WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measurement
2.3. Analytical Approach
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- National Academies of Sciences, Engineering, and Medicine (NASEM). Review of Wic Food Packages: Proposed Framework for Revisions: Final Report; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- USA Department of Agriculture (USDA). Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Breastfeeding Policy and Guidance. 2016. Available online: https://www.fns.usda.gov/sites/default/files/wic/WIC-Breastfeeding-Policy-and-Guidance.pdf (accessed on 1 March 2019).
- Ahluwalia, I.B.; Tessaro, I.; Grummer-Strawn, L.M.; MacGowan, C.; Benton-Davis, S. Georgia’s breastfeeding promotion program for low-income women. Pediatrics 2000, 105, 85. [Google Scholar] [CrossRef] [PubMed]
- Forste, R.; Hoffmann, J.P. Are US mothers meeting the Healthy People 2010 breastfeeding targets for initiation, duration, and exclusivity? The 2003 and 2004 National Immunization Surveys. J. Hum. Lact. 2008, 24, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Jensen, E. Participation in the Supplemental Nutrition Program for Women, Infants and Children (WIC) and breastfeeding: National, regional, and state level analyses. Matern. Child Health J. 2012, 16, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Darling, N.; Maurice, E.; Barker, L.; Grummer-Strawn, L.M. Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 National Immunization Survey. Pediatrics 2005, 115, E31–E37. [Google Scholar] [CrossRef] [PubMed]
- Francescon, J.; Haile, Z.T.; Kling, D.; Chertok, I. Association between WIC enrollment and exclusive breastfeeding at 3 months postpartum among low-income mothers. J. Am. Osteopath. Assoc. 2016, 116, 770–779. [Google Scholar] [CrossRef] [PubMed]
- Topolyan, I.; Xu, X. Differential effects of mother’s and child’s postnatal WIC participation on breastfeeding. Appl. Econ. 2017, 49, 2216–2225. [Google Scholar] [CrossRef]
- Jacknowitz, A.; Novillo, D.; Tiehen, L. Special Supplemental Nutrition Program for Women, Infants, and Children and infant feeding practices. Pediatrics 2007, 119, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Ziol-Guest, K.M.; Hernandez, D.C. First- and second-trimester WIC participation is associated with lower rates of breastfeeding and early introduction of cow’s milk during infancy. J. Am. Diet Assoc. 2010, 110, 702–709. [Google Scholar] [CrossRef]
- Ryan, A.S.; Zhou, W.; Krieger, F.W.; Lewandowski, G.E. Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978–2003. Pediatrics 2006, 117, 1136–1146. [Google Scholar] [CrossRef]
- Deming, D.M.; Briefel, R.R.; Reidy, K.C. Infant feeding practices and food consumption patterns of children participating in WIC. J. Nutr. Educ. Behav. 2014, 46, S29–S37. [Google Scholar] [CrossRef]
- Mao, C.Y.; Narang, S.; Lopreiato, J. Breastfeeding practices in military families: A 12-month prospective population-based study in the national capital region. Mil. Med. 2012, 177, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Ponza, M.; Devaney, B.; Ziegler, P.; Reidy, K.; Squatrito, C. Nutrient intakes and food choices of infants and toddlers participating in WIC. J. Acad. Nutr. Diet. 2004, 104, S71–S79. [Google Scholar] [CrossRef]
- Campbell, L.A.; Wan, J.; Speck, P.M.; Hartig, M.T. Women, Infant and Children (WIC) peer counselor contact with first time breastfeeding mothers. Public Health Nurs. 2014, 31, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Sonchak, L. The impact of WIC on breastfeeding initiation and gestational weight gain: Case study of South Carolina Medicaid mothers. Child Youth Serv. Rev. 2017, 79, 115–125. [Google Scholar] [CrossRef]
- Wojcicki, J.M.; Gugig, R.; Tran, C.; Kathiravan, S.; Holbrook, K.; Heyman, M.B. Early exclusive breastfeeding and maternal attitudes towards infant feeding in a population of new mothers in San Francisco, California. Breastfeed Med. 2010, 5, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Chatterji, P.; Brooks-Gunn, J. 2004, 94, 1324–1327. [CrossRef]
