Burden of Disease Due to Traffic Noise in Germany
Abstract
:1. Introduction
2. Materials and Methods
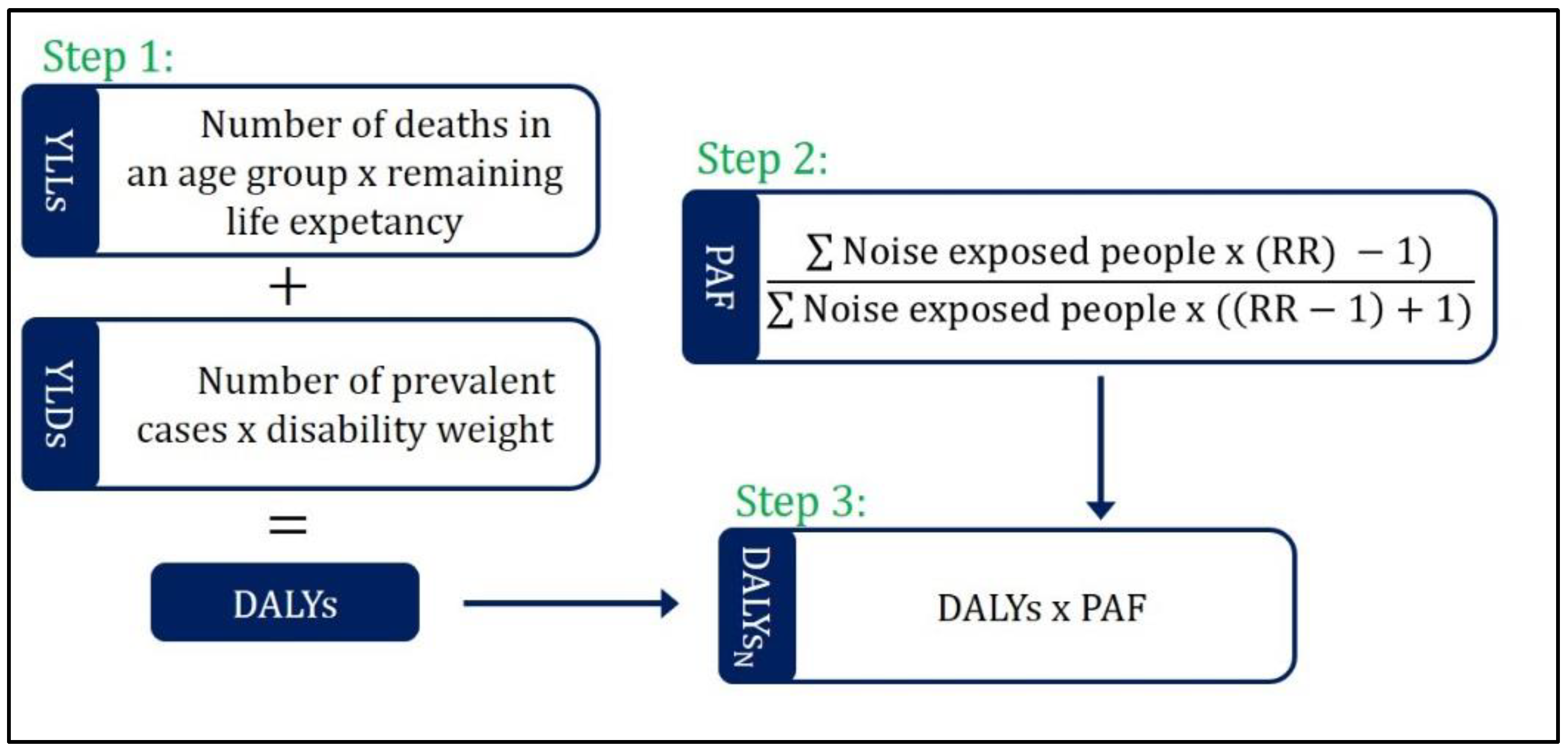
2.1. Quantification Method
2.2. Health Outcomes and Exposure-Response Functions
2.3. Estimation of the Number of Persons Exposed to Traffic Noise in Germany
2.4. Health Data and Disability Weights
2.5. Sensitivity Analysis
3. Results
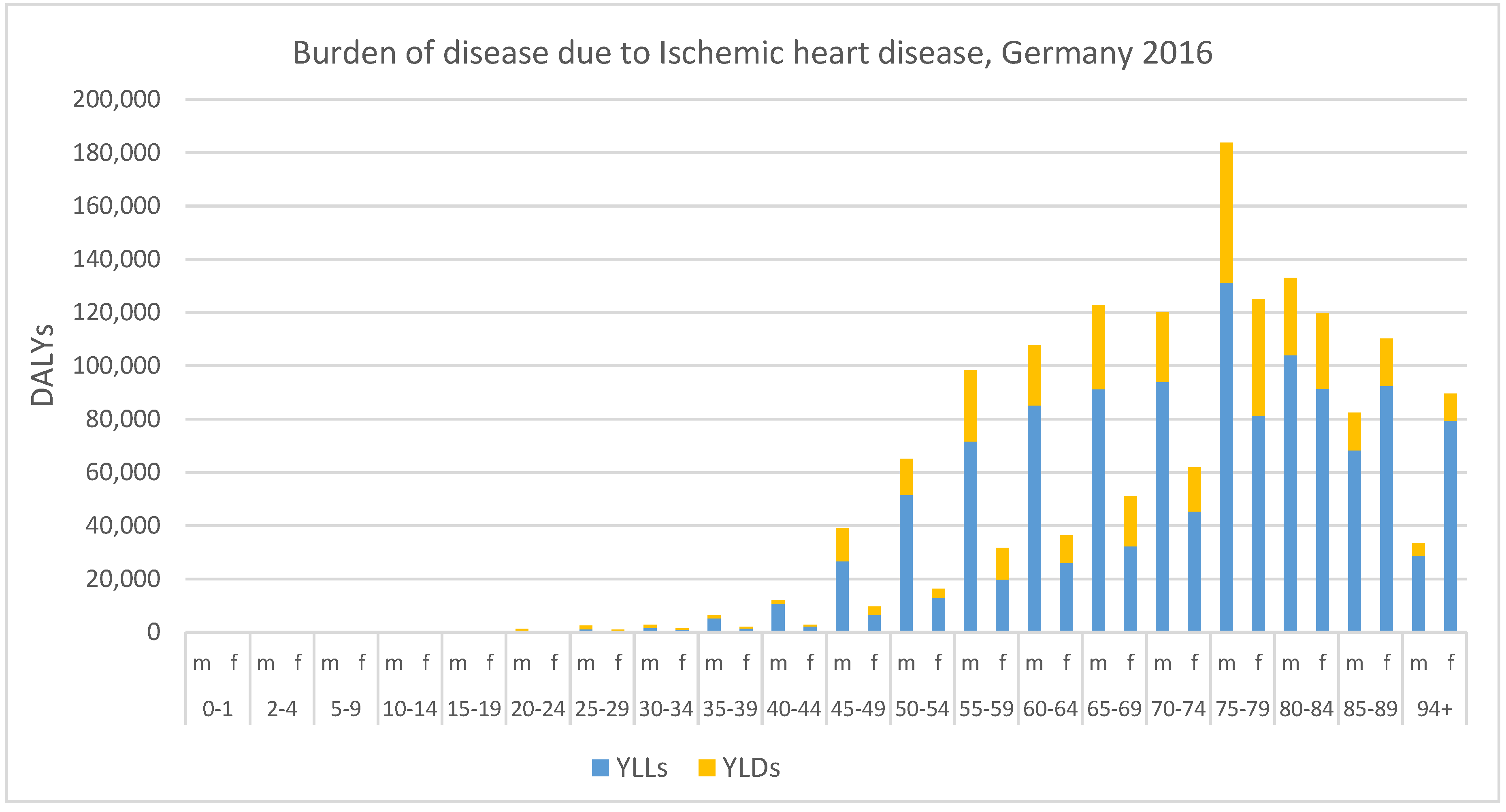
3.1. Ischemic Heart Disease
3.2. Annoyance and Sleep Disturbance
3.3. Combined Burden of the Different Health Outcomes
3.4. Sensitivity Analyses
4. Discussion
4.1. Over- and Underestimation
4.2. Comparison to Other Studies
4.3. Evidence Rating and Influence on the Results
4.4. Input Data
4.5. Necessary Assumptions to Quantify the Burden of Disease:
- People in five-decibel classes are equally distributed.
