scholar]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Lim, S.S.; Lee, W.; Kim, Y.K.; Kim, J.; Park, J.H.; Park, B.R.; Yoon, J.H. The cumulative incidence and trends of rare diseases in South Korea: A nationwide study of the administrative data from the National Health Insurance Service database from 2011–2015. Orphanet J. Rare Dis. 2019, 14, 49. [Google Scholar] [CrossRef]
- Kojo, K.; Aspholm, R.; Auvinen, A. Occupational radiation dose estimation for Finnish aircraft cabin attendants. Scand. J. Work. Environ. Health 2004, 30, 157–163. [Google Scholar] [CrossRef]
- Anderson, J.L.; Waters, M.A.; Hein, M.J.; Schubauer-Berigan, M.K.; Pinkerton, L.E. Assessment of occupational cosmic radiation exposure of flight attendants using questionnaire data. Aviat. Space Environ. Med. 2011, 82, 1049–1054. [Google Scholar] [CrossRef]
- Wrixon, A.D. New ICRP recommendations. J. Radiol. Prot. 2008, 28, 161–168. [Google Scholar] [CrossRef]
- Hammer, G.P.; Zeeb, H.; Tveten, U.; Blettner, M. Comparing different methods of estimating cosmic radiation exposure of airline personnel. Radiat. Environ. Biophys. 2000, 39, 227–231. [Google Scholar] [CrossRef]
- Bütikofer, R.; Flückiger, E.; Desorgher, L.; Moser, M. The extreme solar cosmic ray particle event on 20 January 2005 and its influence on the radiation dose rate at aircraft altitude. Sci. Total Environ. 2008, 391, 177–183. [Google Scholar] [CrossRef]
- McCooey, S.; Ison, D. Female Cabin Crew Radiation Exposure and Cancer Development: A Cross-Study Inquiry. Int. J. Prof. Aviat. Train. Test. Res. 2017, 9, 1–20. [Google Scholar]
- Di Trolio, R.; Di Lorenzo, G.; Fumo, B.; Ascierto, A.P. Cosmic radiation and cancer: Is there a link? Futur. Oncol. 2015, 11, 1123–1135. [Google Scholar] [CrossRef]
- Gundestrup, M.; Andersen, M.K.; Sveinbjornsdottir, E.; Rafnsson, V.; Storm, H.H.; Pedersen-Bjergaard, J. Cytogenetics of myelodysplasia and acute myeloid leukaemia in aircrew and people treated with radiotherapy. Lancet 2000, 356, 2158. [Google Scholar] [CrossRef]
