Medical Clerkship in a State Registration and Reception Center for Forced Migrants in Germany: Students’ Experiences, Teachable Moments, and Psychological Burden
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. The Medical Clerkship
2.3. Student Sample
2.4. The State Registration and Reception Center “Patrick Henry Village” in Heidelberg–Kirchheim
2.5. Ethics
2.6. Sociodemographic Data of the Student Sample
2.7. Qualitative Assessment: Semi-Standardized Pre–Post Interviews
2.8. Qualitative Content Analysis
2.9. Reflective Diaries
2.10. Evaluation of Reflective Diaries
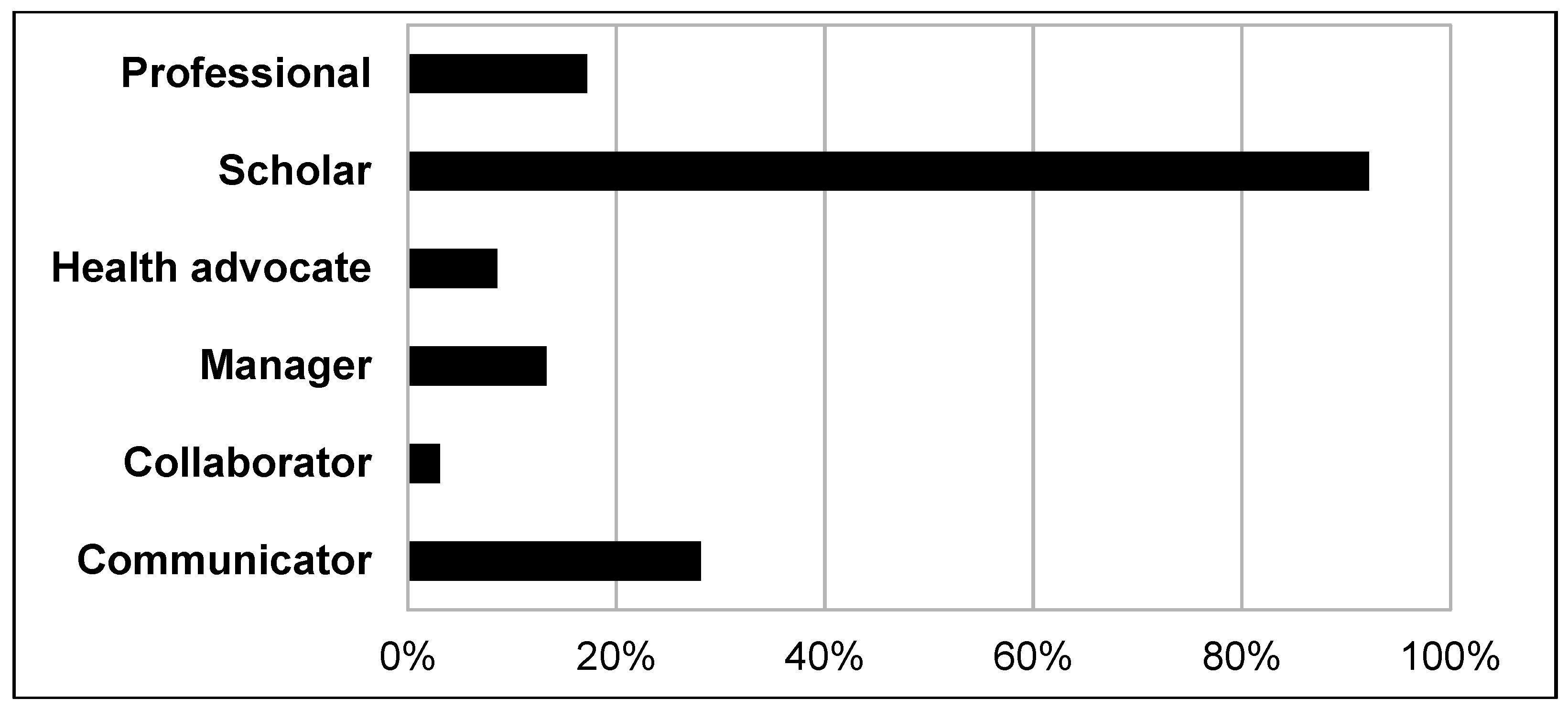
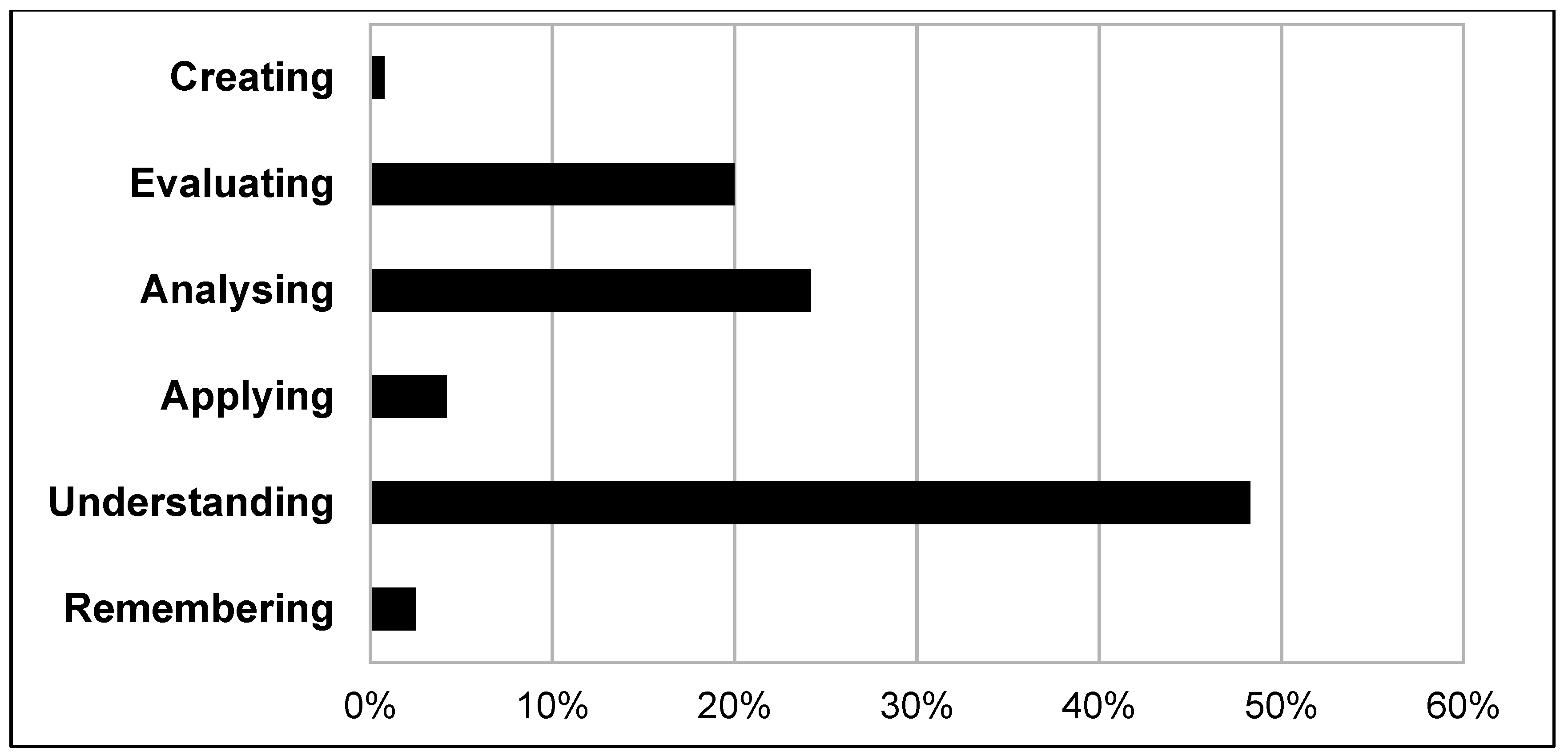
2.11. Bloom´s Taxonomy and the CanMEDS Framework
2.12. Quantitative Pre–Post Assessment of Psychological Strain
