The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
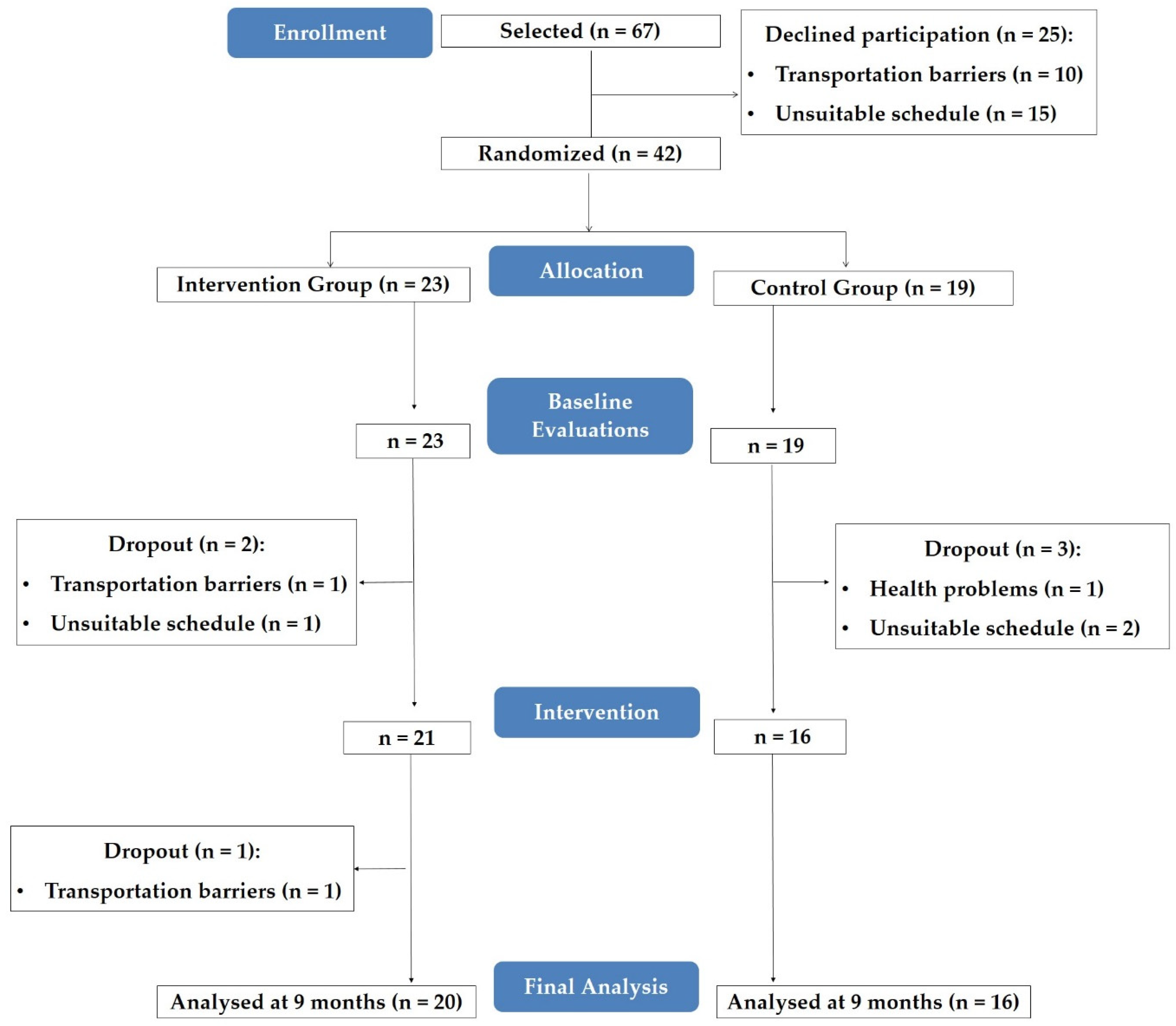
2.1. Study Design
2.2. Participants
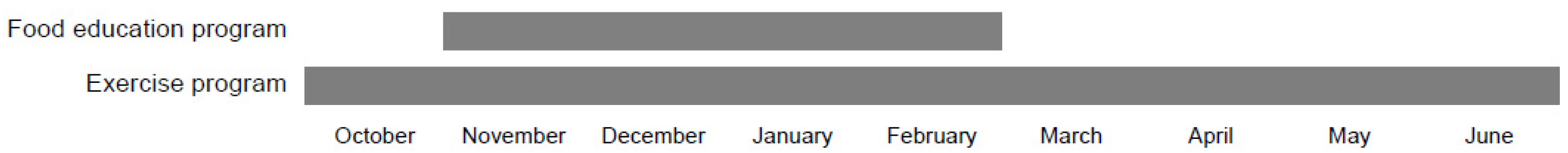
2.3. Exercise Program
2.4. Food Education Program
2.5. Evaluations
2.6. Data Analysis
3. Results
3.1. Program Implementation
3.2. Participants’ Characteristics
3.3. Nutrition-Related Knowledge
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tabish, S.A. Is Diabetes Becoming the Biggest Epidemic of the Twenty-first Century? Int. J. Health Sci. 2007, 1, 5–8. [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas; IDF: Brussels, Belgium, 2017. [Google Scholar]
- Sociedade Portuguesa de Diabetologia. Diabetes: Factos e Números: O ano de 2015 Lisboa: Sociedade Portuguesa de Diabetologia; SPD: Lisboa, Portugal, 2016. [Google Scholar]
- La Puente, J.B.-D.; Mundet-Tudurí, X.; Casellas, A.; Fernandez-Real, J.M.; Mauricio, D.; Mata-Cases, M.; Franch-Nadal, J.; Mundet-Tuduri, X.; Fernández-Real, J.M.; Mata-Cases, M.; et al. Older type 2 diabetic patients are more likely to achieve glycaemic and cardiovascular risk factors targets than younger patients: Analysis of a primary care database. Int. J. Clin. Pr. 2015, 69, 1486–1495. [Google Scholar] [CrossRef] [PubMed]
- Chawla, A.; Chawla, R.; Jaggi, S. Microvasular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J. Endocrinol. Metab. 2016, 20, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Shan, P.-F.; Li, Q.; Khamaisi, M.; Qiang, G.-F. Type 2 Diabetes Mellitus and Macrovascular Complications. Int. J. Endocrinol. 2017, 2017, 4301461. [Google Scholar] [CrossRef] [PubMed]
- Ricci-Cabello, I.; Ruiz-Pérez, I.; Rojas-García, A.; Pastor, G.; Rodríguez-Barranco, M.; Gonçalves, D.C. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: A systematic review, meta-analysis and meta-regression. BMC Endocr. Disord. 2014, 14, 60. [Google Scholar] [CrossRef] [PubMed]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014, 37 (Suppl. 1), S120–S143. [Google Scholar] [CrossRef] [PubMed]
- Vijan, S.; Stuart, N.S.; Fitzgerald, J.T.; Ronis, D.L.; Hayward, R.A.; Slater, S.; Hofer, T.P. Barriers to following dietary recommendations in Type 2 diabetes. Diabet. Med. 2005, 22, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Spronk, I.; Kullen, C.; Burdon, C.; O’Connor, H. Relationship between nutrition knowledge and dietary intake. Br. J. Nutr. 2014, 111, 1713–1726. [Google Scholar] [CrossRef]
