End-Users and Caregivers’ Involvement in Health Interventional Research Carried Out in Geriatric Facilities: A Systematic Review
Abstract
:1. Introduction
2. Method
2.1. The Systematic Review
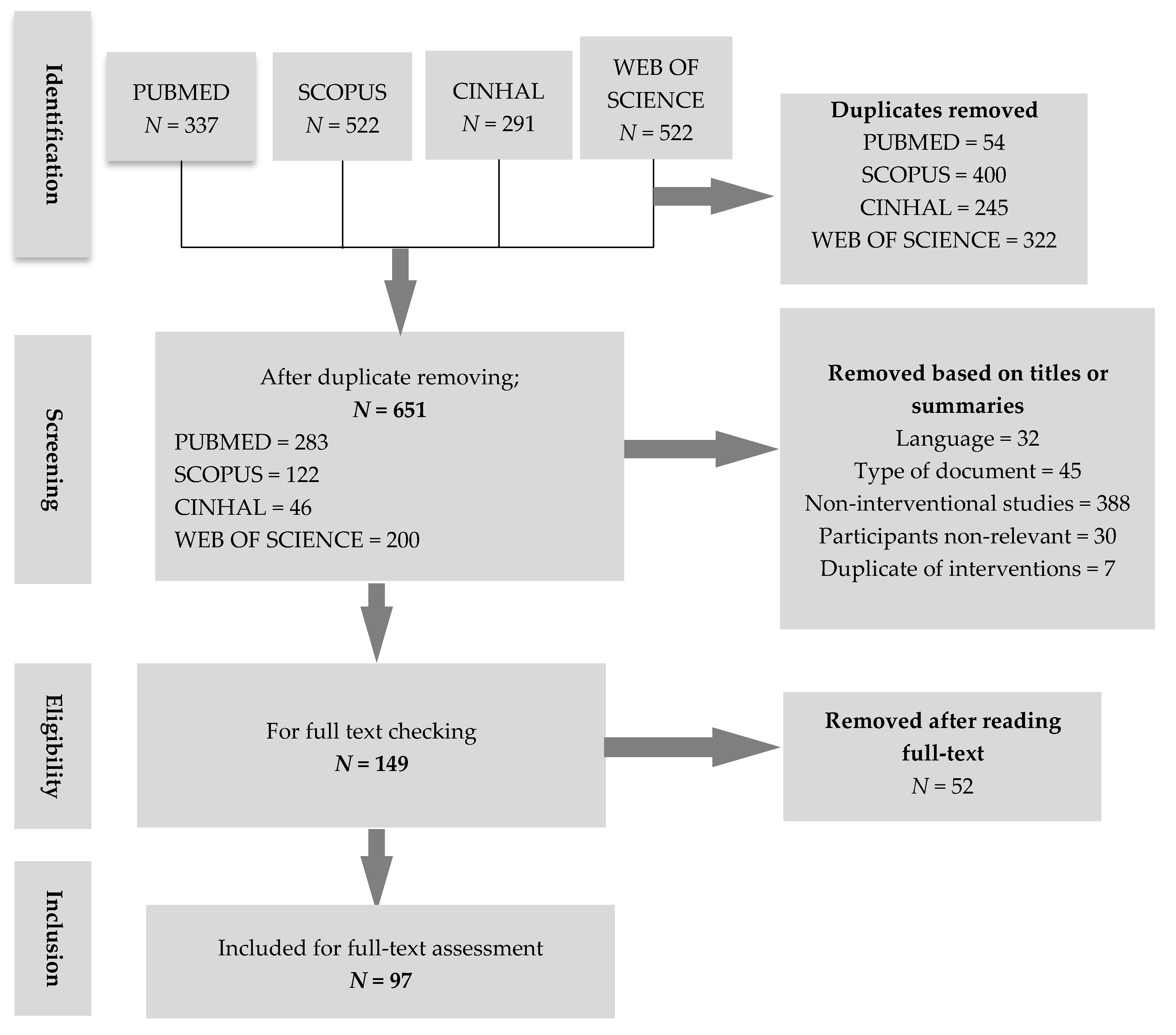
2.1.1. Search Strategy, Criteria, and Approach
2.1.2. Assessment of Involvement in the Full Texts
2.1.3. Quality Assessment of Included Articles
2.2. The Questionnaire
3. Results
3.1. The Systematic Review
3.1.1. Characteristics of Included Articles
3.1.2. Involvement in the Included Articles
3.1.3. Content of the Involvement in the Included Articles
3.2. The Questionnaire
4. Discussion
4.1. Description of the Participants’ Involvement in the Health Interventions Analyzed
4.2. Increase of Participants’ Involvement in Geriatric Institutions Health Interventions
4.3. Limitations of This Review
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dahany, M.M.; Dramé, M.; Mahmoudi, R.; Novella, J.L.; Ciocan, D.; Kanagaratnam, L.; Morrone, I.; Blanchard, F.; Nazeyrollas, P.; Barbe, C.; et al. Factors associated with successful aging in persons aged 65 to 75 years. Eur. Geriatr. Med. 2014, 5, 365–370. [Google Scholar] [CrossRef]
- Bloom, D.E.; Canning, D.; Fink, G. Implications of population ageing for economic growth. Oxf. Rev. Econ. Policy 2010, 26, 583–612. [Google Scholar] [CrossRef] [Green Version]
- Reher, D.S. Baby booms, busts, and population ageing in the developed world. Popul. Stud. 2015, 69, S57–S68. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R. Reducing falls in a care home. BMJ Qual. Improv. Rep. 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Streicher, M.; Themessl-Huber, M.; Schindler, K.; Sieber, C.C.; Hiesmayr, M.; Volkert, D. nutritionDay in Nursing Homes—The Association of Nutritional Intake and Nutritional Interventions With 6-Month Mortality in Malnourished Residents. J. Am. Med Dir. Assoc. 2017, 18, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Yassi, A.; Lockhart, K. Work-relatedness of low back pain in nursing personnel: A systematic review. Int. J. Occup. Environ. Health 2013, 19, 223–244. [Google Scholar] [CrossRef] [PubMed]