- The exposure-response functions are applicable for the population in Germany
- The prevalence rates assessed in the GEDA-study can be applied to entire population in Germany
- The mortality data are valid
- Below the counterfactual value, the risk of ischemic heart disease is one
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Basner, M.; McGuire, S. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and effects on sleep. Int. J. Environ. Res. Public Health 2018, 15, 519. [Google Scholar] [CrossRef] [PubMed]
- WHO. Environmental Noise Guidelines for the European Region; World Health Organization: Copenhagen, Denmark, 2018. [Google Scholar]
- Beutel, M.E.; Junger, C.; Klein, E.M.; Wild, P.; Lackner, K.; Blettner, M.; Binder, H.; Michal, M.; Wiltink, J.; Brahler, E.; et al. Noise annoyance is associated with depression and anxiety in the general population - the contribution of aircraft noise. PLoS ONE 2016, 11, e0155357. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, J.T.; Brauner, E.V.; Backalarz, C.; Laursen, J.E.; Pedersen, T.H.; Jensen, S.S.; Ketzel, M.; Hertel, O.; Lophaven, S.N.; Simonsen, M.K.; et al. Long-term exposure to road traffic noise and incidence of diabetes in the Danish nurse cohort. Environ. Health Perspect. 2019, 127, 57006. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, C.; Pershagen, G.; Nilsson, M. Biological Mechanisms Related to Cardiovascular and Metabolic Effects by Environmental Noise; World Health Organization: Copenhagen, Denmark, 2019. [Google Scholar]
- Brown, A.L.; van Kamp, I. WHO environmental noise guidelines for the European region: A systematic review of transport noise interventions and their impacts on health. Int. J. Environ. Res. Public Health 2017, 14, 873. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, M.J.; Ristovska, G.; Dadvand, P. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and adverse birth outcomes. Int. J. Environ. Res. Public Health 2017, 14, 1252. [Google Scholar] [CrossRef] [PubMed]
- Guski, R.; Schreckenberg, D.; Schuemer, R. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and annoyance. Int. J. Environ. Res. Public Health 2017, 14, 1539. [Google Scholar] [CrossRef] [PubMed]
- Kempen, E.V.; Casas, M.; Pershagen, G.; Foraster, M. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and cardiovascular and metabolic effects: A summary. Int. J. Environ. Res. Public Health 2018, 15, 379. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Paunovic, K. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and cognition. Int. J. Environ. Res. Public Health 2018, 15, 285. [Google Scholar] [CrossRef]
- Sliwinska-Kowalska, M.; Zaborowski, K. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and permanent hearing loss and tinnitus. Int. J. Environ. Res. Public Health 2017, 14, 1139. [Google Scholar] [CrossRef]
- Clark, C.; Paunovic, K. WHO environmental noise guidelines for the European region: A systematic review on environmental noise and quality of life, wellbeing and mental health. Int. J. Environ. Res. Public Health 2018, 15, 2400. [Google Scholar] [CrossRef]
- Murray, C.J. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull. World Health Organ. 1994, 72, 429–445. [Google Scholar] [PubMed]
- Murray, C.J.L.; Salomon, J.A.; Mathers, C.D.; Lopez, A.D. Summary Measures of Population Health: Concepts, ethics, Measurement and Applications; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Field, M.J.; Gold, M.R. Summarizing Population Health: Directions for the Development and Application of Population Metrics; National Academy of Sciences: Washington, DC, USA, 1998. [Google Scholar]
- Mathers, C.; Vos, T.; Lopez, A.; Salomon, J.; Ezzati, M. National Burden of Disease Studies: A Practical Guide; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Devleesschauwer, B.; Havelaar, A.H.; Maertens de Noordhout, C.; Haagsma, J.A.; Praet, N.; Dorny, P.; Duchateau, L.; Torgerson, P.R.; Van Oyen, H.; Speybroeck, N. DALY calculation in practice: A stepwise approach. Int. J. Public Health 2014, 59, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Salomon, J.A.; Mathers, C.D. A critical examination of summary measures of population health. In Summary Measures of Population Health; Concepts, Ethics, Measurements and Applications; Murray, C.J.L., Salomon, J.A., Mathers, C.D., Lopez, A.D., Eds.; World Health Organization: Geneva, Switzerland, 2002; pp. 13–40. [Google Scholar]
- Tobollik, M.; Terschüren, C.; Steckling, N.; McCall, T.; Hornberg, C. Disability weight—Ein umstrittenes Maß zur Bewertung von Gesundheitsbeeinträchtigungen. In Lebensqualität in der Medizin; László Kovács, R.K., Ralf, L., Eds.; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2016; pp. 237–257. [Google Scholar]
- Prüss-Üstün, A.; Mathers, C.; Campbell-Lendrum, D.; Corvalán, C.; Woodward, A. Introduction and Methods. Assessing the Environmental Burden of Disease at National and Local Levels; World Health Organization: Geneva, Switzerland, 2003; Volume 1. [Google Scholar]
- Murray, C.J.; Ezzati, M.; Lopez, A.D.; Rodgers, A.; Vander Hoorn, S. Comparative quantification of health risks: Conceptual framework and methodological issues. Popul. Health Metr. 2003, 1, 1. [Google Scholar] [CrossRef] [PubMed]
- ISO. Acoustics—Assessment of Noise Annoyance by Means of Social and Socio-Acoustic Surveys. Technical Specification 15666; ISO: Geneva, Switzerland, 2003. [Google Scholar]
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Kamp, I.V.; Schreckenberg, D.; Kempen, E.V.; Basner, M.; Clark, A.B.; Houthuijs, D.; Breugelmans, O.; Beek, A.V.; Janssen-Stelde, B. Study on Methodology to Perform an Environmental Noise and Health Assessment—A Guidance Document for Local Authorities in Europe. Rivm Report 2018-0121; National Institute for Public Health and the Environment: Bilthoven, The Netherlands, 2018. [Google Scholar]
- European Commission. Directive 2002/49/ec of the European Parliament and of the Council of 25 June 2002 relating to the assessment and management of environmental noise. Off. J. Eur. Communities L 2002, 159, 12–15. [Google Scholar]
- Thirty-Fourth Ordinance Implementing the Federal Immission Control Act (Noise Mapping Ordinance) of 6 March 2006, as Last Amended by Article 84 of the Ordinance of 31 August 2015. Federal Law Gazette I, 2015; 516.