- Breen, C.; Ryan, M.; Gibney, M.J.; O’Shea, D. Diabetes-related nutrition knowledge and dietary intake among adults with type 2 diabetes. Br. J. Nutr. 2015, 114, 439–447. [Google Scholar] [CrossRef]
- Doherty, M.L.; Owusu-Dabo, E.; Kantanka, O.S.; O Brawer, R.; Plumb, J.D. Type 2 diabetes in a rapidly urbanizing region of Ghana, West Africa: A qualitative study of dietary preferences, knowledge and practices. BMC Public Health 2014, 14, 1069. [Google Scholar] [CrossRef]
- Fitzgerald, N.; Damio, G.; Segura-Pérez, S.; Pérez-Escamilla, R. Nutrition Knowledge, Food Label Use, and Food Intake Patterns among Latinas with and without Type 2 Diabetes. J. Am. Diet. Assoc. 2008, 108, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Klupa, T.; Możdżan, M.; Kokoszka-Paszkot, J.; Kubik, M.; Masierek, M.; Czerwińska, M.; Małecki, M.T. Diet-Related Knowledge and Physical Activity in a Large Cohort of Insulin-Treated Type 2 Diabetes Patients: PROGENS ARENA Study. Int. J. Endocrinol. 2016, 2016, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ranasinghe, P.; Pigera, A.S.A.D.; Ishara, M.H.; Jayasekara, L.M.D.T.; Jayawardena, R.; Katulanda, P. Knowledge and perceptions about diet and physical activity among Sri Lankan adults with diabetes mellitus: A qualitative study. BMC Public Health 2015, 15, 1047. [Google Scholar] [CrossRef] [PubMed]
- Haas, L.; Maryniuk, M.; Beck, J.; Cox, C.E.; Duker, P.; Edwards, L.; Fisher, E.; Hanson, L.; Kent, D.; Kolb, L.; et al. National Standards for Diabetes Self-Management Education and Support. Diabetes Educ. 2012, 38, 619–629. [Google Scholar] [CrossRef] [PubMed]
- Norris, S.L.; Engelgau, M.M.; Narayan, K.V. Effectiveness of Self-Management Training in Type 2 Diabetes: A systematic review of randomized controlled trials. Diabetes Care 2001, 24, 561–587. [Google Scholar] [CrossRef] [PubMed]
- Laranjo, L.; Neves, A.L.; Costa, A.; Ribeiro, R.T.; Couto, L.; Sá, A.B. Facilitators, barriers and expectations in the self-management of type 2 diabetes—a qualitative study from Portugal. Eur. J. Gen. Pr. 2015, 21, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Heller, S.; Skinner, T.C.; Campbell, M.J.; E Carey, M.; Cradock, S.; Dallosso, H.M.; Daly, H.; Doherty, Y.; Eaton, S.; et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: Cluster randomised controlled trial. BMJ 2008, 336, 491–495. [Google Scholar] [CrossRef]
