The Functional and Morphological Changes of the Cervical Intervertebral Disc after Applying Lordotic Curve Controlled Traction: A Double-Blind Randomized Controlled Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Sample
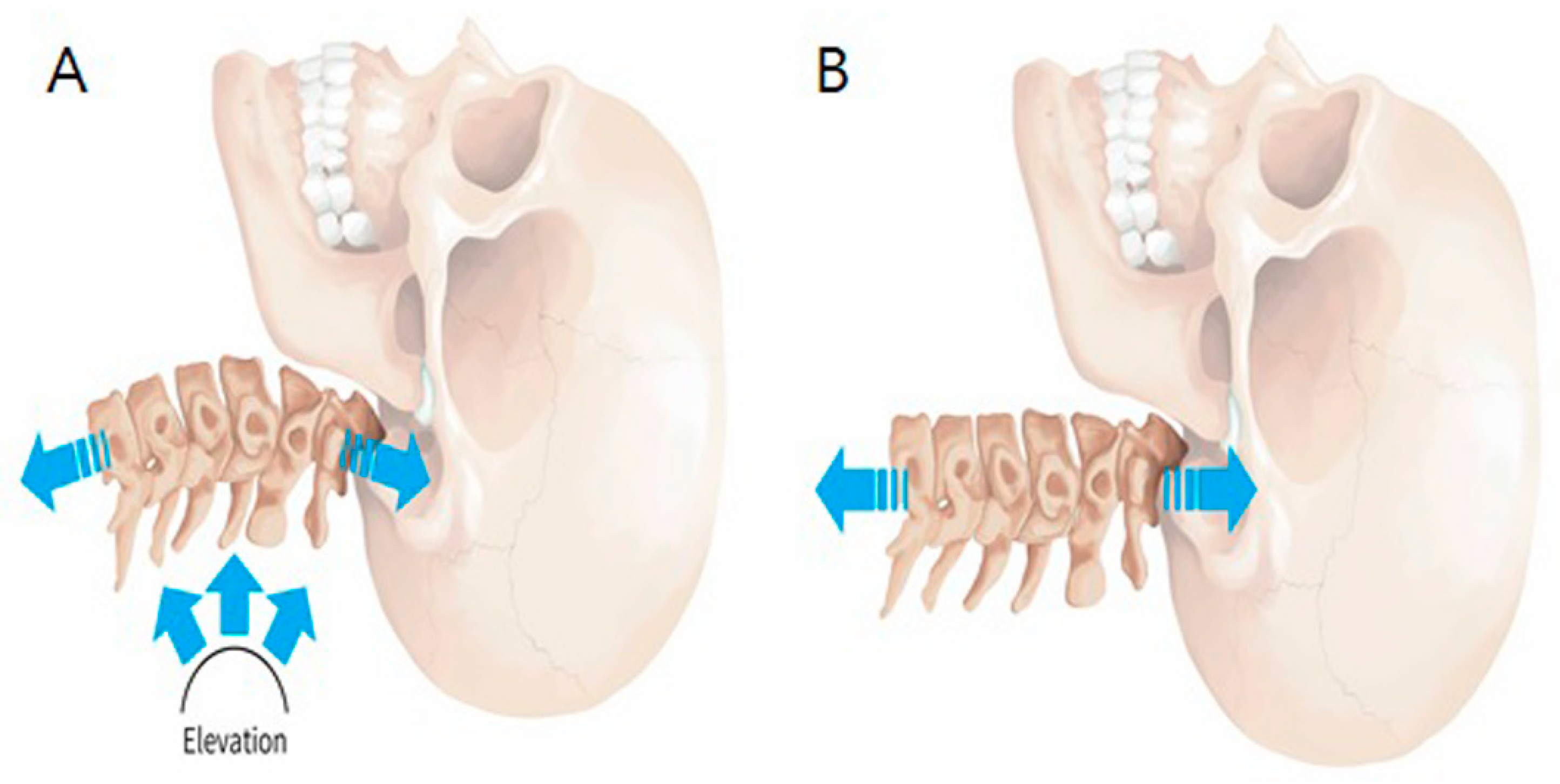
2.2. C-LCCT Versus TT
2.3. Outcome Measurement Using Pain and Functional Status
2.4. Morphological Changes in Cervical Disc Severity
2.4.1. Cervical Lordotic Curve
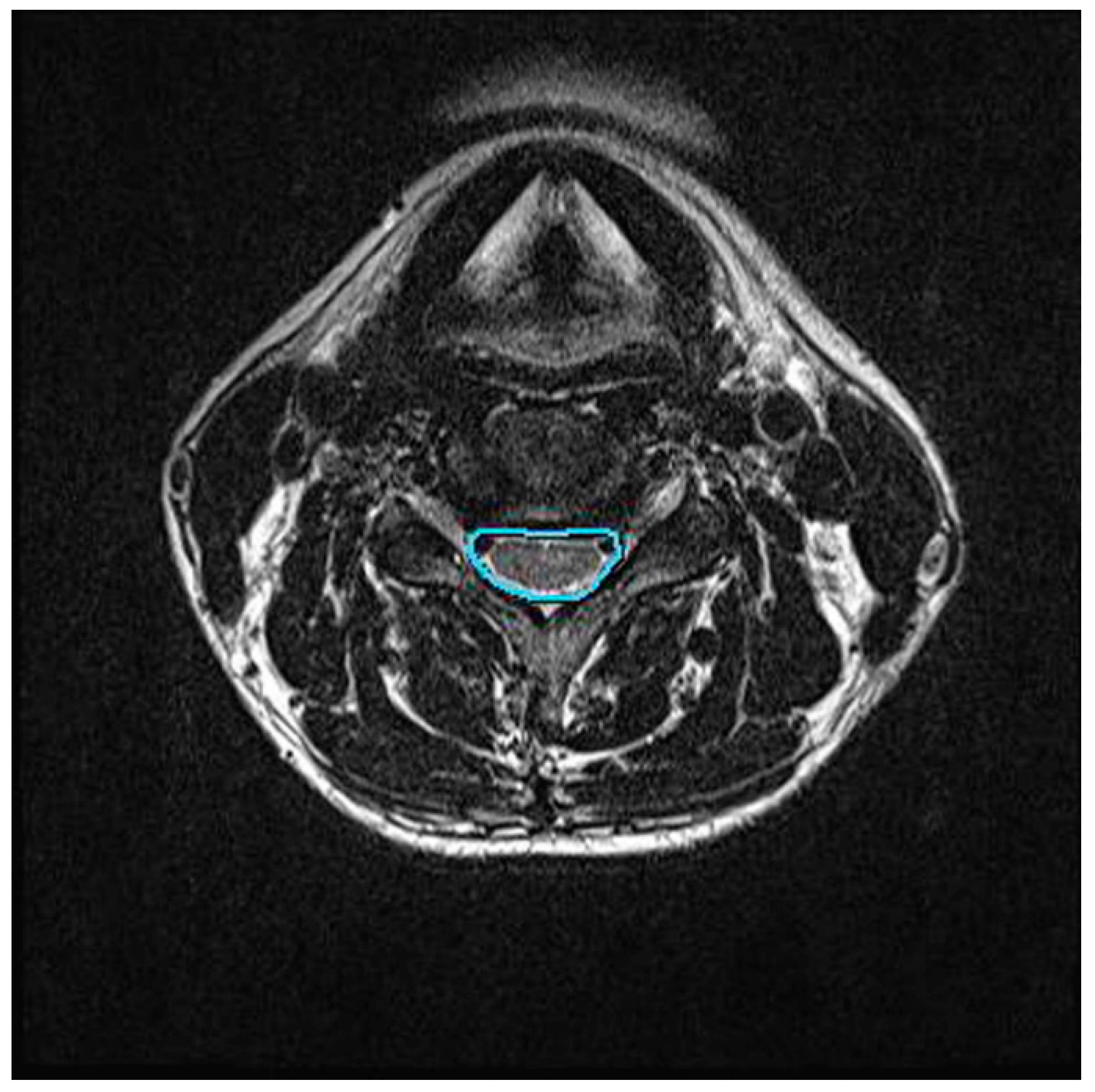
2.4.2. Central Canal Area Assessment
2.5. Statistical Analysis: Sample Size Determination
3. Results
3.1. Pain and Functional Status Measurement
3.2. Morphological Change Measurement: Cobb Angle and Central Canal Aarea
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dedering, A.; Halvorsen, M.; Cleland, J.; Svensson, M.; Peolsson, A. Neck-specific training with a cognitive behavioural approach compared with prescribed physical activity in patients with cervical radiculopathy: A protocol of a prospective randomised clinical trial. BMC Musculoskelet. Disord. 2014, 15, 274. [Google Scholar] [CrossRef] [PubMed]
- Bagheripour, B.; Kamyab, M.; Azadinia, F.; Amiri, A.; Akbari, M. The efficacy of a home-mechanical traction unit for patients with mild to moderate cervical osteoarthrosis: A pilot study. Med. J. Islam. Repub. Iran 2016, 30, 386. [Google Scholar] [PubMed]
- Tadano, S.; Tanabe, H.; Arai, S.; Fujino, K.; Doi, T.; Akai, M. Lumbar mechanical traction: A biomechanical assessment of change at the lumbar spine. BMC Musculoskelet. Disord. 2019, 20, 155. [Google Scholar] [CrossRef] [PubMed]
- Madson, T.J.; Hollman, J.H. Cervical Traction for Managing Neck Pain: A Survey of Physical Therapists in the United States. J. Orthop. Sports Phys. Ther. 2017, 47, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Diab, A.A.M.; Moustafa, I.M. The efficacy of lumbar extension traction for sagittal alignment in mechanical low back pain: A randomized trial. J. Back Musculoskelet. Rehabil. 2013, 26, 213–220. [Google Scholar] [CrossRef]
