Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification
Abstract
1. Introduction
2. Materials and Methods
2.1. Mortality Data for Study Population
2.2. Air Pollution and Meteorological Exposure
2.3. Statistical Methods
- (a)
- Overall effect of PM10:
- (b)
- Modified effect of PM10 according to SSC strata:
2.4. Ethics Approval
3. Results
3.1. Descriptive Statistics of Mortality and Environmental Factors
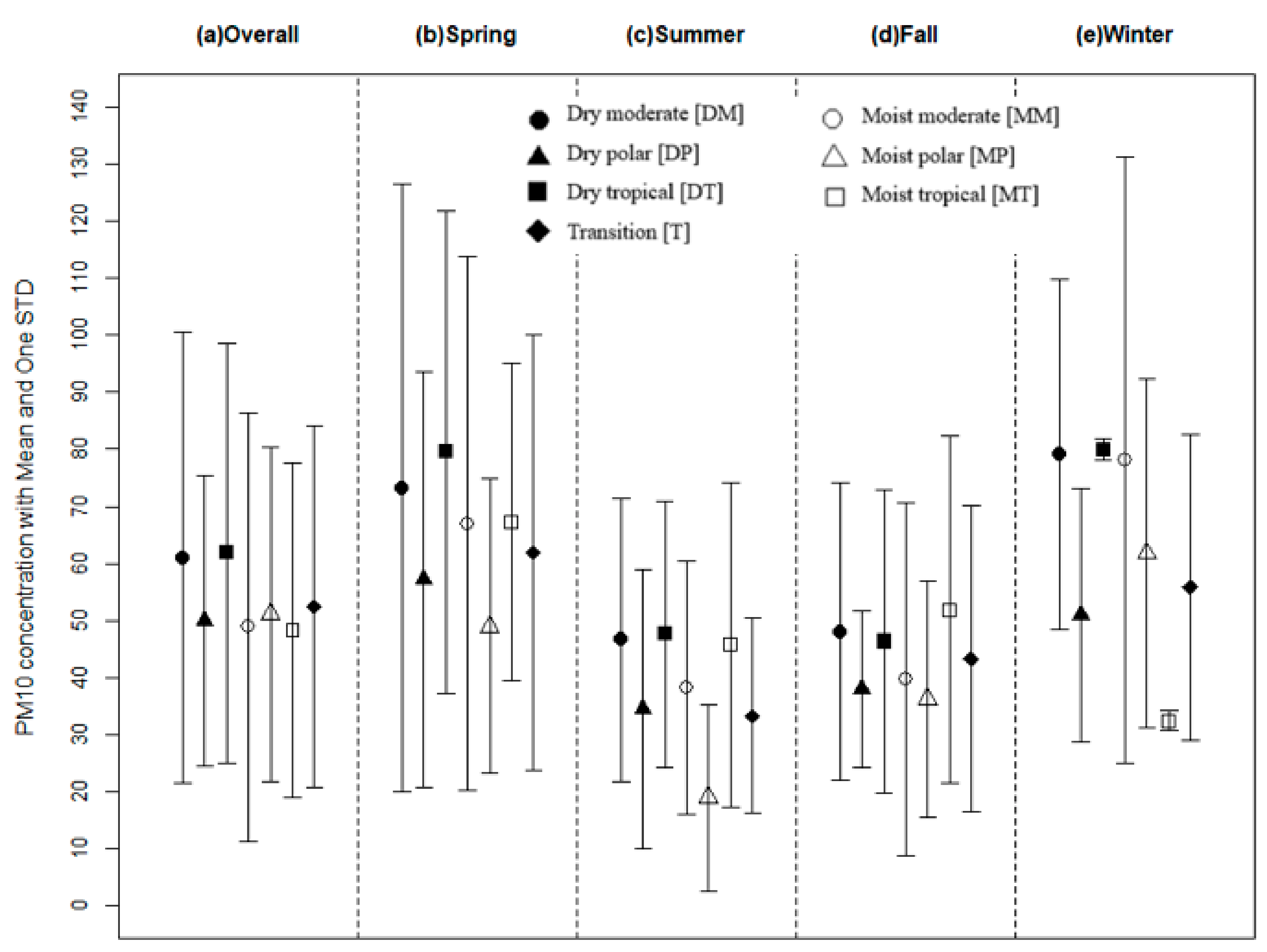
3.2. PM10 Daily Mortality Modification by Weather Type
3.3. Age-Specific PM10 Daily Mortality Affected by Weather Classification
3.4. Weather Classification Influence on the Seasonal Modification of PM10 Daily Mortality
4. Discussion
4.1. Principal Findings
4.2. Relationships between PM10 and Weather Conditions on Mortality
4.2.1. Relationships between Fractions of Particulate Matter and Cause-Specific Mortality
4.2.2. Epidemiological Approach for Modified Effect
4.2.3. Comparisons with Other Studies that Applied the SSC Scheme
4.2.4. Varied Study Designs and Adverse Health Effects of Particulate Matters
4.2.5. Age-Specified Effects between Particulate Matters and SSC Types
4.2.6. Weather Characteristics in SSC Types and Relationships between PM10 and Cause-Specific Mortality
4.3. Practical Implications of This Study
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yu, Y.; Yao, S.; Dong, H.; Wang, L.; Wang, C.; Ji, X.; Zhang, Z. Association between short-term exposure to particulate matter air pollution and cause-specific mortality in Changzhou, China. Environ. Res. 2019, 170, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Jiang, J.; Zhang, G.; Wang, L.; Wang, Z.; Yang, J.; Yu, C. Stroke Mortality Attributable to Ambient Particulate Matter Pollution from 1990 to 2015 in China: An Age-Period-Cohort and Spatial Autocorrelation Analysis. Int. J. Environ. Res. Public Health 2017, 14, 772. [Google Scholar] [CrossRef]
- Liang, H.; Qiu, H.; Tian, L. Short-term effects of fine particulate matter on acute myocardial infraction mortality and years of life lost: A time series study in Hong Kong. Sci. Total Environ. 2018, 615, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Forlivesi, S.; Turcato, G.; Zivelonghi, C.; Zannoni, M.; Ricci, G.; Cervellin, G.; Lippi, G.; Bovi, P.; Bonetti, B.; Cappellari, M. Association of Short- and Medium-Term Particulate Matter Exposure with Risk of Mortality after Spontaneous Intracerebral Hemorrhage. J. Stroke Cerebrovasc. Dis. 2018, 27, 2519–2523. [Google Scholar] [CrossRef] [PubMed]
- Tagliabue, G.; Borgini, A.; Tittarelli, A.; van Donkelaar, A.; Martin, R.V.; Bertoldi, M.; Fabiano, S.; Maghini, A.; Codazzi, T.; Scaburri, A.; et al. Atmospheric fine particulate matter and breast cancer mortality: A population-based cohort study. BMJ Open 2016, 6, e012580. [Google Scholar] [CrossRef] [PubMed]