- Glanz, K.; Rimer, B.; Viswarath, K. Health Behavior and Health Education: Theory, Research and Practice, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Brand, T.; Pischke, C.R.; Steenbock, B.; Schoenbach, J.; Poettgen, S.; Samkange-Zeeb, F.; Zeeb, H. What Works in Community-Based Interventions Promoting Physical Activity and Healthy Eating? A Review of Reviews. Int. J. Environ. Res. Public Health 2014, 11, 5866–5888. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Coveney, J.; Cox, D. Exploring nutrition knowledge and the demographic variation in knowledge levels in an Australian community sample. Public Health Nutr. 2008, 11, 1365–1371. [Google Scholar] [CrossRef]
- Song, H.-J.; Han, H.-R.; Lee, J.-E.; Kim, J.; Kim, K.B.; Nguyen, T.; Kim, M.T. Translating Current Dietary Guidelines into a Culturally Tailored Nutrition Education Program for Korean American Immigrants with Type 2 Diabetes. Diabetes Educ. 2010, 36, 752–761. [Google Scholar] [CrossRef]
- Mendes, R.; Sousa, N.; Reis, V.M.; Themudo-Barata, J.L. Implementing Low-Cost, Community-Based Exercise Programs for Middle-Aged and Older Patients with Type 2 Diabetes: What Are the Benefits for Glycemic Control and Cardiovascular Risk? Int. J. Environ. Res. Public Health 2017, 14, 1057. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.; Sousa, N.; Themudo-Barata, J.; Reis, V. Impact of a community-based exercise programme on physical fitness in middle-aged and older patients with type 2 diabetes. Gac. Sanit. 2016, 30, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.; Sousa, N.; Almeida, A.; Subtil, P.; Guedes-Marques, F.; Reis, V.M.; Themudo-Barata, J.L. Exercise prescription for patients with type 2 diabetes-a synthesis of international recommendations: Narrative review. Br. J. Sports Med. 2016, 50, 1379–1381. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Singh, M.A.F.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. Diabetes Education Modules; IDF: Brussels, Belgium, 2011; Available online: https://d-net.idf.org/en/library/178-diabetes-education-modules-2011.html (accessed on 15 May 2019).
