Primary Care Networks and Eritrean Immigrants’ Experiences with Health Care Professionals in Switzerland: A Qualitative Approach
Abstract
:1. Introduction
2. Materials and Methods
3. Results
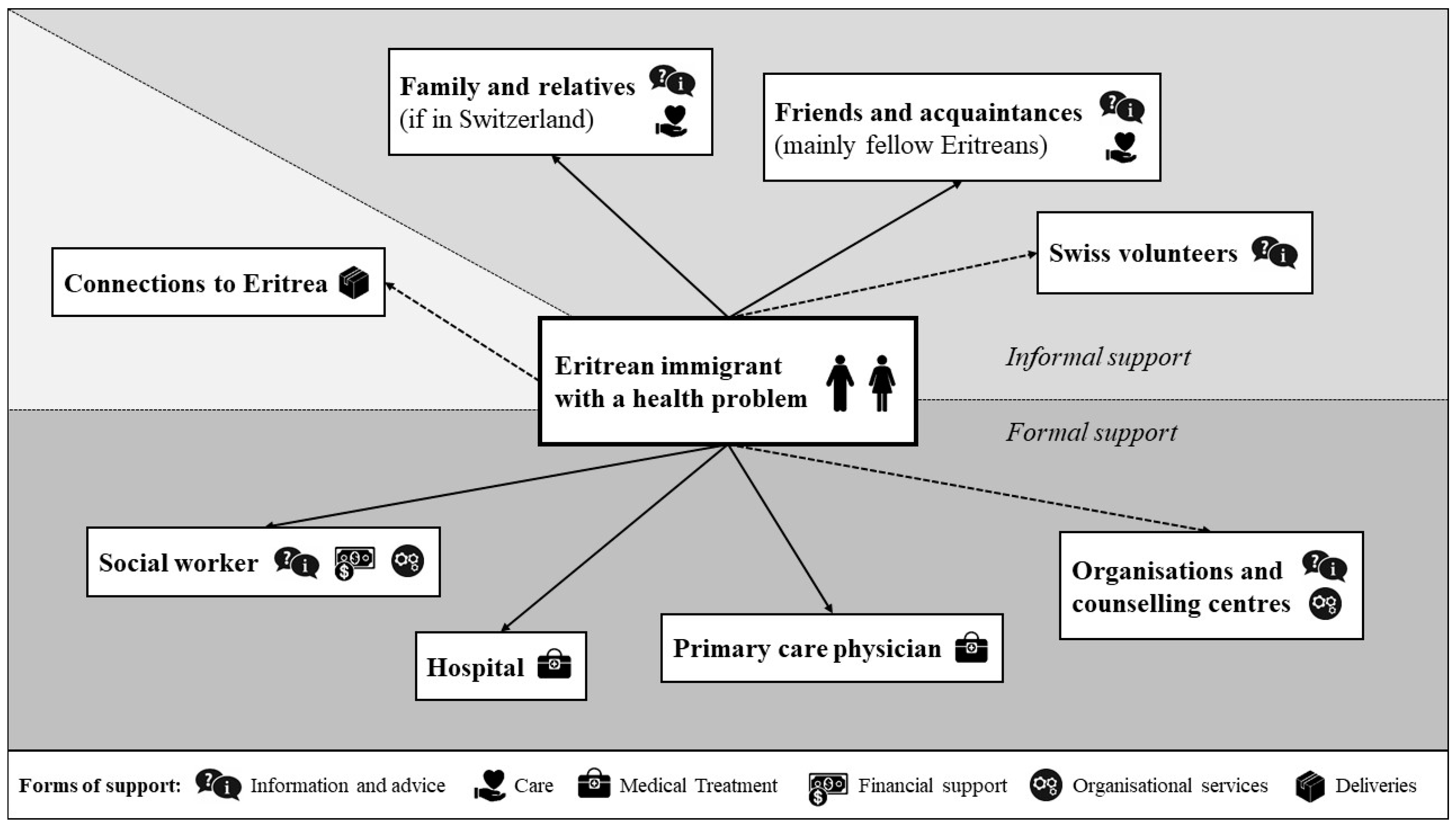
3.1. The Primary Care Networks of Eritrean Immigrants in Switzerland
3.1.1. Informal Support
3.1.2. Formal Support
3.2. Six Key Lessons for Practice
3.2.1. The Challenge of Finding One’s Way in a New Health Care System
3.2.2. The Relevance of Clear and Sometimes More Detailed Explanations
3.2.3. Appropriate Communication to Overcome Language Barriers
3.2.4. Cultural Differences Regarding Gender
3.2.5. Mental Health as a Taboo Topic
3.2.6. Differences in Individual Situations and Cultural Backgrounds among People from the Same Country
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations (Departement of Economic and Social Affairs, Population Division). International Migration Report 2017: Highlights; United Nations: New York, NY, USA, 2017. Available online: http://www.un.org/en/development/desa/population/migration/publications/migrationreport/docs/MigrationReport2017_Highlights.pdf (accessed on 22 June 2019).