- Directive, E.N. Commission Directive (EU) 2015/996 of 19 may 2015 establishing common noise assessment methods according to directive 2002/49/ec of the European Parliament and of the Council. Off. J. Eur. Union L 168 2015, 58. [Google Scholar]
- Announcement of the Calculation Methods for Environmental Noise in Accordance with § 5 Paragraph 1 of the Ordinance on Noise Mapping (34. Bimschv) of 20 November 2018. Federal Gazette AT 28.12.2018 B7. 2018.
- European Environment Agency. Strategic Noise Maps (df 4 and df 8) Copenhagen; European Environment Agency: Copenhagen, Denmark, 2018. [Google Scholar]
- Destatis. Bevölkerungsfortschreibung auf Grundlage des Zensus 2011; Statistisches Bundesamt: Wiesbaden, Germany, 2016.
- Destatis. Sterbetafeln. Ergebnisse aus der Laufenden Berechnung von Periodensterbetafeln für Deutschland und die Bundesländer; Statistisches Bundesamt: Wiesbaden, Germany, 2018.
- Gesundheitsberichterstattung des Bundes. Sterbefälle, Sterbeziffern (je 100.000 Einwohner, Altersstandardisiert) (ab 1998). Gliederungsmerkmale: Jahre, Region, Alter, Geschlecht, Nationalität, ICD-10, Art der Standardisierung; Robert-Koch Institut; Statistisches Bundesamt: Wiesbaden, Germany, 2017.
- Busch, M.A.; Kuhnert, R. 12-Monats-Prävalenz einer koronaren Herzkrankheit in Deutschland. J. Health Monit. 2017, 2, 62–69. [Google Scholar] [CrossRef]
- The Lancet. GBD 2017: A fragile world. Lancet 2018, 392, 1683. [Google Scholar] [CrossRef]
- Institute for Health Metrics and Evaluation. Global Burden of Disease Study 2017 (GBD 2017) Disability Weights; University of Washington: Seattle, WA, USA, 2019. [Google Scholar]
- Moran, A.E.; Forouzanfar, M.H.; Roth, G.A.; Mensah, G.A.; Ezzati, M.; Flaxman, A.; Murray, C.J.; Naghavi, M. The global burden of ischemic heart disease in 1990 and 2010: The global burden of disease 2010 study. Circulation 2014, 129, 1493–1501. [Google Scholar] [CrossRef]
- WHO Regional Office for Europe. Burden of Disease from Environmental Noise. Quantification of Healthy Life Years Lost in Europe; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2011; p. 106. [Google Scholar]
- BMUB; UBA. Umweltbewusstsein in Deutschland 2016. Ergebnisse Einer Repräsentativen Bevölkerungsumfrage; Bundesministerium für Umwelt, Naturschutz, Bau und Reaktorsicherheit, Umweltbundesamt: Berlin, Germany, 2017.