- Li, M.H.; Fan, L.C.; Mao, B.; Yang, J.W.; Choi, A.M.K.; Cao, W.J.; Xu, J.F. Short-term Exposure to Ambient Fine Particulate Matter Increases Hospitalizations and Mortality in COPD: A Systematic Review and Meta-analysis. Chest 2016, 149, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Michikawa, T.; Ueda, K.; Takami, A.; Sugata, S.; Yoshino, A.; Nitta, H.; Yamazaki, S. Japanese Nationwide Study on the Association between Short-term Exposure to Particulate Matter and Mortality. J. Epidemiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Yin, P.; Meng, X.; Wang, L.; Liu, C.; Niu, Y.; Liu, Y.; Liu, Y.; Qi, J.; You, J.; et al. Associations between Coarse Particulate Matter Air Pollution and Cause-Specific Mortality: A Nationwide Analysis in 272 Chinese Cities. Environ. Health Perspect. 2019, 127, 017008. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Zhong, L.; Huang, X.; Xu, H.; Liu, S.; Feng, B.; Wang, T.; Song, X.; Bai, Y.; Wu, F.; et al. Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: A time-series analysis (2006–2016). Sci. Total. Environ. 2018, 645, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Honda, Y.; Hashizume, M.; Guo, Y.L.; Wu, C.F.; Kan, H.; Jung, K.; Lim, Y.H.; Yi, S.; Kim, H. Short-term exposure to fine and coarse particles and mortality: A multicity time-series study in East Asia. Environ. Pollut. 2015, 207, 43–51. [Google Scholar] [CrossRef]
- Adar, S.D.; Filigrana, P.A.; Clements, N.; Peel, J.L. Ambient Coarse Particulate Matter and Human Health: A Systematic Review and Meta-Analysis. Curr. Environ. Health Rep. 2014, 1, 258–274. [Google Scholar] [CrossRef] [PubMed]
- Qu, Y.; Pan, Y.; Niu, H.; He, Y.; Li, M.; Li, L.; Liu, J.; Li, B. Short-term effects of fine particulate matter on non-accidental and circulatory diseases mortality: A time series study among the elder in Changchun. PLoS ONE 2018, 13, e0209793. [Google Scholar] [CrossRef]
- Son, J.Y.; Lee, H.J.; Koutrakis, P.; Bell, M.L. Pregnancy and Lifetime Exposure to Fine Particulate Matter and Infant Mortality in Massachusetts, 2001–2007. Am. J. Epidemiol. 2017, 186, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.; Dominici, F.; Wang, Y.; Coull, B.A.; Bell, M.L. Associations between long-term exposure to chemical constituents of fine particulate matter (PM2.5) and mortality in Medicare enrollees in the eastern United States. Environ. Health Perspect. 2015, 123, 467–474. [Google Scholar] [CrossRef]