- Rifkin, S.B.; Muller, F.; Bichmann, W. Primary health care: On measuring participation. Soc. Sci. Med. 1988, 26, 931–940. [Google Scholar] [CrossRef]
- Van Malderen, L.; De Vriendt, P.; Mets, T.; Verté, D.; Gorus, E. Experiences and Effects of Structurally Involving Residents in the Nursing Home by Means of Participatory Action Research: A Mixed Method Study. J. Am. Med. Dir. Assoc. 2017, 18, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.; Barber, R.; Ward, P.R.; Boote, J.D.; Cooper, C.L.; Armitage, C.J.; Jones, G. Health researchers’ attitudes towards public involvement in health research. Health Expect. 2009, 12, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Bjãrås, G.; Haglund, B.J.A.; Rifkin, S.B. A new approach to community participation assessment. Health Promot. Int. 1991, 6, 199–206. [Google Scholar] [CrossRef]
- Brett, J.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. Mapping the impact of patient and public involvement on health and social care research: A systematic review. Health Expect. 2014, 17, 637–650. [Google Scholar] [CrossRef]
- Draper, A.K.; Hewitt, G.; Rifkin, S. Chasing the dragon: Developing indicators for the assessment of community participation in health programmes. Soc. Sci. Med. 2010, 71, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Nazir, A.; Unroe, K.; Tegeler, M.; Khan, B.; Azar, J.; Boustani, M. Systematic Review of Interdisciplinary Interventions in Nursing Homes. J. Am. Med. Dir. Assoc. 2013, 14, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Schoberer, D.; Leino-Kilpi, H.; EBreimaier, H.; Halfens, R.J.; Lohrmann, C. Educational interventions to empower nursing home residents: A systematic literature review. Clin. Interv. Aging 2016, 11, 1351–1363. [Google Scholar] [CrossRef]
- Mixed Method Appraisal Tool. Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf (accessed on 6 June 2019).
