International Comparison of the Levels and Potential Correlates of Objectively Measured Sedentary Time and Physical Activity among Three-to-Four-Year-Old Children
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Physical Activity Measurement
2.4. Variables
2.5. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. Percentage of Children Meeting Canadian, Australian, USA and UK Guidelines for Sedentary Time, Total Physical Activity, and Moderate-to-Vigorous Physical Activity
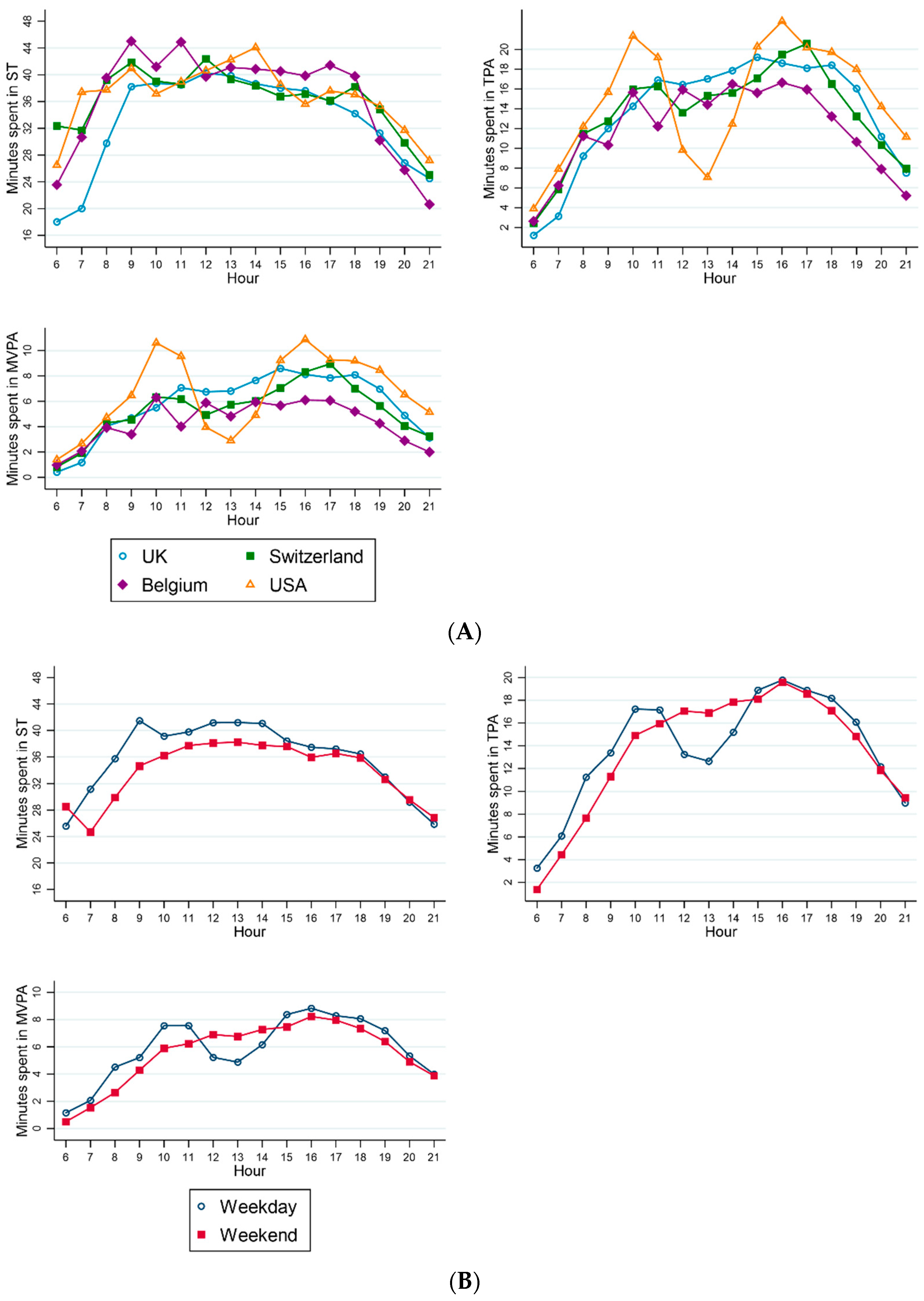
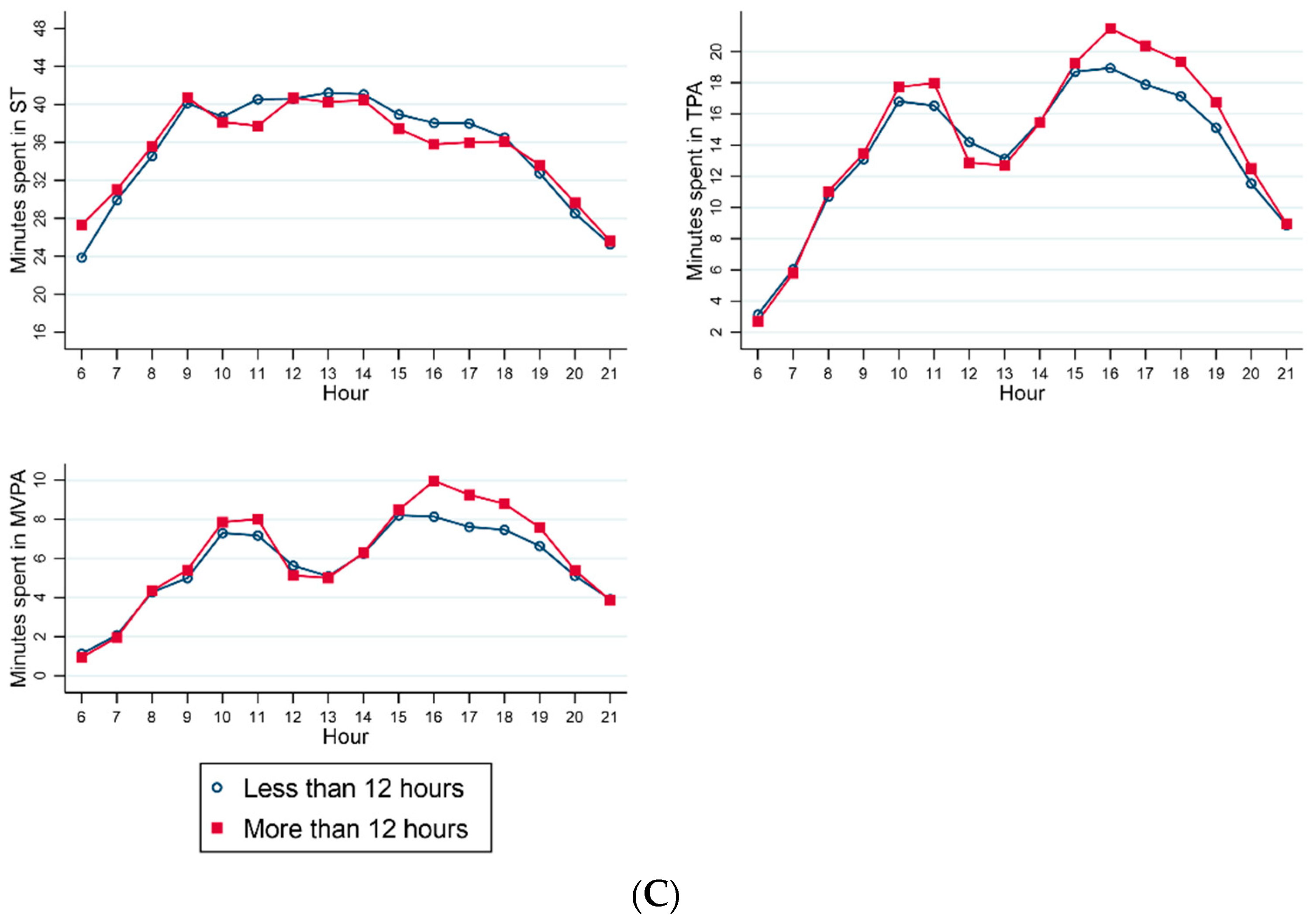
3.3. Patterns of Sedentary Time and Physical Activity across the Day
3.4. Correlates of Sedentary Time and Physical Activity in Preschool-Aged Children
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Malina, R.M. Physical activity and fitness: pathways from childhood to adulthood. Am. J. Hum. Biol. 2001, 13, 162–172. [Google Scholar] [CrossRef]
- Timmons, B.W.; Leblanc, A.G.; Carson, V.; Connor Gorber, S.; Dillman, C.; Janssen, I.; Kho, M.E.; Spence, J.C.; Stearns, J.A.; Tremblay, M.S. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 773–792. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Chaput, J.P.; Adamo, K.B.; Aubert, S.; Barnes, J.D.; Choquette, L.; Duggan, M.; Faulkner, G.; Goldfield, G.S.; Gray, C.E.; et al. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health 2017, 17, 874. [Google Scholar] [CrossRef]
- Australian Government. Get up and Grow: Healthy Eating and Physical Activity for Early Childhood; Department of Health and Aging: Adelaide, Australia, 2010.
