Abstract
Neck pain is a burden to employers and employees amenable to improvement with neck/shoulder strengthening exercises. However, the benefits of such interventions on office workers’ work ability remains unknown. This study evaluated the effects of a 12-week combined ergonomics and neck/shoulder strengthening exercise intervention (EET, n = 177, mean age 41.7 years, 26% female), versus a 12-week combined ergonomics and health promotion intervention (EHP, n = 173, mean age 43 years, 29% female) on work ability among office workers. Work ability was measured by a single question. Differences in the work ability score were analyzed using the intention-to-treat (ITT) and per-protocol (i.e., adherence ≥70%) analyses for between- and within-group differences at baseline, 12 weeks, and 12 months. A sub-group analysis was performed for neck cases, defined as reporting neck pain as ≥3 (out of 10). No significant between-group differences for work ability were observed in the general population, and subgroup of neck cases. A significant group-by-time interaction effect at 12 weeks and the trend for significance at 12 months favored the EET group in the per-protocol analysis of the neck cases. EET was effective in increasing work ability post-intervention and potentially, in the long-term, in symptomatic participants with ≥70% adherence to the intervention. However, EET was not superior to EHP.
1. Introduction
Musculoskeletal pain is a threat to productivity. In particular, neck pain places a significant burden on both the individual and employer due to the costs associated with treatment, reduced productivity, and work absenteeism [1,2,3,4]. As non-specific neck pain is a common and episodic musculoskeletal disorder in office workers [2], it is not surprising that many interventions to address this problem have been developed and tested.
Interventions tested with office workers tend to focus on the reduction of neck symptoms through exercise or changes to the ergonomic work environment [5,6,7]. The evidence from several systematic reviews, however, consistently demonstrates neck/shoulder strengthening exercises to be of greater benefit in reducing musculoskeletal pain in office workers than ergonomic interventions [7,8,9]. Despite this evidence, the impact of neck and shoulder exercise interventions on work ability is limited.
Our research group recently demonstrated that health-related productivity loss can be positively impacted with a workplace-based combined intervention of ergonomics and neck/shoulder exercises in office workers [10]. Thus, it is possible that such a workplace-based intervention will also result in improvements in work ability. The concept of work ability was introduced to define a person’s capacity to meet the demands of their work considering their health, personal resources, and work environment [11]. Poor work ability is associated with early retirement, work disability, and productivity loss due to absenteeism [12,13] and long term sickness absence [14]. A limited number of studies have investigated methods to improve work ability, mostly in occupational groups performing physically demanding roles (e.g., cleaners and laundry workers [15,16,17,18]) due to the perception that their work ability is impaired to a greater degree compared to those performing mostly mentally demanding work (e.g., office workers). Some interventions tested included cognitive behavioral therapy [18], generic aerobic exercise (such as dancing, walking or cycling [16,18,19]), region specific exercise interventions delivered only to those with pain [17], or a combination of muscle strengthening, stretching, and cardiovascular exercise [15]. For office workers, interventions tested to impact work ability have been ergonomic [20] or exercise [21]. Based on the evidence to date, it appears that interventions that are multimodal (i.e., contain more than one type of intervention), including strengthening exercises targeting a specific painful region, are more likely to be more efficacious in improving work ability in office workers.
This study is nested within a recently completed 12-week cluster randomized trial that investigated the impact of a combined ergonomics and neck/shoulder strengthening exercise (EET) intervention compared to a combined ergonomics and health promotion (EHP) intervention in a sample of Australian office workers. This is a secondary analysis of a subsample of office workers who provided data on work ability at baseline, immediately after the intervention, and 12 months after commencement. It was hypothesized that the EET intervention would be more efficacious for improving work ability in office workers compared to EHP, and that this effect would be stronger for those with neck pain at baseline.
2. Materials and Methods
A prospective parallel two-arm cluster-randomized trial (ACTRN12612001154897) was undertaken from May 2013 to July 2016. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Medical Research Ethics Committee of The University of Queensland (#2012001318). The protocol has been published [22] and the CONSORT extension for cluster trials adopted for reporting [23] (Supplementary material Table S1).
