The Mixed-Method 5W2D Approach for Health System Stakeholders Analysis in Quality of Care: An Application to the Moroccan Context
Abstract
:1. Introduction
2. Background
2.1. Quality of Care (QC)
2.2. Stakeholder Theory
- -
- The importance of stakeholders’ participation and involvement in the processes of identification, understanding, and resolution of health issues. Ng et al. [28] sought HSS viewpoints to spot the multiple dimensions and parameters to be included in the development of a medication safety assessment framework. Ong et al. [29] conducted interviews with HSS to identify challenges, opportunities, and ways forward for the implementation of regional health systems. Franco-Trigo et al. [30] conducted a stakeholder analysis of community pharmacy services for the prevention of cardiovascular disease. The authors of these studies highlighted the importance of involving HSS in planning processes to address health programs implementation challenges.
- -
- Understanding and considering the different perspectives of HSS in a project decision-making process ensures its success and survival. Hamilton et al. [31] suggested that stakeholder engagement is needed to support the implementation of clinical initiatives. For instance, the design and development of new medical devices and equipment require HSS consultation to take into consideration their specific needs and guarantee their acceptance of the proposed devices [32].
- -
- Highlighting the contradictory interests of HSS. Achieving the organization’s objectives usually involves conflicts of interests between stakeholders who do not have the same objectives [20]. Patients want effective care, health professionals demand favorable working conditions, managers seek to reduce costs, product makers are interested at defending their commercial interests, etc. [33]. Thus, it is important to maintain balance between these competing interests.
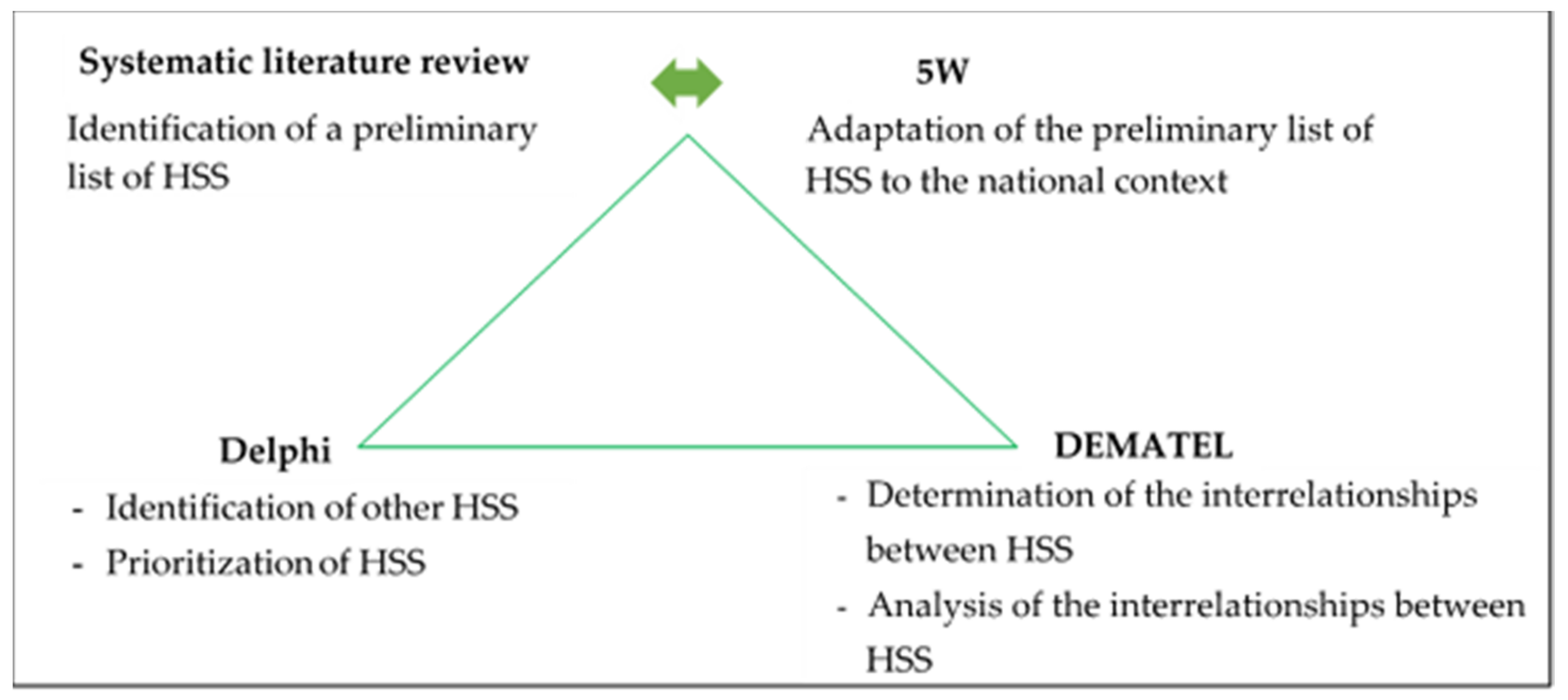
3. Methods
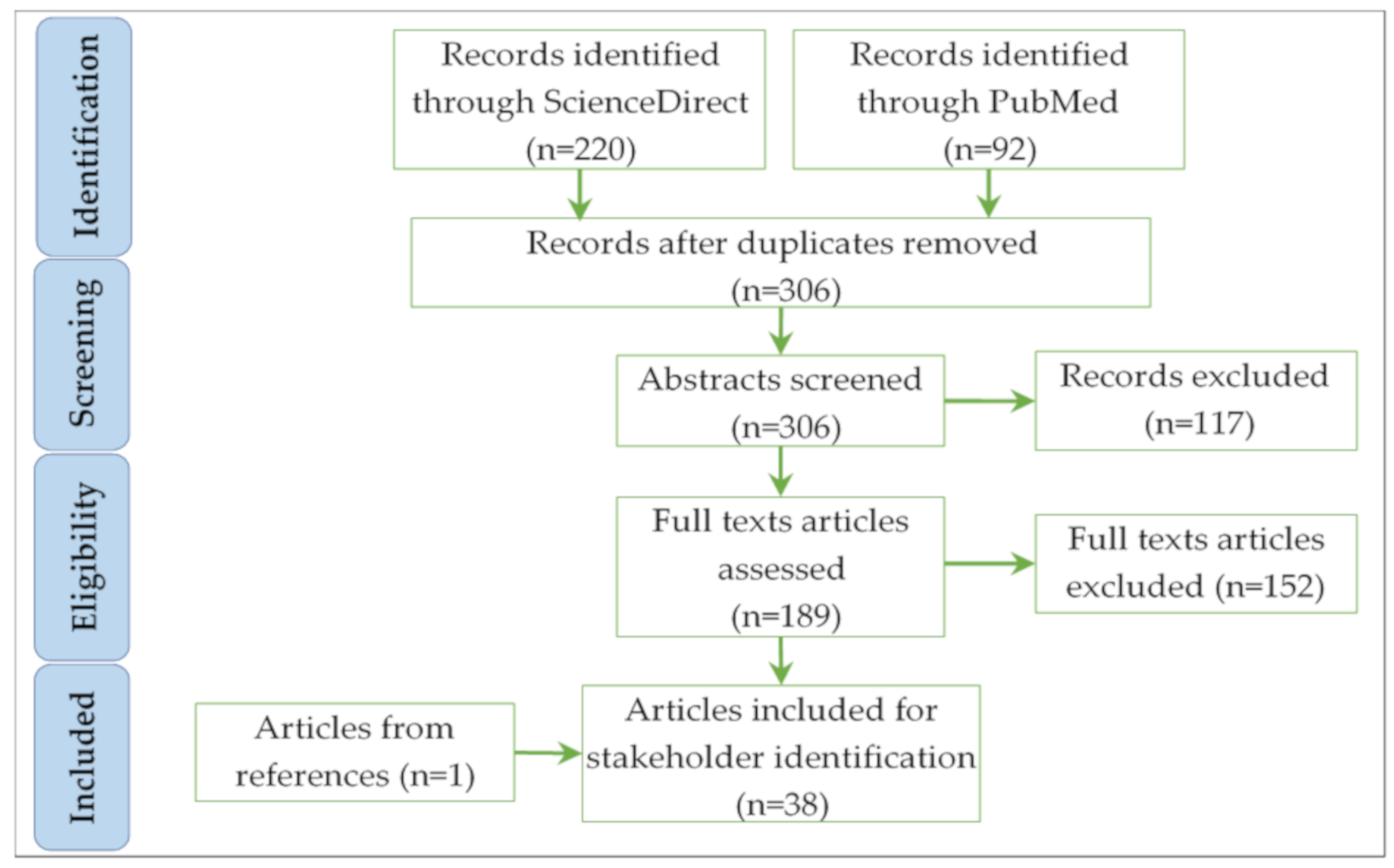
3.1. Systematic Literature Review and 5W
3.2. Delphi
- (1)
- Identification of experts: they should belong to different disciplines (i.e., academics, practitioners, government officials) and have relevant knowledge and experience in their respective fields. We suggest following expert identification steps by Okoli and Pawlowski [39].