- Souza, J. Conhecimentos Nutritionais: Reprodução e Validação do Questionário. Master’s Thesis, University of Porto, Porto, Portugal, 2009. Available online: https://bibliotecadigital.ipb.pt/bitstream/10198/4274/1/tese%20de%20mestrado.pdf (accessed on 15 May 2019).
- Parmenter, K.; Wardle, J. Development of a general nutrition knowledge questionnaire for adults. Eur. J. Clin. Nutr. 1999, 53, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Guerreiro, M.; Silva, A.; Botelho, M.; Leitão, O.; Castro-Caldas, A.; Garcia, C. Adaptação à população portuguesa da tradução do Mini Mental State Examination. Rev. Port Neurol. 1994, 1, 9–10. [Google Scholar]
- Kullen, C.J.; Iredale, L.; Prvan, T.; O’Connor, H.T. Evaluation of General Nutrition Knowledge in Australian Military Personnel. J. Acad. Nutr. Diet. 2016, 116, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Rolstad, S.; Adler, J.; Ryden, A. Response Burden and Questionnaire Length: Is Shorter Better? A Review and Meta-analysis. Value Health 2011, 14, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sánchez, A.E.; Ávila-Ortíz, M.N. Changing Dietary Habits in Persons Living with Type 2 Diabetes. J. Nutr. Educ. Behav. 2013, 45, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Goodarzi, M.; Ebrahimzadeh, I.; Rabi, A.; Saedipoor, B.; Jafarabadi, M.A. Impact of distance education via mobile phone text messaging on knowledge, attitude, practice and self efficacy of patients with type 2 diabetes mellitus in Iran. J. Diabetes Metab. Disord. 2012, 11, 10. [Google Scholar] [CrossRef]
- Islam, N.S.; Wyatt, L.C.; Taher, M.; Riley, L.; Tandon, S.D.; Tanner, M.; Mukherji, B.R.; Trinh-Shevrin, C. A Culturally Tailored Community Health Worker Intervention Leads to Improvement in Patient-Centered Outcomes for Immigrant Patients with Type 2 Diabetes. Clin. Diabetes 2018, 36, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, M.; Fan, R.; Ma, X.; Gu, J.; Cai, X.; Liu, R.; Chen, Q.; Ren, J.; Mao, R.; et al. The Effects of Intensive Nutrition Education on Late Middle-Aged Adults with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2016, 13, 897. [Google Scholar] [CrossRef] [PubMed]
- Muchiri, J.; Gericke, G.; Rheeder, P. Impact of nutrition education on diabetes knowledge and attitudes of adults with type 2 diabetes living in a resource-limited setting in South Africa: A randomised controlled trial. J. Endocrinol. Metab. Diabetes South Afr. 2016, 21, 26–34. [Google Scholar] [CrossRef][Green Version]
- Negarandeh, R.; Mahmoodi, H.; Noktehdan, H.; Heshmat, R.; Shakibazadeh, E. Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Prim. Care Diabetes 2013, 7, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.K.; Edwards, L.; Kissling, G.; Sanville, L. Evaluation of a Theory-based Nutrition Intervention for Older Adults with Diabetes Mellitus. J. Am. Diet. Assoc. 2002, 102, 1069–1081. [Google Scholar] [CrossRef]
- Miller, C.K.; Jensen, G.L.; Achterberg, C.L. Evaluation of a Food Label Nutrition Intervention for Women with Type 2 Diabetes Mellitus. J. Am. Diet. Assoc. 1999, 99, 323–328. [Google Scholar] [CrossRef]
- Miller, C.K.; Kristeller, J.L.; Headings, A.; Nagaraja, H. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Educ. Behav. 2014, 41, 145–154. [Google Scholar] [CrossRef]