2.1. Participants
The participants of this study were recruited from 14 private and government organizations in Brisbane, Queensland. The inclusion criteria were any office worker over 18 years working more than 30 hours per week. Participants were ineligible if they were pregnant, had a previous neck injury or trauma or inflammatory condition, a history of neck surgery, or were unable to exercise due to any medical conditions. Only 366 of the 763 participants recruited into the study received the question related to work ability and constitute the sample for this study (Table 1).

Table 1.
Baseline characteristics.
2.2. Procedure
All participants were allocated to clusters of five to eight individuals according to their office building, floor, or department. This approach was undertaken to minimize contamination of interventions and enhance compliance with the intervention. The clusters were then randomly allocated to either EET or EHP by a blinded statistician using computer-generated block randomization (in blocks of four). Participants were encouraged to continue with their usual physical activity while participating in the research. The ergonomic, exercise, and health education interventions were conducted during work time onsite. This was to minimize business disruption and enhance participation and adherence.
Prior to the commencement of their respective interventions, both groups were provided with one-on-one, best practice ergonomic assessment using a 37 item checklist across seven sub-categories (chair, desk, monitor, keyboard, mouse, telephone, and the physical environment (e.g., lighting, temperature, and noise) based on the local government guidelines [24]. The assessment and intervention were prescribed by a qualified health professional, consisting of a one-hour initial assessment with up to one follow-up session. Adjustments may have been minor, such as advice or education (e.g., take frequent breaks), physical changes to their workstation (e.g., raising the height of their chair), or new equipment (e.g., a headset).
Participants were allocated to clusters of 5–8 participants in the EET group and received progressive exercises three times per week for 12 weeks, with each session lasting no more than 20 minutes conducted in one of the rooms at the workplace. The exercises consisted of postural facilitation, shoulder, and neck exercises (seven exercises in total). The postural facilitation exercise was emphasized in the first 2 weeks. The upper neck flexion exercise were included as a warm up for each session, and the five main exercises were performed in cycles of three exercises/session (i.e., neck flexion, neck extension, front and side arm raise to 90°, and reverse flies) (further details are available in [22]). The five exercises were performed with weights or resistance bands and progressed throughout the intervention period using the principles of periodization and progressive overload. One of the three sessions was supervised by a physiotherapist who progressed the exercises as required. To ensure the correct completion of the exercises, participants were provided with a hard copy diary, which included an explanation of each exercise with accompanying photos. The diary also specified the exercise parameters (sets and repetitions) and which exercise was to be performed at each session for each week. Participants recorded exercises completed at each session in their diary. The EHP group was provided with a one hour health promotion session weekly for 12 weeks, which was facilitated by a different health professional. The weekly health promotion topics included healthy dieting, losing weight, discontinuance of smoking, relaxation, and managing stress. Further details regarding the interventions are published elsewhere [22]. Figure 1 displays the flow of participants through the study.
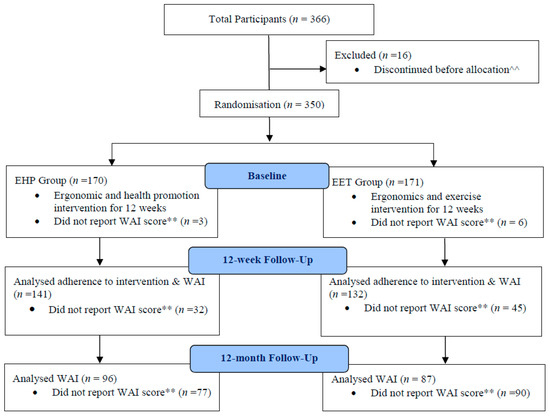
Figure 1.
Flow of participants through the study. WA = Work Ability; ^^ 16 Participants discontinued before allocation: 13 excluded during assessment, 2 due to excessive work demands, 1 due to other reasons; ** Reasons for failure to report work ability scores (1) Participant discontinued due to pregnancy, unrelated illness or injury, change of employer, excessive work demands, or other unstated reasons (2) Participant did not complete response due to: absence for data collection, incomplete response if participants cease surveys part way through or if the online survey portal failed to force the response. EHP = ergonomics and health promotion intervention; EET = ergonomics and neck/shoulder strengthening exercise intervention.