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Chief Medical Officers. Start Active, Stay Active: A Report on Physical Activity for Health from the Four Home Countries’ Chief Medical Officers; Department of Health and Social Care: London, UK, 2011.
- Hesketh, K.R.; Griffin, S.J.; van Sluijs, E.M. UK Preschool-aged children’s physical activity levels in childcare and at home: A cross-sectional exploration. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 123. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, K.R.; McMinn, A.M.; Ekelund, U.; Sharp, S.J.; Collings, P.J.; Harvey, N.C.; Godfrey, K.M.; Inskip, H.M.; Cooper, C.; van Sluijs, E.M. Objectively measured physical activity in four-year-old British children: A cross-sectional analysis of activity patterns segmented across the day. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- De Craemer, M.; McGregor, D.; Androutsos, O.; Manios, Y.; Cardon, G. Compliance with 24-h Movement Behaviour Guidelines among Belgian Pre-School Children: The ToyBox-Study. Int. J. Environ. Res. Public Health 2018, 15, 2171. [Google Scholar] [CrossRef] [PubMed]
- Hinkley, T.; Salmon, J.; Okely, A.D.; Crawford, D.; Hesketh, K. Preschoolers’ physical activity, screen time, and compliance with recommendations. Med. Sci. Sports Exerc. 2012, 44, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Garriguet, D.; Adamo, K.B.; Carson, V.; Janssen, I.; Timmons, B.W.; Tremblay, M.S. Physical activity and sedentary behavior during the early years in Canada: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 54. [Google Scholar] [CrossRef]
- Cliff, D.P.; Reilly, J.J.; Okely, A.D. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J. Sci. Med. Sport 2009, 12, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Oliver, M.; Schofield, G.M.; Kolt, G.S. Physical activity in preschoolers: Understanding prevalence and measurement issues. Sports Med. 2007, 37, 1045–1070. [Google Scholar] [CrossRef]
- Baranowski, T.; Jago, R. Understanding the mechanisms of change in children’s physical activity programs. Exerc. Sport Sci. Rev. 2005, 33, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Hinkley, T.; Salmon, J.; Okely, A.D.; Trost, S.G. Correlates of sedentary behaviours in preschool children: A review. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 66. [Google Scholar] [CrossRef] [PubMed]
- De Craemer, M.; De Decker, E.; De Bourdeaudhuij, I.; Vereecken, C.; Deforche, B.; Manios, Y.; Cardon, G.; ToyBox-Study Group. Correlates of energy balance-related behaviours in preschool children: A systematic review. Obes Rev 2012, 13 (Suppl. 1), 13–28. [Google Scholar] [CrossRef]
- Hinkley, T.; Crawford, D.; Salmon, J.; Okely, A.D.; Hesketh, K. Preschool children and physical activity: A review of correlates. Am. J. Prev. Med. 2008, 34, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Dolinsky, D.H.; Brouwer, R.J.; Evenson, K.R.; Siega-Riz, A.M.; Ostbye, T. Correlates of sedentary time and physical activity among preschool-aged children. Prev. Chronic Dis. 2011, 8, A131. [Google Scholar] [PubMed]
- Byun, W.; Dowda, M.; Pate, R.R. Correlates of objectively measured sedentary behavior in US preschool children. Pediatrics 2011, 128, 937–945. [Google Scholar] [CrossRef]
- Hnatiuk, J.A.; Hesketh, K.R.; van Sluijs, E.M. Correlates of home and neighbourhood-based physical activity in UK 3-4-year-old children. Eur. J. Public Health 2016, 26, 947–953. [Google Scholar] [CrossRef]
- Schmutz, E.A.; Leeger-Aschmann, C.S.; Radtke, T.; Muff, S.; Kakebeeke, T.H.; Zysset, A.E.; Messerli-Burgy, N.; Stulb, K.; Arhab, A.; Meyer, A.H.; et al. Correlates of preschool children’s objectively measured physical activity and sedentary behavior: A cross-sectional analysis of the SPLASHY study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1. [Google Scholar] [CrossRef]
