Abstract
Mortality-to-incidence ratios (MIRs) are alternative parameters used to evaluate the prognosis of a disease. In addition, MIRs are associated with the ranking of health care systems and expenditures for certain types of cancer. However, a lack of association between MIRs and pancreatic cancer has been noted. Given the poor prognosis of brain and nervous system cancers, similar to pancreatic cancer, the relation of MIRs and health care disparities is worth investigating. We used the Spearman’s rank correlation coefficient (CC) to analyze the correlation between the MIRs in brain and nervous system cancers and inter-country disparities, including expenditures on health and human development index. Interestingly, the MIRs in brain and nervous system cancers are associated with the human development index score (N = 157, CC = −0.394, p < 0.001), current health expenditure (CHE) per capita (N = 157, CC = −0.438, p < 0.001), and CHE as percentage of gross domestic product (N = 157, CC = −0.245, p = 0.002). In conclusion, the MIRs in the brain and nervous system cancer are significantly associated with health expenditures and human development index. However, their role as an indicator of health disparity warrants further investigation.
1. Introduction
The incidence of brain and nervous system cancers varies, which is a function of occupation and age distribution; moreover, these cancers have a high mortality rate and are rapidly becoming serious health issues worldwide. A total of 296,851 new cases (age-standardized rate, ASR = 3.9 and 3.1, male and female, respectively) of brain and other nervous system cancers have been diagnosed, and 241,037 cancer deaths (ASR = 3.2 and 2.3, male and female, respectively) worldwide were recorded in 2018 []. In the United States, brain and nervous system cancers are the leading causes of cancer-related death in men under the age of 40 and in women under the age of 20 []. Brain and nervous system cancers can occur at any age, but some studies have shown that they are most common in children (aged 0 to 14 years) and adolescents (aged 15 to 19 years) []. Studies have also shown that brain cancer is associated with patients’ occupation; for instance, steel foundry workers, farmers and pesticide users are at an increased risk of brain cancer [,,]. In addition, evidence supports that brain tumors are associated with ionizing radiation, which is generally emitted from cancer treatments and from nuclear weapons. Exposure to moderate radiation doses (i.e., <1 sievert) is significantly associated with increased incidence of neurological tumors [].
In recent years, many breakthroughs were achieved in brain and nervous system cancer treatment. Surgical resection has proven to be an effective traditional treatment, and chemotherapy or radiation therapy can kill any remaining cancer cells after surgery to reduce the risk of cancer recurrence [,]. Targeted therapy, immunotherapy and nanomedicine therapy are novel, curative treatment methods used to treat brain and nervous system cancers [,,]. Considerable progress has been achieved in these therapies over the last couple of years, and such progress has demonstrated a considerable potential for the development of more effective and less toxic therapeutic interventions. Although the above treatments for brain and nervous system cancers have improved considerably, the number of deaths has remained high, as shown in recent global analyses [,], indicating that precancerous prevention may be an effective method to control the morbidity of brain and nervous system cancers.
An innovative parameter used to assess the prognosis of a specific disease is the mortality-to-incidence ratio (MIR), which has been a prime factor for the long-term success of cancer surveillance and for the efficacy of cancer control programs [,,,]. Because the incidence of brain and nervous system cancers varies as a function of occupation and age distribution, we conjecture that the human development index score and health expenditure affect the incidence, mortality rate or MIRs of these cancers. Because this topic has not yet been investigated, we conducted this study to gain a better understanding of the incidence, mortality and MIR of brain and nervous system cancers.
2. Materials and Methods
Data on cancer incidence and mortality were obtained from the GLOBOCAN 2018 database, which is maintained by the International Agency for Research on Cancer (https://www.iarc.fr/). The International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) of C70–72 (brain, central nervous system) was collected according to the method of GLOBOCAN. A total of 185 countries are included in the database. Human development index was obtained from the Human Development Reports database of the United Nations Development Programme (http://hdr.undp.org/). Parameters including current health expenditure (CHE) per capita, and CHE as percentage of gross domestic product (CHE/GDP) were obtained from the WHO statistics report (https://www.who.int/; World Health Statistics 2018). The data acquisition methods used in this study were described previously [,]. MIR is defined as the ratio of crude mortality rate to incidence [,,,]. The selected countries were further screened based on missing data (N = 12, no data available in World Health Statistics 2018; N = 1, no data on human development index), on having a crude rate of zero for incidence or mortality (N = 8), or on being an outlier according to box-and-whisker diagram of the MIR (N = 7). Ultimately, 157 countries were included in the analyses.