- Gundestrup, M.; Storm, H.H. Radiation-induced acute myeloid leukaemia and other cancers in commercial jet cockpit crew: A population-based cohort study. Lancet 1999, 354, 2029–2031. [Google Scholar] [CrossRef]
- Schuz, J. Airline crew cohorts: Is there more to learn regarding their cancer risk? Occup. Environ. Med. 2014, 71, 307. [Google Scholar] [CrossRef]
- Sigurdson, A.J.; Ron, E. Cosmic Radiation Exposure and Cancer Risk among Flight Crew. Cancer Investig. 2004, 22, 743–761. [Google Scholar] [CrossRef]
- Ward, E.; Jemal, A.; Cokkinides, V.; Singh, G.K.; Cardinez, C.; Ghafoor, A.; Thun, M. Cancer Disparities by Race/Ethnicity and Socioeconomic Status. CA A Cancer J. Clin. 2004, 54, 78–93. [Google Scholar] [CrossRef]
- Delpierre, C.; Lauwers-Cances, V.; Datta, G.D.; Lang, T.; Berkman, L. Using self-rated health for analysing social inequalities in health: A risk for underestimating the gap between socioeconomic groups? J. Epidemiol. Community Health 2009, 63, 426–432. [Google Scholar] [CrossRef]
| Person-year, % | ||||||
|---|---|---|---|---|---|---|
| Air Transportation Industry Workers | Government Employee | Whole Employee | ||||
| Total person-years | 59,751 | 5,678,047 | 85,954,378 | |||
| Gender | ||||||
| Male | 45,673 | 76.4 | 2,898,213 | 51.0 | 57,871,482 | 67.3 |
| Female | 14,078 | 23.6 | 2,779,834 | 49.0 | 28,082,896 | 32.7 |
| Age | ||||||
| Total | ||||||
| 25–30 | 5980 | 10.0 | 290,037 | 5.1 | 9,240,276 | 10.8 |
| 31–35 | 11,398 | 19.1 | 722,694 | 12.7 | 15,509,508 | 18.0 |
| 36–40 | 12,109 | 20.3 | 974,979 | 17.2 | 16,435,257 | 19.1 |
| 41–45 | 10,330 | 17.3 | 1,054,586 | 18.6 | 14,852,909 | 17.3 |
| 46–50 | 8719 | 14.6 | 1,056,016 | 18.6 | 12,825,823 | 14.9 |
| 51–55 | 7108 | 11.9 | 920,516 | 16.2 | 10,270,762 | 11.9 |