- U.S. Department of Agriculture (USDA). Effects of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): A Review of Recent Research. The U.S. Department of Agriculture: Washington, DC, USA, 2012. [Google Scholar]
- Rasmussen, K.M.; Whaley, S.E.; Perez-Escamilla, R.; Ross, A.C.; Baker, S.S.; Hatfield, T.; Latulippe, M.E. New opportunities for breastfeeding promotion and support in WIC: Review of WIC food packages, improving balance and choice. J. Nutr. Educ. Behav. 2017, 49, S197–S201. [Google Scholar] [CrossRef]
- Shinn, L.M.; Tangney, C.C.; Busche, C.; Sharp, C.M.; Mullen, M.C. Demographic correlates of infant feeding practices and growth performance in the first year of life. Int. J. Pediatr 2018, 6569204. [Google Scholar] [CrossRef]
- Darfour-Oduro, S.A.; Kim, J. WIC mothers’ social environment and postpartum health on breastfeeding initiation and duration. Breastfeed Med. 2014, 9, 524–529. [Google Scholar] [CrossRef]
- Tenfelde, S.M.; Finnegan, L.; Miller, A.M.; Hill, P.D. Risk of breastfeeding cessation among low-income women, infants, and children: A discrete time survival analysis. Nurs. Res. 2012, 61, 86–95. [Google Scholar] [CrossRef]
- Kim, J.H.; Fiese, B.H.; Donovan, S.M. Breastfeeding is natural but not the cultural norm: A mixed-methods study of first-time breastfeeding, African American mothers participating in WIC. J. Nutr. Educ. Behav. 2017, 49, S151.e1–S161.e1. [Google Scholar] [CrossRef] [PubMed]
- Perez-Escamilla, R.; Sellen, D. Equity in breastfeeding: Where do we go from here? J. Hum. Lact. 2015, 31, 12–14. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Foster, E.M.; Gibson-Davis, C.M. The effect of WIC on breastfeeding: A new look at an established relationship. Child Youth Serv. Rev. 2010, 32, 264–273. [Google Scholar] [CrossRef]
- Gregory, E.F.; Gross, S.M.; Nguyen, T.Q.; Butz, A.M.; Johnson, S.B. WIC participation and breastfeeding at 3 months postpartum. Matern. Child Health J. 2016, 20, 1735–1744. [Google Scholar] [CrossRef] [PubMed]
- National WIC Association. WIC Program Overview and History. Available online: https://www.nwica.org/overview-and-history (accessed on 8 February 2019).
- California WIC Association. WIC WORKS: A Series of Policy Briefs Produced by the California WIC Association and the PHFE WIC Program. Available online: http://www.calwic.org/storage/WIC_WORKS_Policy_Changes_Raise_Breastfeeding_Rates.pdf (accessed on 18 July 2019).
- Schultz, D.J.; Byker, S.C.; Houghtaling, B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. J. Acad. Nutr. Diet. 2015, 115, 1832–1846. [Google Scholar] [CrossRef] [PubMed]
- Langellier, B.A.; Chaparro, M.P.; Wang, M.C.; Koleilat, M.; Whaley, S.E. The new food package and breastfeeding outcomes among women, infants, and children participants in Los Angeles County. Am. J. Public Health 2014, 104, S112–S118. [Google Scholar] [CrossRef] [PubMed]
- Panzera, A.D.; Castellanos-Brown, K.; Paolicelli, C.; Morgan, R.; Potter, A.; Berman, D. The impact of federal policy changes and initiatives on breastfeeding initiation rates and attitudes toward breastfeeding among WIC participants. J. Nutr. Educ. Behav. 2017, 49, S207. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Whaley, S.E.; Koleilat, M.; Whaley, M.; Gomez, J.; Meehan, K.; Saluja, K. Impact of policy changes on infant feeding decisions among low-income women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am. J. Public Health 2012, 102, 2269–2273. [Google Scholar] [CrossRef]
- Joyce, T.; Reeder, J. Changes in breastfeeding among WIC participants following implementation of the new food package. Matern. Child Health J. 2015, 19, 868–876. [Google Scholar] [CrossRef]
- Wilde, P.; Wolf, A.; Fernandez, M.; Collins, A.; Robare, J.F. Evaluation of the Birth Month Breastfeeding Changes to the WIC Food Packages. In Alexandria, VA: US Department of Agriculture, Food and Nutrition Service, Office of Research and Analysis; 2011. Available online: https://www.fns.usda.gov/wic/evaluation-birth-month-breastfeeding-changes-wic-food-packages (accessed on 1 March 2019).