- (2)
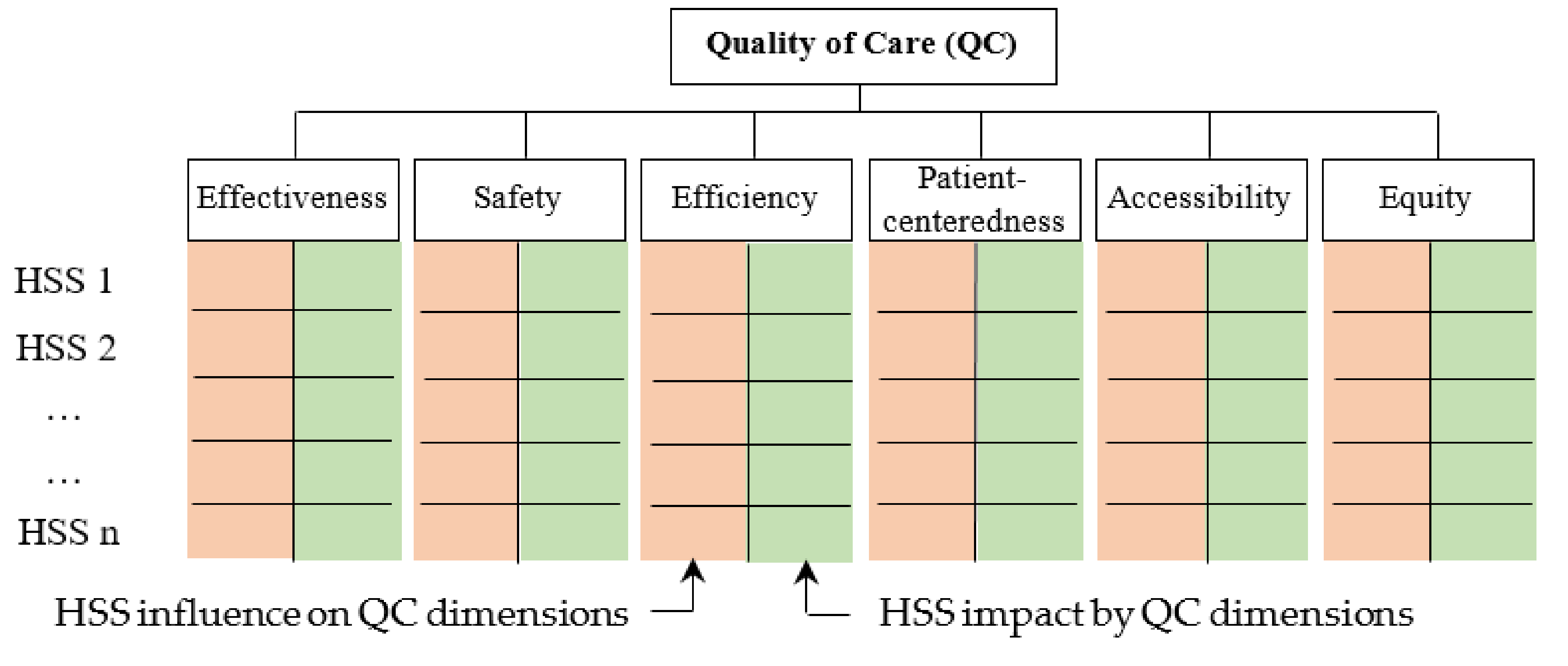
- Questionnaire design: the questionnaire contains two main questions. The first one invites experts to consult the HSS list and add others, if any, that they may consider relevant. The second one asks experts to assign two scores to each HSS regarding their influence on and impact by QC dimensions (Figure 2), using a scale from 1 to 5: “very low (1)”, “low (2)”, “medium (3)”, “high (4)”, and “very high (5)”. Table 1 about QC dimensions is appended to the questionnaire so that experts have a common understanding of the different dimensions.
- (3)
- Consultation of experts and result analysis: the questionnaire can be administered by e-mail or by post. Before analyzing the results, expert’s responses are completed by calculating the sum of the scores assigned to each HSS with respect to its influence on and impact by QC dimensions. Let us note,
- d: QC dimension index (1 ≤ d ≤ 6)
- E: number of experts
- e: expert index (1 ≤ e ≤ E)
- n: number of HSS
- k: HSS index (1 ≤ k ≤ n)
- Me,k,d: rating given by the expert e to the influence of HSSk on the QC dimension d
- Ne,k,d: rating given by the expert e to the impact of HSSk by the QC dimension d
- Mk: the average score of the influence of HSSk on QC
- Nk: the average score of the impact of HSSk by QC
3.3. DEMATEL
- Step 1: generate the direct-relation average matrix D
- Step 2: construct the normalized direct-relation matrix M
- Step 3: establish the total-relation matrix T
- Step 4: compute the column vector R and row vector C
4. Application of the Proposed Method: Case of Morocco
4.1. Preliminary List of HSS
4.2. List of HSS in Morocco
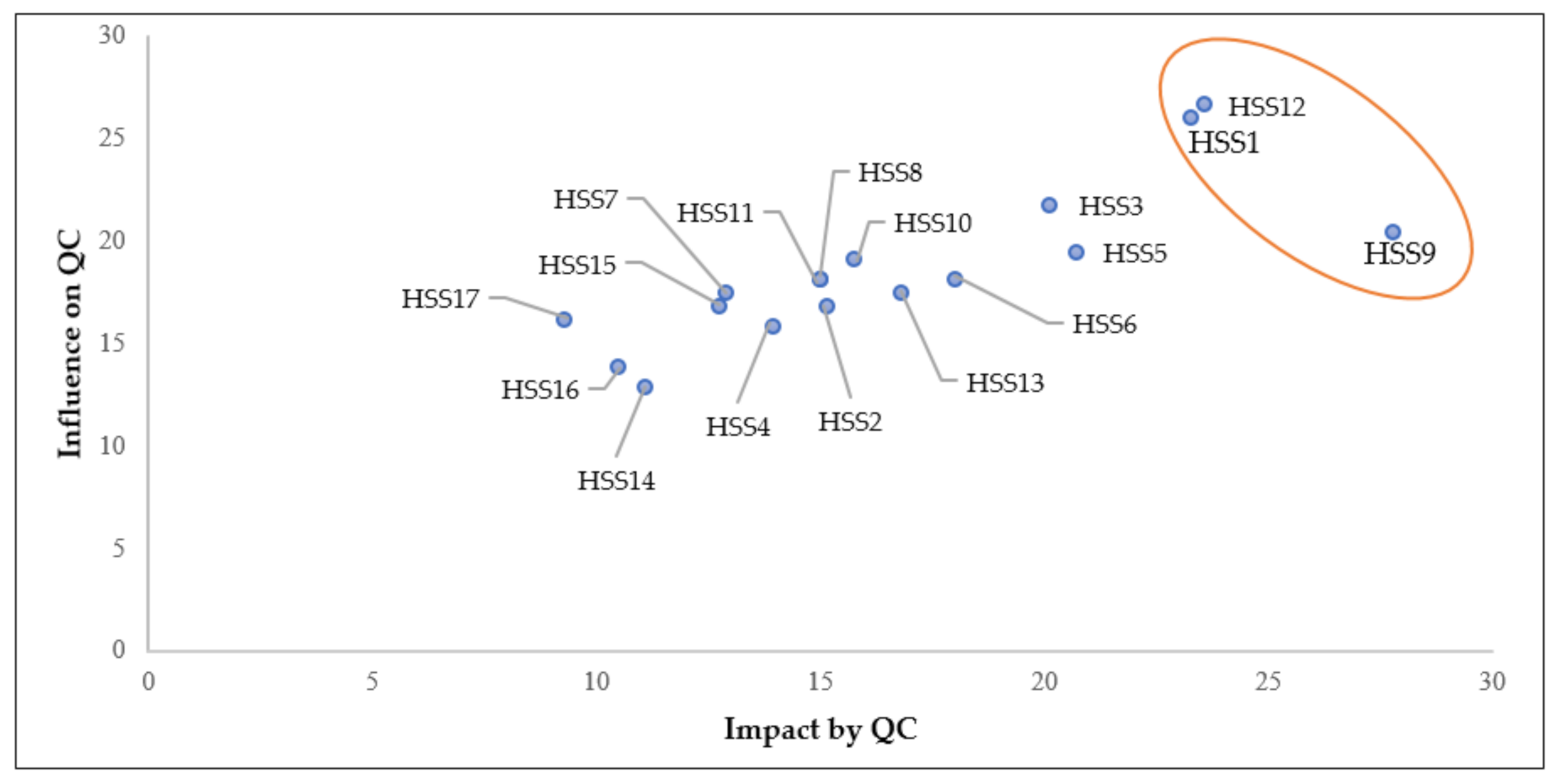
4.3. Prioritization of HSS
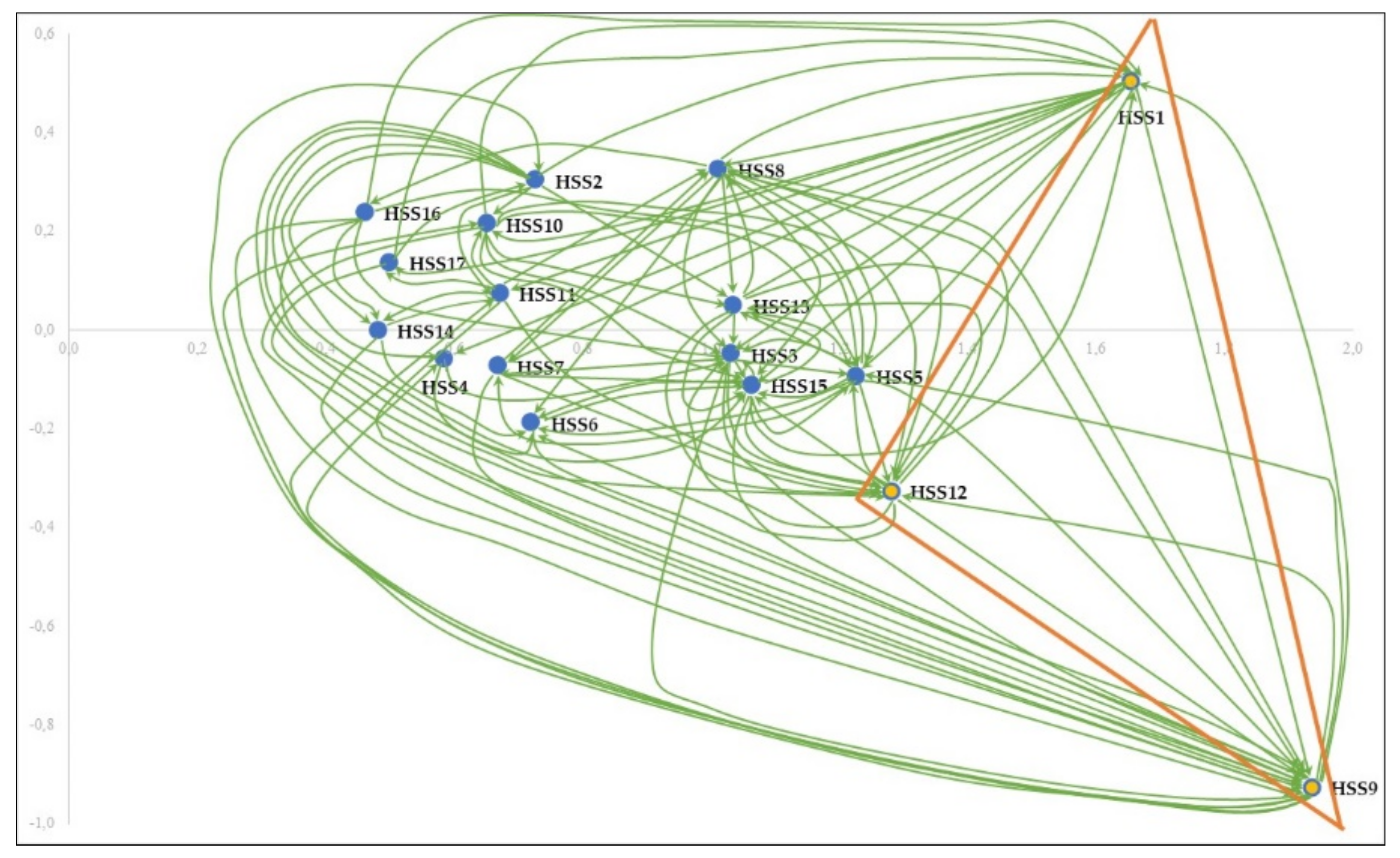
4.4. Analysis of Interrelationships between the HSS
5. Discussion
- -
- Patients: are the most important group and the reason behind the existence of health systems as the target of healthcare activities [32]. WHO emphasizes the need to place patients and populations at the center of health systems by meeting their needs and expectations [84]. The results of this study clearly showed that the action of all HSS has an impact on patients and, therefore, on the QC the way they perceive it. Similarly, patients influence QC because the care process is initiated at the patient level; patients are who decide when and where to seek care, and to continue or stop it [85]. Patients and populations also play the role of contributors to finance the health system through taxes and social security. Furthermore, the availability and access to information has radically changed the position of patients, who are no longer mere consumers of care, directed and guided by their physicians, but have become aware and able to make choices and decisions [86]. Another way that patients can influence QC is through satisfaction surveys, which are the most widely considered indicators in QC assessment. In this regard, some studies considered patients’ experience and involvement as an opportunity to improve healthcare services and bring new innovative ideas in delivering care [86].