- Pereira, D.A.; Costa, N.M.D.S.C.; Sousa, A.L.; Jardim, P.C.B.V.; Zanini, C.R.D.O. The effect of educational intervention on the disease knowledge of diabetes mellitus patients. Rev. Latino Am. Enferm. 2012, 20, 478–485. [Google Scholar] [CrossRef]
- Ward, E.V.; Berry, C.J.; Shanks, D.R.; Berry, C. Age effects on explicit and implicit memory. Front. Psychol. 2013, 4, 639. [Google Scholar] [CrossRef]
- Worsley, A. Nutrition Knowledge and Food Consumption: Can Nutrition Knowledge Change Food Behaviour? Asia Pac. J. Clin. Nutr. 2002, 11 (Suppl. 3), S579–S585. [Google Scholar] [CrossRef]
- Hemmati Maslakpak, M.; Razmara, S.; Niazkhani, Z. Effects of Face-to-Face and Telephone-Based Family-Oriented Education on Self-Care Behavior and Patient Outcomes in Type 2 Diabetes: A Randomized Controlled Trial. J. Diabetes Res. 2017, 2017, 8404328. [Google Scholar] [CrossRef] [PubMed]
- Dyson, P.A.; Beatty, S.; Matthews, D.R. An assessment of lifestyle video education for people newly diagnosed with type 2 diabetes. J. Hum. Nutr. Diet. 2010, 23, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Kandula, N.R.; Nsiah-Kumi, P.A.; Makoul, G.; Sager, J.; Zei, C.P.; Glass, S.; Stephens, Q.; Baker, D.W. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ. Couns. 2009, 75, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Moussa, M.; Sherrod, D.; Choi, J. An e-health intervention for increasing diabetes knowledge in African Americans. Int. J. Nurs. Pract. 2013, 19 (Suppl. 3), 36–43. [Google Scholar] [CrossRef] [PubMed]
- Alanzi, T.; Bah, S.; Alzahrani, S.; Alshammari, S.; Almunsef, F.; Turki, A.; Sulaiman, B.; Sara, A.; Sirah, A.; Fatima, A. Evaluation of a mobile social networking application for improving diabetes Type 2 knowledge: An intervention study using WhatsApp. J. Comp. Eff. Res. 2018, 7, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G.; Hansen, M.; Rosal, M.C.; Heyden, R.; Mejilla, R.; DePaoli, M.R.; Veerappa, C.; Wiecha, J.M. Design and Methods for a Comparative Effectiveness Pilot Study: Virtual World vs. Face-to-Face Diabetes Self-Management. JMIR Res. Protoc. 2012, 1, e24. [Google Scholar]
- Coppola, A.; Sasso, L.; Bagnasco, A.; Giustina, A.; Gazzaruso, C. The role of patient education in the prevention and management of type 2 diabetes: An overview. Endocrine 2016, 53, 18–27. [Google Scholar] [CrossRef]
- Odgers-Jewell, K.; Ball, L.E.; Kelly, J.; Isenring, E.A.; Reidlinger, D.; Thomas, R. Effectiveness of group-based self-management education for individuals with Type 2 diabetes: A systematic review with meta-analyses and meta-regression. Diabet. Med. 2017, 34, 1027–1039. [Google Scholar] [CrossRef] [PubMed]
- Steinsbekk, A.; Rygg, L.; Lisulo, M.; Rise, M.B.; Fretheim, A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv. Res. 2012, 12, 213. [Google Scholar] [CrossRef]
- Odgers-Jewell, K.; Isenring, E.A.; Thomas, R.; Reidlinger, D.P. Group participants’ experiences of a patient-directed group-based education program for the management of type 2 diabetes mellitus. PLoS ONE 2017, 12, e0177688. [Google Scholar] [CrossRef]
- Sharifirad, G.; Entezari, M.H.; Kamran, A.; Azadbakht, L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J. Res. Med. Sci. 2009, 14, 1–6. [Google Scholar] [PubMed]