- Uccelli, R.; Mastrantonio, M.; Altavista, P.; Caiaffa, E.; Cattani, G.; Belli, S.; Comba, P. Female lung cancer mortality and long-term exposure to particulate matter in Italy. Eur. J. Public Health 2017, 27, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Parker, J.D.; Kravets, N.; Vaidyanathan, A. Particulate Matter Air Pollution Exposure and Heart Disease Mortality Risks by Race and Ethnicity in the United States: 1997 to 2009 National Health Interview Survey With Mortality Follow-Up Through 2011. Circulation 2018, 137, 1688–1697. [Google Scholar] [CrossRef]
- Pinault, L.L.; Weichenthal, S.; Crouse, D.L.; Brauer, M.; Erickson, A.; Donkelaar, A.V.; Martin, R.V.; Hystad, P.; Chen, H.; Fines, P.; et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ. Res. 2017, 159, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, C.; Linares, C.; Carmona, R.; Diaz, J. Evaluation of short-term mortality attributable to particulate matter pollution in Spain. Environ. Pollut. 2017, 224, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Kim, O.J.; Kim, S.Y.; Kim, H. Association between Long-Term Exposure to Particulate Matter Air Pollution and Mortality in a South Korean National Cohort: Comparison across Different Exposure Assessment Approaches. Int. J. Environ. Res. Public Health 2017, 14, 1103. [Google Scholar] [CrossRef]
- Badaloni, C.; Cesaroni, G.; Cerza, F.; Davoli, M.; Brunekreef, B.; Forastiere, F. Effects of long-term exposure to particulate matter and metal components on mortality in the Rome longitudinal study. Environ. Int. 2017, 109, 146–154. [Google Scholar] [CrossRef]
- Achilleos, S.; Kioumourtzoglou, M.A.; Wu, C.D.; Schwartz, J.D.; Koutrakis, P.; Papatheodorou, S.I. Acute effects of fine particulate matter constituents on mortality: A systematic review and meta-regression analysis. Environ. Int. 2017, 109, 89–100. [Google Scholar] [CrossRef]
- Macintyre, H.L.; Heaviside, C.; Neal, L.S.; Agnew, P.; Thornes, J.; Vardoulakis, S. Mortality and emergency hospitalizations associated with atmospheric particulate matter episodes across the UK in spring 2014. Environ. Int. 2016, 97, 108–116. [Google Scholar] [CrossRef]
- Su, C.; Hampel, R.; Franck, U.; Wiedensohler, A.; Cyrys, J.; Pan, X.; Wichmann, H.E.; Peters, A.; Schneider, A.; Breitner, S. Assessing responses of cardiovascular mortality to particulate matter air pollution for pre-, during- and post-2008 Olympics periods. Environ. Res. 2015, 142, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Zu, K.; Tao, G.; Long, C.; Goodman, J.; Valberg, P. Long-range fine particulate matter from the 2002 Quebec forest fires and daily mortality in Greater Boston and New York City. Air Qual. Atmos. Health 2016, 9, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A., 3rd; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S.; et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef]