- Kristensen, E.; Rausa, F.; Heiniger, M. Statistischer Bericht zur Integration der Bevölkerung mit Migrationshintergrund; Bundesamt für Statistik: Neuchâtel, Switzerland, 2017; Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/bevoelkerung/migration-integration.assetdetail.2546310.htm (accessed on 20 June 2019).
- Grützmann, T.; Rose, C.; Peters, T. Interkulturelle Kompetenz in der medizinischen Praxis. Ethik Med. 2012, 24, 323–334. [Google Scholar] [CrossRef]
- Blaser, A.; Gasser, K.; Spang, T. National Programme on Migration and Health: 2008–2013 results and priorities for 2014–2017; Federal Office of Public Health FOPH: Berne, Switzerland, 2013.
- Schweizerisches Rotes Kreuz (Ed.) Transkulturelle Public Health: Ein Weg zur Chancengleichheit; Seismo: Zürich, Switzerland, 2012. [Google Scholar]
- World Health Organization (Regional Office for Europe). Report on the Health of Refugees and Migrants in the WHO European Region: No Public Health without Refugees and Migrant Health—Summary; WHO: Copenhagen, Denmark, 2018; Available online: https://apps.who.int/iris/handle/10665/311348 (accessed on 22 June 2019).
- Puchner, K.; Karamagioli, E.; Pikouli, A.; Tsiamis, C.; Kalogeropoulos, A.; Kakalou, E.; Pavlidou, E.; Pikoulis, E. Time to Rethink Refugee and Migrant Health in Europe: Moving from Emergency Response to Integrated and Individualized Health Care Provision for Migrants and Refugees. Int. J. Environ. Res. Public Health 2018, 15, 1100. [Google Scholar] [CrossRef] [PubMed]
- Lattof, S.R.; Coast, E.; Leone, T. Priorities and Challenges Accessing Health care Among Female Migrants. Health Serv. Insights 2018, 11, 1–5. [Google Scholar] [CrossRef] [PubMed]
- San Giorgi, M. The Human Right to Equal Access to Health Care; Intersentia: Cambridge, UK, 2012. [Google Scholar]
- Ledoux, C.; Pilot, E.; Diaz, E.; Krafft, T. Migrants’ access to healthcare services within the European Union: A content analysis of policy documents in Ireland, Portugal and Spain. Glob. Health 2018, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Mladovsky, P.; Rechel, B.; Ingleby, D.; McKee, M. Responding to diversity: An exploratory study of migrant health policies in Europe. Health Policy 2012, 105, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bundesamt für Gesundheit BAG (Ed.) Gesundheit der Migrantinnen und Migranten in der Schweiz: Wichtigste Ergebnisse des zweiten Gesundheitsmonitorings der Migrationsbevölkerung in der Schweiz, 2010; BAG: Bern, Switzerland, 2012; Available online: https://www.ub.unibas.ch/digi/a125/sachdok/2014/BAU_1_6295616.pdf (accessed on 20 June 2019).
- Guggisberg, J.; Gardiol, L.; Graf, I.; Oesch, T.; Künzi, K.; Volken, T.; Rüesch, P.; Abel, T.; Ackermann, S.; Müller, C. Gesundheitsmonitoring der Migrationsbevölkerung (GMM) in der Schweiz: Schlussbericht. 2011. Available online: https://www.buerobass.ch/fileadmin/Files/2011/SCHLUSSBERICHT_GMMII_20110916.pdf (accessed on 22 June 2019).