- Wilde, P.; Wolf, A.; Fernandes, M.; Collins, A. Food-package assignments and breastfeeding initiation before and after a change in the Special Supplemental Nutrition Program for Women, Infants, and Children. Am. J. Clin. Nutr. 2012, 96, 560–566. [Google Scholar] [CrossRef]
- Zhang, Q.; Lamichhane, R.; Wright, M.; McLaughlin, P.W.; Stacy, B. Trends in breastfeeding disparities in USA infants by WIC eligibility and participation: Evidence from NHANES 1999–2014. J. Nutr. Edu. Behav. 2019, 51, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Ploeg, M.V.; Betson, D.M. (Eds.) Estimating Eligibility and Participation for the WIC Program; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Rosenbaum, P.R.; Rubin, D.B. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41. [Google Scholar] [CrossRef]
- Oakes, J.M.; Johnson, P.J. Propensity Score Matching for Social Epidemiology. In Methods in Social Epidemiology; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Guo, S.; Fraser, M.W. Propensity Score Analysis: Statistical Methods and Applications, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Heckman, J.J. The scientific model of causality. Sociol. Methodol. 2005, 35, 1–97. [Google Scholar] [CrossRef]
- Bullinger, L.R.; Gurley-Calvez, T. WIC participation and maternal behavior: Breastfeeding and work leave. Contemp. Econ. Policy 2016, 34, 158–172. [Google Scholar] [CrossRef]