- Kim, S.E.; Lim, Y.H.; Kim, H. Temperature modifies the association between particulate air pollution and mortality: A multi-city study in South Korea. Sci. Total Environ. 2015, 524, 376–383. [Google Scholar] [CrossRef]
- Tian, L.; Liang, F.; Guo, Q.; Chen, S.; Xiao, S.; Wu, Z.; Jin, X.; Pan, X. The effects of interaction between particulate matter and temperature on mortality in Beijing, China. Environ. Sci. Process Impacts 2018, 20, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Cao, P.; Chan, K.P.; Tsang, H.; Wong, C.M.; Thach, T.Q. Temperature as a modifier of the effects of fine particulate matter on acute mortality in Hong Kong. Environ. Pollut. 2015, 205, 357–364. [Google Scholar] [CrossRef]
- Corraini, P.; Olsen, M.; Pedersen, L.; Dekkers, O.M.; Vandenbroucke, J.P. Effect modification, interaction and mediation: An overview of theoretical insights for clinical investigators. Clin. Epidemiol. 2017, 9, 331–338. [Google Scholar] [CrossRef]
- Sheridan, S.C. The redevelopment of a weather-type classification scheme for North America. Int. J. Clim. 2002, 22, 51–68. [Google Scholar] [CrossRef]
- Hondula, D.M.; Vanos, J.K.; Gosling, S.N. The SSC: A decade of climate-health research and future directions. Int. J. Biometeorol. 2014, 58, 109–120. [Google Scholar] [CrossRef]
- Zhao, N.; Cao, G.; Vanos, J.K.; Vecellio, D.J. The effects of synoptic weather on influenza infection incidences: A retrospective study utilizing digital disease surveillance. Int. J. Biometeorol. 2018, 62, 69–84. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, N.Z.; Vanos, J.K.; Cao, G.F. Effects of synoptic weather on ground-level PM2.5 concentrations in the United States. Atmos. Environ. 2017, 148, 297–305. [Google Scholar] [CrossRef]
- Cakmak, S.; Hebbern, C.; Vanos, J.; Crouse, D.L.; Burnett, R. Ozone exposure and cardiovascular-related mortality in the Canadian Census Health and Environment Cohort (CANCHEC) by spatial synoptic classification zone. Environ. Pollut. 2016, 214, 589–599. [Google Scholar] [CrossRef]
- Urban, A.; Kysely, J. Application of spatial synoptic classification in evaluating links between heat stress and cardiovascular mortality and morbidity in Prague, Czech Republic. Int. J. Biometeorol. 2018, 62, 85–96. [Google Scholar] [CrossRef]
- Hebbern, C.; Cakmak, S. Synoptic weather types and aeroallergens modify the effect of air pollution on hospitalisations for asthma hospitalisations in Canadian cities. Environ. Pollut. 2015, 204, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.M.; Kim, J.; Jung, K.; Eo, S.; Ahn, K. The effects of particulate matter on atopic dermatitis symptoms are influenced by weather type: Application of spatial synoptic classification (SSC). Int. J. Hygiene Environ. Health 2018, 221, 823–829. [Google Scholar] [CrossRef]