- Sharoni, S.K.A.; Rahman, H.A.; Minhat, H.S.; Ghazali, S.S.; Ong, M.H.A. A self-efficacy education programme on foot self-care behaviour among older patients with diabetes in a public long-term care institution, Malaysia: A Quasi-experimental Pilot Study. BMJ Open 2017, 7, e014393. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, J. Intergenerational Program for Nursing Home Residents and Adolescents in Korea. J. Gerontol. Nurs. 2018, 44, 32–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, J.Y.; Park, S.Y.; Kim, J.K. The effects of a client-centered leisure activity program on satisfaction, self-esteem, and depression in elderly residents of a long-term care facility. J. Phys. Ther. Sci. 2018, 30, 73–76. [Google Scholar] [CrossRef] [Green Version]
- Diegelmann, M.; Jansen, C.P.; Wahl, H.W.; Schilling, O.K.; Schnabel, E.L.; Hauer, K. Does a physical activity program in the nursing home impact on depressive symptoms? A generalized linear mixed-model approach. Aging Ment. Health 2018, 22, 784–793. [Google Scholar] [CrossRef]
- Elpers, K.; Amano, T.; DeCoster, V.; Johnson, M. Effectiveness of a psycho-educational staff training program on attitudes of staff in a long-term care facility: A pilot study and framework. Educ. Gerontol. 2017, 43, 431–439. [Google Scholar] [CrossRef]
- Aasmul, I.; Husebo, B.S.; Flo, E. Description of an advance care planning intervention in nursing homes: Outcomes of the process evaluation. BMC Geriatr. 2018, 18, 26. [Google Scholar] [CrossRef]
- De Souto Barreto, P.; Lapeyre-Mestre, M.; Cestac, P.; Vellas, B.; Rolland, Y. Effects of a geriatric intervention aiming to improve quality care in nursing homes on benzodiazepine use and discontinuation. Br. J. Clin. Pharmacol. 2016, 81, 759–767. [Google Scholar] [CrossRef]
- Gordon, S.E.; Dufour, A.B.; Monti, S.M.; Mattison, M.L.; Catic, A.G.; Thomas, C.P.; Lipsitz, L.A. Impact of a Videoconference Educational Intervention on Physical Restraint and Antipsychotic Use in Nursing Homes: Results From the ECHO-AGE Pilot Study. J. Am. Med Dir. Assoc. 2016, 17, 553–556. [Google Scholar] [CrossRef] [Green Version]
- Connolly, M.J.; Broad, J.B.; Boyd, M.; Zhang, T.X.; Kerse, N.; Foster, S.; Lumley, T.; Whitehead, N. The ‘Big Five’. Hypothesis generation: A multidisciplinary intervention package reduces disease-specific hospitalisations from long-term care: A post hoc analysis of the ARCHUS cluster-randomised controlled trial. Age Ageing 2016, 45, 415–420. [Google Scholar] [CrossRef]
- Kataoka-Yahiro, M.R.; McFarlane, S.; Koijane, J.; Li, D. Culturally Competent Palliative and Hospice Care Training for Ethnically Diverse Staff in Long-Term Care Facilities. Am. J. Hosp. Palliat. Care 2017, 34, 335–346. [Google Scholar] [CrossRef]
- Hartmann, C.W.; Mills, W.L.; Pimentel, C.B.; APalmer, J.; Allen, R.S.; Zhao, S.; Wewiorski, N.J.; Sullivan, J.L.; Dillon, K.; Clark, V.; et al. Impact of Intervention to Improve Nursing Home Resident-Staff Interactions and Engagement. Gerontologist 2018, 58, e291–e301. [Google Scholar] [CrossRef]
- Berendonk, C.; Kaspar, R.; Bär, M.; Hoben, M. Improving quality of work life for care providers by fostering the emotional well-being of persons with dementia: A cluster-randomized trial of a nursing intervention in German long-term care settings. Dementia 2017, 18. [Google Scholar] [CrossRef]
- Franzmann, J.; Haberstroh, J.; Pantel, J. Train the trainer in dementia care. A program to foster communication skills in nursing home staff caring for dementia patients. Z. Gerontol. Geriatr. 2016, 49, 209–215. [Google Scholar] [CrossRef]
- Jackson, K.M. Improving nursing home falls management program by enhancing standard of care with collaborative care multi-interventional protocol focused on fall prevention. J. Nurs. Educ. Pr. 2016, 6, 84–96. [Google Scholar] [CrossRef]
- Staniszewska, S.; Jones, N.; Newburn, M.; Marshall, S. User involvement in the development of a research bid: Barriers, enablers and impacts 1. Health Expect. 2007, 10, 173–183. [Google Scholar] [CrossRef]
- Whitson, H.E.; Hastings, S.N.; Lekan, D.A.; Sloane, R.; White, H.K.; McConnell, E.S. A Quality Improvement Program to Enhance After-Hours Telephone Communication Between Nurses and Physicians in a Long-Term Care Facility. J. Am. Geriatr. Soc. 2008, 56, 1080–1086. [Google Scholar] [CrossRef]
- Brett, J.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. A Systematic Review of the Impact of Patient and Public Involvement on Service Users, Researchers and Communities. Patient Patient Cent. Outcomes Res. 2014, 7, 387–395. [Google Scholar] [CrossRef]