- -
- Health personnel: are the providers of healthcare services and are involved throughout the care process. This HSS group includes medical, paramedical, administrative, and other health workers, all of whom are the point of contact with patients and largely influence their perception of received care. Also, health personnel play a very potential role in QC through professional skills (effectiveness and safety of care), respect of patients’ preferences and values (patient-centeredness), optimal use of available resources (efficiency), etc. [2].
- -
- Government: Through the Ministry of Health and other ministries of Finance, Education, Interior, Agriculture and Transport, the government has a significant impact on QC. The health system governance is carried out by the government, whose action is materialized by the strategies and policies it implements, as well as the funds it provides to the health system for its functioning, improvement, and innovation. The government plays a leadership role in the regulation, monitoring, and improvement of QC [87]. Generally speaking, governments play a crucial role in health development, through strengthening health systems and generating human and financial resources, to achieve objectives of improving health, efficiency and equity in health care financing [88].
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Al-Shdaifat, E.A.; Shdaifat, E. Implementation of total quality management in hospitals. J. Taibah Univ. Med. Sci. 2015, 10, 461–466. [Google Scholar] [CrossRef] [Green Version]
- Bautista, J.M.S.J.; Tangsoc, C. Hospital Service Quality Assessment and Analysis: A Multi-Perspective Approach. DLSU Bus. Econ. Rev. 2016, 26, 30–49. [Google Scholar]
- Leviton, L.C.; Melichar, L. Balancing stakeholder needs in the evaluation of healthcare quality improvement. BMJ Qual. Saf. 2016, 25, 803–807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendes, L.; Dias, D. Corporate Social Responsibility and Total Quality Management: The Stakeholders’ Value Creation Debate Revisited. In Applying Quality of Life Research; Springer Science and Business Media LLC: Berlin, Germany, 2018; pp. 255–283. [Google Scholar]
- Sebai, J. L’évaluation de la performance dans le système de soins. Que disent les théories? Santé Publique 2015, 27, 395. [Google Scholar] [CrossRef] [PubMed]
- Jawab, F.; Frichi, Y.; Boutahari, S. Hospital Logistics Activities. In Proceedings of the International Conference on Industrial Engineering and Operations Management, Bandung, Indonesia, 6–8 March 2018; pp. 3228–3237. [Google Scholar]
- Bryson, J.M. What to do when stakeholders matter: Stakeholder identification and analysis techniques. Public Manag. Rev. 2004, 6, 21–53. [Google Scholar] [CrossRef]
- Ju, B.; Jin, T. Incorporating nonparametric statistics into Delphi studies in library and information science. Inf. Res. Int. Electron. J. 2013, 18, 1–11. [Google Scholar]
- Bakir, S.; Khan, S.; Ahsan, K.; Rahman, S. Exploring the critical determinants of environmentally oriented public procurement using the DEMATEL method. J. Environ. Manag. 2018, 225, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The Definition of Quality and Approaches to Its Assessment. Volume 1. Explorations in Quality Assessment and Monitoring; Health Administration: Chicago, IL, USA, 1980. [Google Scholar]
- Lohr, K.N.; Schroeder, S.A. A Strategy for Quality Assurance in Medicare. N. Engl. J. Med. 1990, 322, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Nylenna, M.; Bjertnaes, Ø.A.; Saunes, I.S.; Lindahl, A.K. What is Good Quality of Health Care? Prof. Prof. 2015, 5, 1–16. [Google Scholar] [CrossRef]
- WHO. Quality of Care: A Process for Making Strategic Choices in Health Systems; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century; Institute of Medicine: Washington, DC, USA, 2001. [Google Scholar]
- Kelley, E.; Hurst, J. Health Care Quality Indicators Project: Conceptual Framework Paper. Mar. Sci. J. 2006, 23, 13–14. [Google Scholar]
- Mas, A.; Parra, P.; Bermejo, R.; Hidalgo, M.; Calle, J. Improving quality in healthcare: What makes a satisfied patient? Rev. Calid. Asist. 2016, 31, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Chougrani, S.; Ouhadj, S. Les questionnaires de sortie et la place des usagers dans le projet qualité à l’Établissement hospitalier universitaire d’Oran. Santé Publique 2014, 26, 499. [Google Scholar] [CrossRef] [PubMed]
- Frichi, Y.; Jawab, F.; Boutahari, S. Elaboration of an Association Matrix of Satisfaction Factors in Healthcare Facilities and Hospital Logistics Activities. In Proceedings of the 2018 International Colloquium on Logistics and Supply Chain Management (LOGISTIQUA), Tangier, Morocco, 26–27 April 2018; pp. 32–37. [Google Scholar]
- Norris, J.M.; White, D.E.; Nowell, L.; Mrklas, K.; Stelfox, H.T. How do stakeholders from multiple hierarchical levels of a large provincial health system define engagement? A qualitative study. Implement. Sci. 2017, 12, 98. [Google Scholar] [CrossRef] [PubMed]
- Tullberg, J. Stakeholder theory: Some revisionist suggestions. J. Socio. Econ. 2013, 42, 127–135. [Google Scholar] [CrossRef]
- Freeman, R.E. Strategic Management: A Stakeholder Approach; Cambridge University Press: Boston, MA, USA, 1984. [Google Scholar]
- Dos Muchangos, L.S.; Tokai, A.; Hanashima, A. Stakeholder analysis and social network analysis to evaluate the stakeholders of a MSWM system—A pilot study of Maputo City. Environ. Dev. 2017, 24, 124–135. [Google Scholar] [CrossRef]
- Fritz, M.M.; Rauter, R.; Baumgartner, R.J.; Dentchev, N. A supply chain perspective of stakeholder identification as a tool for responsible policy and decision-making. Environ. Sci. Policy 2018, 81, 63–76. [Google Scholar] [CrossRef]
- Mitchell, R.K.; Agle, B.R.; Wood, D.J. Toward a Theory of Stakeholder Identification and Salience: Defining the Principle of who and What Really Counts. Acad. Manag. Rev. 1997, 22, 853–886. [Google Scholar] [CrossRef]
- Kochan, T.A.; Rubinstein, S.A. Toward a Stakeholder Theory of the Firm: The Saturn Partnership. Organ. Sci. 2000, 11, 367–386. [Google Scholar] [CrossRef]
- Sobczak, A.; Girard, C. Pour une cartographie des parties prenantes fondée sur leur engagement: Une application aux sociétaires d’une banque mutualiste française. Manag. Avenir. 2010, 33, 157. [Google Scholar]
- Näsi, J.; Carroll, A.B. Understanding Stakeholder Thinking: Themes from a Finnish Conference. Bus. Ethic Eur. Rev. 1997, 6, 46–51. [Google Scholar]
- Ng, J.; Scahill, S.; Harrison, J. Stakeholder views do matter: A conceptual framework for medication safety measurement. J. Pharm. Health Serv. Res. 2018, 9, 21–31. [Google Scholar] [CrossRef]
- Ong, S.E.; Tyagi, S.; Lim, J.M.; Chia, K.S.; Legido-Quigley, H.; Lim, M.J.; Chia, S.K. Health systems reforms in Singapore: A qualitative study of key stakeholders. Health Policy 2018, 122, 431–443. [Google Scholar] [CrossRef] [PubMed]
- Franco-Trigo, L.; Hossain, L.; Durks, D.; Fam, D.; Inglis, S.; Benrimoj, S.; Sabater-Hernández, D. Stakeholder analysis for the development of a community pharmacy service aimed at preventing cardiovascular disease. Res. Soc. Adm. Pharm. 2017, 13, 539–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, A.B.; Brunner, J.; Cain, C.; Chuang, E.; Luger, T.M.; Canelo, I.; Rubenstein, L.; Yano, E.M. Engaging multilevel stakeholders in an implementation trial of evidence-based quality improvement in VA women’s health primary care. Transl. Behav. Med. 2017, 7, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Symmank, C.; Krause, J.; Gurtner, S. Stakeholder Variety in Healthcare and Their Integration in the Medical Device Development Process. In Challenges and Opportunities in Health Care Management; Gurtner, S., Soyez, K., Eds.; Springer: Berlin/Heidelberg, Germany, 2015; pp. 247–258. [Google Scholar]
- Concannon, T.W.; Meissner, P.; Grunbaum, J.A.; McElwee, N.; Guise, J.M.; Santa, J.; Conway, P.H.; Daudelin, D.; Morrato, E.H.; Leslie, L.K. A New Taxonomy for Stakeholder Engagement in Patient-Centered Outcomes Research. J. Gen. Intern. Med. 2012, 27, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Frullani, Y.; Pitet, L. Pharmacien, un savoir-faire, un objectif: Satisfaire les patients. Actual. Pharm. 2015, 54, 40–43. [Google Scholar] [CrossRef]