- Gasser, K.; Houmard, S. Soziale Benachteiligung erzeugt ungleiche Gesundheitschancen. Spectra Gesundh. Prävent. 2018, 119, 2–3. [Google Scholar]
- Wimmer-Puchinger, B.; Wolf, H.; Engleder, A. Migrantinnen im Gesundheitssystem: Inanspruchnahme, Zugangsbarrieren und Strategien zur Gesundheitsförderung. Bundesgesundheitsblatt Gesundh. Gesundh. 2006, 49, 884–892. [Google Scholar] [CrossRef] [PubMed]
- Schweizerisches Gesundheitsobservatorium (Ed.) Gesundheit in der Schweiz: Fokus Chronische Erkrankungen: Nationaler Gesundheitsbericht 2015; Hogrefe: Bern, Switzerland, 2015. [Google Scholar]
- Abebe, D.S.; Lien, L.; Hjelde, K.H. What we know and don’t know about mental health problems among Immigrants in Norway. J. Immigr. Minor Health 2014, 16, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Mohammed, S.A.; Leavell, J.; Collins, C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann. N. Y. Acad. Sci. 2010, 1186, 69–101. [Google Scholar] [CrossRef] [PubMed]
- Agudelo-Suárez, A.A.; Gil-González, D.; Vives-Cases, C.; Love, J.G.; Wimpenny, P.; Ronda-Pérez, E. A metasynthesis of qualitative studies regarding opinions and perceptions about barriers and deter-minants of health services’ accessibility in economic migrants. BMC Health Serv. Res. 2012, 12, 461. [Google Scholar] [CrossRef] [PubMed]
- Sottas, B.; Brügger, S.; Jaquier, A. Zugangsprobleme zur Gesundheitsversorgung? Eine Explorative Studie auf Grund von Expertengesprächen: Schlussbericht; Sottas Formative Works: Bourguillon, Switzerland, 2014; Available online: https://skos.ch/fileadmin/user_upload/skos_main/public/pdf/grundlagen_und_positionen/themendossiers/Gesundheit/zugangsprobleme-gesundheitsversorgung.pdf (accessed on 22 June 2019).
- Rüefli, C. Grundlagenanalyse zur Zukunft des Themas Migration und Gesundheit beim Bund (Zusammenfassung); Büro Vatter: Bern, Switzerland, 2015; Available online: https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/gesundheitliche-chancengleichheit/programm-migration-und-gesundheit-2002-2017.html (accessed on 21 June 2019).
- Oetterli, M.; Laubereau, B.; Krongrava, P.; Essig, S.; Studer, C. Unterstützung von Hausärzten/-innen bei der Behandlung von Patienten/-innen mit Migrationshintergrund: Situationsanalyse, Handlungsbedarf und Empfehlungen zu Massnahmen: Studie zuhanden der Sektion Migration und Gesundheit des Bundesamtes für Gesundheit (BAG) und der Dienststelle Soziales und Gesellschaft (DISG) des Kantons Luzern; Interface Politikstudien Forschung Beratung and Institut für Hausarztmedizin und Community Care IHAM&CC: Luzern, Switzerland, 2016; Available online: https://www.interface-pol.ch/app/uploads/2018/09/Be_Hausaerzte_Migration.pdf (accessed on 22 June 2019).
- Priebe, S.; Sandhu, S.; Dias, S.; Gaddini, A.; Greacen, T.; Ioannidis, E.; Kluge, U.; Krasnik, A.; Lamkaddem, M.; Lorant, V.; et al. Good practice in health care for migrants: Views and experiences of care professionals in 16 European countries. BMC Public Health 2011, 11, 187. [Google Scholar] [CrossRef] [PubMed]
- Ackermann Rau, S.; Sakarya, S.; Abel, T. When to see a doctor for common health problems: Distribution patterns of functional health literacy across migrant populations in Switzerland. Int. J. Public Health 2014, 59, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Pfluger, T.; Biedermann, A.; Salis Gross, C. Transkulturelle Prävention und Gesundheitsförderung in der Schweiz: Grundlagen und Empfehlungen; Public Health Services: Herzogenbuchsee, Switzerland, 2009.