- Cakmak, S.; Hebbern, C.; Pinault, L.; Lavigne, E.; Vanos, J.; Crouse, D.L.; Tjepkema, M. Associations between long-term PM2.5 and ozone exposure and mortality in the Canadian Census Health and Environment Cohort (CANCHEC), by spatial synoptic classification zone. Environ. Int. 2018, 111, 200–211. [Google Scholar] [CrossRef]
- Vignal, C.; Pichavant, M.; Alleman, L.Y.; Djouina, M.; Dingreville, F.; Perdrix, E.; Waxin, C.; Alami, A.O.; Gover-Rosseau, C.; Desreumaux, P.; et al. Effects of urban coarse particles inhalation on oxidative and inflammatory parameters in the mouse lung and colon. Part. Fibre Toxicol. 2017, 14, 46. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Kim, S.E.; Bell, M.L.; Hashizume, M.; Honda, Y.; Kan, H.; Kim, H. Associations between mortality and prolonged exposure to elevated particulate matter concentrations in East Asia. Environ. Int. 2018, 110, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Fang, B.; Wang, C.; Xia, T.; Bottai, M.; Fang, F.; Cao, Y. Relationship between fine particulate matter, weather condition and daily non-accidental mortality in Shanghai, China: A Bayesian approach. PLoS ONE 2017, 12, e0187933. [Google Scholar] [CrossRef]
- Miettinen, O. Confounding and effect-modification. Am. J. Epidemiol. 1974, 100, 350–353. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J. On the distinction between interaction and effect modification. Epidemiology 2009, 20, 863–871. [Google Scholar] [CrossRef]
- Judd, C.M.; Kenny, D.A. Process Analysis:Estimating Mediation in Treatment Evaluations. Evaluat. Rev. 1981, 5, 602–619. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.; Kweon, J. Hourly differences in air pollution on the risk of asthma exacerbation. Environ. Pollut. 2015, 203, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Yi, O.; Hong, Y.C.; Kim, H. Seasonal effect of PM(10) concentrations on mortality and morbidity in Seoul, Korea: A temperature-matched case-crossover analysis. Environ. Res. 2010, 110, 89–95. [Google Scholar] [CrossRef]
- Kim, S.E.; Honda, Y.; Hashizume, M.; Kan, H.; Lim, Y.H.; Lee, H.; Kim, C.T.; Yi, S.M.; Kim, H. Seasonal analysis of the short-term effects of air pollution on daily mortality in Northeast Asia. Sci. Total Environ. 2017, 576, 850–857. [Google Scholar] [CrossRef]
| Variable | Overall a | Spring | Summer | Fall | Winter | |
|---|---|---|---|---|---|---|
| (Mar.–May) a | (Jun.–Aug.) a | (Sep.–Nov.) a | (Dec.–Feb.) a | |||
| Non-accidental mortality | 95.4 (12.3) | 95.9 (11.3) | 89.0 (10.7) | 95.5 (11.6) | 101.3 (12.5) | |
| Cardiovascular mortality | 23.8 (5.7) | 24.0 (5.5) | 21.6 (5.1) | 23.7 (5.7) | 25.8 (5.6) | |
| Respiratory mortality | 6.7 (2.8) | 6.9 (2.7) | 6.1 (2.5) | 6.3 (2.6) | 7.3 (3.1) | |
| Temperature (°C) | 12.8 (10.4) | 12.1 (6.2) | 24.6 (2.5) | 14.8 (6.7) | −0.7 (4.6) | |