- Rossin-Slater, M. WIC in your neighborhood: New evidence on the impacts of geographic access to- clinics. J. Pub. Econ. 2013, 102, 51–69. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.I. Early childhood WIC participation, cognitive development and academic achievement. Soc. Sci. Med. 2015, 126, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Hoynes, H.; Schanzenbach, D.W.; Almond, D. Long-run impacts of childhood access to the safety net. Am. Econ. Rev. 2016, 106, 903–934. [Google Scholar] [CrossRef]
| Variables | Birth Year 2000–2008 | Birth Year 2009–2014 | p-Value |
|---|---|---|---|
| Breastfeeding | |||
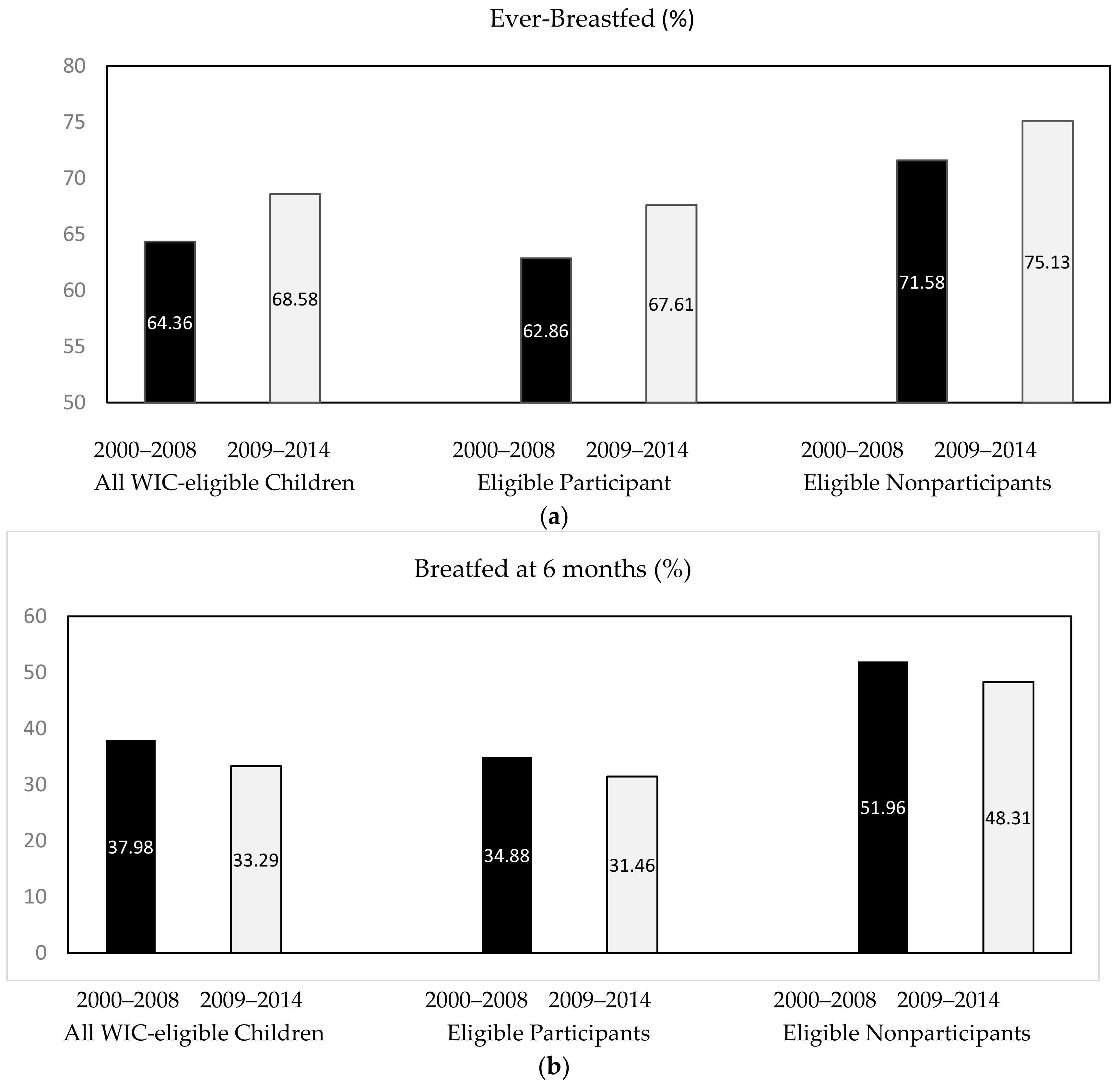
| Ever-breastfed | 64.36% | 68.58% | 0.005 |
| Breastfed at 6 months | 37.98% | 33.29% | 0.024 |
| WIC Participation | 0.000 | ||
| Eligible participants | 82.64% | 87.13% | |
| Eligible nonparticipants | 17.36% | 12.87% | |
| Child Characteristics | |||
| Age (months) | 28.54 (17.44) | 19.74 (15.97) | 0.000 |
| Male | 52.45% | 49.54% | 0.067 |
| Race | 0.000 | ||
| White | 25.31% | 22.63% | |
| Black | 22.20% | 27.63% | |
| Mexican | 36.43% | 26.92% | |
| Other Hispanic | 9.49% | 13.00% | |
| Other races | 6.57% | 9.82% | |
| Family Characteristics | |||
| Marital status | 0.616 | ||
| Married/living with partner | 66.36% | 65.19% | |
| Widowed/divorced/separated | 15.25% | 15.16% | |
| Never married | 18.40% | 19.65% | |
| Educational attainment | <0.001 | ||
| Less than high school | 43.74% | 34.31% | |
| High school graduate/GED | 28.30% | 29.00% | |
| Some college/AA degree | 21.98% | 29.26% | |
| College graduate or higher Income–poverty ratio | 5.98% 0.87 (0.45) | 7.43% 0.85 (0.47) | 0.084 |
| Ever received food stamp (Yes) | 53.61% | 63.20% | <0.001 |
| Sample Size (N) | 2770 | 1538 |
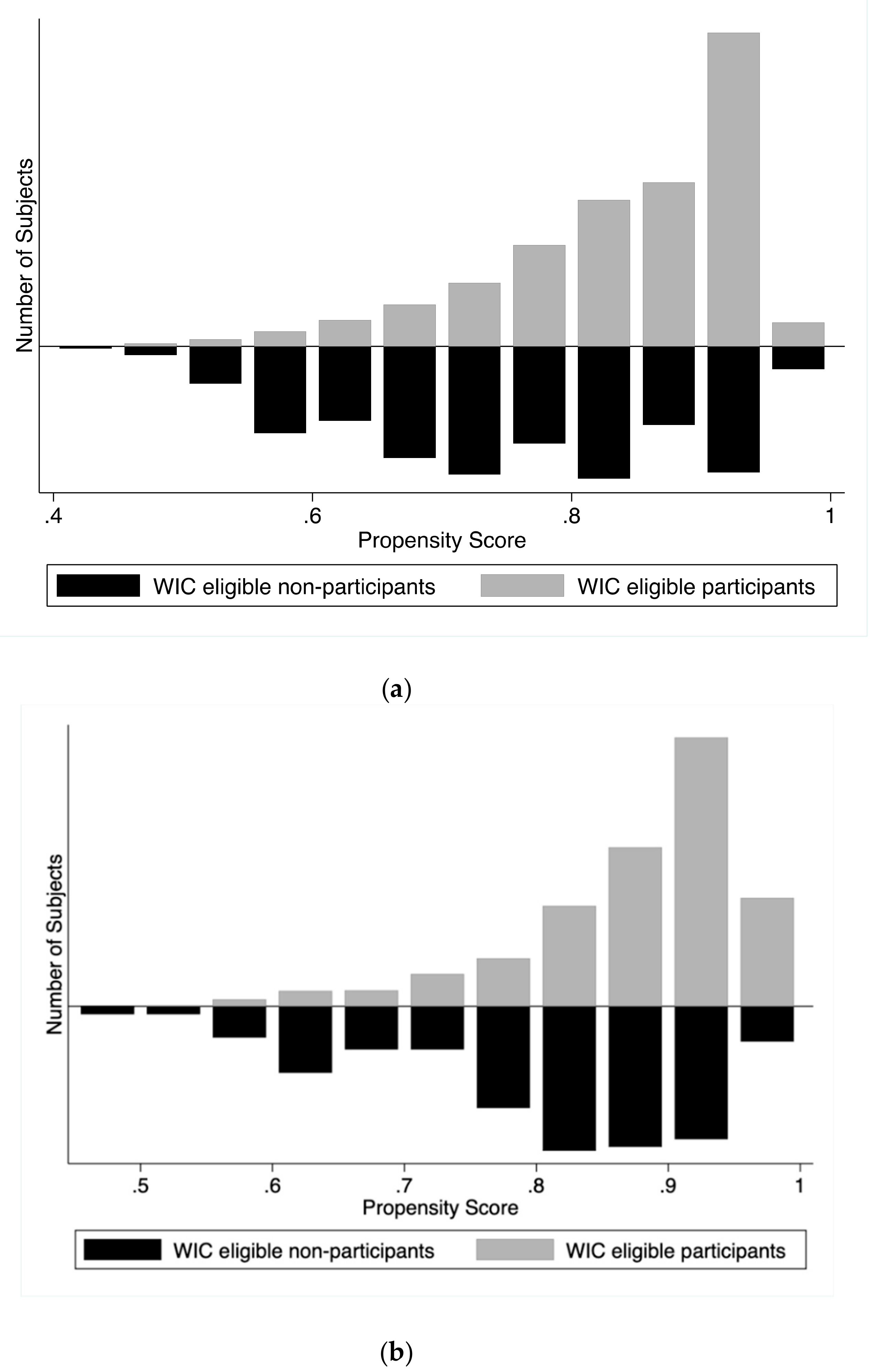