- Wang, H.; Song, Z.; Ba, Y.; Zhu, L.; Wen, Y. Nutritional and eating education improves knowledge and practice of patients with type 2 diabetes concerning dietary intake and blood glucose control in an outlying city of China. Public Health Nutr. 2014, 17, 2351–2358. [Google Scholar] [CrossRef] [PubMed]
- Charlton, B.G. Lectures are such an effective teaching method because they exploit evolved human psychology to improve learning. Med. Hypotheses 2006, 67, 1261–1265. [Google Scholar] [CrossRef] [PubMed]
- Kimbler, K.J. Everyday Problem Solving and Instrumental Activities of Daily Living: Support for Domain Specificity. Behav. Sci. 2013, 3, 170–191. [Google Scholar] [CrossRef] [PubMed]
- Liebherr, M.; Schubert, P.; Schiebener, J.; Kersten, S.; Haas, C.T. Dual-tasking and aging—About multiple perspectives and possible implementations in interventions for the elderly. Cogent Psychol. 2016, 3. [Google Scholar] [CrossRef]
- Borson, S. Cognition, Aging and Disabilities: Conceptual Issues. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Bruce, D.G.; Davis, W.A.; Cull, C.A.; Davis, T.M.E. Diabetes education and knowledge in patients with type 2 diabetes from the community: The Fremantle Diabetes Study. J. Diabetes Complicat. 2003, 17, 82–89. [Google Scholar] [CrossRef]
- Brown, S.A.; Blozis, S.A.; Kouzekanani, K.; Garcia, A.A.; Winchell, M.; Hanis, C.L. Dosage Effects of Diabetes Self-Management Education for Mexican Americans: The Starr County Border Health Initiative. Diabetes Care 2005, 28, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Silverman, K.; Braunschweig, C.; Quinn, L.; Liu, Y. Feasibility of a Health Promotion Intervention for a Group of Predominantly African American Women with Type 2 Diabetes. Diabetes Educ. 2002, 28, 571–580. [Google Scholar] [CrossRef]
- Spencer, M.S.; Rosland, A.-M.; Kieffer, E.C.; Sinco, B.R.; Valerio, M.; Palmisano, G.; Anderson, M.; Guzman, J.R.; Heisler, M. Effectiveness of a Community Health Worker Intervention Among African American and Latino Adults With Type 2 Diabetes: A Randomized Controlled Trial. Am. J. Public Health 2011, 101, 2253–2260. [Google Scholar] [CrossRef]
- Rosal, M.C.; Olendzki, B.; Reed, G.W.; Ockene, I.; Gumieniak, O.; Scavron, J. Diabetes self-management among low-income spanish-speaking patients: A pilot study. Ann. Behav. Med. 2005, 29, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Vitolins, M.Z.; Rand, C.S.; Rapp, S.R.; Ribisl, P.M.; Sevick, M.A. Measuring Adherence to Behavioral and Medical Interventions. Control. Clin. Trials 2000, 21, S188–S194. [Google Scholar] [CrossRef]
- Leung, A.W.Y.; Chan, R.S.M.; Sea, M.M.M.; Woo, J. An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults. Int. J. Environ. Res. Public Health 2017, 14, 922. [Google Scholar] [CrossRef] [PubMed]
- Shawley-Brzoska, S.; Misra, R. Perceived Benefits and Barriers of a Community-Based Diabetes Prevention and Management Program. J. Clin. Med. 2018, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Rosal, M.C.; Ockene, I.S.; Restrepo, A.; White, M.J.; Borg, A.; Olendzki, B.; Scavron, J.; Candib, L.; Welch, G.; Reed, G. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: Latinos en control. Diabetes Care 2011, 34, 838–844. [Google Scholar] [CrossRef]