- Chung, C.-T.; Tsai, S.-W.; Chen, C.-J.; Wu, T.-C.; Wang, D.; Lan, H.-C.H.; Wu, S.-K. Comparison of the intervertebral disc spaces between axial and anterior lean cervical traction. Eur. Spine J. 2009, 18, 1669–1676. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Choi, J.; Lee, S.; Jeon, C. Effects of flexion-distraction manipulation therapy on pain and disability in patients with lumbar spinal stenosis. J. Phys. Ther. Sci. 2015, 27, 1937–1939. [Google Scholar] [CrossRef] [PubMed]
- Ishida, T.; Tanaka, S.; Sekiguchi, T.; Sugiyama, D.; Kawamata, M. Spinal nociceptive transmission by mechanical stimulation of bone marrow. Mol. Pain 2016, 12, 12. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.R. Cervical Traction: Review of Literature and Treatment Guidelines. Phys. Ther. 1977, 57, 910–914. [Google Scholar] [CrossRef]
- Shahar, D.; Sayers, M.G.L. Changes in the sagittal cranio-cervical posture following a 12-week intervention using a simple spinal traction device. Spine 2019, 44, 447–453. [Google Scholar] [CrossRef]
- Li, Y.; Liu, X.; Han, J.; Zhang, J.; Zhang, L.; Yu, H. Clinical efficacy of glucosamine hydrochloride tablets in the treatment of cervical spondylosis. Pak. J. Pharm. Sci. 2018, 31, 1617–1621. [Google Scholar] [PubMed]
- Ojoawo, A.O.; Olabode, A.D. Comparative effectiveness of transverse oscillatory pressure and cervical traction in the management of cervical radiculopathy: A randomized controlled study. Hong Kong Physiother. J. 2018, 38, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Mo, Z.; Li, D.; Zhang, R.; Chang, M.; Yang, B.; Tang, S. Comparisons of the effectiveness and safety of tuina, acupuncture, traction, and Chinese herbs for lumbar disc herniation: A systematic review and network meta-analysis. Evid. Based Complement. Alternat. Med. 2019, 2019, 6821310. [Google Scholar] [CrossRef] [PubMed]
- Thackeray, A.; Fritz, J.M.; Childs, J.D.; Brennan, G.P. The effectiveness of mechanical traction among subgroups of patients with low back pain and leg pain: A randomized trial. J. Orthop. Sports Phys. Ther. 2016, 46, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Harte, A.A.; Baxter, G.D.; Gracey, J.H. The effectiveness of motorised lumbar traction in the management of LBP with lumbo sacral nerve root involvement: A feasibility study. BMC Musculoskelet. Disord. 2007, 8, 118. [Google Scholar] [CrossRef] [PubMed]