| Birth Year 2000–2008 | Birth Year 2009–2014 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcomes | WIC | Non-WIC | Diff | SE | t-statistic | WIC | Non-WIC | Diff | SE | t-Statistic |
| Ever-Breastfed | ||||||||||
| Unmatched | 0.63 | 0.74 | −0.11 | 0.03 | −4.32 * | 0.69 | 0.76 | −0.07 | 0.04 | −1.94 * |
| Matched | 0.66 | 0.74 | −0.08 | 0.03 | −2.51 * | 0.69 | 0.73 | −0.04 | 0.05 | −0.83 |
| Breastfed at 6 months | ||||||||||
| Unmatched | 0.36 | 0.52 | −0.16 | 0.03 | −4.97 * | 0.32 | 0.48 | −0.17 | 0.05 | -3.13 * |
| Matched | 0.40 | 0.51 | −0.11 | 0.04 | −2.52 * | 0.32 | 0.45 | −0.13 | 0.08 | −1.67 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, K.; Wen, M.; Reynolds, M.; Zhang, Q. WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach. Int. J. Environ. Res. Public Health 2019, 16, 2645. https://doi.org/10.3390/ijerph16152645
Li K, Wen M, Reynolds M, Zhang Q. WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach. International Journal of Environmental Research and Public Health. 2019; 16(15):2645. https://doi.org/10.3390/ijerph16152645
Chicago/Turabian StyleLi, Kelin, Ming Wen, Megan Reynolds, and Qi Zhang. 2019. "WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach" International Journal of Environmental Research and Public Health 16, no. 15: 2645. https://doi.org/10.3390/ijerph16152645
APA StyleLi, K., Wen, M., Reynolds, M., & Zhang, Q. (2019). WIC Participation and Breastfeeding after the 2009 WIC Revision: A Propensity Score Approach. International Journal of Environmental Research and Public Health, 16(15), 2645. https://doi.org/10.3390/ijerph16152645