- European Communities. Position Paper on Dose Response Relationships between Transportation Noise and Annoyance; European Communities: Luxembourg, 2002. [Google Scholar]
- Miedema, H.M.E.; Passchier-Vermeer, W.; Vos, H. Elements for a Position Paper on Night-Time Transportation Noise and Sleep Disturbance; TNO (Nederlandse Organisatie voor toegepast-natuurwetenschappelijk onderzoek): Delft, The Netherlands, 2003. [Google Scholar]
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Supplemnent to global and regional burden of stroke during 1990–2010: Findings from the global burden of disease study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Myck, T.; Vorgelsang, B. Assessment of the Impact of Multiple Types of Noise Sources on Humans. In Proceedings of the INTER-NOISE 2016 45th International Congress and Exposition on Noise Control Engineering, Towards a Quieter Future, Hamburg, Germany, 21–24 August 2016. [Google Scholar]
- Seidler, A.; Hegewald, J.; Seidler, A.L.; Schubert, M.; Zeeb, H. Is the whole more than the sum of its parts? Health effects of different types of traffic noise combined. Int. J. Environ. Res. Public Health 2019, 16, 1665. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.M. A comparison of models to predict annoyance reactions to noise from mixed sources. J. Sound Vib. 1982, 81, 123–138. [Google Scholar] [CrossRef]
- Diamond, I.D.; Rice, C.G. Models of community reaction to noise from more than one source. In Environmental Annoyance: Characterization, Measurement, and Control; Koelega, H.S., Ed.; Elsevier Science Publishers: Amsterdam, The Netherlands, 1987; pp. 301–310. [Google Scholar]
- Rice, C.G.; Izumi, K. Factors affecting the annoyance of combinations of noise sources. Proc. Inst. Acoust 1986, 8, 325–332. [Google Scholar]
- Miedema, H.M. Relationship between exposure to multiple noise sources and noise annoyance. J. Acoust. Soc. Am. 2004, 116, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Wothge, J.; Belke, C.; Mohler, U.; Guski, R.; Schreckenberg, D. The combined effects of aircraft and road traffic noise and aircraft and railway noise on noise annoyance-an analysis in the context of the joint research initiative NORAH. Int. J. Environ. Res. Public Health 2017, 14, 871. [Google Scholar] [CrossRef] [PubMed]
- Öhrstrom, E.; Barregard, L.; Andersson, E.; Skanberg, A.; Svensson, H.; Angerheim, P. Annoyance due to single and combined sound exposure from railway and road traffic. J. Acoust. Soc. Am. 2007, 122, 2642–2652. [Google Scholar] [CrossRef] [PubMed]
- Pierrette, M.; Marquis-Favre, C.; Morel, J.; Rioux, L.; Vallet, M.; Viollon, S.; Moch, A. Noise annoyance from industrial and road traffic combined noises: A survey and a total annoyance model comparison. J. Environ. Psychol. 2012, 32, 178–186. [Google Scholar] [CrossRef]
- Matheson, M.; Clark, C.; Martin, R.; van Kempen, E.; Haines, M.; Barrio, I.L.; Hygge, S.; Stansfeld, S. The effects of road traffic and aircraft noise exposure on children's episodic memory: The RANCH project. Noise Health 2010, 12, 244–254. [Google Scholar]
- Guski, R.; Schreckenberg, D. Norah Noise-Related Annoyance, Cognition, and Health: Verkehrslärmwirkungen im Flughafenumfeld: Gesamtbetrachtung des Forschungsprojekts; Gemeinnützige Umwelthaus GmbH: Kelsterbach, Germany, 2015. [Google Scholar]
- Eriksson, C.; Hilding, A.; Pyko, A.; Bluhm, G.; Pershagen, G.; Ostenson, C.G. Long-term aircraft noise exposure and body mass index, waist circumference, and type 2 diabetes: A prospective study. Environ. Health Perspect. 2014, 122, 687–694. [Google Scholar] [CrossRef]
- Babisch, W.; Kim, R. Environmental noise and cardiovascular disease. In Burden of Disease from Environmental Noise. Quantification of Healthy Life Years Lost in Europe; World Health Organization Regional office for Europe, Ed.; World Health Organization: Copenhagen, Denmark, 2011; pp. 15–42. [Google Scholar]
- Hornberg, C.; Claßen, T.; Steckling, N.; Samson, R.; McCall, T.; Tobollik, M.; Mekel, O.; Terschüren, C.; Schillmöller, Z.; Popp, J.; et al. Quantifizierung der Auswirkungen Verschiedener Umweltbelastungen Auf Die Gesundheit der Menschen in Deutschland unter Berücksichtigung der Bevölkerungsbezogenen Expositionsermittlung (Verteilungsbasierte Analyse Gesundheitlicher Auswirkungen von Umwelt-Stressoren, Vegas); Umweltbundesamt: Dessau-Roßlau, Germany, 2013.