2.13. Quantitative Statistical Analysis
3. Results
3.1. Sample Description and Response Rate
3.2. Qualitative Assessment: Results of Pre–Post Interviews
3.2.1. Main Categories and Themes from the Pre-Interviews
“[I have been thinking about] the language barrier and how it will influence the quality of treatment. Otherwise I am just a little curious if there will be cultural difficulties and if you will try and speak about specific issues, or if you just formulate some issues badly.”(A1.11)
“I think it [the medical clerkship] can be stressful when you are confronted with different fates and get in touch with the individual patients.”(A1.2)
“I look forward to perhaps broadening my horizon and to interacting with different patients; I can probably use this expertise for my future profession.”(A1.9)
3.2.2. Main Categories and Themes from the Post-Interviews
“In fact, the main problem was the language barrier, which was not really unbreachable but nevertheless a major obstacle, especially when there was no interpreter available. Some common foreign languages were helpful, for instance English or French. Fortunately, I speak a bit of French.”(A1.2)
“There were a few individual background stories about which I had to think again, because those stories were just mad; although you hear about those stories in the newscast, it is crazy if someone who experienced such things on their own is standing right in front of you. Especially in the psychosocial outpatient clinic you hear a lot of those stories. In general medicine you sometimes do not even get in touch with it [the stories], but in Psychosomatics [the psychosocial outpatient clinic] there were some cases which kept coming back to me later on.”(A1.4)
“In fact, I had the feeling that this problem [war and flight] was so big, that you cannot do a lot about it. It feels like waking up, saying ´Okay, this is a huge problem and I have to do something, but I am just not in the position to do so´. In fact, this is a sad feeling; but actually, it seems to be a mixture of positive and negative feelings.”(A1.6)
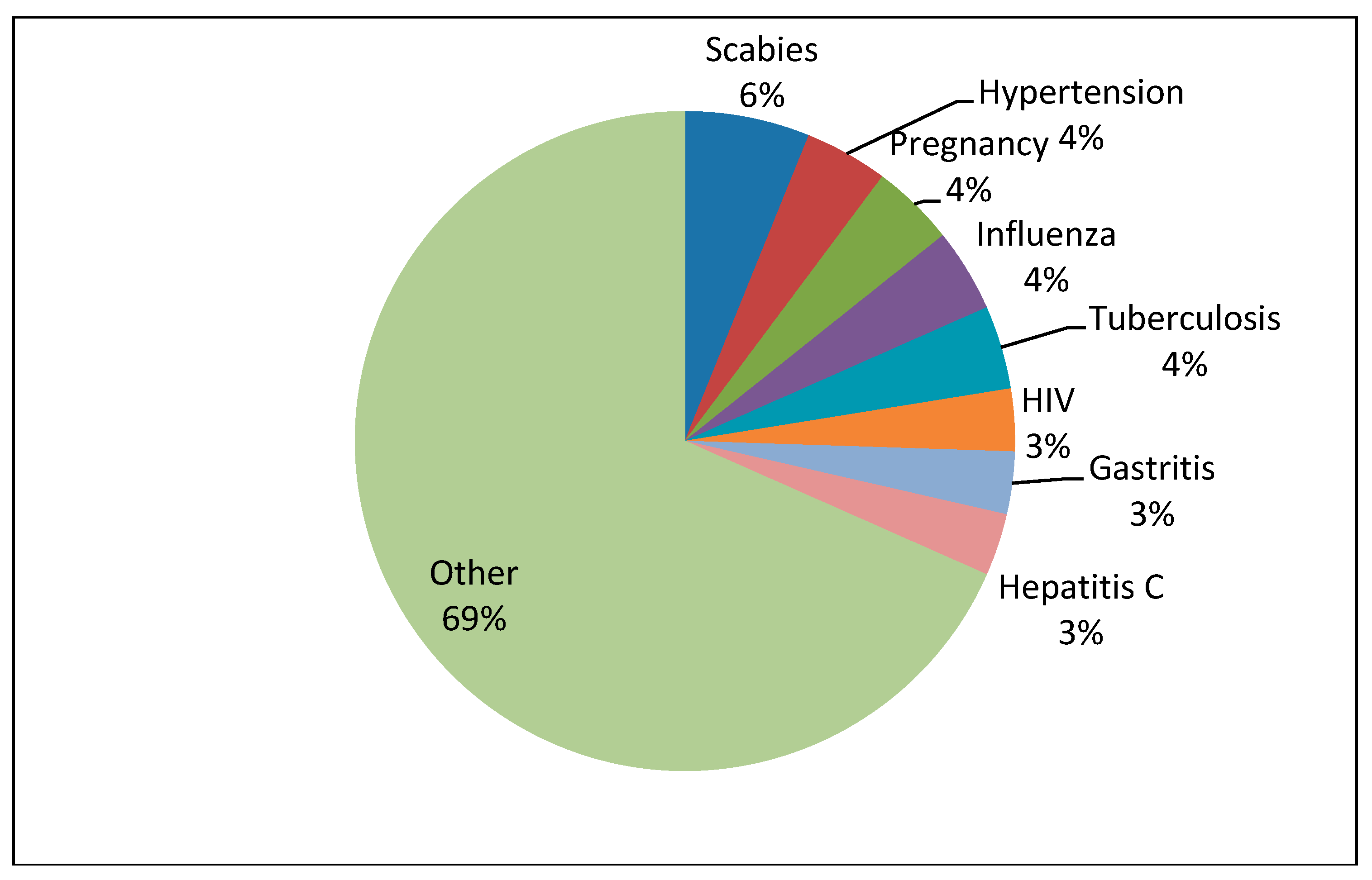
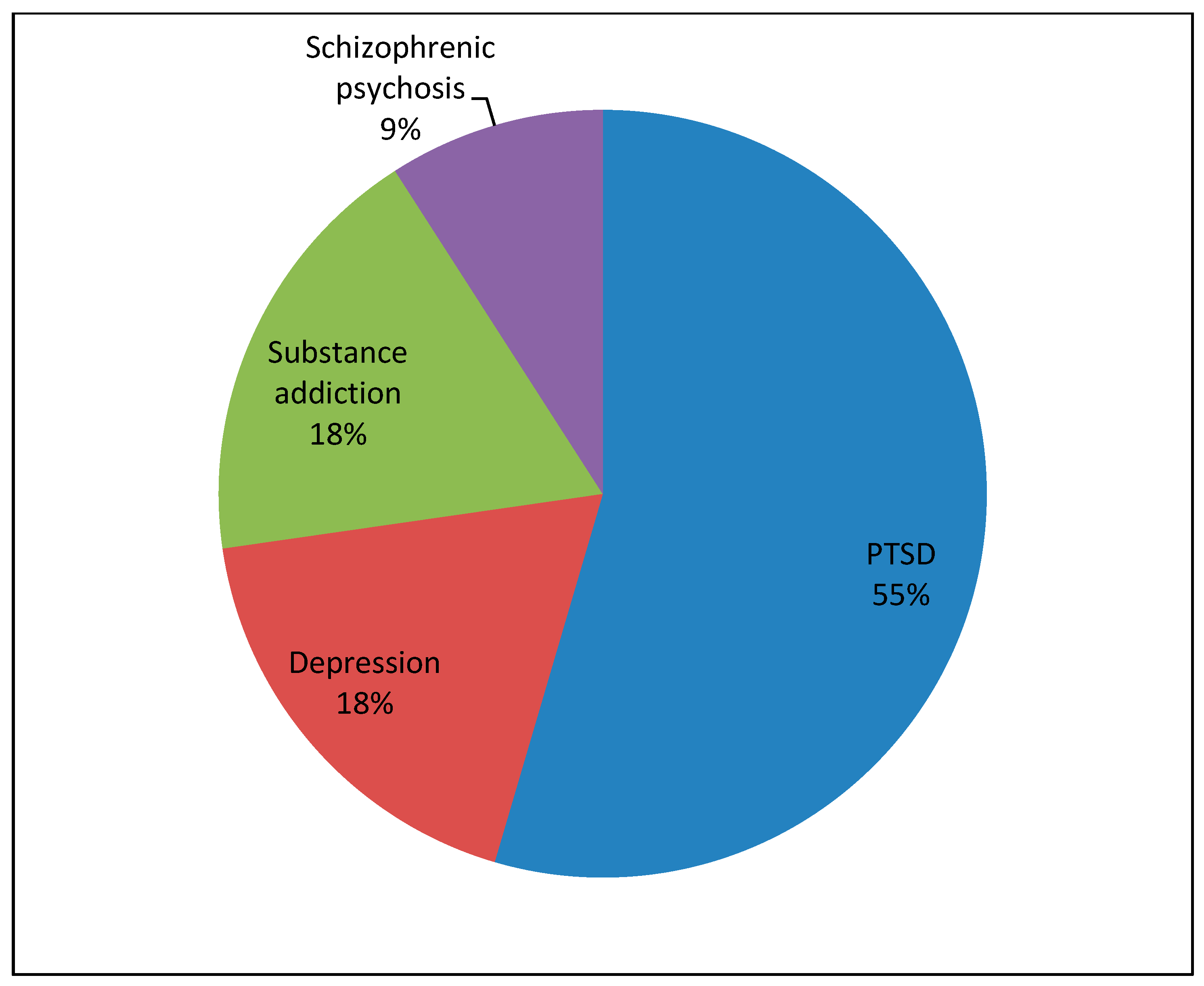
3.3. The Students’ Reflective Diaries
3.4. Psychological Strain and Secondary Traumatization of the Medical Students
4. Discussion
4.1. Psychological Distress and STS
4.2. Cultural Horizons and Sensitivity
4.3. Teachable Moments and Learning Achievements
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Quotations from pre-interviews |
|---|
Category (A) Expectations of the medical clerkship (110 codes)
|
Category (B) Motivations for the assignment (75 codes)
|
| Quotations from post-interviews |
|---|
Category (C) Subjective experiences during the medical clerkship (209 codes)
|
Category (D) Subjective experiences after the medical clerkship and reflection (149 codes)
|
References
- BAMF. Das bundesamt in zahlen 2017; asyl. Federal Office for Migration and Refugees. Available online: https://www.bamf.de/SharedDocs/Anlagen/DE/Publikationen/Broschueren/bundesamt-in-zahlen-2017-asyl.pdf?__blob=publicationFile (accessed on 23 August 2018).