2.3. Primary Outcome
Work ability was measured by a single question, which has been validated to be accurate in predicting work ability compared with the original 7 item Work Ability Index [25]. This question required participants to rate their current work ability, compared to their work ability at its best, on an 11 point scale (from 0 to 10). Participants reported their work ability at three time points (baseline, post-intervention at 12 weeks and follow-up at 12 months). This data and all independent variables were collected via an online survey with the baseline data collected prior to randomization.
2.4. Independent Variables
Several individual and work-related factors potentially impacting work ability were assessed. Individual variables evaluated included the severity of neck pain (0–9 scale for pain in the last 7 days), physical activity using the International Physical Activity Questionnaire ((IPAQ), coded as Inactive/Minimally Active/Active) [26], and psychological distress measured with the Kessler 6 (K6) scale [27] (scores range from 0–15). Data on participant demographics (age, gender, BMI (kg/m2), education level (three levels), and existing total comorbidities were also collected and entered as covariates. Participants were asked to report their total comorbidities from a list of 15 common health conditions, such as cancer, asthma, osteoarthritis, and depression. Work-related factors evaluated at baseline included job satisfaction measured by a single question on a 7 point scale [28], occupational category (three categories), work industry (government/private), the duration of computer usage (</> 6 h per day), and total ergonomic score (assessed on a checklist with scores ranging from 0–38). Information relating to individuals who received workers’ compensation, or those who sought help from a healthcare professional (Yes/No) for their neck/shoulder symptoms in the last 12 months, were also obtained and evaluated at baseline.
Adherence during the 12-week intervention was recorded by the facilitators in the EET and EHP groups and analyzed as a total adherence percentage score. Adherence after the 12-week intervention was monitored but not reported here.
2.5. Data Analysis
The data collected were analyzed according to the intention-to-treat (ITT) and per-protocol principles for all participants. Multiple imputation was performed to impute missing data for individual variables (e.g., age and gender). A comparison of results (with and without imputation) showed no significant differences. The sub-sample analysis of the neck cases only, was also performed using ITT and per-protocol analysis. Cases were defined as those who reported neck pain of three or more on the 10-point scale at baseline [29]. The per-protocol analysis included participants with adherence of ≥70% during the 12-week intervention [30]. Descriptive statistics for between-group differences in the baseline characteristics were performed using t-test for continuous variables and chi-square test for categorical variables. Between-group and within-group changes in work ability were analyzed using the Multilevel Mixed Effects Linear Model with group, time, and group-by-time interactions as the fixed-effects independent variables. The analyses were controlled for age, gender, baseline ergonomic score, whether care was sought from a health professional, and BMI. Organization and cluster were entered into the analyses as random factors.
All data analyses were performed using STATA/IC (Statistical Software for Data Science) version 15 (Stata Corporation, College Station, TX, USA), adopting a statistical significance of p < 0.05.
3. Results
According to the ITT and per-protocol analyses, 350 participants comprised the final sample in this study, as 16 participants discontinued before group allocation (Figure 1). There were no significant between-group differences in any baseline measures. However, the mean total ergonomic score was statistically greater in the EET group (p < 0.05), albeit only by a mean of 0.86 (2%) points, and there was a greater proportion of participants who did not seek health professional help in both the EET and EHP groups (p < 0.05) (Table 1). For all participants, the mean (SD) baseline work ability score for the EET and EHP groups were 8.43 (1.27) and 8.45 (1.25) for the ITT analysis, and similarly in the per-protocol analysis, at 8.45 (1.23) and 8.52 (1.25), respectively. For the sub-sample of neck cases, the mean (SD) baseline work ability score for the EET and EHP groups was 8.31 (1.18) and 8.38 (1.27) for the ITT analysis, and 8.16 (1.17) and 8.42 (1.35) for the per-protocol analysis, respectively.