- Wijtzes, A.I.; Kooijman, M.N.; Kiefte-de Jong, J.C.; de Vries, S.I.; Henrichs, J.; Jansen, W.; Jaddoe, V.W.; Hofman, A.; Moll, H.A.; Raat, H. Correlates of physical activity in 2-year-old toddlers: The generation R study. J. Pediatr. 2013, 163, 791–799. [Google Scholar] [CrossRef]
- Johansson, E.; Hagstromer, M.; Svensson, V.; Ek, A.; Forssen, M.; Nero, H.; Marcus, C. Objectively measured physical activity in two-year-old children—Levels, patterns and correlates. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 3. [Google Scholar] [CrossRef]
- Downing, K.L.; Hinkley, T.; Salmon, J.; Hnatiuk, J.A.; Hesketh, K.D. Do the correlates of screen time and sedentary time differ in preschool children? BMC Public Health. 2017, 17, 285. [Google Scholar]
- Hager, E.R.; Gormley, C.E.; Latta, L.W.; Treuth, M.S.; Caulfield, L.E.; Black, M.M. Toddler physical activity study: Laboratory and community studies to evaluate accelerometer validity and correlates. BMC Public Health 2016, 16, 936. [Google Scholar] [CrossRef]
- Sherar, L.B.; Griew, P.; Esliger, D.W.; Cooper, A.R.; Ekelund, U.; Judge, K.; Riddoch, C. International children’s accelerometry database (ICAD): Design and methods. BMC Public Health 2011, 11, 485. [Google Scholar] [CrossRef]
- Hinkley, T.; O’Connell, E.; Okely, A.D.; Crawford, D.; Hesketh, K.; Salmon, J. Assessing volume of accelerometry data for reliability in preschool children. Med. Sci. Sports Exerc. 2012, 44, 2436–2441. [Google Scholar] [CrossRef]
- Niederer, I.; Kriemler, S.; Zahner, L.; Burgi, F.; Ebenegger, V.; Hartmann, T.; Meyer, U.; Schindler, C.; Nydegger, A.; Marques-Vidal, P.; et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): Study design of a cluster randomized controlled trial. BMC Public Health 2009, 9, 94. [Google Scholar] [CrossRef]
- Cardon, G.; Labarque, V.; Smits, D.; De Bourdeaudhuij, I. Promoting physical activity at the pre-school playground: The effects of providing markings and play equipment. Prev. Med. 2009, 48, 335–340. [Google Scholar] [CrossRef]
- Cardon, G.; De Bourdeaudhuij, I. Comparison of pedometer and accelerometer measures of physical activity in preschool children. Pediatr. Exerc. Sci. 2007, 19, 205–214. [Google Scholar] [CrossRef]
- Van Cauwenberghe, E.; Labarque, V.; Trost, S.G.; de Bourdeaudhuij, I.; Cardon, G. Calibration and comparison of accelerometer cut points in preschool children. Int. J. Pediatr. Obes. 2010, 6, e582–e589. [Google Scholar] [CrossRef]
- Gidlow, C.J.; Cochrane, T.; Davey, R.; Smith, H. In-school and out-of-school physical activity in primary and secondary school children. J. Sports Sci. 2008, 26, 1411–1419. [Google Scholar] [CrossRef]
- Smith, H.; Grogan, S.; Davey, R.; Cochrane, T. Developing a successful physical activity intervention in primary schools. Educ. Health 2009, 27, 63–66. [Google Scholar]
- Pfeiffer, K.A.; Dowda, M.; McIver, K.L.; Pate, R.R. Factors related to objectively measured physical activity in preschool children. Pediatr. Exerc. Sci. 2009, 21, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Janz, K.F.; Burns, T.L.; Torner, J.C.; Levy, S.M.; Paulos, R.; Willing, M.C.; Warren, J.J. Physical activity and bone measures in young children: The Iowa bone development study. Pediatrics 2001, 107, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Janz, K.F.; Gilmore, J.M.; Burns, T.L.; Levy, S.M.; Torner, J.C.; Willing, M.C.; Marshall, T.A. Physical activity augments bone mineral accrual in young children: The Iowa Bone Development study. J. Pediatr. 2006, 148, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, L.; Montgomery, C.; Williamson, A.; Fisher, A.; McColl, J.H.; Lo Conte, R.; Paton, J.Y.; Grant, S. Physical activity to prevent obesity in young children: Cluster randomised controlled trial. BMJ 2006, 333, 1041. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Van Sluijs, E.M.; McMinn, A.M.; Inskip, H.M.; Ekelund, U.; Godfrey, K.M.; Harvey, N.C.; Griffin, S.J. Correlates of light and moderate-to-vigorous objectively measured physical activity in four-year-old children. PLoS ONE 2013, 8, e74934. [Google Scholar] [CrossRef]