The statistical analysis methods used in this study were described previously [,,,]. We evaluated the association between the MIRs and variables with Spearman’s rank correlation coefficient (CC) by using SPSS statistical software version 15.0 (SPSS, Inc., Chicago, IL, USA). p values of <0.05 indicated statistical significance. Scatter plots were generated using Microsoft Excel 2016.
2.1. Research Involving Human Participants
All data were obtained from the global statistics of GLOBOCAN (https://www.iarc.fr/), United Nations Development Programme, Human Development Reports (http://hdr.undp.org/), and WHO statistics report (https://www.who.int/). This work is an analytic epidemiological study, and we did not perform any intervention on human participants.
2.2. Informed Consent
All data were obtained from the global statistics of GLOBOCAN (https://www.iarc.fr/), United Nations Development Programme, Human Development Reports (http://hdr.undp.org/), and WHO statistics report (https://www.who.int/). This research is an analytic epidemiological study that involved no intervention on human participants, so no informed consent was required.
2.3. Declarations
Ethics committee approval and consent to participate are not applicable. All data were obtained from the global statistics of GLOBOCAN (https://www.iarc.fr/), United Nations Development Programme, Human Development Reports (http://hdr.undp.org/), and WHO statistics report (https://www.who.int/). This work is an analytic epidemiological study, and we did not perform any intervention on human participants. We confirm that this study complies with the national guidelines (http://law.moj.gov.tw/LawClass/LawAll.aspx?PCode=L0020162).
3. Results
3.1. Incidence and Mortality of Brain and Nervous System Cancers According to Region
The incidence and mortality rates, rank, percentage of brain and nervous system cancers in all types of cancer and cumulative risk are summarized in Table 1. The total number of cases and deaths worldwide were 296,851 and 241,037, respectively, during the survey period. Among all types of cancer, brain and nervous system cancers accounted for 1.84% of the total number of cases and 2.73% of the total number of deaths. In terms of regions, Africa had the lowest incidence and mortality cumulative risk (0.18 and 0.17, respectively), whereas the highest values (0.56 and 0.44, respectively) were observed in Europe.

Table 1.
Summary of the number of cases, rank and percentage of brain and nervous system in all cancers in the selected regions.
3.2. Incidence and Mortality of Brain and Nervous System Cancers According to Country
Table 2 summarizes the human development index, CHE and MIR of brain and nervous system cancers in 40 representative countries selected according to their ranking for incidence crude rate. The six countries with an incidence crude rate higher than 10 were Serbia (10.3), Croatia (10.3), Greece (10.4), Bosnia and Herzegovina (10.5), Lithuania (11.0) and North Macedonia (12.0). Three of these countries were also among those with a crude mortality rate higher than 8.0, with Lithuania (7.4), Greece (7.7) and Croatia (7.9) being the three exceptions. The other country with a mortality rate higher than 8.0 was Bulgaria (8.8). The calculated MIRs are also presented in Table 2. The four countries with MIRs higher than or equal to 0.90 were Georgia (0.90), Armenia (0.93), Denmark (0.97) and Bulgaria (1.00). Only Sweden has an MIR that is lower than 0.65 (i.e., 0.53).

Table 2.
Representative data for human development index, current health expenditure, cancer incidence, cancer mortality and mortality-to-incidence ratio in brain and nervous system cancers in selected countries according to ranking of incidence (N = 40).