- Pergolotti, M.; Lyons, K.D.; Williams, G.R. Moving beyond symptom management towards cancer rehabilitation for older adults: Answering the 5W’s. J. Geriatr. Oncol. 2018, 9, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Sabtu, N.; Enoch, D.A.; Brown, N.M. Antibiotic resistance: What, why, where, when and how? Br. Med. Bull. 2015, 116, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.; Hunter, D. Consensus methods for medical and health services research. BMJ 1995, 311, 376–380. [Google Scholar] [CrossRef]
- Caire, J.M. Les différentes possibilités de la technique DELPHI. Rev. Francoph. Rech. Ergothérapie 2016, 2, 45–51. [Google Scholar]
- Okoli, C.; Pawlowski, S.D. The Delphi method as a research tool: An example, design considerations and applications. Inf. Manag. 2004, 42, 15–29. [Google Scholar] [CrossRef]
- Si, S.L.; You, X.Y.; Liu, H.C.; Zhang, P. DEMATEL Technique: A Systematic Review of the State-of-the-Art Literature on Methodologies and Applications. Math. Probl. Eng. 2018, 2018, 1–33. [Google Scholar] [CrossRef] [Green Version]
- Gardas, B.B.; Raut, R.D.; Narkhede, B. Modelling the challenges to sustainability in the textile and apparel (T&A) sector: A Delphi-DEMATEL approach. Sustain. Prod. Consum. 2018, 15, 96–108. [Google Scholar]
- Bhatia, S.M.; Srivastava, R.K. Analysis of external barriers to remanufacturing using grey-DEMATEL approach: An Indian perspective. Resour. Conserv. Recycl. 2018, 136, 79–87. [Google Scholar] [CrossRef]
- Wei, D.; Liu, H.; Shi, K. What are the key barriers for the further development of shale gas in China? A grey-DEMATEL approach. Energy Rep. 2019, 5, 298–304. [Google Scholar] [CrossRef]
- Govindan, K.; Chaudhuri, A. Interrelationships of risks faced by third party logistics service providers: A DEMATEL based approach. Transp. Res. Part. E Logist. Transp. Rev. 2016, 90, 177–195. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.C.; You, J.X.; Lu, C.; Chen, Y.Z. Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision making model. Renew. Sustain. Energy Rev. 2015, 41, 932–942. [Google Scholar] [CrossRef]
- Shieh, J.I.; Wu, H.H.; Huang, K.K. A DEMATEL method in identifying key success factors of hospital service quality. Knowl. Based Syst. 2010, 23, 277–282. [Google Scholar] [CrossRef]
- Zhou, Q.; Huang, W.; Zhang, Y. Identifying critical success factors in emergency management using a fuzzy DEMATEL method. Saf. Sci. 2011, 49, 243–252. [Google Scholar] [CrossRef]
- Frichi, Y.; Jawab, F.; Boutahari, S. Identification of Health System Stakeholders in Morocco. In Proceedings of the International Conference on Industrial Engineering and Operations Management, Bangkok, Thailand, 5–7 March 2019; pp. 1193–1199. [Google Scholar]
- Duong, M.H.; Moles, R.J.; Chaar, B.; Chen, T.F. Stakeholder roles in facilitating access to essential medicines. Res. Soc. Adm. Pharm. 2019, 15, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.Q.; Medaglia, R. Mapping the challenges of Artificial Intelligence in the public sector: Evidence from public healthcare. Gov. Inf. Q. 2019, 36, 368–383. [Google Scholar] [CrossRef]
- Khan, N.; Puthussery, S. Stakeholder perspectives on public-private partnership in health service delivery in Sindh province of Pakistan: A qualitative study. Public Health 2019, 170, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Musyimi, C.W.; Mutiso, V.N.; Nyamai, D.N.; Ebuenyi, I.D.; Ndetei, D.M. Integration of Traditional Birth Attendants into Mental Healthcare: A Multistakeholder Qualitative Study Exploration. BioMed Res. Int. 2019, 2019, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Martin, G.P.; Chew, S.; Dixon-Woods, M. Senior stakeholder views on policies to foster a culture of openness in the English National Health Service: A qualitative interview study. J. R. Soc. Med. 2019, 112, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Brousselle, A.; Contandriopoulos, D.; Haggerty, J.; Breton, M.; Rivard, M.; Beaulieu, M.D.; Champagne, G.; Perroux, M. Stakeholder Views on Solutions to Improve Health System Performance. Healthc. Policy Polit. St. 2018, 14, 71–85. [Google Scholar] [CrossRef]
- Franklin, P.D.; Chenok, K.E.; Lavalee, D.; Love, R.; Paxton, L.; Segal, C.; Holve, E. Framework to Guide the Collection and Use of Patient-Reported Outcome Measures. In the Learning Healthcare System. eGEMs 2017, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- Trevino, K.M.; Healy, C.; Martin, P.; Canin, B.; Pillemer, K.; Sirey, J.A.; Reid, M.C. Improving implementation of psychological interventions to older adult patients with cancer: Convening older adults, caregivers, providers, researchers. J. Geriatr. Oncol. 2018, 9, 423–429. [Google Scholar] [CrossRef]
- Carello, G.; Lanzarone, E.; Mattia, S. Trade-off between stakeholders’ goals in the home care nurse-to-patient assignment problem. Oper. Res. Health Care 2018, 16, 29–40. [Google Scholar] [CrossRef]
- Parimbelli, E.; Bottalico, B.; Losiouk, E.; Tomasi, M.; Santosuosso, A.; Lanzola, G.; Quaglini, S.; Bellazzi, R. Trusting telemedicine: A discussion on risks, safety, legal implications and liability of involved stakeholders. Int. J. Med. Inform. 2018, 112, 90–98. [Google Scholar] [CrossRef]
- Van Veenendaal, H.; Van Der Weijden, T.; Ubbink, D.T.; Stiggelbout, A.M.; Van Mierlo, L.A.; Hilders, C.G. Accelerating implementation of shared decision-making in the Netherlands: An exploratory investigation. Patient Educ. Couns. 2018, 101, 2097–2104. [Google Scholar] [CrossRef] [Green Version]
- Mayo, C.S.; Moran, J.M.; Bosch, W.; Xiao, Y.; McNutt, T.; Popple, R.; Michalski, J.; Feng, M.; Marks, L.B.; Fuller, C.D.; et al. American Association of Physicists in Medicine Task Group 263: Standardizing Nomenclatures in Radiation Oncology. Int. J. Radiat. Oncol. 2018, 100, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Reddy, A.; Lester, C.A.; Stone, J.A.; Holden, R.J.; Phelan, C.H.; Chui, M.A. Applying participatory design to a pharmacy system intervention. Res. Soc. Adm. Pharm. 2018. [Google Scholar] [CrossRef] [PubMed]
- Habli, I.; White, S.; Sujan, M.; Harrison, S.; Ugarte, M. What is the safety case for health IT? A study of assurance practices in England. Saf. Sci. 2018, 110, 324–335. [Google Scholar] [CrossRef] [Green Version]
- Hébert, G.J.; Colasante, C.; Ilse, R.G.; Forster, A.J. Using structured incentives to increase value for money in an academic health sciences centre. Health Manag. Forum 2017, 30, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Van Schendel, R.V.; Van El, C.G.; Pajkrt, E.; Henneman, L.; Cornel, M.C. Implementing non-invasive prenatal testing for aneuploidy in a national healthcare system: Global challenges and national solutions. BMC Health Serv. Res. 2017, 17, 670. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, L.; Bergström, A.; Hoa, D.T.P.; Nga, N.T.; Eldh, A.C. Sustainability of knowledge implementation in a low- and middle- income context: Experiences from a facilitation project in Vietnam targeting maternal and neonatal health. PLoS ONE 2017, 12, e0182626. [Google Scholar] [CrossRef] [PubMed]
- Mazor, K.M.; Richards, A.; Gallagher, M.; Arterburn, D.E.; Raebel, M.A.; Nowell, W.B.; Curtis, J.R.; Paolino, A.R.; Toh, S. Stakeholders’ Views on Data Sharing in Multi-Center Studies. J. Comp. Eff. Res. 2017, 6, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Toumi, M.; Rémuzat, C. Value added medicines: What value repurposed medicines might bring to society? J. Mark. Access Health Policy 2017, 5, 1264717. [Google Scholar] [CrossRef] [PubMed]
- Gardarsdottir, H.; Bekker, C.L.; Egberts, T.C.; Bouvy, M.L.; Van den Bemt, B.J. Redispensing of medicines unused by patients: A qualitative study among stakeholders. Int. J. Clin. Pharm. 2017, 39, 196–204. [Google Scholar]