| 56–60 | 4107 | 6.9 | 659,219 | 11.6 | 6,819,843 | 7.9 |
| Male | ||||||
| 25–30 | 2378 | 5.2 | 57,160 | 2.0 | 4,240,331 | 7.3 |
| 31–35 | 6997 | 15.3 | 210,875 | 7.3 | 9,019,025 | 15.6 |
| 36–40 | 9883 | 21.6 | 390,711 | 13.5 | 11,470,377 | 19.8 |
| 41–45 | 9102 | 19.9 | 516,571 | 17.8 | 10,897,150 | 18.8 |
| 46–50 | 7615 | 16.7 | 615,957 | 21.3 | 9,434,555 | 16.3 |
| 51–55 | 6121 | 13.4 | 622,025 | 21.5 | 7,639,526 | 13.2 |
| 56–60 | 3577 | 7.8 | 484,914 | 16.7 | 5,170,518 | 8.9 |
| Female | ||||||
| 25–30 | 3602 | 25.6 | 232,877 | 8.4 | 4,999,945 | 17.8 |
| 31–35 | 4401 | 31.3 | 511,819 | 18.4 | 6,490,483 | 23.1 |
| 36–40 | 2226 | 15.8 | 584,268 | 21.0 | 4,964,880 | 17.7 |
| 41–45 | 1228 | 8.7 | 538,015 | 19.4 | 3,955,759 | 14.1 |
| 46–50 | 1104 | 7.8 | 440,059 | 15.8 | 3,391,268 | 12.1 |
| 51–55 | 987 | 7.0 | 298,491 | 10.7 | 2,631,236 | 9.4 |
| 56–60 | 530 | 3.8 | 174,305 | 6.3 | 1,649,325 | 5.9 |
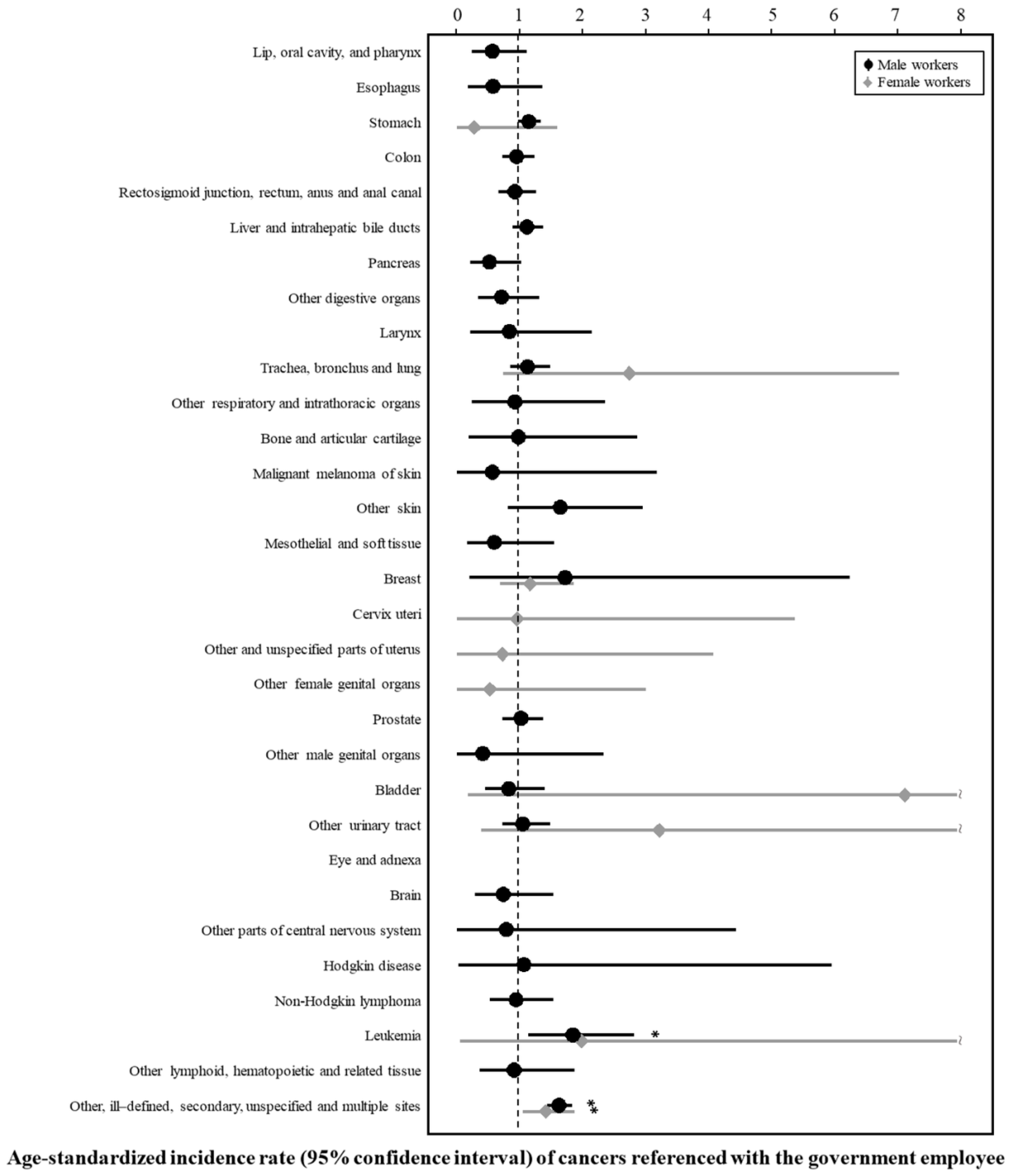
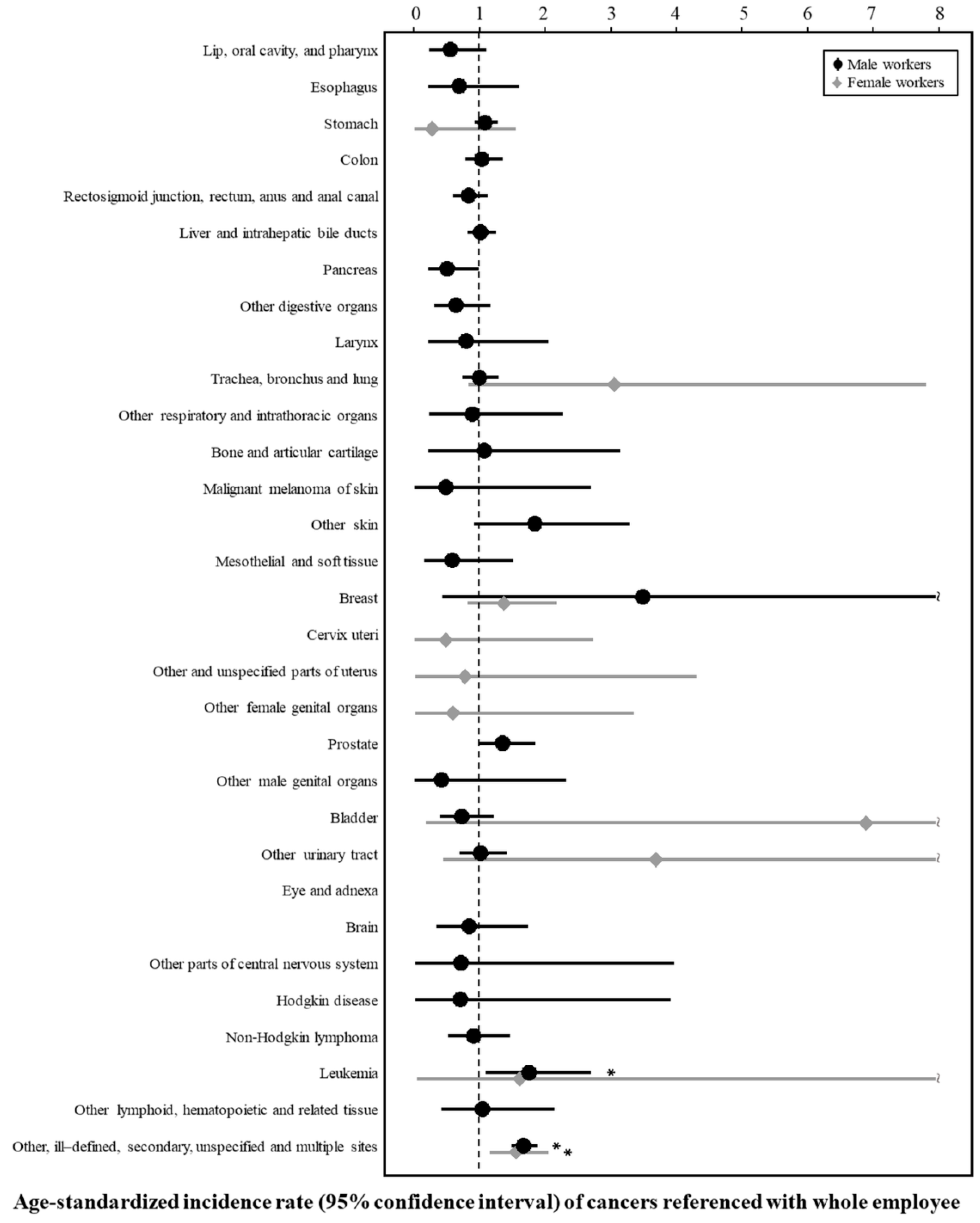
| Cancer | ICD-10 | Reference, SIR (95% CI) for Cancers | |
|---|---|---|---|
| Government Employee | Whole Employee | ||
| All cancer | 0.58 (0.54–0.62) | 0.57 (0.53–0.61) | |
| Gastrointestinal tract system | |||
| Malignant neoplasms of lip, oral cavity, and pharynx | C00–C14 | 0.58 (0.25–1.13) | 0.56 (0.24–1.11) |
| Malignant neoplasm of esophagus | C15 | 0.59 (0.19–1.37) | 0.69 (0.22–1.61) |
| Malignant neoplasm of stomach | C16 | 1.16 (0.98–1.35) | 1.09 (0.93–1.28) |
| Malignant neoplasm of colon | C18 | 0.96 (0.73–1.25) | 1.04 (0.79–1.36) |
| Malignant neoplasms of rectosigmoid junction, rectum, anus, and anal canal | C19–C21 | 0.93 (0.67–1.27) | 0.84 (0.60–1.14) |
| Malignant neoplasm of liver and intrahepatic bile ducts | C22 | 1.13 (0.90–1.39) | 1.02 (0.82–1.26) |
| Malignant neoplasm of pancreas | C25 | 0.52 (0.23–1.04) | 0.51 (0.22–1.00) |
| Other malignant neoplasms of digestive organs | C17, C23–C24, C26 | 0.72 (0.34–1.32) | 0.64 (0.31–1.17) |