- Eyer, P.; Schweizer, R. Die somalische und die eritreische Diaspora in der Schweiz; BBL: Bern, Switzerland, 2010. [Google Scholar]
- Christen, D.; Balthasar, A. Approaches to improve the interaction between general practitioners and migrants—A systematic review of international literature. Int. J. Migr. Health Soc. Care 2017, 13, 321–333. [Google Scholar] [CrossRef]
- Rey, L. Sprachliche Brücken zur Genesung: Interkulturelles Übersetzen im Gesundheitswesen der Schweiz; Bundesamt für Gesundheit BAG: Bern, Switzerland, 2017. [Google Scholar]
- Cheng, I.-H.; Drillich, A.; Schattner, P. Refugee experiences of general practice in countries of re-settle-ment: A literature review. Br. J. Gen. Pract. 2015, 65, e171–e176. [Google Scholar] [CrossRef] [PubMed]
- Staatssekretariat für Migration SEM (Ed.) Ausländer-und Asylstatistik 2018; SEM: Bern-Wabern, Switzerland, 2019; Available online: https://www.sem.admin.ch/sem/de/home/publiservice/publikationen.html (accessed on 20 June 2019).
- Navarra, K.; Liewald, K. Gesundheitswegweiser Schweiz: Das Schweizerische Gesundheitssystem kurz erklärt—Ein Ratgeber für Migrantinnen und Migranten in der Schweiz, 4th ed.; Federal Office of Public Health FOPH & Schweizerisches Rotes Kreuz: Bern-Wabern, Switzerland, 2017. Available online: https://www.migesplus.ch/publikationen/gesundheitswegweiser-schweiz (accessed on 20 June 2019).
- Schweizerische Interessengemeinschaft für Interkulturelles Dolmetschen und Vermitteln INTERPRET. Vermittlungsstellen für Interkulturelles Dolmetschen (Mai 2019). Available online: https://www.inter-pret.ch/de/angebote/regionale-vermittlungsstellen-44.html (accessed on 20 June 2019).
- Von Ameln, F. Soziales Atom/Rollenatom. In Diagnostik im Coaching: Grundlagen, Analyseebenen, Praxisbeispiele; Möller, H., Kotte, S., Eds.; Springer: Berlin, Germany, 2013; pp. 251–261. [Google Scholar]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; Sage: London, UK, 2013. [Google Scholar]
- Thiel, R.; Deimel, L.; Schmidtmann, D.; Piesche, K.; Hüsing, T.; Rennoch, J.; Stroetmann, V.; Stroetmann, K.; Kostera, T. #SmartHealthSystems: Digitalisierungsstrategien im Internationalen Vergleich: Gesundheitssystem-Vergleich Fokus Digitalisierung Smart Health Systems; Bertelsmann Stiftung: Gütersloh, Germany, 2018. [Google Scholar]
- Spiess, R.; Kilcher, A. Arzt-Patienten-Interaktion im Migrationskontext. Praxis 2003, 92, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Ilkilic, I. Medizinische Aspekte des interkulturellen Arzt-Patienten-Verhältnisses. In Migration und Gesundheit: Kulturelle Vielfalt als Herausforderung für die Medizinische Versorgung; Ethikrat, D., Ed.; Dt. Ethikrat: Berlin, Germany, 2010; pp. 29–40. [Google Scholar]
- Kleinman, A.; Eisenberg, L.; Good, B. Culture, illness, and care: Clinical lessons from anthropologic and cross-cultural research. Ann. Int. Med. 1978, 88, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Horn, A.; Vogt, D.; Messer, M.; Schaeffer, D. Health Literacy von Menschen mit Migrationshinter grund in der Patientenberatung stärken: Ergebnisse einer qualitativen Evaluation. Bundesgesundheitsblatt Gesundh. Gesundh. 2015, 58, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Broszinsky-Schwabe, E. Interkulturelle Kommunikation: Missverständnisse und Verständigung, 2nd ed.; Springer: Wiesbaden, Switzerland, 2017. [Google Scholar]
- Domenig, D. Migrationsspezifische Aspekte der gesundheitlichen Chancengleichheit. In Transkulturelle Public Health: Ein Weg zur Chancengleichheit; Schweizerisches Rotes Kreuz, Ed.; Seismo: Zürich, Switzerland, 2012; pp. 18–35. [Google Scholar]