Adherence during the intervention period ranged from 0 to 100%. The EET intervention had a mean adherence of 60%, while the EHP group had a mean adherence of 55%. For the neck cases, the mean adherence was 63% for EET (8% to 100%) and 54% for EHP (0 to 92%). A total of 116 participants demonstrated ≥70% adherence to the allocated 12 week intervention, with 52% and 48% participants from the EET and EHP groups, respectively.
For all participants, there were no between-group differences, and no group-by-time interaction effect in work ability at 12 weeks or 12 months in the ITT and per-protocol analyses (Table 2). There was also a lack of significant between-group and group-by-time interaction effect for the neck cases using ITT analysis. There was, however, a significant group-by-time interaction effect for the per-protocol analysis of neck cases at 12 weeks (p < 0.05), and a near significant finding at 12 months (p = 0.06) that favored the EET group. This was reflected by the 0.66 (6%) and 0.77 (7%) improvement in mean (SD) work ability score from 8.16 (1.17) at baseline, to 8.82 (0.95) at 12 weeks, and 8.93 (1.14) at 12 months.

Table 2.
Differences in mean work ability scores between groups over time for ITT and Per-protocol analyses a.
Adverse Events
There were two participants who experienced musculoskeletal symptoms during the EET intervention. The intervention physiotherapist followed these participants who both completed the intervention without further problems.
4. Discussion
This study found no significant between-group differences in work ability when participating in an EET intervention or an EHP intervention. However, those who had neck pain at baseline and had completed more than 70% of the EET intervention showed an improvement in work ability at 12 weeks, which appeared to be maintained for the next nine months. In other words, for office workers with neck pain, the EET intervention was superior to the EHP intervention after 12 weeks. These findings partly support our hypothesis that the EET intervention could be more efficacious for improving work ability in office workers, compared to the EHP intervention, and that this effect would be stronger in those with neck pain at baseline.
The parent study, from which this study was derived, was powered to detect a difference in productivity loss between the two groups [10]. However, work ability data were only obtained from half of the sample, which may have been insufficient to detect a change in work ability. This is unlikely as the magnitude of the change in workability of 6%–7% is consistent with previous studies of a smaller (work ability improved by 7% [16]) and similar (work ability improved 4% [21]) sample size. As reported in another study with office workers, Justesen et al. [21] found that office workers had a greater improvement in work ability if adherence was 70% or more. A new finding from this research is that this change was greater in those with neck pain at baseline.
The relatively high mean baseline level of work ability in the moderate/good range [25] may have resulted in a ceiling effect, thereby mitigating the potential for a greater positive change at 12 weeks and 12 months. Various studies have found that the work ability scale may be prone to a ceiling effect [31]. Two intervention studies showed that improvement was especially significant for participants with poor to moderate baseline work abilities [19,31].
The EET intervention targeted individual physical factors, while the EHP intervention addressed psychosocial and work-related factors. The latter factors include health beliefs, mental health issues, healthy diet, job contentment, work attitudes, conflict management and resilience, and maintaining a healthy lifestyle. It has been hypothesized that work ability in office workers is not solely dictated by changes in physical activity but also changes in psychosocial well-being [32]. Therefore, the lack of difference between groups could have resulted from each intervention targeting a different aspect of work ability, with the EET intervention targeting the physical aspect and the EHP intervention targeting the psychosocial and work-related aspect. Another workplace intervention study in Australian office workers found a similar baseline work ability score (8.4/10, [33]). In their study, an activity-based work environment was introduced for 4 weeks but resulted in a reduction in work ability rather than the expected increase.
Future studies should consider interventions that combine exercise with psychosocial and work-related factors, as well as the contemporary workplace environment, as these domains affect work ability [13,33]. Future research should also consider revising the work ability questionnaire to include specific psychosocial and work-related factors, as it currently focuses more on physical factors. This may provide a more sensitive measure of work ability in office workers, the nature of whose work is more mentally demanding than physically demanding.