| Respiratory system | |||
| Malignant neoplasm of larynx | C32 | 0.85 (0.23–2.16) | 0.80 (0.22–2.06) |
| Malignant neoplasm of trachea, bronchus, and lung | C33–C34 | 1.14 (0.86–1.49) | 1.00 (0.75–1.30) |
| Other malignant neoplasms of respiratory and intrathoracic organs | C30–C31, C37–C39 | 0.93 (0.25–2.37) | 0.90 (0.24–2.29) |
| Bone and skin | |||
| Malignant neoplasms ofbone and articular cartilage | C40–C41 | 0.99 (0.20–2.89) | 1.08 (0.22–3.16) |
| Malignant melanoma of skin | C43 | 0.58 (0.01–3.21) | 0.49 (0.01–2.71) |
| Other malignant neoplasm of skin | C44 | 1.66 (0.83–2.97) | 1.85 (0.92–3.31) |
| Malignant neoplasms of mesothelial and soft tissue | C45–C49 | 0.61 (0.17–1.56) | 0.59 (0.16–1.52) |
| Genitourinary tract system | |||
| Malignant neoplasm of prostate | C61 | 1.03 (0.74–1.39) | 1.36 (0.98–1.85) |
| Other malignant neoplasms of male genital organs | C60, C62–C63 | 0.42 (0.01–2.35) | 0.42 (0.01–2.34) |
| Malignant neoplasm of bladder | C67 | 0.84 (0.46–1.42) | 0.73 (0.40–1.22) |
| Other malignant neoplasms of urinary tract | C64–C66, C68 | 1.06 (0.73–1.49) | 1.02 (0.70–1.43) |
| Nervous system | |||
| Malignant neoplasm of eye and adnexa | C69 | None | None |
| Malignant neoplasm of brain | C71 | 0.75 (0.30–1.55) | 0.85 (0.34–1.75) |
| Malignant neoplasm of other parts of central nervous system | C70, C72 | 0.80 (0.02–4.46) | 0.72 (0.02–3.98) |
| Lymphoid and hematopoietic system | |||
| Hodgkin disease | C81 | 1.08 (0.03–5.99) | 0.71 (0.02–3.93) |
| Non-Hodgkin lymphoma | C82–C86 | 0.95 (0.54–1.54) | 0.91 (0.52–1.47) |
| Leukemia | C91–C95 | 1.86 (1.15–2.84) | 1.77 (1.10–2.70) |
| Other malignant neoplasms of lymphoid, hematopoietic and related tissue | C88–C90, C96 | 0.92 (0.37–1.89) | 1.05 (0.42–2.16) |
| Other | |||
| Malignant neoplasm of other, ill-defined, secondary, unspecified, and multiple sites | C73–C80, C97 | 1.64 (1.45–1.85) | 1.68 (1.49–1.89) |