- Hossain, L.N.; Tudball, J.; Franco-Trigo, L.; Durks, D.; Benrimoj, S.I.; Sabater-Hernández, D. A multilevel stakeholder approach for identifying the determinants of implementation of government-funded community pharmacy services at the primary care level. Res. Soc. Adm. Pharm. 2017, 14, 765–775. [Google Scholar] [CrossRef]
- Denburg, A.; Wilson, M.G.; Johnson, I.S.; Kutluk, T.; Torode, J.; Gupta, S. Advancing the development of national childhood cancer care strategies in Latin America. J. Cancer Policy 2017, 12, 7–15. [Google Scholar] [CrossRef]
- Davidson, G.H.; Austin, E.; Thornblade, L.; Simpson, L.; Ong, T.D.; Pan, H.; Flum, D.R. Improving transitions of care across the spectrum of healthcare delivery: A multidisciplinary approach to understanding variability in outcomes across hospitals and skilled nursing facilities. Am. J. Surg. 2017, 213, 910–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foley, C.; Droog, E.; Healy, O.; McHugh, S.; Buckley, C.; Browne, J.P. Understanding perspectives on major system change: A comparative case study of public engagement and the implementation of urgent and emergency care system reconfiguration. Health Policy 2017, 121, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Gagnon, M.P.; Payne-Gagnon, J.; Breton, E.; Fortin, J.P.; Khoury, L.; Dolovich, L.; Price, D.; Wiljer, D.; Bartlett, G.; Archer, N. Adoption of Electronic Personal Health Records in Canada: Perceptions of Stakeholders. Int. J. Health Policy Manag. 2016, 5, 425–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Rourke, T.; Higuchi, K.S.; Hogg, W. Stakeholder Participation in System Change: A New Conceptual Model. Worldviews Evid. Nurs. 2016, 13, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Helena, R. Cross-border healthcare directive: Assessing stakeholders’ perspectives in Poland and Portugal. Health Policy 2016, 120, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Yassoub, R.; Alameddine, M.; Saleh, S. The Path Toward Universal Health Coverage: Stakeholder Acceptability of a Primary Care Health Benefits Package in Lebanon. Int. J. Health Serv. 2016, 47, 352–373. [Google Scholar]
- Stelfox, H.T.; Niven, D.J.; Clement, F.M.; Bagshaw, S.M.; Cook, D.J.; McKenzie, E.; Potestio, M.L.; Doig, C.J.; O’Neill, B.; Zygun, D. Stakeholder Engagement to Identify Priorities for Improving the Quality and Value of Critical Care. PLoS ONE 2015, 10, e0140141. [Google Scholar] [CrossRef]
- Ovseiko, P.V.; Buchan, A.M. Medical workforce education and training: A failed decentralisation attempt to reform organisation, financing, and planning in England. Health Policy 2015, 119, 1545–1549. [Google Scholar] [CrossRef]
- Bond, R.R.; Mulvenna, M.D.; Finlay, D.D.; Martin, S. Multi-faceted informatics system for digitising and streamlining the reablement care model. J. Biomed. Inform. 2015, 56, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Andriopoulou, F.G.; Birkos, K.; Lymberopoulos, D. Computers in Industry P2Care: A dynamic peer-to-peer network for collaboration in personalized healthcare service delivery. Comput. Ind. 2015, 69, 45–60. [Google Scholar] [CrossRef]
- Saleem, J.J.; Plew, W.R.; Speir, R.C.; Herout, J.; Wilck, N.R.; Ryan, D.M.; Cullen, T.A.; Scott, J.M.; Beene, M.S.; Phillips, T. Understanding Barriers and Facilitators to the use of Clinical Information Systems for Intensive Care Units and Anesthesia Record Keeping: A Rapid Ethnography. Int. J. Med. Inform. 2015, 84, 500–511. [Google Scholar] [CrossRef] [PubMed]
- Caniato, M.; Tudor, T.; Vaccari, M. Understanding the perceptions, roles and interactions of stakeholder networks managing health-care waste: A case study of the Gaza Strip. Waste Manag. 2015, 35, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Ibn El Farouk, I.; Talbi, A.; Jawab, F. Modeling and simulation of hospital supply chain: State of the art and research perspectives. In Proceedings of the 2011 4th International Conference on Logistics, Hammamet, Tunisia, 31 May–3 June 2011; pp. 287–291. [Google Scholar]
- WHO. The World Health Report 2000–Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Madison, K. Patients as regulators? Patients’ evolving influence over health care delivery. J. Leg. Med. 2010, 31, 9–34. [Google Scholar] [CrossRef] [PubMed]
- Pomey, M.P.; Hihat, H.; Khalifa, M.; Lebel, P.; Néron, A.; Dumez, V. Patient partnership in quality improvement of healthcare services: Patients’ inputs and challenges faced. Patient Exp. J. 2015, 2, 29–42. [Google Scholar] [CrossRef]
- Farrag, A.; Harris, Y. A discussion of the United States’ and Egypt’s health care quality improvement efforts. Int. J. Health Manag. 2019, 29, 1–8. [Google Scholar] [CrossRef]
- WHO. The Role of Government in Health Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Lupo, T. A fuzzy framework to evaluate service quality in the healthcare industry: An empirical case of public hospital service evaluation in Sicily. Appl. Soft Comput. 2016, 40, 468–478. [Google Scholar] [CrossRef]
- Piligrimienė, Ž.; Bučiūnienė, I. Different Perspectives on Health Care Quality: Is the Consensus Possible? Eng. Econ. 2008, 1, 104–111. [Google Scholar]

| Dimension | Definition | Observable Indicators |
|---|---|---|
| (1) Effectiveness | Health care is based on current scientific knowledge and provided to those in need. |
|
| (2) Safety | The extent to which health care processes avoid and prevent adverse events. |
|
| (3) Efficiency | Health care is produced with optimal use of available resources to achieve the best results. |
|
| (4) Accessibility | The availability of healthcare services and the ease with which they are reached (physical, financial, psychological accessibility). |
|
| (5) Patient-leftedness | The extent to which healthcare delivery takes into account patient preferences, values and choices. |
|
| (6) Equity | Services quality does not vary because of patients’ personal characteristics such as gender, ethnicity, geographical location and socio-economic status. |
|
| Ref | Objective | Country | Main HSS Groups |
| [49] | Examine stakeholders’ roles to facilitate access to essential medicines. | Australia |
|
| [50] | Mapping challenges related to the adoption of Artificial Intelligence in the public health sector. | China | |
| [51] | Exploring stakeholders’ perspectives on public-private partnership in health service delivery in the Pakistani context. | Pakistan | |
| [52] | Studying the feasibility of integrating traditional birth attendants into maternal mental healthcare. | Kenya | |
| [53] | Examine the openness of health policies in terms of integrating the employees voice. | England | |
| [54] | Analysis of stakeholders’ views on proposed solutions to improve the performance of the Quebec health system. | Canada | |
| [55] | Proposition of a framework to guide the collection, planning of the implementation and use of Patient-Reported Outcome Measures. | USA | |
| [56] | Identification of barriers and strategies for implementing psychological interventions for older adults with cancer. | USA | |
| [57] | Modeling the nurse-to-patient assignment problem in home care under continuity of care while taking into consideration stakeholders’ perspectives. | Italy | |
| [58] | Discussing risks and legal implications of using modern telemedicine systems. | Italy | |
| [59] | Formulation and prioritization of strategies for the implementation of Shared Decision Making, based on the identification of obstacles to change. | Netherlands | |
| [60] | Establishment of guidelines for the development of radiation oncology nomenclature for clinical trials, data sharing initiatives, and population-based studies. | USA | |
| [61] | Description of a blueprint for the use of participatory design in the design of community pharmacy interventions. | USA | |
| [29] | Identification of challenges and opportunities for the implementation of regional health systems. | Singapore | |
| [62] | Analysis of health information technology safety assurance practices. | England | |
| [30] | Stakeholder analysis to identify a planning group for the development of community pharmacy service to prevent cardiovascular disease. | Australia | |