Strengths and Limitations
These findings can be generalized to all office workers for several reasons. This study was rigorously conducted with a large sample of workers recruited from 14 different organizations, representing both the private and public government workforce. The clustering of participants according to their building, floor, or department was designed to encourage compliance within work teams and minimize contamination bias. Another strength was the range of individual and work-related characteristics evaluated and included for potential confounding.
The limitations of this study were the amount of missing data and low adherence to the intervention. However, adherence to interventions is a common problem reported in similar intervention studies varying from 56% [21] to 81% [17]. In our study, steps were taken to enhance adherence, such as ensuring that the exercises were easy to perform without the need to change or shower, conducted during work hours without leaving the workplace, and required very little equipment. Other measures introduced promoted a group champion and featured regular reminders via email. However, these strategies target the individual and there is evidence to indicate that a more holistic approach that considers the psychosocial work environment and organizational structures is needed to positively impact health behaviours in the workplace [34]. Indeed, a recent qualitative study investigating the barriers to physical exercise in the workplace suggests that the internal organizational working culture is the main barrier to compliance [35].
5. Conclusions
The main finding of this study is that a workplace-based ergonomics and exercise intervention is not superior to ergonomics and health promotion intervention in improving work ability in the general office worker population. However, this intervention was more efficacious in office workers with neck pain at baseline in the short- and potentially the long-term when 70% or more of the exercise sessions were completed. Further improvements in work ability may be possible with interventions that target individual, psychosocial, and work environments.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/16/15/2633/s1, Table S1: CONSORT 2010 checklist of information to include when reporting a randomised trial.
Author Contributions
Conceptualization, V.J. and X.C.; Methodology, V.J., X.C., J.Z.R.T.; Formal Analysis, J.Z.R.T., X.C., V.J.; Investigation, X.C., J.Z.R.T., V.J.; Resources, V.J.; Data Curation, X.C.; Writing—Original Draft Preparation, J.Z.R.T., X.C.; Writing—Review & Editing, V.J., X.C., J.Z.R.T.; Supervision, V.J.; Project Administration, V.J.; Funding Acquisition, V.J.
Funding
This research was funded by The National Health and Medical Research Council (NHMRC) of Australia under Grant #12609000051246.
Acknowledgments
Xiaoqi Chen was supported by an Australian Postgraduate Award. The authors thank the participating organizations for their support of this research study, Alyssa Welch (Project Manager) and Jessica Larkin (Physiotherapist) for their contributions to data collection and project management, and Asad Khan for undertaking the cluster randomization process.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Pereira, M.J.; Johnston, V.; Straker, L.M.; Sjøgaard, G.; Melloh, M.; O’Leary, S.P.; Comans, T.A. An investigation of self-reported health-related productivity losses in office workers and associations with individual and work-related factors using an employer’s perspective. JOEM 2017, 59, e138–e144. [Google Scholar] [PubMed]
- Cote, P.; van der Velde, G.; Cassidy, J.D.; Carroll, L.J.; Hogg-Johnson, S.; Holm, L.W.; Carragee, E.J.; Haldeman, S.; Nordin, M.; Hurwitz, E.L.; et al. The burden and determinants of neck pain in workers: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. J. Manipulative Physiol. Ther. 2009, 32, S70–S86. [Google Scholar] [CrossRef] [PubMed]