- Puyau, M.R.; Adolph, A.L.; Vohra, F.A.; Butte, N.F. Validation and calibration of physical activity monitors in children. Obes. Res. 2002, 10, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Almeida, M.J.; McIver, K.L.; Pfeiffer, K.A.; Dowda, M. Validation and calibration of an accelerometer in preschool children. Obesity 2006, 14, 2000–2006. [Google Scholar] [CrossRef]
- Snijders, T.; Bosker, R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling; SAGE Publications Ltd.: London, UK, 1999. [Google Scholar]
- Byun, W.; Beets, M.W.; Pate, R.R. Sedentary Behavior in Preschoolers: How Many Days of Accelerometer Monitoring Is Needed? Int. J. Environ. Res. Public Health 2015, 12, 13148–13161. [Google Scholar] [CrossRef]
- Addy, C.L.; Trilk, J.L.; Dowda, M.; Byun, W.; Pate, R.R. Assessing preschool children’s physical activity: How many days of accelerometry measurement. Pediatr. Exerc. Sci. 2014, 26, 103–109. [Google Scholar] [CrossRef]
- Wong, S.L.; Colley, R.; Connor Gorber, S.; Tremblay, M. Actical accelerometer sedentary activity thresholds for adults. J. Phys. Act. Health 2011, 8, 587–591. [Google Scholar] [CrossRef]
- Reilly, J.J.; Coyle, J.; Kelly, L.; Burke, G.; Grant, S.; Paton, J.Y. An objective method for measurement of sedentary behavior in 3- to 4-year olds. Obes. Res. 2003, 11, 1155–1158. [Google Scholar] [CrossRef]
- Sirard, J.R.; Trost, S.G.; Pfeiffer, K.A.; Dowda, M.; Pate, R.R. Calibration and Evaluation of an Objective Measure of Physical Activity in Preschool Children. J. Phys. Act. Health 2005, 3, 345–357. [Google Scholar] [CrossRef]
- Van Cauwenberghe, E.; Jones, R.A.; Hinkley, T.; Crawford, D.; Okely, A.D. Patterns of physical activity and sedentary behaviour in preschool children. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 138. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Sakashita, Y. Sleeping pattern of kindergartners and nursery school children: Function of daytime nap. Percept. Mot Skills 2002, 94, 219–228. [Google Scholar] [CrossRef]
- Pattinson, C.L.; Staton, S.L.; Smith, S.S.; Sinclair, D.M.; Thorpe, K.J. Emotional Climate and Behavioral Management during Sleep Time in Early Childhood Education Settings. Early Child. Res. Q. 2014, 29, 660–668. [Google Scholar] [CrossRef]
- Ward, T.M.; Gay, C.; Anders, T.F.; Alkon, A.; Lee, K.A. Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. J. Pediatr. Psychol. 2008, 33, 666–672. [Google Scholar] [CrossRef]
- Byun, W.; Blair, S.N.; Pate, R.R. Objectively measured sedentary behavior in preschool children: Comparison between Montessori and traditional preschools. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 2. [Google Scholar] [CrossRef]
- Bringolf-Isler, B.; Mader, U.; Dossegger, A.; Hofmann, H.; Puder, J.J.; Braun-Fahrlander, C.; Kriemler, S. Regional differences of physical activity and sedentary behaviour in Swiss children are not explained by socio-demographics or the built environment. Int. J. Public Health 2015, 60, 291–300. [Google Scholar] [CrossRef]
- Leeger-Aschmann, C.S.; Schmutz, E.A.; Radtke, T.; Kakebeeke, T.H.; Zysset, A.E.; Messerli-Burgy, N.; Stulb, K.; Arhab, A.; Meyer, A.H.; Munsch, S.; et al. Regional sociocultural differences as important correlate of physical activity and sedentary behaviour in Swiss preschool children. Swiss Med. Wkly. 2016, 146, w14377. [Google Scholar] [CrossRef][Green Version]