| [63] | Development of an innovative system of structured incentives model in an academic health sciences center, linking distribution of government payments to quality and performance outcomes. | Canada | |
| [64] | Identification of challenges in the implementation of non-invasive prenatal testing for fetal aneuploidy. | Netherlands | |
| [65] | Identification of factors promoting or hindering the sustainability of the implementation of knowledge implementation strategies in low- and middle-income contexts. | Vietnam | |
| [66] | Analysis of stakeholders’ opinions on the benefits and risks of data sharing in multicenter comparative efficacy research studies. | USA | |
| [19] | Studying stakeholders’ understanding of engagement in care improvement initiatives. | Canada | |
| [67] | Evaluation of the value and potential of drug repositioning. | European Union | |
| [68] | Analysis of stakeholders’ opinions on the Redispensing of medicines unused by patients, and their reuse by other patients. | Netherlands | |
| [31] | Engaging stakeholders to adapt patient-centered home care tenets for veterans to the needs of women veterans. | USA | |
| [69] | Identification of key determinants of practice influencing the implementation of community pharmacy services in the primary care network. | Australia | |
| [70] | Identification of the main problems and potential solutions to the implementation of national strategies for childhood cancer in Latin America. | Latin America | |
| [71] | Improving coordination between health care facilities in patient transition by identifying factors that lead to poor clinical outcomes. | USA | |
| [72] | Analysis of the views of different stakeholders on public engagement in the reconfiguration of emergency care systems. | Ireland | |
| [73] | Description of the current status of the use of electronic personal health records and identification of facilitators and barriers to their adoption. | Canada | |
| [74] | Analyzing stakeholder perspectives and participation in the health system change process that led to the introduction of the first Nurse Practitioner-Led clinics in Ontario. | Canada | |
| [75] | Analysis of stakeholders’ views on the European Union’s cross-border healthcare directive. | European Union | |
| [76] | Determination of the health benefits package to be included in universal health coverage that is acceptable and sustainable to stakeholders. | Lebanon | |
| [77] | Identification and prioritization of gaps between current scientific evidence and the actual care provided, as well as opportunities to improve the QC. | Canada | |
| [78] | Discussion and analysis of the reform on the organization, financing and planning of medical workforce education in England during the Conservative and Liberal Democrat coalition government’s time in office. | England | |
| [79] | Establishment of a comprehensive set of design requirements for digital reablement system to increase the home autonomy of older people. | England | |
| [80] | Proposal and development of a decentralized information system for collaboration purposes linking medical providers, paramedical providers and patients for personalized quality services. | Greece | |
| [81] | Understanding and analyzing facilitators and barriers to the adoption and use of clinical information systems in intensive care units. | USA | |
| [82] | Understanding and examining the manner in which function the networks managing health-care waste. | Palestine |
| What | ||
|---|---|---|
| Identification of Organizations, Institutions, Individuals and Groups of Individuals Who Have an Influence or are Influenced by Health System Actions in Morocco. | ||
| Who | Why | Where |
| Government: Ministries of Health, Economy and Finance, Interior, National Defense, Transport, Education, Agriculture, etc. | Responsible for the development and implementation of national health strategies. It defines the budget allocated to the implementation of health programs and ensures its monitoring and control. The government is accountable for opening up the isolated rural areas through its policies of road network development and transportation. It is also responsible for education and scientific research development strategies. | Strategic |
| Parliament | It is the legislative institution that passes laws, oversees government actions, and evaluates public policies, particularly those related to the health sector. | Strategic |
| Regional and Provincial Directorates of Ministries | Responsible for the implementation of national policies in their territories. | Tactical |
| Local authorities: Regions, Wilayas, prefectures, provinces and municipalities | Participate in the regional and local implementation of national policies and strategies in the health, education, and transportation sectors, etc. They ensure the diagnosis of health and hygiene needs and the maintenance of rural roads. They also manage urban transportation, patients and deceased transportation, etc. | Tactical and operational |
| Public and private healthcare facilities: Basic health care centers network, hospital networks, hospital clinics, hemodialysis centers, laboratories, pharmacies, etc. | Provide preventive, curative and promotional care services (consultations, nursing care, chronic disease follow-up, etc.). They also contribute to medical and pharmaceutical training activities. | Operational |
| Health insurance bodies: National Agency of Health Insurance (NAHI), Moroccan Health Insurance Fund (MHIF), National Fund for Social Security (NFSS), private supplementary health insurance companies. | The NAHI ensures the proper functioning of the medical coverage system by providing technical support for the obligatory health insurance. It also manages the regime of medical aid to poor populations. The MHIF manages the obligatory health insurance for civil servants and students. The NFSS manages the obligatory health insurance for employees of private enterprises and self-employed persons. | Strategic, tactical, and operational |
| Training and research institutions: Universities, Faculties of Medicine and Pharmacy, Health Career Training Institutes, National School of Public Health, Pasteur Institute of Morocco, Learned societies, etc. | Provide initial and in-service training in various medical, managerial and technical disciplines. They also develop research in health sciences. | Tactical and operational |
| International health organizations: WHO, UNICEF, UNAIDS, World Bank, etc. | Provide technical and financial assistance to the State for the development of health policies and the implementation of related programs. | Strategic Supranational |
| Patients and their families | Patients are the beneficiaries of healthcare services, but also any person acting on their behalf, in particular their families. | Operational |
| Patient advocates: consumer protection associations. | Promote consumers’ right to have access to clear, objective and fair information in particular with regard to service prices and safety. | Tactical and operational |
| Civil society organizations: NGOs and private not-for-profit entities working in the health field. | Help to reach disadvantaged populations and raise awareness of public health issues. | Tactical and operational |
| Health personnel: physicians, biologists, pharmacists, dentists, nurses, medical assistants, and administrative staff | Physicians are responsible, each within their respective areas of competence, for diagnosis and care, supervision of trainee physicians, prevention and health education. Nurses carry out medical prescriptions, provide nursing care and prepare the necessary equipment and products for medical analysis and care. The administrative staff is responsible for the management of administrative affairs. | Operational |
| Health personnel representatives: Order of Physicians, Order of Dentists, Order of Pharmacists, Trade unions, etc. | Professional Orders represent the medical professions vis-a-vis the government, participate in the development and implementation of health policy and defend the moral and professional interests of the medical/pharmaceutical profession. Trade unions protect the economic, industrial, commercial and professional interests of their members. | Tactical and operational |