- Hänninen, O.; Knol, A.B.; Jantunen, M.; Lim, T.A.; Conrad, A.; Rappolder, M.; Carrer, P.; Fanetti, A.C.; Kim, R.; Buekers, J.; et al. Environmental burden of disease in Europe: Assessing nine risk factors in six countries. Environ. Health Perspect. 2014, 122, 439–446. [Google Scholar] [CrossRef]
- Vienneau, D.; Schindler, C.; Perez, L.; Probst-Hensch, N.; Roosli, M. The relationship between transportation noise exposure and ischemic heart disease: A meta-analysis. Environ. Res. 2015, 138, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Wagner, M.; Schubert, M.; Dröge, P.; Hegewald, J. Sekundärdatenbasierte Fallkontrollstudie mit Vertiefender Befragung; Gemeinnützige Umwelthaus gGmbH: Kelsterbach, Germany, 2015. [Google Scholar]
- Houthuijs, D.; Fons, J.; Maza, M.S.D.L.; Swart, W.; Beek, A.V. Method to Estimate the Road Traffic Noise Exposure Distribution in Europe, ETC/ACM Technical Paper 2017/10; European Topic Centre on Air Pollution and Climate Change Mitigation: Bilthoven, The Netherlands, 2018. [Google Scholar]
- Heritier, H.; Vienneau, D.; Foraster, M.; Eze, I.C.; Schaffner, E.; de Hoogh, K.; Thiesse, L.; Rudzik, F.; Habermacher, M.; Kopfli, M.; et al. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: A nationwide cohort study in Switzerland. Eur. Heart J. 2019, 40, 598–603. [Google Scholar] [CrossRef] [PubMed]
| Health Outcomes | Evidence Quality Assessment for | Source | ||
|---|---|---|---|---|
| Road Traffic Noise | Aircraft Noise | Railway Noise | ||
| IHD morbidity | •• | • | • | [9] |
| IHD mortality | ••• | •• | * | [9] |
| Annoyance | •• | ••• | ••• | [8] |
| Sleep disturbance | ••• | ••• | ••• | [1] |
| Health Outcomes | Exposure-Response Functions for | Source | ||
|---|---|---|---|---|
| Road Traffic Noise | Aircraft Noise | Railway Noise | ||
| IHD morbidity | 1.24 (95% CI: 1.08–1.42) ** | 1.07 (95% CI: 0.94–1.23) ** | 1.18 (95% CI: 0.82–1.68) ** | [9] |
| IHD mortality | 1.05 (95% CI: 0.97–1.13) ** | 1.04 (95% CI: 0.98–1.11) ** | -* | [9] |
| Annoyance | 78.9270 − 3.1162 × Lden + 0.034 × Lden2 | −50.9693 + 1.0168 × Lden + 0.0072 × Lden2 | 38.1596 − 2.05538 × Lden + 0.0285 × Lden2 | [8] |
| Sleep disturbance | 19.4312 − 0.9336 × Lnight + 0.0126 × Lnight2 | 16.7885 − 0.9293 × Lnight + 0.0198 × Lnight2 | 67.5406 − 3.1852 × Lnight + 0.0391 × Lnight 2 | [1] |
| Lden/Lnight in dB | Number of People Exposed to | |||||
|---|---|---|---|---|---|---|
| Road Traffic Noise | Aircraft Noise | Railway Noise | ||||
| Lden | Lnight | Lden | Lnight | Lden | Lnight | |
| >50–55 | 2,835,300 | 206,800 | 3,144,400 | |||
| >55–60 | 3,822,500 | 1,772,300 | 606,400 | 34,700 | 3,782,700 | 1,310,700 |
| >60–65 | 2,349,000 | 726,400 | 205,800 | 1500 | 1,639,300 | 483,600 |
| >65–70 | 1,603,200 | 97,000 | 30,700 | 679,900 | 154,700 | |
| >70–75 | 600,300 | 6800 * | 3700 | 230,700 | 62,200 * | |
| >75 | 60,100 | 92,500 | ||||
| Health Outcomes | Health Data | Reference Year | Source | DW | Source |
|---|---|---|---|---|---|
| IHD morbidity | GEDA-study | 2014/2015 | [33] | 0.114 | * |
| IHD mortality | Cause of death register | 2016 | [32] | - | - |
| Annoyance | - | 0.02 | [2] | ||
| Sleep disturbance | - | 0.07 | [2] |
| Scenario | Road Traffic Noise | Aircraft Noise | Railway Noise | Source |
|---|---|---|---|---|
| S 1: Exposure data | %HA (23% males, 23% females) | %HA (10% males, 8% females) | %HA (7% males, 6% females) | [38] |