3.3. Association among Human Development Index, CHE Per Capita, CHE/GDP, and MIR in Different Countries
The linear correlation among human development index, CHE per capita, CHE/GDP, age-standardized incidence, and mortality rates in 157 different countries are shown in Figure 1. Figure 1A and 1B present the human development index, which is significantly associated with the ASR of incidence/mortality (N = 157, CC = 0.722, p < 0.001, Figure 1A; N = 157, CC = 0.640, p < 0.001, Figure 1B, respectively). Figure 1C,D show that CHE per capita is markedly associated with ASR of incidence/mortality (N = 157, CC = 0.644, p < 0.001, Figure 1C; N = 157, CC = 0.549, p < 0.001, Figure 1D, respectively). Moreover, CHE/GDP is significantly associated with ASR of incidence/mortality as shown in Figure 1E,F (N = 157, CC = 0.438, p < 0.001, Figure 1E; N = 157, CC = 0.383, p < 0.001, Figure 1F, respectively).
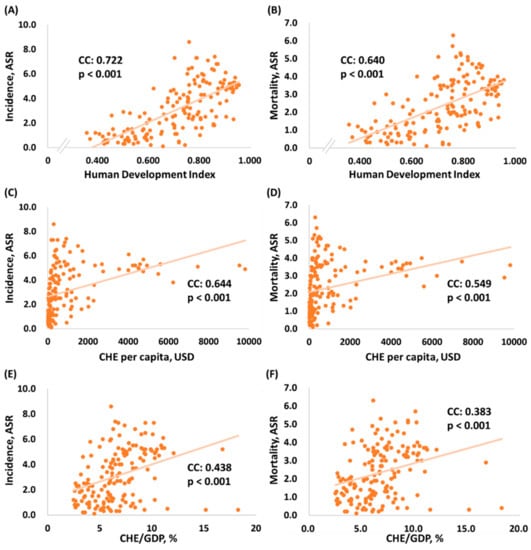
Figure 1.
Association among human development index, current health expenditure and age-standardized rate of (A,C,E) incidence and (B,D,F) mortality in brain and nervous system cancers (N = 157). CHE: current health expenditure; CHE/GDP: current health expenditure as percentage of gross domestic product; ASR: age-standardized rate.
In Figure 2A–C, human development index, CHE per capita and CHE/GDP are all significantly associated with the MIRs of the 157 countries. The negative correlation between human development index and MIRs (N = 157, CC = −0.394, p < 0.001, Figure 2A) indicates that the countries with a higher level of development have a lower MIR. In addition, CHE per capita and CHE/GDP showed a negative correlation (N = 157, CC = −0.438, p < 0.001, Figure 2B; N = 157, CC = −0.245, p < 0.002, Figure 2C, respectively), indicating that the countries with a higher CHE per capita and CHE/GDP have a lower MIRs for brain and nervous system cancers.
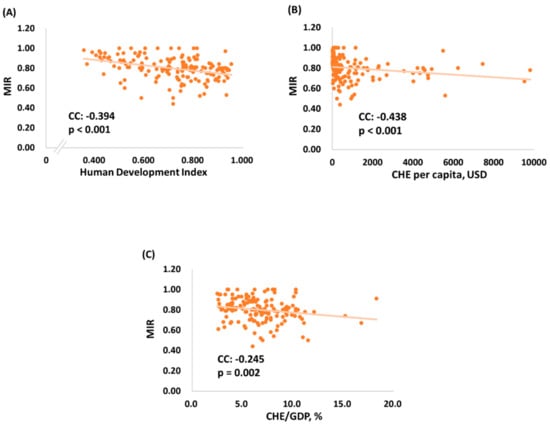
Figure 2.
The association of (A) human development index, (B) current health expenditure per capita (CHE per capita), (C) current health expenditure as percentage of gross domestic product (CHE/GDP) and mortality-to-incidence ratio for brain and nervous system cancers (N = 157).
4. Discussion
The results show that the crude rates and ASRs of incidence and mortality are higher in more developed regions than in less developed regions. We speculate that this trend is attributed to higher exposure of individuals in more developed regions to risk factors (e.g., exposure to more carcinogens) that are associated with brain and nervous system cancers. Ionizing radiation is one such carcinogen, which is used in various applications that are common in more developed countries; these applications include nuclear weapons, nuclear power plants, co-contaminated buildings, and medical examinations and procedures. Exposure to ionizing radiation can increase the risk of brain and nervous system cancers [,,]. In addition, although the association between electromagnetic fields and brain cancer remains uncertain, some studies have indicated that long-term use of mobile phones might increase the risk of intracranial tumors [].