| National consultation institutions: Economic, Social and Environmental Council (ESEC), National Observatory for Human Development (NOHD), National Human Rights Council (NHRC), etc. | The ESEC provides advisory services to the government on social and environmental policies. The NOHD analyses and evaluates the impact of human development programs. The NHRC sees to the observation, surveillance and monitoring of human rights. | Strategic |
| Healthcare industry: manufacturers, wholesalers, distributors and subcontractors | Responsible for product development, production, and distribution. They provide healthcare facilities with goods (medicines, medical supplies, equipment, etc.) and services (IT, maintenance, food services, cleaning, etc.), that are necessary for their operations and the production of care. | Tactical and operational |
| Employers | Provide workers with a healthy and safe working environment. They are responsible for implementing appropriate environmental and health protection measures against pollution generated by industrial activities. | Operational |
| Media | Contribute to the promotion of health information and public awareness. | Tactical and operational |
| N° | Affiliation | Position | Years of Experience | Degree | City |
|---|---|---|---|---|---|
| 1 | Regional Hospital | Quality manager | 13 | Doctor | Fez |
| 2 | Head of Medical Affairs Department | 17 | Doctor | Fez | |
| 3 | Administrator | 10 | Master | Fez | |
| 4 | Quality manager | 10 | Maser | Tangier | |
| 5 | Purchasing manager | 16 | Master | Fez | |
| 6 | Head of the Nursing Care Unit | 10 | Technician | Fez | |
| 7 | Ministry of Health | Administrator | 12 | Master | Rabat |
| 8 | University | Health researcher | 10 | Doctor | Casablanca |
| 9 | Health researcher | 11 | Doctor | Tangier | |
| 10 | Moroccan Association for Consumer Protection and Guidance | Member of the Association | 13 | Master | Kenitra |
| 11 | University Hospital | Head of Performance Evaluation Department | 24 | Master | Rabat |
| 12 | Prefectural Hospital | Quality manager | 15 | Doctor | Casablanca |
| 13 | Pasteur Institute | Health researcher | 11 | Doctor | Casablanca |
| 14 | Regional Oncology Centre | Administrator | 12 | Master | Meknes |
| 15 | Head of Medical Affairs Department | 23 | Doctor | Meknes | |
| 16 | Administrator | 12 | Master | Meknes |
| HSS | Influence on QC | Impact by QC | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Round | Second Round | Third Round | First Round | Second Round | Third Round | |||||||
| Mean(Mk) | Standard Deviation | Mean(Mk) | Standard Deviation | Mean(Mk) | Standard Deviation | Mean(Nk) | Standard Deviation | Mean(Nk) | Standard Deviation | Mean(Nk) | Standard Deviation | |
| HSS1: Government | 25.25 | 4.18 | 25.33 | 3.27 | 26.13 | 2.80 | 22.83 | 3.46 | 23.83 | 3.04 | 23.20 | 2.73 |
| HSS2: Parliament | 18.58 | 3.40 | 17.13 | 3.31 | 16.80 | 1.90 | 15.25 | 6.22 | 16.67 | 4.42 | 15.07 | 4.82 |
| HSS3: Regional and Provincial Directorates of Ministries of Health, Transport, Interior, etc. | 22.33 | 3.20 | 22.53 | 2.56 | 21.80 | 2.18 | 19.67 | 4.19 | 20.33 | 4.01 | 20.13 | 3.60 |
| HSS4: Local authorities | 16.17 | 2.92 | 16.00 | 1.51 | 16.00 | 1.51 | 14.17 | 5.25 | 15.17 | 3.30 | 13.87 | 4.60 |
| HSS5: Public and private healthcare facilities | 19.00 | 2.95 | 19.53 | 2.59 | 19.47 | 2.00 | 20.75 | 4.45 | 20.08 | 3.50 | 20.67 | 3.44 |
| HSS6: Health insurance bodies | 17.50 | 3.18 | 17.93 | 1.94 | 18.27 | 1.75 | 19.00 | 4.16 | 18.42 | 3.65 | 18.00 | 3.27 |
| HSS7: Training and research institutions | 17.33 | 3.17 | 17.80 | 1.70 | 17.47 | 1.81 | 13.42 | 4.34 | 13.33 | 4.12 | 12.87 | 3.83 |
| HSS8: International health organizations | 20.00 | 3.64 | 18.67 | 2.35 | 18.27 | 2.09 | 16.25 | 4.94 | 16.00 | 4.71 | 15.00 | 3.72 |
| HSS9: Patients and their families | 21.92 | 3.94 | 19.87 | 2.26 | 20.60 | 2.23 | 26.83 | 2.92 | 27.92 | 2.43 | 27.80 | 2.31 |
| HSS10: Patient advocates | 20.00 | 2.95 | 17.33 | 2.87 | 19.07 | 1.71 | 15.50 | 2.94 | 14.75 | 2.18 | 15.80 | 2.04 |
| HSS11: Civil society organizations | 18.33 | 2.10 | 18.00 | 1.46 | 18.00 | 1.46 | 14.17 | 4.45 | 14.92 | 4.25 | 14.93 | 3.47 |
| HSS12: Health personnel | 26.42 | 3.82 | 25.73 | 2.94 | 26.53 | 2.80 | 21.50 | 4.42 | 23.92 | 4.52 | 23.60 | 3.87 |
| HSS13: Health personnel representatives | 18.75 | 3.02 | 17.53 | 2.20 | 17.53 | 2.20 | 17.00 | 3.79 | 17.67 | 3.20 | 16.80 | 2.86 |
| HSS14: Employers | 14.00 | 3.16 | 13.40 | 1.96 | 12.87 | 1.92 | 12.00 | 4.00 | 11.50 | 3.21 | 11.07 | 2.81 |
| HSS15: Healthcare industry | 17.08 | 2.75 | 16.80 | 2.01 | 16.93 | 2.02 | 13.00 | 2.63 | 13.25 | 2.30 | 12.73 | 2.22 |
| HSS16: National consultation institutions | 14.83 | 3.97 | 13.80 | 2.54 | 13.80 | 2.54 | 11.17 | 4.34 | 11.00 | 4.11 | 10.53 | 3.66 |
| HSS17: Media | 16.50 | 3.61 | 16.27 | 2.22 | 16.27 | 2.12 | 9.58 | 4.25 | 9.42 | 3.82 | 9.33 | 3.22 |
| Kendall’s W coefficient of concordance | 0.468 | 0.626 | 0.705 | 0.560 | 0.665 | 0.708 | ||||||
| HSS1 | HSS2 | HSS3 | HSS4 | HSS5 | HSS6 | HSS7 | HSS8 | HSS9 | HSS10 | HSS11 | HSS12 | HSS13, | HSS14 | HSS15 | HSS16, | HSS17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HSS1 | 0.0000 | 0.6667 | 4.0000 | 2.0000 | 3.0000 | 3.0000 | 3.6667 | 1.3333 | 4.0000 | 1.3333 | 2.3333 | 4.0000 | 2.6667 | 3.3333 | 3.0000 | 0.6667 | 2.0000 |
| HSS2 | 2.3333 | 0.0000 | 0.6667 | 1.3333 | 1.0000 | 0.6667 | 0.6667 | 0.3333 | 1.6667 | 1.6667 | 1.3333 | 1.6667 | 1.0000 | 2.0000 | 0.6667 | 1.3333 | 0.3333 |
| HSS3 | 0.6667 | 0.0000 | 0.0000 | 0.6667 | 4.0000 | 0.0000 | 1.3333 | 0.3333 | 4.0000 | 0.3333 | 1.0000 | 2.6667 | 0.6667 | 0.0000 | 1.6667 | 0.0000 | 0.3333 |
| HSS4 | 0.3333 | 0.0000 | 1.3333 | 0.0000 | 0.6667 | 0.0000 | 0.3333 | 0.0000 | 3.6667 | 0.0000 | 1.3333 | 0.6667 | 0.0000 | 1.0000 | 0.0000 | 0.0000 | 0.3333 |
| HSS5 | 0.6667 | 0.0000 | 1.3333 | 0.3333 | 0.0000 | 1.3333 | 2.0000 | 1.6667 | 4.0000 | 0.3333 | 0.6667 | 4.0000 | 1.6667 | 0.0000 | 2.0000 | 0.0000 | 0.6667 |
| HSS6 | 0.3333 | 0.0000 | 0.0000 | 0.0000 | 1.0000 | 0.0000 | 0.0000 | 0.6667 | 4.0000 | 0.0000 | 0.0000 | 0.3333 | 0.3333 | 0.0000 | 2.6667 | 0.0000 | 0.0000 |
| HSS7 | 0.6667 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.3333 | 0.0000 | 1.6667 | 3.6667 | 0.0000 | 0.0000 | 1.3333 | 0.3333 | 0.0000 | 2.3333 | 0.0000 | 0.0000 |
| HSS8 | 2.6667 | 0.3333 | 1.3333 | 0.3333 | 2.0000 | 1.3333 | 1.3333 | 0.0000 | 3.0000 | 0.0000 | 1.0000 | 3.3333 | 2.3333 | 0.0000 | 3.0000 | 1.3333 | 0.3333 |
| HSS9 | 2.3333 | 2.0000 | 1.6667 | 2.3333 | 1.0000 | 0.3333 | 0.6667 | 0.3333 | 0.0000 | 1.3333 | 1.3333 | 2.3333 | 0.6667 | 0.0000 | 0.6667 | 0.6667 | 0.3333 |
| HSS10 | 1.6667 | 0.6667 | 2.3333 | 0.3333 | 2.3333 | 0.0000 | 0.0000 | 0.3333 | 2.0000 | 0.0000 | 0.3333 | 1.0000 | 1.6667 | 0.3333 | 1.3333 | 0.0000 | 0.6667 |
| HSS11 | 0.6667 | 0.6667 | 0.0000 | 0.6667 | 0.0000 | 0.0000 | 0.0000 | 1.3333 | 3.6667 | 1.3333 | 0.0000 | 1.3333 | 0.6667 | 1.6667 | 0.0000 | 0.0000 | 1.6667 |
| HSS12 | 0.6667 | 0.0000 | 1.3333 | 0.0000 | 1.6667 | 1.6667 | 1.0000 | 1.6667 | 4.0000 | 0.0000 | 0.3333 | 0.0000 | 3.3333 | 0.0000 | 1.3333 | 0.0000 | 0.0000 |
| HSS13 | 2.3333 | 0.3333 | 1.6667 | 0.3333 | 2.0000 | 0.3333 | 0.6667 | 1.6667 | 3.3333 | 0.3333 | 0.3333 | 3.6667 | 0.0000 | 0.0000 | 1.6667 | 0.0000 | 0.0000 |
| HSS14 | 0.6667 | 0.3333 | 0.0000 | 1.0000 | 0.0000 | 3.0000 | 0.0000 | 0.0000 | 4.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| HSS15 | 2.0000 | 0.3333 | 1.6667 | 0.0000 | 2.6667 | 2.6667 | 0.6667 | 0.6667 | 4.0000 | 0.0000 | 0.0000 | 0.6667 | 1.3000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| HSS16 | 1.3333 | 0.0000 | 1.3333 | 1.0000 | 1.6667 | 1.3333 | 0.3333 | 0.0000 | 2.3333 | 0.3333 | 0.0000 | 0.6667 | 0.3333 | 1.3333 | 0.6667 | 0.0000 | 0.0000 |