- Lam, H.R.; Chow, S.; Taylor, K.; Chow, R.; Lam, H.; Bonin, K.; Rowbottom, L.; Herrmann, N. Challenges of conducting research in long-term care facilities: A systematic review. BMC Geriatr. 2018, 18, 242. [Google Scholar] [CrossRef]
- Stevens, B. How seniors learn. Issue Brief Cent. Med. Educ. 2003, 4, 1–8. [Google Scholar]
- Schoberer, D.; Breimaier, H.E.; Mandl, M.; Halfens, R.J.; Lohrmann, C. Involving the consumers: An exploration of users’ and caregivers’ needs and expectations on a fall prevention brochure: A qualitative study. Geriatr. Nurs. 2016, 37, 207–214. [Google Scholar] [CrossRef]
- Froggatt, K.; Goodman, C.; Morbey, H.; Davies, S.L.; Masey, H.; Dickinson, A.; Martin, W.; Victor, C. Public involvement in research within care homes: Benefits and challenges in the APPROACH study. Health Expect. 2016, 19, 1336–1345. [Google Scholar] [CrossRef]
- Wight, D.; Wimbush, E.; Jepson, R.; Doi, L. Six steps in quality intervention development (6SQuID). J. Epidemiol. Community Health 2016, 70, 520–525. [Google Scholar] [CrossRef]
- Martinez, C.; Olander, S. Stakeholder Participation for Sustainable Property Development. Procedia Econ. Financ. 2015, 21, 57–63. [Google Scholar] [CrossRef] [Green Version]
- Martin, G.P.; Learmonth, M. A critical account of the rise and spread of ‘leadership’: The case of UK healthcare. Soc. Sci. Med. 2012, 74, 281–288. [Google Scholar] [CrossRef]
- Whelan, J.; Love, P.; Pettman, T.; Doyle, J.; Booth, S.; Smith, E.; Waters, E. Cochrane Update: Predicting sustainability of intervention effects in public health evidence: Identifying key elements to provide guidance. J. Public Health 2014, 36, 347–351. [Google Scholar] [CrossRef]
- Porter-O’Grady, T. A different age for leadership, part 1: New context, new content. JONA J. Nurs. Adm. 2003, 33, 105–110. [Google Scholar] [CrossRef]
- Barnes, M.; Walker, A. Consumerism versus empowerment: A principled approach to the involvement of older service users. Policy Politics 1996, 24, 375–393. [Google Scholar] [CrossRef]
- Westoby, A. Squaring the Circle: User and Carer Participation in Needs Assessment. Disabil. Handicap. Soc. 1993, 8, 439–440. [Google Scholar] [CrossRef]
- Ocloo, J.E.; Fulop, N.J. Developing a ‘critical’ approach to patient and public involvement in patient safety in the NHS: Learning lessons from other parts of the public sector: Critical approach to patient and public involvement in patient safety. Health Expect. 2012, 15, 424–432. [Google Scholar] [CrossRef]
- Morrison, C.; Dearden, A. Beyond tokenistic participation: Using representational artefacts to enable meaningful public participation in health service design. Health Policy 2013, 112, 179–186. [Google Scholar] [CrossRef] [Green Version]
- Supple, D.; Roberts, A.; Hudson, V.; Masefield, S.; Fitch, N.; Rahmen, M.; Flood, B.; de Boer, W.; Powell, P.; Wagers, S. From tokenism to meaningful engagement: Best practices in patient involvement in an EU project. Res. Involv. Engagem. 2015, 1. [Google Scholar] [CrossRef]
- McKeown, J.K.; Fortune, D.; Dupuis, S.L. “It is like stepping into another world”: Exploring the possibilities of using appreciative participatory action research to guide culture change work in community and long-term care. Action Res. 2016, 14, 318–334. [Google Scholar] [CrossRef]
- Kuokkanen, L.; Leino-Kilpi, H.; Leino-Kilpi, H. Power and empowerment in nursing: Three theoretical approaches. J. Adv. Nurs. 2000, 31, 235–241. [Google Scholar] [CrossRef]
- Jenkins, C.; Smythe, A.; Galant-Miecznikowska, M.; Bentham, P.; Oyebode, J. Overcoming challenges of conducting research in nursing homes: Catharine Jenkins, Analisa Smythe and colleagues explore the processes, barriers and make recommendations for research in long-term care settings. Nurs. Older People 2016, 28, 16–23. [Google Scholar] [CrossRef]
- Spector, A.; Orrell, M.; Goyder, J. A systematic review of staff training interventions to reduce the behavioural and psychological symptoms of dementia. Ageing Res. Rev. 2013, 12, 354–364. [Google Scholar] [CrossRef]
- Sheehan, K.B. E-mail Survey Response Rates: A Review. J. Comput. Mediat. Commun. 2001, 6. [Google Scholar] [CrossRef]
- OMS|Déclaration D’Alma-Ata sur les soins de Santé Primaires. WHO n.d. Available online: http://www.who.int/topics/primary_health_care/alma_ata_declaration/fr/ (accessed on 10 May 2018).