Human development index, CHE per capita and CHE/GDP are all markedly positively associated with the ASR of incidence/mortality. This finding indicates that incidence and mortality rates are higher in countries with a better economy. These associations are expected, and as discussed earlier, the incidence and mortality rates of brain and nervous system cancers are higher in more developed regions, which are usually more willing to invest more in health, leading to a higher human development index ranking, CHE per capita and CHE/GDP [].
A negative correlation was observed between human development index ranking and MIR for brain and nervous system cancers in 157 different countries, that is, the countries with a lower human development index ranking have a higher MIR. This correlation may indicate that countries with higher human development index rankings tend to have better public health policies and tools to screen and treat brain and nervous system cancers. Image testing is one of the critical parameters used to evaluate tumors and to plan treatments. Magnetic resonance imaging is commonly used to diagnose brain tumors; other imaging instruments, such as computed tomography and positron emission tomography, are also used to screen brain and nervous system cancers [,]. These screening instruments are more readily available in countries with higher health care rankings. Overall, early detection combined with effective treatment decreases MIR, which makes sense based on the results.
To our best knowledge, our study is the first to investigate the association among MIR of brain and nervous system cancer, human development index, CHE per capita and CHE/GDP. However, our study has some limitations. First, we did not include the countries with poor data quality or those without available data quality assessments, which might cause misleading findings on MIR. Second, because we collected cross-sectional data for one year only, these data may not accurately describe the actual trend of the disease or they may not allow us to infer causality. Third, no detailed categories of cancer types were analyzed in this study. Despite these limitations, our research shows that in more developed regions and countries with higher CHE/GDP, the incidence and mortality rates for brain and nervous system cancers are higher.
5. Conclusions
MIRs for brain and nervous system cancers are significantly associated with health expenditures and human development index. Considering the limitation of using MIR to predict cancer prognosis, their role and causal relationship are still debatable.
Author Contributions
Conceptualization, T.-H.L., and W.-W.S.; Data curation, H.-L.L.; Formal analysis, W.-W.S.; Investigation, T.-H.L., and L.C.; Resources, H.-L.L.; Supervision, W.-W.S., S.-L.C., Y.-H.H. and A.-L.K.; Writing—original draft, T.-H.L. and L.C.; Writing—review & editing, W.-W.S., S.-L.C. and Y.-H.H.
Funding
There was no funding or grant supports this study.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
| ASR: | age-standardized rate |
| CC: | correlation coefficient |
| CHE: | current health expenditure |
| CHE/GDP: | current health expenditure as percentage of gross domestic product |
| CR: | crude rate |
| cum. risk: | cumulative risk |
| MIR: | mortality-to-incidence ratio |
| WHO: | World Health Organization |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Fallahi, P.; Foddis, R.; Cristaudo, A.; Antonelli, A. High risk of brain tumors in farmers: A mini-review of the literature, and report of the results of a case control study. Clin. Ter. 2017, 168, e290–e292. [Google Scholar] [PubMed]
- Piel, C.; Pouchieu, C.; Tual, S.; Migault, L.; Lemarchand, C.; Carles, C.; Boulanger, M.; Gruber, A.; Rondeau, V.; Marcotullio, E.; et al. Central nervous system tumors and agricultural exposures in the prospective cohort AGRICAN. Int. J. Cancer 2017, 141, 1771–1782. [Google Scholar] [CrossRef] [PubMed]