| HSS17 | 1.6667 | 1.6667 | 0.3333 | 0.6667 | 1.0000 | 0.6667 | 0.0000 | 0.0000 | 2.6667 | 0.6667 | 0.3333 | 0.6667 | 0.3333 | 0.0000 | 0.3333 | 0.0000 | 0.0000 |
| HSS1 | HSS2 | HSS3 | HSS4 | HSS5 | HSS6 | HSS7 | HSS8 | HSS9 | HSS10 | HSS11 | HSS12 | HSS13 | HSS14 | HSS15 | HSS16 | HSS17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HSS1 | 0.0000 | 0.0123 | 0.0741 | 0.0370 | 0.0556 | 0.0556 | 0.0679 | 0.0247 | 0.0741 | 0.0247 | 0.0432 | 0.0741 | 0.0494 | 0.0617 | 0.0556 | 0.0123 | 0.0370 |
| HSS2 | 0.0432 | 0.0000 | 0.0123 | 0.0247 | 0.0185 | 0.0123 | 0.0123 | 0.0062 | 0.0309 | 0.0309 | 0.0247 | 0.0309 | 0.0185 | 0.0370 | 0.0123 | 0.0247 | 0.0062 |
| HSS3 | 0.0123 | 0.0000 | 0.0000 | 0.0123 | 0.0741 | 0.0000 | 0.0247 | 0.0062 | 0.0741 | 0.0062 | 0.0185 | 0.0494 | 0.0123 | 0.0000 | 0.0309 | 0.0000 | 0.0062 |
| HSS4 | 0.0062 | 0.0000 | 0.0247 | 0.0000 | 0.0123 | 0.0000 | 0.0062 | 0.0000 | 0.0679 | 0.0000 | 0.0247 | 0.0123 | 0.0000 | 0.0185 | 0.0000 | 0.0000 | 0.0062 |
| HSS5 | 0.0123 | 0.0000 | 0.0247 | 0.0062 | 0.0000 | 0.0247 | 0.0370 | 0.0309 | 0.0741 | 0.0062 | 0.0123 | 0.0741 | 0.0309 | 0.0000 | 0.0370 | 0.0000 | 0.0123 |
| HSS6 | 0.0062 | 0.0000 | 0.0000 | 0.0000 | 0.0185 | 0.0000 | 0.0000 | 0.0123 | 0.0741 | 0.0000 | 0.0000 | 0.0062 | 0.0062 | 0.0000 | 0.0494 | 0.0000 | 0.0000 |
| HSS7 | 0.0123 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0062 | 0.0000 | 0.0309 | 0.0679 | 0.0000 | 0.0000 | 0.0247 | 0.0062 | 0.0000 | 0.0432 | 0.0000 | 0.0000 |
| HSS8 | 0.0494 | 0.0062 | 0.0247 | 0.0062 | 0.0370 | 0.0247 | 0.0247 | 0.0000 | 0.0556 | 0.0000 | 0.0185 | 0.0617 | 0.0432 | 0.0000 | 0.0556 | 0.0247 | 0.0062 |
| HSS9 | 0.0432 | 0.0370 | 0.0309 | 0.0432 | 0.0185 | 0.0062 | 0.0123 | 0.0062 | 0.0000 | 0.0247 | 0.0247 | 0.0432 | 0.0123 | 0.0000 | 0.0123 | 0.0123 | 0.0062 |
| HSS10 | 0.0309 | 0.0123 | 0.0432 | 0.0062 | 0.0432 | 0.0000 | 0.0000 | 0.0062 | 0.0370 | 0.0000 | 0.0062 | 0.0185 | 0.0309 | 0.0062 | 0.0247 | 0.0000 | 0.0123 |
| HSS11 | 0.0123 | 0.0123 | 0.0000 | 0.0123 | 0.0000 | 0.0000 | 0.0000 | 0.0247 | 0.0679 | 0.0247 | 0.0000 | 0.0247 | 0.0123 | 0.0309 | 0.0000 | 0.0000 | 0.0309 |
| HSS12 | 0.0123 | 0.0000 | 0.0247 | 0.0000 | 0.0309 | 0.0309 | 0.0185 | 0.0309 | 0.0741 | 0.0000 | 0.0062 | 0.0000 | 0.0617 | 0.0000 | 0.0247 | 0.0000 | 0.0000 |
| HSS13 | 0.0432 | 0.0062 | 0.0309 | 0.0062 | 0.0370 | 0.0062 | 0.0123 | 0.0309 | 0.0617 | 0.0062 | 0.0062 | 0.0679 | 0.0000 | 0.0000 | 0.0309 | 0.0000 | 0.0000 |
| HSS14 | 0.0123 | 0.0062 | 0.0000 | 0.0185 | 0.0000 | 0.0556 | 0.0000 | 0.0000 | 0.0741 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| HSS15 | 0.0370 | 0.0062 | 0.0309 | 0.0000 | 0.0494 | 0.0494 | 0.0123 | 0.0123 | 0.0741 | 0.0000 | 0.0000 | 0.0123 | 0.0241 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| HSS16 | 0.0247 | 0.0000 | 0.0247 | 0.0185 | 0.0309 | 0.0247 | 0.0062 | 0.0000 | 0.0432 | 0.0062 | 0.0000 | 0.0123 | 0.0062 | 0.0247 | 0.0123 | 0.0000 | 0.0000 |
| HSS17 | 0.0309 | 0.0309 | 0.0062 | 0.0123 | 0.0185 | 0.0123 | 0.0000 | 0.0000 | 0.0494 | 0.0123 | 0.0062 | 0.0123 | 0.0062 | 0.0000 | 0.0062 | 0.0000 | 0.0000 |
| HSS1 | HSS2 | HSS3 | HSS4 | HSS5 | HSS6 | HSS7 | HSS8 | HSS9 | HSS10 | HSS11 | HSS12 | HSS13 | HSS14 | HSS15 | HSS16 | HSS17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HSS1 | 0.0244 | 0.0217 | 0.0940 | 0.0497 | 0.0829 | 0.0740 | 0.0822 | 0.0409 | 0.1373 | 0.0329 | 0.0545 | 0.1073 | 0.0697 | 0.0672 | 0.0804 | 0.0159 | 0.0432 |
| HSS2 | 0.0538 | 0.0048 | 0.0253 | 0.0322 | 0.0322 | 0.0230 | 0.0209 | 0.0136 | 0.0607 | 0.0354 | 0.0313 | 0.0473 | 0.0294 | 0.0430 | 0.0243 | 0.0266 | 0.0108 |
| HSS3 | 0.0240 | 0.0053 | 0.0122 | 0.0192 | 0.0851 | 0.0094 | 0.0337 | 0.0153 | 0.1010 | 0.0109 | 0.0249 | 0.0678 | 0.0245 | 0.0029 | 0.0426 | 0.0021 | 0.0100 |
| HSS4 | 0.0125 | 0.0040 | 0.0299 | 0.0055 | 0.0185 | 0.0041 | 0.0101 | 0.0036 | 0.0804 | 0.0036 | 0.0285 | 0.0216 | 0.0048 | 0.0205 | 0.0050 | 0.0013 | 0.0085 |
| HSS5 | 0.0268 | 0.0059 | 0.0376 | 0.0136 | 0.0165 | 0.0347 | 0.0458 | 0.0402 | 0.1053 | 0.0109 | 0.0192 | 0.0924 | 0.0444 | 0.0029 | 0.0516 | 0.0028 | 0.0155 |
| HSS6 | 0.0144 | 0.0040 | 0.0076 | 0.0049 | 0.0262 | 0.0059 | 0.0048 | 0.0160 | 0.0864 | 0.0030 | 0.0039 | 0.0163 | 0.0122 | 0.0013 | 0.0548 | 0.0017 | 0.0018 |
| HSS7 | 0.0214 | 0.0041 | 0.0084 | 0.0051 | 0.0093 | 0.0129 | 0.0054 | 0.0349 | 0.0825 | 0.0030 | 0.0044 | 0.0353 | 0.0139 | 0.0018 | 0.0503 | 0.0022 | 0.0019 |
| HSS8 | 0.0645 | 0.0122 | 0.0418 | 0.0154 | 0.0568 | 0.0387 | 0.0373 | 0.0119 | 0.0947 | 0.0063 | 0.0270 | 0.0855 | 0.0588 | 0.0063 | 0.0725 | 0.0273 | 0.0113 |
| HSS9 | 0.0534 | 0.0404 | 0.0433 | 0.0496 | 0.0333 | 0.0152 | 0.0216 | 0.0140 | 0.0304 | 0.0296 | 0.0322 | 0.0600 | 0.0243 | 0.0072 | 0.0244 | 0.0147 | 0.0110 |
| HSS10 | 0.0410 | 0.0165 | 0.0540 | 0.0127 | 0.0567 | 0.0086 | 0.0092 | 0.0133 | 0.0622 | 0.0045 | 0.0128 | 0.0367 | 0.0406 | 0.0100 | 0.0357 | 0.0020 | 0.0160 |
| HSS11 | 0.0228 | 0.0178 | 0.0092 | 0.0191 | 0.0095 | 0.0070 | 0.0053 | 0.0287 | 0.0855 | 0.0287 | 0.0056 | 0.0365 | 0.0202 | 0.0337 | 0.0078 | 0.0025 | 0.0333 |
| HSS12 | 0.0256 | 0.0052 | 0.0361 | 0.0071 | 0.0446 | 0.0384 | 0.0268 | 0.0387 | 0.0996 | 0.0046 | 0.0126 | 0.0206 | 0.0707 | 0.0024 | 0.0382 | 0.0026 | 0.0031 |
| HSS13 | 0.0557 | 0.0114 | 0.0453 | 0.0142 | 0.0536 | 0.0179 | 0.0240 | 0.0400 | 0.0927 | 0.0113 | 0.0145 | 0.0882 | 0.0154 | 0.0047 | 0.0458 | 0.0031 | 0.0046 |
| HSS14 | 0.0180 | 0.0098 | 0.0055 | 0.0234 | 0.0055 | 0.0581 | 0.0032 | 0.0026 | 0.0847 | 0.0031 | 0.0040 | 0.0074 | 0.0036 | 0.0021 | 0.0061 | 0.0016 | 0.0017 |
| HSS15 | 0.0477 | 0.0112 | 0.0425 | 0.0079 | 0.0625 | 0.0572 | 0.0221 | 0.0202 | 0.1000 | 0.0051 | 0.0074 | 0.0324 | 0.0343 | 0.0038 | 0.0146 | 0.0026 | 0.0040 |
| HSS16 | 0.0317 | 0.0034 | 0.0329 | 0.0240 | 0.0401 | 0.0316 | 0.0126 | 0.0050 | 0.0633 | 0.0093 | 0.0051 | 0.0247 | 0.0131 | 0.0275 | 0.0211 | 0.0014 | 0.0027 |
| HSS17 | 0.0385 | 0.0344 | 0.0149 | 0.0183 | 0.0271 | 0.0180 | 0.0062 | 0.0046 | 0.0653 | 0.0167 | 0.0118 | 0.0244 | 0.0134 | 0.0045 | 0.0139 | 0.0022 | 0.0032 |
| ri | ci | ri + ci (Prominence Degree) | ri − ci (Cause Degree) | |
|---|---|---|---|---|
| HSS1 | 1.0782 | 0.5760 | 1.6542 | 0.5021 |
| HSS2 | 0.5146 | 0.2121 | 0.7267 | 0.3025 |
| HSS3 | 0.4910 | 0.5407 | 1.0317 | −0.0498 |
| HSS4 | 0.2624 | 0.3219 | 0.5843 | −0.0595 |
| HSS5 | 0.5662 | 0.6606 | 1.2268 | −0.0944 |
| HSS6 | 0.2654 | 0.4546 | 0.7200 | −0.1892 |
| HSS7 | 0.2969 | 0.3712 | 0.6681 | −0.0743 |
| HSS8 | 0.6681 | 0.3435 | 1.0116 | 0.3246 |
| HSS9 | 0.5047 | 1.4320 | 1.9367 | −0.9272 |
| HSS10 | 0.4325 | 0.2189 | 0.6515 | 0.2136 |
| HSS11 | 0.3731 | 0.2998 | 0.6729 | 0.0733 |
| HSS12 | 0.4769 | 0.8044 | 1.2814 | −0.3275 |
| HSS13 | 0.5423 | 0.4935 | 1.0358 | 0.0488 |
| HSS14 | 0.2401 | 0.2418 | 0.4819 | −0.0016 |
| HSS15 | 0.4756 | 0.5891 | 1.0647 | −0.1135 |
| HSS16 | 0.3495 | 0.1126 | 0.4621 | 0.2370 |
| HSS17 | 0.3176 | 0.1825 | 0.5001 | 0.1351 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frichi, Y.; Jawab, F.; Boutahari, S. The Mixed-Method 5W2D Approach for Health System Stakeholders Analysis in Quality of Care: An Application to the Moroccan Context. Int. J. Environ. Res. Public Health 2019, 16, 2899. https://doi.org/10.3390/ijerph16162899
Frichi Y, Jawab F, Boutahari S. The Mixed-Method 5W2D Approach for Health System Stakeholders Analysis in Quality of Care: An Application to the Moroccan Context. International Journal of Environmental Research and Public Health. 2019; 16(16):2899. https://doi.org/10.3390/ijerph16162899
Chicago/Turabian StyleFrichi, Youness, Fouad Jawab, and Said Boutahari. 2019. "The Mixed-Method 5W2D Approach for Health System Stakeholders Analysis in Quality of Care: An Application to the Moroccan Context" International Journal of Environmental Research and Public Health 16, no. 16: 2899. https://doi.org/10.3390/ijerph16162899
APA StyleFrichi, Y., Jawab, F., & Boutahari, S. (2019). The Mixed-Method 5W2D Approach for Health System Stakeholders Analysis in Quality of Care: An Application to the Moroccan Context. International Journal of Environmental Research and Public Health, 16(16), 2899. https://doi.org/10.3390/ijerph16162899