| Diurnal temperature range (°C) | 7.7 (2.7) | 8.8 (2.8) | 6.8 (2.6) | 8.1 (2.6) | 7.1 (2.2) | |
| Relative Humidity (%) | 61.2 (14.8) | 55.7 (14.8) | 71.5 (12.2) | 62.0 (12.7) | 55.6 (13.2) | |
| Air pressure (hPa) | 1016.1 (8.2) | 1014.7 (6.2) | 1007.2 (4.2) | 1018.3 (5.6) | 1024.3 (5.2) | |
| Rain (mm) | 29.5 (145.3) | 16.8 (59.1) | 52.6 (222.2) | 25.1 (95.2) | 7.0 (38.3) | |
| PM10 (µg/m3) a | 54.4 (35.0) | 67.8 (46.3) | 43.3 (25.5) | 45.1 (25.9) | 61.4 (31.0) | |
| O3 (ppb) a | 17.1 (14.0) | 22.1 (14.7) | 22.2 (17.1) | 14.3 (10.5) | 9.7 (7.3) | |
| NO2 (ppb) a | 30.1 (18.7) | 32.5 (19.2) | 24.5 (14.8) | 29.8 (18.4) | 33.6 (20.5) | |
| Spatial synoptic classification, N. of day (%) | Dry moderate (DM) | 2037 (37.2) | 604 (43.8) | 309 (22.4) | 737 (54.0) | 387 (28.6) |
| Dry polar (DP) | 1052 (19.2) | 194 (14.1) | 4 (0.3) | 214 (15.7) | 640 (47.3) | |
| Dry tropical (DT) | 274 (5.0) | 136 (9.9) | 101 (7.3) | 33 (2.4) | 4 (0.3) | |
| Moist moderate (MM) | 868 (15.8) | 193 (14.0) | 429 (31.1) | 152 (11.1) | 94 (6.9) | |
| Moist polar (MP) | 217 (4.0) | 65 (4.7) | 12 (0.9) | 43 (3.2) | 97 (7.2) | |
| Moist tropical (MT) | 636 (11.6) | 61 (4.4) | 490 (35.5) | 80 (5.9) | 5 (0.4) | |
| Transition (T) | 395 (7.2) | 127 (9.2) | 35 (2.5) | 106 (7.8) | 127 (9.4) | |
| Category | Variables | Relative Risk Percentage Change (95% Confidence Interval) a | ||
|---|---|---|---|---|
| Non-Accidental Death | Cardiovascular Death | Respiratory Death | ||
| Overall effect b | PM10 | 1.11 (0.50, 1.73) | 1.87 (0.68, 3.08) | 0.83 (−1.27, 2.98) |
| Modification | Dry moderate (DM) | 1.08 (0.41, 1.76) | 2.20 (0.88, 3.53) | 0.25 (−2.05, 2.60) |
| Dry polar (DP) | 0.06 (−0.72, 0.85) | 0.48 (−1.04, 2.03) | −0.79 (−3.44, 1.93) | |
| Dry tropical (DT) | 1.86 (0.81, 2.93) | 2.83 (0.74, 4.96) | −0.24 (−3.83, 3.48) | |
| Moist moderate (MM) | 1.50 (0.67, 2.33) | 3.00 (1.38, 4.64) | 0.28 (−2.56, 3.19) | |
| Moist polar (MP) | 0.90 (−0.25, 2.06) | 1.34 (−0.91, 3.65) | 0.17 (−3.70, 4.19) | |
| Moist tropical (MT) | 1.86 (1.02, 2.70) | 2.01 (0.37, 3.67) | 3.78 (0.89, 6.76) | |
| Transition (T) | 1.00 (0.07, 1.94) | 1.91 (0.08, 3.78) | 1.89 (−1.29, 5.17) | |
| Variables | Age-Specified Relative Risk Percentage Change (95% Confidence Interval) a | ||||
|---|---|---|---|---|---|
| 40–59 | 60–74 | 75–84 | 85+ | ||
| Non-accidental death | Overall effect b | 1.78 (0.38, 3.19) | 0.88 (−0.20, 1.97) | 1.19 (0.06, 2.33) | 1.16 (−0.16, 2.51) |
| Dry c | 1.54 (0.09, 3.00) | 0.74 (−0.37, 1.87) | 1.03 (−0.14, 2.20) | 0.91 (−0.45, 2.29) | |
| Moist c | 2.32 (0.74, 3.93) | 1.11 (−0.12, 2.35) | 1.55 (0.26, 2.85) | 1.75 (0.23, 3.28) | |
| Transition c | 0.88 (−1.22, 3.04) | 1.52 (−0.12, 3.18) | 1.06 (−0.64, 2.78) | 1.00 (−0.97, 3.02) | |