- Van Eerd, D.; Côté, P.; Kristman, V.; Rezai, M.; Hogg-Johnson, S.; Vidmar, M.; Dorcas, D. The Course of Work Absenteeism Involving Neck Pain A Cohort Study of Ontario Lost-Time Claimants. Spine 2011, 36, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, M.; Tornqvist, E.W.; Toomingas, A. Self-reported reduced productivity due to musculoskeletal symptoms: Associations with workplace and individual factors among white-collar computer users. J. Occup. Rehabil. 2002, 12, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Aas, R.W.; Tuntland, H.; Holte, K.A.; Roe, C.; Lund, T.; Marklund, S.; Moller, A. Workplace interventions for neck pain in workers. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef] [PubMed]
- Leyshon, R.; Chalova, K.; Gerson, L.; Savtchenko, A.; Zakrzewski, R.; Howie, A.; Shaw, L. Ergonomic interventions for office workers with musculoskeletal disorders: A systematic review. Work 2010, 35, 335–348. [Google Scholar] [PubMed]
- Chen, X.; Coombes, B.K.; Sjogaard, G.; Jun, D.; O’Leary, S.; Johnston, V. Workplace-Based Interventions for Neck Pain in Office Workers: Systematic Review and Meta-Analysis. Phys. Ther. 2018, 98, 40–62. [Google Scholar] [CrossRef] [PubMed]
- Sihawong, R.; Janwantanakul, P.; Sitthipornvorakul, E.; Pensri, P. Exercise therapy for office workers with nonspecific neck pain: A systematic review. J. Manipulative Physiol. Ther. 2011, 34, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Van Eerd, D.; Munhall, C.; Irvin, E.; Rempel, D.; Brewer, S.; van der Beek, A.J.; Dennerlein, J.T.; Tullar, J.; Skivington, K.; Pinion, C.; et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup. Environ. Med. 2016, 73, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.; Comans, T.; Sjogaard, G.; Straker, L.; Melloh, M.; O’Leary, S.; Chen, X.; Johnston, V. The impact of workplace ergonomics and neck-specific exercise versus ergonomics and health promotion interventions on office worker productivity: A cluster-randomized trial. Scand. J. Work Environ. Health 2019, 45, 42–52. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, J. Work ability—A comprehensive concept for occupational health research and prevention. Scand. J. Work Environ. Health 2009, 35, 1–5. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, T.I.; Elders, L.A.; de Zwart, B.C.; Burdorf, A. The effects of work-related and individual factors on the Work Ability Index: A systematic review. Occup. Environ. Med. 2009, 66, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Kuoppala, J.; Lamminpaa, A.; Husman, P. Work health promotion, job well-being, and sickness absences—A systematic review and meta-analysis. J. Occup. Environ. Med. 2008, 50, 1216–1227. [Google Scholar] [CrossRef] [PubMed]
- Schouten, L.S.; Joling, C.I.; van der Gulden, J.W.; Heymans, M.W.; Bultmann, U.; Roelen, C.A. Screening manual and office workers for risk of long-term sickness absence: Cut-off points for the Work Ability Index. Scand. J. Work Environ. Health 2015, 41, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Nurminen, E.; Malmivaara, A.; Ilmarinen, J.; Ylostalo, P.; Mutanen, P.; Ahonen, G.; Aro, T. Effectiveness of a worksite exercise program with respect to perceived work ability and sick leaves among women with physical work. Scand. J. Work Environ. Health 2002, 28, 85–93. [Google Scholar] [CrossRef]
- Barene, S.; Krustrup, P.; Holtermann, A. Effects of the Workplace Health Promotion Activities Soccer and Zumba on Muscle Pain, Work Ability and Perceived Physical Exertion among Female Hospital Employees. PLoS ONE 2014, 9, e115059. [Google Scholar] [CrossRef]
- Sundstrup, E.; Jakobsen, M.D.; Brandt, M.; Jay, K.; Persson, R.; Aagaard, P.; Andersen, L.L. Workplace strength training prevents deterioration of work ability among workers with chronic pain and work disability: A randomized controlled trial. Scand. J. Work Environ. Health 2014, 40, 244–251. [Google Scholar] [CrossRef]
- Jorgensen, M.B.; Faber, A.; Hansen, J.V.; Holtermann, A.; Sogaard, K. Effects on musculoskeletal pain, work ability and sickness absence in a 1-year randomised controlled trial among cleaners. BMC Public Health 2011, 11, 840–851. [Google Scholar] [CrossRef]