- Haher, T.R.; O’brien, M.; Dryer, J.W.; Nucci, R.; Zipnick, R.; Leone, D.J. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine 1994, 19, 2667–2670; discussion 2671. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169. [Google Scholar] [CrossRef] [PubMed]
- Roland, M.; Fairbank, J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Scrimshaw, S.V.; Maher, C. Responsiveness of visual analogue and McGill pain scale measures. J. Manip. Physiol. Ther. 2001, 24, 501–504. [Google Scholar] [CrossRef]
- Chung, T.S.; Yang, H.E.; Ahn, S.J.; Park, J.H. Herniated lumbar disks: Real-time MR imaging evaluation during continuous traction. Radiology 2015, 275, 755–762. [Google Scholar] [CrossRef]
- Choi, J.; Lee, S.; Hwangbo, G. Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J. Phys. Ther. Sci. 2015, 27, 481–483. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Romeo, A.; Vanti, C.; Boldrini, V.; Ruggeri, M.; Guccione, A.A.; Pillastrini, P.; Bertozzi, L. Cervical radiculopathy: Effectiveness of adding traction to physical therapy-a systematic review and meta-analysis of randomized controlled trials. Phys. Ther. 2018, 98, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Ming, G.; Ng, L.Y. Development of a clinical prediction rule to identify patients with neck pain who are likely to benefit from home-based mechanical cervical traction. Eur. Spine J. 2011, 20, 912–922. [Google Scholar] [CrossRef] [PubMed]

| Variables | All (n = 40) | C-LCCT (n = 20) | TT (n = 20) | p Value |
|---|---|---|---|---|
| Age (years) | 46 ± 14.6 | 48.8 ± 13.3 | 43.2 ± 16.2 | 0.684 |
| Height (cm) | 165.0 ± 8.2 | 163.6 ± 7.5 | 167.6 ± 9.2 | 0.628 |
| Weight (kg) | 63.3 ± 11.4 | 62.4 ± 11.2 | 64.9 ± 12.0 | 0.713 |
| BMI | 23.1 ± 3.2 | 23.2 ± 3.4 | 23.0 ± 3.0 | 0.669 |
| Duration of cervical pain (mean, months) | 15.5 ± 13.4 | 16.5 ± 12.8 | 13.5 ± 15.1 | 0.541 |
| Initial VAS | 6.7 ± 0.4 | 6.8 ± 0.8 | 7.0 ± 0.0 | 0.852 |
| Initial ODI (%) | 29.2±10.2 | 29.9 ± 15.7 | 28.5 ± 4.6 | 0.788 |
| Variables | Before Treatment | After Treatment | p Value |
|---|---|---|---|
| A. C-LCCT group | |||
| VAS | 6.78 ± 0.8 | 3.33 ± 0.8 | <0.001 * |
| ODI (%) | 29.85 ± 15.6 | 20.15 ± 11.8 | 0.003 * |
| B. TT group | |||
| VAS | 7.0 ± 0.0 | 4.27 ± 0.9 | 0.006 * |