- Kläui, H. Diversität, transkulturelle Kompetenz und die hausärztliche Praxis: Chancengleichheit in der medizinischen Grundversorgung. In Transkulturelle Public Health: Ein Weg zur Chancengleichheit; Schweizerisches Rotes Kreuz, Ed.; Seismo: Zürich, Switzerland, 2012; pp. 118–128. [Google Scholar]
- Kayser, A.; Bühlmann, R. Transkulturelle Kompetenz: Herausforderungen für die Weiterbildung und Umsetzung im Arbeitsfeld. In Transkulturelle Public Health: Ein Weg zur Chancengleichheit; Schweizerisches Rotes Kreuz, Ed.; Seismo: Zürich, Switzerland, 2012; pp. 41–58. [Google Scholar]
- Asefaw, F. Weibliche Genitalbeschneidung: Hintergründe, gesundheitliche Folgen und Nachhaltige Prävention; Boox-verlag: Urnäsch, Switzerland, 2017. [Google Scholar]
- Lipson, J.; Afaf, M. Methodological issues in research with immigrants. Med. Anthropol. 1989, 12, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Pernice, R. Methodological issues in research with refugees and immigrants. Prof. Psychol. Res. Pract. 1994, 25, 207–213. [Google Scholar] [CrossRef]
| Demographic Characteristics | N = 8 |
|---|---|
| Gender (n) | Female (4), male (4) |
| Age in years (mean) | 26–53 (41.1) |
| Place of birth (n) | Eritrea (6), Ethiopia (1), Sudan (1) |
| Duration of stay in Switzerland in years (mean) | 6–33 (13.6) |
| Duration of activity as an intercultural interpreter in years (mean) | 1–8 (5.3) |
| Languages spoken (n) | Covered by all: Tigrinya (8), English (8), German (8) Further: Amharic (6), Tigre (2), Bilen (1), Arabic (1), French (1), Italian (1) |
| Educational background (n) (education was acquired in Eritrea or in Switzerland. Some participants had completed several studies or training courses) | Tertiary education in social, health, natural or environmental sciences (4), nursing (2), education in the fields of clothing and beauty (2), secondary school (1) |
| Religious affiliation (n) | Orthodox (4), Catholic (2), Protestant (1), non-denominational (1) |
| Work Characteristics | |
| Geographical area of activity | Urban and rural areas in German-speaking Switzerland |
| Main fields of activity in health care | Hospitals, in particular maternity wards, surgical wards, mental health facilities, and with primary care physicians |
| Characteristics of their clients | Eritrean immigrants of all ages with a lack of local language skills, most of them living in Switzerland for less than five years (sometimes up to 10 years) |
| Frequency of interpreting | About 3–5 assignments per week |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wallimann, C.; Balthasar, A. Primary Care Networks and Eritrean Immigrants’ Experiences with Health Care Professionals in Switzerland: A Qualitative Approach. Int. J. Environ. Res. Public Health 2019, 16, 2614. https://doi.org/10.3390/ijerph16142614
Wallimann C, Balthasar A. Primary Care Networks and Eritrean Immigrants’ Experiences with Health Care Professionals in Switzerland: A Qualitative Approach. International Journal of Environmental Research and Public Health. 2019; 16(14):2614. https://doi.org/10.3390/ijerph16142614
Chicago/Turabian StyleWallimann, Carla, and Andreas Balthasar. 2019. "Primary Care Networks and Eritrean Immigrants’ Experiences with Health Care Professionals in Switzerland: A Qualitative Approach" International Journal of Environmental Research and Public Health 16, no. 14: 2614. https://doi.org/10.3390/ijerph16142614
APA StyleWallimann, C., & Balthasar, A. (2019). Primary Care Networks and Eritrean Immigrants’ Experiences with Health Care Professionals in Switzerland: A Qualitative Approach. International Journal of Environmental Research and Public Health, 16(14), 2614. https://doi.org/10.3390/ijerph16142614