| Cancer | ICD-10 | Reference, SIR (95% CI) for Cancers | |
|---|---|---|---|
| Government Employee | Whole Employee | ||
| All cancer | 2.27 (1.79–2.84) | 2.09 (1.65–2.62) | |
| Gastrointestinal tract system | |||
| Malignant neoplasms of lip, oral cavity, and pharynx | C00–C14 | None | None |
| Malignant neoplasm of esophagus | C15 | None | None |
| Malignant neoplasm of stomach | C16 | 0.29 (0.01–1.61) | 0.28 (0.01–1.55) |
| Malignant neoplasm of colon | C18 | None | None |
| Malignant neoplasm of rectosigmoid junction, rectum, anus, and anal canal | C19–C21 | None | None |
| Malignant neoplasm of liver and intrahepatic bile ducts | C22 | None | None |
| Malignant neoplasm of pancreas | C25 | None | None |
| Other malignant neoplasm of digestive organs | C17, C23–C24, C26 | None | None |
| Respiratory system | |||
| Malignant neoplasm of larynx | C32 | None | None |
| Malignant neoplasm of trachea, bronchus, and lung | C33–C34 | 2.76 (0.76–7.06) | 3.07 (0.84–7.85) |
| Other malignant neoplasms of respiratory and intrathoracic organs | C30–C31, C37–C39 | None | None |
| Bone and skin | |||
| Malignant neoplasms ofbone and articular cartilage | C40–C41 | None | None |
| Malignant melanoma of skin | C43 | None | None |
| Other malignant neoplasm of skin | C44 | None | None |
| Malignant neoplasms of mesothelial and soft tissue | C45–C49 | None | None |
| Genitourinary tract system | |||
| Malignant neoplasm of breast | C50 | 1.18 (0.70–1.87) | 1.38 (0.82–2.18) |
| Malignant neoplasm of cervixuteri | C53 | 0.97 (0.02–5.40) | 0.49 (0.01–2.74) |
| Malignant neoplasms of other and unspecified parts of uterus | C54–C55 | 0.74 (0.02–4.11) | 0.78 (0.02–4.33) |
| Other malignant neoplasms of female genital organs | C51–C52, C56–C58 | 0.54 (0.01–3.02) | 0.60 (0.02–3.37) |
| Malignant neoplasm of bladder | C67 | 7.16 (0.18–39.90) | 6.93 (0.8–38.61) |