| ODI (%) | 28.48 ± 4.6 | 26.87 ± 11.1 | 0.470 |
| Variables | Before Treatment | After Treatment | p Value |
|---|---|---|---|
| A. C-LCCT group | |||
| Cobb angle at C2–7 (°) | 4.8 ± 10.9 | 16.9 ± 12.7 | <0.001 * |
| Central canal area (mm2) | 130.9 ± 40.5 | 136.0 ± 43.2 | <0.001 * |
| B. TT group | |||
| Cobb angle at C2–7 (°) | 5.2 ± 8.6 | 4.9 ± 9.8 | 0.781 |
| Central canal area (mm2) | 137.9 ± 37.6 | 136.7 ± 41.4 | 0.549 |
| Variables | C-LCCT | TT | T | p Value |
|---|---|---|---|---|
| VAS | −2.7 ± 1.5 | −2.7 ± 1.0 | −1.6 | >0.05 |
| ODI (%) | −9.7 ± 9.8 | −1.6 ± 7.1 | −2.3 | <0.05 * |
| Cobb angle | 10.1 ± 4.5 | −0.3 ± 5.3 | 7.6 | <0.001 * |
| Central canal area (mm2) | 5.1 ± 5.3 | −2.5 ± 5.8 | 3.7 | <0.001 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-H.; Heo, S.J.; Park, S.H.; Jeong, H.S.; Kim, S.-Y. The Functional and Morphological Changes of the Cervical Intervertebral Disc after Applying Lordotic Curve Controlled Traction: A Double-Blind Randomized Controlled Study. Int. J. Environ. Res. Public Health 2019, 16, 2162. https://doi.org/10.3390/ijerph16122162
Lee C-H, Heo SJ, Park SH, Jeong HS, Kim S-Y. The Functional and Morphological Changes of the Cervical Intervertebral Disc after Applying Lordotic Curve Controlled Traction: A Double-Blind Randomized Controlled Study. International Journal of Environmental Research and Public Health. 2019; 16(12):2162. https://doi.org/10.3390/ijerph16122162
Chicago/Turabian StyleLee, Chang-Hyung, Sung Jin Heo, So Hyun Park, Hee Seok Jeong, and Soo-Yeon Kim. 2019. "The Functional and Morphological Changes of the Cervical Intervertebral Disc after Applying Lordotic Curve Controlled Traction: A Double-Blind Randomized Controlled Study" International Journal of Environmental Research and Public Health 16, no. 12: 2162. https://doi.org/10.3390/ijerph16122162
APA StyleLee, C.-H., Heo, S. J., Park, S. H., Jeong, H. S., & Kim, S.-Y. (2019). The Functional and Morphological Changes of the Cervical Intervertebral Disc after Applying Lordotic Curve Controlled Traction: A Double-Blind Randomized Controlled Study. International Journal of Environmental Research and Public Health, 16(12), 2162. https://doi.org/10.3390/ijerph16122162