- Oddone, E.; Scaburri, A.; Bai, E.; Modonesi, C.; Stracci, F.; Marchionna, G.; Crosignani, P.; Imbriani, M. Occupational brain cancer risks in Umbria (Italy), with a particular focus on steel foundry workers. G. Ital. Med. Lav. Ergon. 2014, 36, 111–117. [Google Scholar] [PubMed]
- Preston, D.L.; Ron, E.; Yonehara, S.; Kobuke, T.; Fujii, H.; Kishikawa, M.; Tokunaga, M.; Tokuoka, S.; Mabuchi, K. Tumors of the nervous system and pituitary gland associated with atomic bomb radiation exposure. J. Natl. Cancer Inst. 2002, 94, 1555–1563. [Google Scholar] [CrossRef] [PubMed]
- Galmarini, D.; Galmarini, C.M.; Galmarini, F.C. Cancer chemotherapy: A critical analysis of its 60 years of history. Crit. Rev. Oncol. Hematol. 2012, 84, 181–199. [Google Scholar] [CrossRef]
- Lam, T.C.; Sahgal, A.; Lo, S.S.; Chang, E.L. An update on radiation therapy for brain metastases. Chin. Clin. Oncol. 2017, 6, 35. [Google Scholar] [CrossRef]
- Shah, V.; Kochar, P. Brain Cancer: Implication to Disease, Therapeutic Strategies and Tumor Targeted Drug Delivery Approaches. Recent Pat. Anticancer Drug Discov. 2018, 13, 70–85. [Google Scholar] [CrossRef]
- Dunn-Pirio, A.M.; Vlahovic, G. Immunotherapy approaches in the treatment of malignant brain tumors. Cancer 2017, 123, 734–750. [Google Scholar] [CrossRef]
- Kang, C.; Sun, Y.; Zhu, J.; Li, W.; Zhang, A.; Kuang, T.; Xie, J.; Yang, Z. Delivery of Nanoparticles for Treatment of Brain Tumor. Curr. Drug Metab. 2016, 17, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Lee, S.; Nhung, B.C.; Suh, M.; Park, B.; Jun, J.K.; Choi, K.S. Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol. Health 2017, 39, e2017006. [Google Scholar] [CrossRef] [PubMed]
- Sunkara, V.; Hebert, J.R. The application of the mortality-to-incidence ratio for the evaluation of cancer care disparities globally. Cancer 2016, 122, 487–488. [Google Scholar] [CrossRef]
- Cordero-Morales, A.; Savitzky, M.J.; Stenning-Persivale, K.; Segura, E.R. Conceptual considerations and methodological recommendations for the use of the mortality-to-incidence ratio in time-lagged, ecological-level analysis for public health systems-oriented cancer research. Cancer 2016, 122, 486–487. [Google Scholar] [CrossRef] [PubMed]
- Asadzadeh Vostakolaei, F.; Karim-Kos, H.E.; Janssen-Heijnen, M.L.; Visser, O.; Verbeek, A.L.; Kiemeney, L.A. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur. J. Public Health 2011, 21, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, T.M.; Drain, C.M.; Grimm, J. Optical Imaging of Ionizing Radiation from Clinical Sources. J. Nucl. Med. 2016, 57, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Tang, F.R.; Loganovsky, K. Low dose or low dose rate ionizing radiation-induced health effect in the human. J. Environ. Radioact. 2018, 192, 32–47. [Google Scholar] [CrossRef]
- Bortkiewicz, A.; Gadzicka, E.; Szymczak, W. Mobile phone use and risk for intracranial tumors and salivary gland tumors—A meta-analysis. Int. J. Occup. Med. Environ. Health 2017, 30, 27–43. [Google Scholar] [CrossRef]
- Jakovljevic, M.M. Comparison of historical medical spending patterns among the BRICS and G7. J. Med. Econ. 2016, 19, 70–76. [Google Scholar] [CrossRef]
- Kar, S.; Majumder, D.D. A mathematical theory of shape and neuro-fuzzy methodology-based diagnostic analysis: A comparative study on early detection and treatment planning of brain cancer. Int. J. Clin. Oncol. 2017, 22, 667–681. [Google Scholar] [CrossRef]
- Abrol, S.; Kotrotsou, A.; Salem, A.; Zinn, P.O.; Colen, R.R. Radiomic Phenotyping in Brain Cancer to Unravel Hidden Information in Medical Images. Top. Magn. Reson. Imaging 2017, 26, 43–53. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).