- Kettunen, O.; Vuorimaa, T.; Vasankari, T. 12-Mo Intervention of Physical Exercise Improved Work Ability, Especially in Subjects with Low Baseline Work Ability. Int. J. Environ. Res. Public Health 2014, 11, 3859–3869. [Google Scholar] [CrossRef]
- Martimo, K.P.; Shiri, R.; Miranda, H.; Ketola, R.; Varonen, H.; Viikari-Juntura, E. Effectiveness of an ergonomic intervention on the productivity of workers with upper-extremity disorders—A randomized controlled trial. Scand. J. Work. Environ. Health 2010, 36, 25–33. [Google Scholar] [CrossRef][Green Version]
- Justesen, J.B.; Sogaard, K.; Dalager, T.; Christensen, J.R.; Sjogaard, G. The Effect of Intelligent Physical Exercise Training on Sickness Presenteeism and Absenteeism among Office Workers. J. Occup. Environ. Med. 2017, 59, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Johnston, V.; O’Leary, S.; Comans, T.; Straker, L.; Melloh, M.; Khan, A.; Sjogaard, G. A workplace exercise versus health promotion intervention to prevent and reduce the economic and personal burden of non-specific neck pain in office personnel: Protocol of a cluster-randomised controlled trial. J. Physiother. 2014, 60, 233. [Google Scholar] [CrossRef]
- Campbell, M.K.; Elbourne, D.R.; Altman, D.G. CONSORT statement: Extension to cluster randomised trials. BMJ 2004, 328, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Comcare, C.O.A. Officewise: A Guide to Health and Safety in the Office; Commonwealth of Australia: Canberra, Australia, 2008; pp. 1–90. [Google Scholar]
- El Fassi, M.; Bocquet, V.; Majery, N.; Lair, M.L.; Couffignal, S.; Mairiaux, P. Work ability assessment in a worker population: Comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health 2013, 13, 305. [Google Scholar] [CrossRef] [PubMed]
- IPAQ Research Committee. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms. Available online: https://www.researchgate.net/file.PostFileLoader.html?id=5641f4c36143250eac8b45b7&assetKey=AS%3A294237418606593%401447163075131 (accessed on 23 July 2019).
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Wanous, J.P.; Hudy, M.J. Single-item reliability: A replication and extension. Organ. Res. Methods 2001, 4, 361–375. [Google Scholar] [CrossRef]
- Kaergaard, A.; Andersen, J.H.; Rasmussen, K.; Mikkelsen, S. Identification of neck-shoulder disorders in a 1 year follow-up study. Validation of a questionnaire-based method. Pain 2000, 86, 305–310. [Google Scholar] [CrossRef]
- Dalager, T.; Justesen, J.B.; Sjogaard, G. Intelligent Physical Exercise Training in a Workplace Setting Improves Muscle Strength and Musculoskeletal Pain: A Randomized Controlled Trial. Biomed Res. Int. 2017. [Google Scholar] [CrossRef]
- Larsson, A.; Karlqvist, L.; Gard, G. Effects of work ability and health promoting interventions for women with musculoskeletal symptoms: A 9-month prospective study. BMC Musculoskelet. Disord. 2008, 9, 105. [Google Scholar] [CrossRef]
- Sjogren-Ronka, T.; Ojanen, M.T.; Leskinen, E.K.; Tmustalampi, S.; Malkia, E.A. Physical and psychosocial prerequisites of functioning in relation to work ability and general subjective well-being among office workers. Scand. J. Work Environ. Health 2002, 28, 184–190. [Google Scholar] [CrossRef]
- Foley, B.; Engelen, L.; Gale, J.; Bauman, A.; Mackey, M. Sedentary Behavior and Musculoskeletal Discomfort Are Reduced When Office Workers Trial an Activity-Based Work Environment. J. Occup. Environ. Med. 2016, 58, 924–931. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Five Keys to Healthy Workplaces: No Business Wealth without Workers’ Health. Available online: http://www.who.int/occupational_health/5keys_healthy_workplaces.pdf?ua=1 (accessed on 5 July 2019).
- Bredahl, T.V.; Saervoll, C.A.; Kirkelund, L.; Sjogaard, G.; Andersen, L.L. When Intervention Meets Organisation, a Qualitative Study of Motivation and Barriers to Physical Exercise at the Workplace. Sci. World J. 2015, 518–561. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).