| Moderate d | 1.28 (−0.23, 2.80) | 1.12 (−0.04, 2.29) | 1.05 (−0.16, 2.27) | 1.70 (0.28, 3.14) | |
| Polar d | 1.12 (−0.62, 2.88) | 0.17 (−1.18, 1.53) | 0.15 (−1.25, 1.56) | −0.13 (−1.76, 1.52) | |
| Tropical d | 3.07 (1.34, 4.83) | 0.98 (−0.37, 2.35) | 2.25 (0.84, 3.69) | 1.36 (−0.31, 3.06) | |
| Transition d | 0.59 (−1.53, 2.75) | 1.51 (−0.14, 3.19) | 0.81 (−0.90, 2.54) | 1.00 (−0.99, 3.03) | |
| Cardiovascular death | Overall effect b | 1.01 (−1.94, 4.05) | 1.08 (−0.98, 3.17) | 1.75 (−0.24, 3.77) | 1.10 (−1.34, 3.60) |
| Dry c | 1.10 (−1.96, 4.26) | 1.22 (−0.90, 3.40) | 1.33 (−0.72, 3.41) | 0.77 (−1.77, 3.37) | |
| Moist c | 0.92 (−2.41, 4.36) | 0.76 (−1.56, 3.14) | 2.68 (0.42, 4.99) | 1.36 (−1.39, 4.18) | |
| Transition c | 0.11 (−4.40, 4.84) | 1.45 (−1.68, 4.67) | 0.75 (−2.25, 3.84) | 4.00 (0.29, 7.84) | |
| Moderate d | 0.93 (−2.21, 4.17) | 1.56 (−0.66, 3.83) | 1.77 (−0.37, 3.95) | 2.07 (−0.56, 4.77) | |
| Polar d | 1.51 (−2.21, 5.38) | 1.15 (−1.46, 3.83) | 0.46 (−2.01, 2.99) | −2.02 (−5.05, 1.11) | |
| Tropical d | 0.88 (−2.86, 4.77) | 0.26 (−2.29, 2.87) | 2.77 (0.28, 5.33) | 1.30 (−1.76, 4.47) | |
| Transition d | 0.15 (−4.40, 4.91) | 1.63 (−1.53, 4.90) | 0.60 (−2.42, 3.72) | 3.83 (0.10, 7.69) | |
| Respiratory death | Overall effect b | N/A | 1.04 (−3.52, 5.81) | −2.24 (−5.29, 0.92) | −2.24 (−5.29, 0.92) |
| Dry c | N/A | 1.75 (−2.87, 6.59) | −2.72 (−5.87, 0.52) | −1.88 (−5.46, 1.83) | |
| Moist c | N/A | −1.20 (−6.37, 4.25) | −1.34 (−4.81, 2.26) | −3.30 (−7.42, 1.00) | |
| Transition c | N/A | 3.78 (−3.02, 11.06) | −1.00 (−5.71, 3.94) | 1.16 (−4.08, 6.68) | |
| Moderate d | N/A | 1.51 (−3.32, 6.57) | −2.32 (−5.68, 1.16) | −0.91 (−4.65, 2.97) | |
| Polar d | N/A | −1.67 (−6.92, 3.89) | −2.81 (−6.59, 1.11) | −4.03 (−8.21, 0.35) | |
| Tropical d | N/A | 4.06 (−1.83, 10.31) | −1.78 (−5.53, 2.12) | −3.18 (−7.85, 1.72) | |
| Transition d | N/A | 3.47 (−3.35, 10.76) | −1.00 (−5.77, 4.02) | 1.25 (−4.00, 6.78) | |
| Variable | SSC Category | Relative Risk Percentage Change (95% Confidence Interval) a | ||||
|---|---|---|---|---|---|---|
| Overall | Spring | Summer | Fall | Winter | ||
| Non-accidental death | Dry b | 0.94 (0.31, 1.58) | 0.97 (0.21, 1.74) | 1.77 (0.44, 3.11) | 0.80 (−0.46, 2.07) | 0.72 (−0.22, 1.66) |
| Moist b | 1.48 (0.78, 2.18) | 0.84 (−0.06, 1.75) | 2.18 (0.92, 3.45) | 2.30 (0.92, 3.70) | 1.63 (0.43, 2.86) | |
| Transition b | 1.12 (0.20, 2.05) | 0.74 (−0.50, 2.00) | −1.95 (−5.36, 1.59) | 0.88 (−1.07, 2.87) | 1.95 (0.51, 3.40) | |
| Moderate c | 1.13 (0.48, 1.79) | 1.07 (0.26, 1.88) | 1.78 (0.52, 3.06) | 1.57 (0.32, 2.84) | 1.00 (0.01, 1.99) | |
| Polar c | 0.22 (−0.54, 0.98) | 0.33 (−0.73, 1.41) | N/A | 0.21 (−1.41, 1.85) | 0.21 (−0.84, 1.27) | |