| S 2–3: Exposure-response function | %SD (20.8 − 1.05 × (Lnight) + 0.01486 × (Lnight)2) %HA (9.868 × 10−4 × (Lden-42)3 − 1.436 × 10−2 × (Lden-42)2 + 0.5118(Lden-42)) | %SD (18.147 − 0.956 × (Lnight) + 0.01482 × (Lnight)2) %HA (−9.199 × 10−5 × (Lden-42)3 + 3.932 × 10−2 × (Lden-42)2 + 0.2939 (Lden-42)) | %SD (11.3 − 0.55 × (Lnight) + 0.00759 × Lnight)2) %HA (7.239 × 10−4 × (Lden-42)3 − 7.851 × 10−3 × (Lden-42)2 + 0.1695 (Lden-42)) | [37,39,40] |
| S 4–9: Disability weight | IHD (0.266) %HA (0.01–0.12, 0.01) %SD (0.04–0.10, 0.0175) | [24,35,37,41] | ||
| S 10: Counterfactual value for IHD | 53 dB Lden | 53 dB Lden | 53 dB Lden | [24] |
| Health Outcomes | Road Traffic Noise | Aircraft Noise | Railway Noise | |||
|---|---|---|---|---|---|---|
| PAF | Life Years Lost | PAF | Life Years Lost | PAF | Life Years Lost | |
| Morbidity | 1.83% (0.65–2.93%) | 7452 (2706–11,905) YLDs | 0.08% (0.00–0.24%) | 327 (0–976) YLDs | 0.92% (0.00–2.8%) | 3738 (0–11,402) YLDs |
| Mortality | 0.42% (0.00–1.05%) | 5345 (0–13,299) YLLs | 0.05% (0.00–0.12%) | 591 (0–1557) YLLs | – | – |
| Sum | 12.797 (2706–25,204) DALYs | 918 (0–2533) DALYs | 3.738 (0–11.402) DALYs | |||
| Per 100,000 * | 15.54 (3.29–30.61) DALYs | 1.11 (0–3.08) DALYs | 4.54 (0–13.85) DALYs | |||
| Lden in dB | Road Traffic Noise | Aircraft Noise | Railway Noise | ||||||
|---|---|---|---|---|---|---|---|---|---|
| in % | # | YLDs | in % | # | YLDs | in % | # | YLDs | |
| >55–60 | 12.4 | 474,732 | 9495 | 30.4 | 184,231 | 3685 | 13.6 | 514,426 | 10,289 |
| >60–65 | 17.2 | 403,732 | 8075 | 39.8 | 81,804 | 1636 | 20.3 | 332,451 | 6649 |
| >65–70 | 23.7 | 379,404 | 7588 | 49.5 | 15,189 | 304 | 28.4 | 192,994 | 3860 |
| >70–75 | 31.9 | 191,216 | 3824 | 59.6 | 2204 | 44 | 37.9 | 87,473 | 1749 |
| >75 | 37.6 | 22,590 | 452 | 65.8 | 0 | 0 | 44.3 | 40,995 | 820 |
| Sum | 1,471,673 | 29,433 | 283,236 | 5669 | 1,168,338 | 23,367 | |||
| Per 100,000 * | 349 | 670 | 364 | ||||||
| Lnight in dB | Road Traffic Noise | Aircraft Noise | Railway Noise | ||||||
|---|---|---|---|---|---|---|---|---|---|
| in % | # | YLDs | in % | # | YLDs | in % | # | YLDs | |
| >50–55 | 5.0 | 140,472 | 9833 | 22.0 | 45,504 | 3185 | 7.6 | 240,125 | 16,809 |
| >55–60 | 7.2 | 126,780 | 8875 | 28.2 | 9768 | 684 | 13.0 | 170,654 | 11,946 |
| >60–65 | 10.0 | 72,512 | 5076 | 35.3 | 529 | 37 | 20.3 | 98,454 | 6892 |
| >65–70 | 12.0 | 11,623 | 814 | 40.0 | 0 | 0 | 25.7 | 39,758 | 2783 |
| >70 | 12.0 | 815 | 57 | 40.0 | 0 | 0 | 25.7 | 15,985 | 1119 |
| Sum | 352,201 | 24,654 | 55,801 | 3906 | 564,977 | 39,548 | |||
| Per 100,000 * | 454 | 1607 | 767 | ||||||
| Health Outcomes | Road Traffic Noise | Aircraft Noise | Railway Noise |
|---|---|---|---|
| IHD morbidity | 7452 | 327 | 3.738 |
| Evidence | •• | • | • |
| IHD mortality | 5345 | 591 | * |
| Evidence | ••• | •• | * |
| Annoyance | 29,433 | 5669 | 23,367 |
| Evidence | •• | ••• | ••• |
| Sleep disturbance | 24,654 | 3906 | 39,548 |
| Evidence | ••• | ••• | ••• |
| Sum (moderate evidence) | 29,999 | 9575 | 62,915 |
| Sum (low quality and better) | 66,884 | 10,166 | 62,915 |
| Sum (all) | 66,884 | 10,493 | 66,653 |
| Scenarios | Road Traffic Noise | Aircraft Noise | Railway Noise |
|---|---|---|---|
| Main analysis YLDs | 71,558 | 31,773 | 45,987 |
| (25,954–114,473) YLDs | (0–94,953) YLDs | (0–141,591) YLDs | |