- Dowda, M.; Pfeiffer, K.A.; Brown, W.H.; Mitchell, J.A.; Byun, W.; Pate, R.R. Parental and environmental correlates of physical activity of children attending preschool. Arch. Pediatr. Adolesc. Med. 2011, 165, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Olesen, L.G.; Kristensen, P.L.; Korsholm, L.; Froberg, K. Physical activity in children attending preschools. Pediatrics 2013, 132, e1310–e1318. [Google Scholar] [CrossRef] [PubMed]
- Eichinger, M.; Schneider, S.; De Bock, F. Subjectively and objectively assessed social and physical environmental correlates of preschoolers’ accelerometer-based physical activity. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Hinkley, T.; Salmon, J.; Okely, A.D.; Hesketh, K.; Crawford, D. Correlates of preschool children’s physical activity. Am. J. Prev. Med. 2012, 43, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Cardon, G.M.; De Bourdeaudhuij, I.M. Are preschool children active enough? Objectively measured physical activity levels. Res. Q. Exerc. Sport 2008, 79, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Goodman, A.; Page, A.S.; Cooper, A.R.; International Children’s Accelerometry Database (ICAD) Collaborators. Daylight saving time as a potential public health intervention: An observational study of evening daylight and objectively-measured physical activity among 23,000 children from 9 countries. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 84. [Google Scholar] [CrossRef]
- Mullan, K. Technology and Children’s Screen-Based Activities in the UK: The Story of the Millennium So Far. Child Indic. Res. 2018, 11, 1781–1800. [Google Scholar] [CrossRef]
- Gupta, N.; Mathiassen, S.E.; Mateu-Figueras, G.; Heiden, M.; Hallman, D.M.; Jorgensen, M.B.; Holtermann, A. A comparison of standard and compositional data analysis in studies addressing group differences in sedentary behavior and physical activity. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 53. [Google Scholar] [CrossRef]
- Hesketh, K.R.; O’Malley, C.; Paes, V.M.; Moore, H.; Summerbell, C.; Ong, K.K.; Lakshman, R.; van Sluijs, E.M.F. Determinants of Change in Physical Activity in Children 0–6 years of Age: A Systematic Review of Quantitative Literature. Sports Med. 2017, 47, 1349–1374. [Google Scholar] [CrossRef]
| Characteristic | N (%) |
|---|---|
| Overall | 1052 (100.00) |
| Age | |
| 3 | 343 (32.60) |
| 4 | 709 (67.40) |
| Gender | |
| Male | 528 (50.19) |
| Female | 524 (49.81) |
| Country | |
| UK | 426 (40.49) |
| Switzerland | 142 (13.50) |
| Belgium | 104 (9.89) |
| USA | 380 (36.12) |
| Season | |
| Winter | 136 (12.93) |
| Spring | 110 (10.46) |
| Summer | 117 (11.12) |
| Autumn | 689 (65.49) |
| Ethnicity | |
| White | 200 (19.01) |
| Other | 219 (20.82) |
| Missing/Not available | 633 (60.17) |
| Parental Education | |
| Up to and including completion of compulsory vocational training | 86 (8.17) |
| Any post-compulsory education including vocational training | 300 (28.52) |
| Missing/Not available | 666 (63.31) |
| Day of the Week | |
| Weekday | 1052 (100.00) |
| Weekend | 626 (59.51) |
| Time of Sunrise | |
| Before 07:00 | 433 (41.16) |
| After 07:00 | 619 (58.84) |
| Time of Sunset | |
| Before 19:00 | 548 (52.09) |
| After 19:00 | 504 (47.91) |
| Hours of Daylight | |
| Less than 12 h | 589 (55.99) |
| More than 12 h | 463 (44.01) |
| Study | |
| Ballabeina | 142 (13.50) |
| Belgium Pre-School | 104 (9.89) |
| CHAMPS U.S. | 361 (34.32) |
| MAGIC | 387 (36.79) |
| CHAMPS UK | 39 (3.71) |
| IBDS | 19 (1.81) |
| Correlate | N | ≥180 min of TPA | X2 | p | ≥60 min of MVPA | X2 | p |
|---|---|---|---|---|---|---|---|
| Overall | 1052 | 736 (69.96) | N/A | N/A | 829 (78.80) | N/A | N/A |
| Age | |||||||
| 3 | 343 | 223 (65.01) | 257 (74.93) | ||||
| 4 | 709 | 513 (72.36) | 5.93 | 0.015 | 572 (80.68) | 4.58 | 0.032 |