| Tropical c | 1.79 (1.03, 2.56) | 1.26 (0.33, 2.20) | 2.59 (1.27, 3.93) | 2.32 (0.58, 4.09) | N/A | |
| Transition c | 0.98 (0.05, 1.91) | 0.81 (−0.44, 2.08) | −1.87 (−5.28, 1.67) | 0.97(−0.98, 2.96) | 1.75 (0.31, 3.21) | |
| Cardiovascular death | Dry b | 1.72 (0.49, 2.97) | 2.09 (0.60, 3.60) | 2.85 (0.24, 5.52) | 2.01 (−0.47, 4.55) | 0.73 (−1.11, 2.60) |
| Moist b | 2.18 (0.82, 3.55) | 0.82 (−0.93, 2.60) | 3.29 (0.82, 5.82) | 2.68 (−0.03, 5.47) | 3.69 (1.31, 6.13) | |
| Transition b | 1.90 (0.08, 3.75) | 2.05 (−0.40, 4.57) | 0.05 (−6.67, 7.24) | −0.37 (−4.21, 3.63) | 2.82 (0.01, 5.72) | |
| Moderate c | 2.30 (1.01, 3.60) | 2.59 (1.00, 4.21) | 3.12 (0.63, 5.67) | 2.64 (0.17, 5.17) | 1.61 (−0.33, 3.59) | |
| Polar c | 0.63 (−0.85, 2.13) | 0.23 (−1.84, 2.34) | N/A | 0.90 (−2.26, 4.17) | 0.59 (−1.48, 2.70) | |
| Tropical c | 2.15 (0.66, 3.67) | 1.33 (−0.50, 3.19) | 3.65 (1.04, 6.32) | 3.30 (−0.10, 6.82) | N/A | |
| Transition c | 1.84 (0.02, 3.71) | 2.20 (−0.28, 4.74) | 0.27 (−6.46, 7.50) | −0.38 (−4.23, 3.62) | 2.69 (−0.14, 5.60) | |
| Respiratory death | Dry b | 0.37 (−1.78, 2.58) | −0.38 (−2.95, 2.26) | −0.30 (−4.85, 4.47) | −0.78 (−5.25, 3.91) | 2.33 (−0.81, 5.57) |
| Moist b | 1.75 (−0.67, 4.22) | −0.08 (−3.16, 3.09) | 2.34 (−2.10, 6.98) | 3.13 (−1.82, 8.34) | 3.59 (−0.51, 7.85) | |
| Transition b | 2.44 (−0.72, 5.71) | 2.41 (−1.80, 6.79) | −0.27 (−12.34, 13.46) | −0.85 (−7.50, 6.26) | 4.61 (−0.25, 9.71) | |
| Moderate c | 0.40 (−1.85, 2.69) | −0.76 (−3.50, 2.05) | 0.83 (−3.57, 5.43) | −0.17 (−4.61, 4.48) | 2.86 (−0.43, 6.27) | |
| Polar c | −0.48 (−3.06, 2.16) | −0.98 (−4.59, 2.76) | −0.79 (−17.97, 19.98) | −0.61 (−6.29, 5.42) | 1.05 (−2.47, 4.70) | |
| Tropical c | 2.49 (−0.16, 5.22) | 1.29 (−1.86, 4.54) | 2.41 (−2.25, 7.29) | 5.63 (−0.75, 12.41) | 13.57 (−4.33, 34.82) | |
| Transition c | 2.09 (−1.09, 5.37) | 2.36 (−1.87, 6.79) | 0.00 (−12.12, 13.80) | −0.88 (−7.52, 6.24) | 4.14 (−0.72, 9.24) | |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J. Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification. Int. J. Environ. Res. Public Health 2019, 16, 1904. https://doi.org/10.3390/ijerph16111904
Kim J. Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification. International Journal of Environmental Research and Public Health. 2019; 16(11):1904. https://doi.org/10.3390/ijerph16111904
Chicago/Turabian StyleKim, Jayeun. 2019. "Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification" International Journal of Environmental Research and Public Health 16, no. 11: 1904. https://doi.org/10.3390/ijerph16111904
APA StyleKim, J. (2019). Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification. International Journal of Environmental Research and Public Health, 16(11), 1904. https://doi.org/10.3390/ijerph16111904