- Services WSG on CI in HDCH, Organization WH. Community Involvement in Health Development: Challenging Health Services, Report of a WHO Study Group [Meeting in Geneva from 11 to 18 December 1989]. Available online: https://apps.who.int/iris/bitstream/handle/10665/40624/WHO_TRS_809.pdf?sequence=1&isAllowed=y (accessed on 5 August 2019).



| Points | Items | Needs Assessment | Leadership | Organization | Resources Mobilization | Management |
|---|---|---|---|---|---|
| 1 point | Researchers are the unique decision makers about the interventions | ||||
| 2 points | Both researchers and end-users are involved in the item | ||||
| 3 points | End-users are the main decision makers for all items | ||||
| Total of the five items | XXX | ||||
| Participants | Number of Articles |
|---|---|
| Residents + nurses | 4 articles |
| Residents + relatives | 2 articles |
| Relatives + nurses + physicians | 1 article |
| Residents + nurses+ physicians | 1 article |
| Physicians + nurses | 11 articles |
| TOTAL | 19 articles |
| Respondents | Verbatim |
|---|---|
| Corresponding Author A from Germany | “The study took part between 2004 and 2010. The intervention was developed in 2006 and 2007. At this time, the involvement of end users and participants in developing interventions was not common in Germany. So, we did not involve any residents and nurses in developing the intervention. But some of our team members were nurses (I for example).” |
| Corresponding Author B from Switzerland | “Thanks for your mail and interest. We did not involve older people in the design and management of the intervention.” |
| Corresponding Author C from USA | “To quickly answer your questions, nursing staff were not involved in the design of the intervention—a third party company designed and implemented the program. The third party managed the training and implementation for xx years.” |
| Corresponding Author D from the Netherlands | “Staff of research did the education component of the interventions (teaching, newsletter, etc.)” |
| Corresponding Author E from the Netherlands | “There was a lot of work and consultations that were done in the design and creation of the videos, including long-term care staff, administrators, and people living with HIV. In terms of the brief evaluation to inform the implementation and dissemination of the videos, we had a member of our team (who is an author on the paper) who was a nursing home administrator. He was involved in the design of the evaluation. In terms of implementing the training at the different homes as discussed in the paper we reached out to the individual nursing homes and worked with their staff to help facilitate the education sessions.” |
| Corresponding Author F from the Netherlands | “Yes, dual sensory impaired older adults, nurses, and care professionals (specialized in dual sensory impairment) were involved in the choice of the primary outcome measure and in the development of the intervention. To determine the primary outcome of the intervention, a focus group of dual sensory impaired older adults and their care professionals was asked ‘to identify the key aim of the psychosocial intervention’. Also, the group received and examined a variety of outcome measures. After discussion, they advised that social participation should be assigned as the primary outcome of the intervention. We performed a try-out in two different care facilities, discussed and collected the reactions and advices of the older adults and nurses, and adjusted the intervention.” |
| Corresponding Author G from the Netherlands | “The intervention comprised the … tools (development described by …) and improvement suggestions based on direct family feedback.” |
| Corresponding Author H from South Korea | “The health coaching program is that recipients actively join the intervention and finally set their own goals. Therefore, recipients involved the intervention. Qualified coaches formed rapports with recipients. Coaches gave recipients individual or group education. During the training, the coaches kept encouraging participants to set their own goals. It is an important intervention in the health coaching program to set and practice goals by oneself. Facilities provided a place for group training.” |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahouah, M.; Rothan-Tondeur, M. End-Users and Caregivers’ Involvement in Health Interventional Research Carried Out in Geriatric Facilities: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 2812. https://doi.org/10.3390/ijerph16162812
Ahouah M, Rothan-Tondeur M. End-Users and Caregivers’ Involvement in Health Interventional Research Carried Out in Geriatric Facilities: A Systematic Review. International Journal of Environmental Research and Public Health. 2019; 16(16):2812. https://doi.org/10.3390/ijerph16162812
Chicago/Turabian StyleAhouah, Mathieu, and Monique Rothan-Tondeur. 2019. "End-Users and Caregivers’ Involvement in Health Interventional Research Carried Out in Geriatric Facilities: A Systematic Review" International Journal of Environmental Research and Public Health 16, no. 16: 2812. https://doi.org/10.3390/ijerph16162812