| Gender | |||||||
| Male | 528 | 406 (76.89) | 451 (85.42) | ||||
| Female | 524 | 330 (62.98) | 24.24 | <0.001 | 378 (72.14) | 27.76 | <0.001 |
| Country | |||||||
| UK | 426 | 297 (69.72) | 332 (77.93) | ||||
| Switzerland | 142 | 99 (69.72) | 108 (76.06) | ||||
| Belgium | 104 | 46 (44.23) | 52 (50.00) | ||||
| USA | 380 | 294 (77.37) | 42.70 | <0.001 | 337 (88.68) | 74.70 | <0.001 |
| Season | |||||||
| Winter | 136 | 82 (60.29) | 93 (68.38) | ||||
| Spring | 110 | 79 (71.82) | 85 (77.27) | ||||
| Summer | 117 | 90 (76.92) | 106 (90.60) | ||||
| Autumn | 689 | 485 (70.39) | 8.99 | 0.029 | 545 (79.10) | 18.78 | <0.001 |
| Ethnicity | |||||||
| White | 200 | 143 (71.50) | 156 (78.00) | ||||
| Other | 219 | 171 (78.08) | 2.41 | 0.120 | 203 (92.69) | 18.40 | <0.001 |
| Parental Education | |||||||
| Up to and including completion of compulsory vocational training | 86 | 73 (84.88) | 81 (94.19) | ||||
| Any post-compulsory education including vocational training | 300 | 226 (75.33) | 3.49 | 0.062 | 260 (86.67) | 3.67 | 0.055 |
| Weekday vs. Weekend | |||||||
| Weekday | 1052 | 720 (68.44) | 813 (77.28) | ||||
| Weekend | 626 | 386 (61.66) | 8.03 | 0.005 | 423 (67.57) | 19.07 | <0.001 |
| Time of Sunrise | |||||||
| Before 07:00 | 433 | 344 (79.45) | 382 (88.22) | ||||
| After 07:00 | 619 | 392 (63.33) | 31.49 | <0.001 | 447 (72.21) | 39.09 | <0.001 |
| Time of Sunset | |||||||
| Before 19:00 | 548 | 350 (63.87) | 399 (72.81) | ||||
| After 19:00 | 504 | 386 (76.59) | 20.21 | <0.001 | 430 (85.32) | 24.59 | <0.001 |
| Hours of daylight | |||||||
| Less than 12 h | 589 | 383 (65.03) | 435 (73.85) | ||||
| More than 12 h | 463 | 353 (76.24) | 15.52 | <0.001 | 394 (85.10) | 19.62 | <0.001 |
| Sedentary Time | ||||||
| Correlate (Reference Category) | N | β | (95% CI) | p | ICC | R2 |
| Age (ref = 3−years) | 1052 | −3.54 | (−9.85, 2.77) | 0.272 | 0.085 | 0.635 |
| Gender (ref = Male) | 1052 | 17.81 | (12.14, 23.49) | <0.001 | 0.085 | 0.635 |
| Country (ref = UK) | 1052 | 0.000 | 0.944 | |||
| Switzerland | 22.06 | (12.09, 32.03) | <0.001 | |||
| Belgium | 36.68 | (25.34, 48.02) | <0.001 | |||
| USA | 10.73 | (2.54, 18.91) | 0.010 | |||
| Season (ref = Winter) | 1052 | 0.085 | 0.635 | |||
| Spring | −14.01 | (−26.28, −1.74) | 0.025 | |||
| Summer | −12.16 | (−24.90, 0.57) | 0.061 | |||
| Autumn | 0.93 | (−9.42, 11.28) | 0.861 | |||
| Ethnicity (ref = White) | 419 | −3.07 | (−12.71, 6.56) | 0.532 | 0.000 | 0.903 |
| Parental Education (ref = Up to/including compulsory education) | 386 | 14.91 | (3.65, 26.17) | 0.009 | 0.000 | 0.609 |
| Weekday vs. Weekend (ref = Weekday) | 1678 | −33.60 | (−40.03, −27.18) | <0.001 | 0.084 | 0.511 |
| Time of Sunrise (ref = Before 07:00) | 1052 | 10.80 | (3.88, 17.72) | 0.002 | 0.070 | 0.696 |
| Time of Sunset (ref = Before 19:00) | 1052 | −15.20 | (−22.20, −8.19) | <0.001 | 0.089 | 0.626 |
| Hours of daylight (ref = Less than 12 h) | 1052 | −10.33 | (−17.53, −3.13) | 0.005 | 0.085 | 0.636 |
| Total Physical Activity | ||||||
| Correlate (Reference Category) | N | β | (95% CI) | p | ICC | R2 |
| Age (ref = 3−years) | 1052 | 3.54 | (−2.77, 9.85) | 0.272 | 0.085 | 0.273 |
| Gender (ref = Male) | 1052 | −17.81 | (−23.48, −12.14) | <0.001 | 0.085 | 0.273 |
| Country (ref = UK) | 1052 | 0.000 | 0.888 | |||
| Switzerland | −22.05 | (−32.02, −12.08) | <0.001 | |||
| Belgium | −36.68 | (−48.02, −25.35) | <0.001 | |||
| USA | −10.72 | (−18.90, −2.53) | 0.010 | |||
| Season (ref = Winter) | 1052 | 0.085 | 0.273 | |||
| Spring | 14.00 | (1.73, 26.28) | 0.025 | |||
| Summer | 12.16 | (−0.58, 24.89) | 0.061 | |||
| Autumn | −0.93 | (−11.28, 9.42) | 0.860 | |||
| Ethnicity (ref = White) | 419 | 3.07 | (−6.56, 12.71) | 0.532 | 0.000 | 0.884 |