- Ortiz, M.; Lujan, J.; Ostwald, S.K. Promotora Diabetes Intervention for Mexican Americans. Diabetes Educ. 2007, 33, 660–670. [Google Scholar]
- Hassing, L.B.; Hofer, S.M.; Nilsson, S.E.; Berg, S.; Pedersen, N.L.; McClearn, G.; Johansson, B. Comorbid type 2 diabetes mellitus and hypertension exacerbates cognitive decline: Evidence from a longitudinal study. Age Ageing 2004, 33, 355–361. [Google Scholar] [CrossRef]
- Roberts, R.O.; Geda, Y.E.; Knopman, D.S.; Christianson, T.J.; Pankratz, V.S.; Boeve, B.F.; Vella, A.; Rocca, W.A.; Petersen, R.C. Association of duration and severity of diabetes mellitus with mild cognitive impairment. Arch Neurol. 2008, 65, 1066–1073. [Google Scholar] [CrossRef]
- Kodl, C.T.; Seaquist, E.R. Cognitive Dysfunction and Diabetes Mellitus. Endocr. Rev. 2008, 29, 494–511. [Google Scholar] [CrossRef]
- Ko, S.-H.; Park, S.-A.; Cho, J.-H.; Ko, S.-H.; Shin, K.-M.; Lee, S.-H.; Song, K.-H.; Park, Y.-M.; Ahn, Y.-B. Influence of the Duration of Diabetes on the Outcome of a Diabetes Self-Management Education Program. Diabetes Metab. J. 2012, 36, 222–229. [Google Scholar] [CrossRef]
- Vogel, S.; Schwabe, L. Learning and memory under stress: Implications for the classroom. NPJ Sci. Learn. 2016, 1, 16011. [Google Scholar] [CrossRef] [PubMed]
- Eom, Y.S.; Park, H.S.; Kim, S.-H.; Yang, S.M.; Nam, M.S.; Lee, H.W.; Lee, K.Y.; Lee, S.; Kim, Y.S.; Park, I.B. Evaluation of Stress in Korean Patients with Diabetes Mellitus Using the Problem Areas in Diabetes-Korea Questionnaire. Diabetes Metab. J. 2011, 35, 182–187. [Google Scholar] [CrossRef] [PubMed]





| Inclusion Criteria for Participation in the Study |
|---|
| Diagnosed with T2D for at least six months |
| Aged between 50 and 80 years old |
| Non-smokers |
| Not engaged in supervised exercise |
| Independent living in the community |
| Medical recommendation for lifestyle intervention |
| Known medical history |
| Diabetes comorbidities under control (diabetic foot, retinopathy, and nephropathy) |
| No cardiovascular, respiratory, and musculoskeletal contraindications to exercise |
| Without major problems in gait or balance |
| Not started insulin therapy in the past three months |
| Week | Contents |
|---|---|
| Week 1 | Diabetes, insulin, and glycaemia |
| Week 2 | Functions of nutrients |
| Week 3 | Sources of nutrients |
| Week 4 | Food Wheel (fruit, vegetables, cereals, rice, and potatoes) |
| Week 5 | Food Wheel (meat, fish and eggs, dairy products, fats, and oils) |
| Week 6 | Glycemic index and glycemic load |
| Week 7 | Added sugars |
| Week 8 | Carbohydrate counting |
| Week 9 | Food label interpretation (carbohydrates; sugars) |
| Week 10 | Food label interpretation (fats; saturated fats) |
| Week 11 | Dietetic products (lean, diet, light, zero) |
| Week 12 | Fats |
| Week 13 | Soup and salt |
| Week 14 | Drinks |
| Week 15 | Cooking methods |
| Week 16 | Meal planning and the healthy eating plate |
| Section | GNKQ | Portuguese Modified Short Version of GNKQ |
|---|---|---|
| Section 1 | Three multiple choice and one open-ended question | One multiple choice question |
| Section 2 | 21 multiple choice questions | Eight multiple choice questions |