| Main analysis YLLs | 51,242 | 57,462 | - |
| (0–127,595) YLLs | (0–151,475) YLLs | ||
| Main analysis DALYs | 122,800 | 89,236 | 45,987 |
| (25,954–242,068) DALYs | (0–246,429) DALYs | (0–141,591) DALYs | |
| S4: DW | 166,969 | 74,138 | 107,303 |
| (60,559–267,104) YLDs | (0–221,558) YLDs | (0–330,380) YLDs | |
| Difference in YLDs | +95,411 | +42,365 | +61,316 |
| (34,605–152,631) YLDs | (0–126,605) YLDs | (0–188.789) YLDs | |
| S10: counterfactual value 53 dB | 122,800 | 43,829 | 45,987 |
| (25,954–242,068) DALYs | (0–124,342) DALYs | (0–141,591) DALYs | |
| Difference in DALYs | 0 | −45,407 | 0 |
| (0–122,087) DALYs |
| Scenarios | Road Traffic Noise | Aircraft Noise | Railway Noise | ||||||
|---|---|---|---|---|---|---|---|---|---|
| in % | # | YLDs | in % | # | YLDs | in % | # | YLDs | |
| Main analysis | 17 | 1,471,673 | 29,433 | 33 | 283,428 | 5669 | 18 | 1,168,338 | 23,367 |
| S1a: exposure m | 23 | 8,042,860 | 160,857 | 10 | 3,496,896 | 69,938 | 7 | 2,447,827 | 48,957 |
| S1b: exposure f | 23 | 8,375,424 | 167,508 | 8 | 2,913,191 | 58,264 | 6 | 2,184,893 | 43,698 |
| S1: exposure sum | 16,418,284 | 328,366 | 6,410,087 | 128,202 | 4,632,720 | 92,654 | |||
| Difference | +14,949,611 | +298,932 | +6126,659 | +122,533 | +3,464,382 | +69,288 | |||
| S3: ERF | 13 | 1,093,241 | 21,865 | 16 | 132,352 | 2647 | 6 | 355,001 | 7100 |
| Difference | −378,432 | −7569 | −151,076 | −3022 | −813,337 | −16,267 | |||
| S5: DW low | 14,717 | 2834 | 11,683 | ||||||
| Difference | −14,717 | −2834 | −11,683 | ||||||
| S6: DW high | 176,601 | 34,011 | 140,201 | ||||||
| Difference | +147,167 | +28,343 | +116,834 | ||||||
| Scenarios | Road Traffic Noise | Aircraft Noise | Railway Noise | ||||||
|---|---|---|---|---|---|---|---|---|---|
| in % | # | YLDs | in % | # | YLDs | in % | # | YLDs | |
| Main analysis | 6 | 352,201 | 24,654 | 23 | 55,801 | 3906 | 11 | 564,977 | 39,548 |
| S2: ERF | 8 | 453,573 | 31,750 | 9 | 21,929 | 1535 | 4 | 209,134 | 14,639 |
| Difference | +101,371 | +7096 | −33,872 | −2371 | −355,843 | −24,909 | |||
| S7: DW low | 14,088 | 2232 | 22,599 | ||||||
| Difference | −10,566 | −1674 | −16,949 | ||||||
| S8: DW high | 35,220 | 5580 | 56,498 | ||||||
| Difference | +10,566 | +1674 | +16,949 | ||||||
| S9: DW alternative | 6164 | 977 | 9887 | ||||||
| Difference | −18,490 | −2929 | −29,661 | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobollik, M.; Hintzsche, M.; Wothge, J.; Myck, T.; Plass, D. Burden of Disease Due to Traffic Noise in Germany. Int. J. Environ. Res. Public Health 2019, 16, 2304. https://doi.org/10.3390/ijerph16132304
Tobollik M, Hintzsche M, Wothge J, Myck T, Plass D. Burden of Disease Due to Traffic Noise in Germany. International Journal of Environmental Research and Public Health. 2019; 16(13):2304. https://doi.org/10.3390/ijerph16132304
Chicago/Turabian StyleTobollik, Myriam, Matthias Hintzsche, Jördis Wothge, Thomas Myck, and Dietrich Plass. 2019. "Burden of Disease Due to Traffic Noise in Germany" International Journal of Environmental Research and Public Health 16, no. 13: 2304. https://doi.org/10.3390/ijerph16132304
APA StyleTobollik, M., Hintzsche, M., Wothge, J., Myck, T., & Plass, D. (2019). Burden of Disease Due to Traffic Noise in Germany. International Journal of Environmental Research and Public Health, 16(13), 2304. https://doi.org/10.3390/ijerph16132304