| Parental Education (ref = Up to/including compulsory education) | 386 | −14.91 | (−26.17, −3.65) | 0.009 | 0.000 | 0.203 |
| Weekday vs Weekend (ref = Weekday) | 1678 | −3.65 | (−9.30, 2.00) | 0.205 | 0.096 | 0.224 |
| Time of Sunrise (ref = Before 07:00) | 1052 | −10.80 | (−17.72, −3.87) | 0.002 | 0.070 | 0.395 |
| Time of Sunset (ref = Before 19:00) | 1052 | 15.20 | (8.19, 22.20) | <0.001 | 0.089 | 0.256 |
| Hours of daylight (ref = Less than 12 h) | 1052 | 10.33 | (3.12, 17.53) | 0.005 | 0.085 | 0.276 |
| Moderate−to−Vigorous Physical Activity | ||||||
| Correlate (Reference Category) | N | β | (95% CI) | p | ICC | R2 |
| Age (ref = 3−years) | 1052 | 4.91 | (0.77, 9.05) | 0.020 | 0.095 | 0.299 |
| Gender (ref = Male) | 1052 | −14.94 | (−18.66, −11.21) | <0.001 | 0.095 | 0.299 |
| Country (ref = UK) | 1052 | 0.000 | 0.904 | |||
| Switzerland | −15.93 | (−22.46, −9.41) | <0.001 | |||
| Belgium | −22.48 | (−29.90, −15.05) | <0.001 | |||
| USA | 4.06 | (−1.30, 9.42) | 0.137 | |||
| Season (ref = Winter) | 1052 | 0.095 | 0.299 | |||
| Spring | 7.96 | (−0.10, 16.03) | 0.053 | |||
| Summer | 11.94 | (3.57, 20.32) | 0.005 | |||
| Autumn | 3.58 | (−3.24, 10.39) | 0.304 | |||
| Ethnicity (ref = White) | 419 | 9.53 | (2.89, 16.18) | 0.005 | 0.000 | 0.865 |
| Parental Education (ref = Up to/including compulsory education) | 386 | −7.75 | (−15.59, 0.09) | 0.053 | 0.000 | 0.149 |
| Weekday vs Weekend (ref = Weekday) | 1678 | −1.39 | (−4.96, 2.18) | 0.446 | 0.095 | 0.289 |
| Time of Sunrise (ref = Before 07:00) | 1052 | −4.96 | (−9.52, −0.40) | 0.033 | 0.086 | 0.364 |
| Time of Sunset (ref = Before 19:00) | 1052 | 9.47 | (4.86, 14.08) | <0.001 | 0.099 | 0.281 |
| Hours of daylight (ref = Less than 12 h) | 1052 | 7.04 | (2.30, 11.77) | 0.004 | 0.098 | 0.284 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dias, K.I.; White, J.; Jago, R.; Cardon, G.; Davey, R.; Janz, K.F.; Pate, R.R.; Puder, J.J.; Reilly, J.J.; Kipping, R., on behalf of the International Children’s Accelerometry Database (ICAD) Collaborators. International Comparison of the Levels and Potential Correlates of Objectively Measured Sedentary Time and Physical Activity among Three-to-Four-Year-Old Children. Int. J. Environ. Res. Public Health 2019, 16, 1929. https://doi.org/10.3390/ijerph16111929
Dias KI, White J, Jago R, Cardon G, Davey R, Janz KF, Pate RR, Puder JJ, Reilly JJ, Kipping R on behalf of the International Children’s Accelerometry Database (ICAD) Collaborators. International Comparison of the Levels and Potential Correlates of Objectively Measured Sedentary Time and Physical Activity among Three-to-Four-Year-Old Children. International Journal of Environmental Research and Public Health. 2019; 16(11):1929. https://doi.org/10.3390/ijerph16111929
Chicago/Turabian StyleDias, Kaiseree I, James White, Russell Jago, Greet Cardon, Rachel Davey, Kathleen F Janz, Russell R Pate, Jardena J Puder, John J Reilly, and Ruth Kipping on behalf of the International Children’s Accelerometry Database (ICAD) Collaborators. 2019. "International Comparison of the Levels and Potential Correlates of Objectively Measured Sedentary Time and Physical Activity among Three-to-Four-Year-Old Children" International Journal of Environmental Research and Public Health 16, no. 11: 1929. https://doi.org/10.3390/ijerph16111929
APA StyleDias, K. I., White, J., Jago, R., Cardon, G., Davey, R., Janz, K. F., Pate, R. R., Puder, J. J., Reilly, J. J., & Kipping, R., on behalf of the International Children’s Accelerometry Database (ICAD) Collaborators. (2019). International Comparison of the Levels and Potential Correlates of Objectively Measured Sedentary Time and Physical Activity among Three-to-Four-Year-Old Children. International Journal of Environmental Research and Public Health, 16(11), 1929. https://doi.org/10.3390/ijerph16111929