| Section 3 | 10 multiple choice questions | No questions—lack of internal consistency and item validation |
| Section 4 | Five multiple choice and five open-ended questions | Five multiple choice and four open-ended questions |
| Characteristics | CON Group (n = 16) | EXP Group (n = 20) |
|---|---|---|
| Age, mean ± SD | 63.00 ± 5.39 | 68.25 ± 5.60 |
| Gender, n (%) | ||
| Male | 10 (62.5) | 10 (50.0) |
| Female | 6 (37.5) | 10 (50.0) |
| Education level, n (%) | ||
| ≤4 years | 9 (56.3) | 11 (55.0) |
| 5 to 9 years | 4 (25.0) | 6 (30.0) |
| >9 years | 3 (18.8) | 3 (15.0) |
| Personal monthly income, n (%) | ||
| <500 € | 3 (18.8) | 11 (55.0) |
| Between 500 and 1000 € | 7 (43.7) | 6 (30.0) |
| More than 1000 € | 6 (37.5) | 3 (15.0) |
| Marital status, n (%) | ||
| Single, divorced, or widower | 3 (18.8) | 4 (20.0) |
| Married or with domestic partner | 13 (81.2) | 16 (80.0) |
| Living situation, n (%) | ||
| Living alone | 1 (6.3) | 3 (15.0) |
| Living with others | 15 (93.7) | 17 (85.0) |
| Glycated hemoglobin, mean ± SD | 6.87 ± 1.13 | 7.18 ± 1.13 |
| Diabetes duration, mean ± SD | 7.63 ± 5.73 | 5.30 ± 4.57 |
| Mini Mental State score, mean ± SD | 26.56 ± 2.94 | 26.25 ± 2.97 |
| Nutrition-Related Knowledge (Points) | Control Group | Experimental Group | p | η2p | ||
|---|---|---|---|---|---|---|
| Baseline | 9 Months | Baseline | 9 Months | |||
| Total score | 30.2 ± 6.1 | 31.3 ± 7.4 | 29.4 ± 6.2 | 35.2 ± 5.7 | 0.001 | 0.290 |
| Dietary recommendations section | 5.0 ± 0.5 | 5.1 ± 0.6 | 4.9 ± 0.8 | 5.5 ± 0.6 | 0.053 | 0.106 |
| Sources of nutrients section | 18.8 ± 4.9 | 19.1 ± 5.5 | 17.8 ± 5.1 | 21.9 ± 4.5 | 0.004 | 0.217 |
| Diet-disease relationship section | 6.4 ± 1.5 | 7.1 ± 2.1 | 6.8 ± 1.7 | 7.9 ± 1.5 | 0.513 | 0.013 |
| Factors | β (95% CI) | p |
|---|---|---|
| Age | −0.043 (−0.355, 0.270) | 0.763 |
| Gender | 0.710 (−2.814, 4.234) | 0.659 |
| Education level | −2.819 (−6.015, 0.378) | 0.077 |
| Personal monthly income | 1.522 (−1.632, 4.677) | 0.303 |
| Marital status | 4.034 (−2.649, 10.717) | 0.205 |
| Living situation | −3.394 (−10.682, 3.895) | 0.320 |
| Glycated hemoglobin | 0.154 (−1.504, 1.811) | 0.839 |
| Diabetes duration | −0.543 (−0.977, −0.109) | 0.020 |
| Mini Mental State Examination score | −0.042 (−0.863, 0.778) | 0.910 |
| Attendance to food education program | 0.096 (0.028, 0.165) | 0.011 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasconcelos, C.; Almeida, A.; Cabral, M.; Ramos, E.; Mendes, R. The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 2403. https://doi.org/10.3390/ijerph16132403
Vasconcelos C, Almeida A, Cabral M, Ramos E, Mendes R. The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(13):2403. https://doi.org/10.3390/ijerph16132403
Chicago/Turabian StyleVasconcelos, Carlos, António Almeida, Maria Cabral, Elisabete Ramos, and Romeu Mendes. 2019. "The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 13: 2403. https://doi.org/10.3390/ijerph16132403
APA StyleVasconcelos, C., Almeida, A., Cabral, M., Ramos, E., & Mendes, R. (2019). The Impact of a Community-Based Food Education Program on Nutrition-Related Knowledge in Middle-Aged and Older Patients with Type 2 Diabetes: Results of a Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(13), 2403. https://doi.org/10.3390/ijerph16132403