| Other malignant neoplasms of urinary tract | C64–C66, C68 | 3.24 (0.39–11.72) | 3.71 (0.45–13.40) |
| Nervous system | |||
| Malignant neoplasm of eye and adnexa | C69 | None | None |
| Malignant neoplasm of brain | C71 | None | None |
| Malignant neoplasm of other parts of central nervous system | C70, C72 | None | None |
| Lymphoid and hematopoietic system | |||
| Hodgkin disease | C81 | None | None |
| Non-Hodgkin lymphoma | C82–C86 | None | None |
| Leukemia | C91–C95 | 2.00 (0.05–11.16) | 1.62 (0.04–9.00) |
| Other malignant neoplasms of lymphoid, hematopoietic and related tissue | C88–C90, C96 | None | None |
| Other | |||
| Malignant neoplasm of other, ill-defined, secondary, unspecified, and multiple sites | C73–C80, C97 | 1.43 (1.06–1.89) | 1.57 (1.16–2.06) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.; Kang, M.-Y.; Yoon, J.-H. Cancer Incidence Among Air Transportation Industry Workers Using the National Cohort Study of Korea. Int. J. Environ. Res. Public Health 2019, 16, 2906. https://doi.org/10.3390/ijerph16162906
Lee W, Kang M-Y, Yoon J-H. Cancer Incidence Among Air Transportation Industry Workers Using the National Cohort Study of Korea. International Journal of Environmental Research and Public Health. 2019; 16(16):2906. https://doi.org/10.3390/ijerph16162906
Chicago/Turabian StyleLee, Wanhyung, Mo-Yeol Kang, and Jin-Ha Yoon. 2019. "Cancer Incidence Among Air Transportation Industry Workers Using the National Cohort Study of Korea" International Journal of Environmental Research and Public Health 16, no. 16: 2906. https://doi.org/10.3390/ijerph16162906
APA StyleLee, W., Kang, M.-Y., & Yoon, J.-H. (2019). Cancer Incidence Among Air Transportation Industry Workers Using the National Cohort Study of Korea. International Journal of Environmental Research and Public Health, 16(16), 2906. https://doi.org/10.3390/ijerph16162906