- Manok, N.; Huhn, D.; Kohl, R.M.; Ludwig, M.; Schweitzer, J.; Kaufmann, C.; Terhoeven, V.; Ditzen, B.; Herpertz, S.C.; Herzog, W.; et al. Outpatient clinic for refugees with posttraumatic disorders and mental burdens in a state reception center. Psychotherapeut 2017, 62, 1–8. [Google Scholar]
- Bozorgmehr, K.; Mohsenpour, A.; Saure, D.; Stock, C.; Loerbroks, A.; Joos, S.; Schneider, C. Systematic review and evidence mapping of empirical studies on health status and medical care among refugees and asylum seekers in germany (1990-2014). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2016, 59, 599–620. [Google Scholar] [CrossRef]
- Maercker, A.; Forstmeier, S.; Wagner, B.; Glaesmer, H.; Brähler, E. Post-traumatic stress disorder in germany. Results of a nationwide epidemiological study. Der Nervenarzt 2008, 79, 577–586. [Google Scholar] [CrossRef]
- Lee, D.; Philen, R.; Wang, Z.; McSpadden, P.; Posey, D.L.; Ortega, L.S. Disease surveillance among newly arriving refugees and immigrants—Electronic disease notification system, united states, 2009. MMWR Surveill Summ. 2013, 62, 1–20. [Google Scholar]
- Ravensbergen, S.J.; Lokate, M.; Cornish, D.; Kloeze, E.; Ott, A.; Friedrich, A.W.; van Hest, R.; Akkerman, O.W.; de Lange, W.C.; van der Werf, T.S. High prevalence of infectious diseases and drug-resistant microorganisms in asylum seekers admitted to hospital; no carbapenemase producing enterobacteriaceae until september 2015. PLoS ONE 2016, 11, e0154791. [Google Scholar] [CrossRef] [PubMed]
- Meier, V.; Artelt, T.; Cierpiol, S.; Gossner, J.; Scheithauer, S. Tuberculosis in newly arrived asylum seekers: A prospective 12 month surveillance study at friedland, germany. Int. J. Hyg. Environ. Health 2016, 219, 811–815. [Google Scholar] [CrossRef]
- Sonden, K.; Castro, E.; Tornnberg, L.; Stenstrom, C.; Tegnell, A.; Farnert, A. High incidence of plasmodium vivax malaria in newly arrived eritrean refugees in sweden since May 2014. Eur. Surveill 2014, 19, 20890. [Google Scholar] [CrossRef]
- Drain, P.K.; Primack, A.; Hunt, D.D.; Fawzi, W.W.; Holmes, K.K.; Gardner, P. Global health in medical education: A call for more training and opportunities. Acad. Med. 2007, 82, 226–230. [Google Scholar] [CrossRef]
- Bateman, C.; Baker, T.; Hoornenborg, E.; Ericsson, U. Bringing global issues to medical teaching. Lancet 2001, 358, 1539–1542. [Google Scholar]
- Izadnegahdar, R.; Correia, S.; Ohata, B.; Kittler, A.; ter Kuile, S.; Vaillancourt, S.; Saba, N.; Brewer, T.F. Global health in canadian medical education: Current practices and opportunities. Acad. Med. 2008, 83, 192–198. [Google Scholar] [CrossRef]
- Peluso, M.J.; Forrestel, A.K.; Hafler, J.P.; Rohrbaugh, R.M. Structured global health programs in us medical schools: A web-based review of certificates, tracks, and concentrations. Acad. Med. 2013, 88, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Battat, R.; Seidman, G.; Chadi, N.; Chanda, M.Y.; Nehme, J.; Hulme, J.; Li, A.; Faridi, N.; Brewer, T.F. Global health competencies and approaches in medical education: A literature review. BMC Med. Educ. 2010, 10, 94. [Google Scholar] [CrossRef]
- Houpt, E.R.; Pearson, R.D.; Hall, T.L. Three domains of competency in global health education: Recommendations for all medical students. Acad. Med. 2007, 82, 222–225. [Google Scholar] [CrossRef]
- Peluso, M.J.; Encandela, J.; Hafler, J.P.; Margolis, C.Z. Guiding principles for the development of global health education curricula in undergraduate medical education. Med. Teach. 2012, 34, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Duke, P.; Brunger, F. The mun med gateway project: Marrying medical education and social accountability. Can. Fam. Phys. 2015, 61, e81–e87. [Google Scholar]
- Griswold, K.S. Refugee health and medical student training. Fam. Med. 2003, 35, 649–654. [Google Scholar] [PubMed]
- Mohamed-Ahmed, R.; Daniels, A.; Goodall, J.; O’kelly, E.; Fisher, J. “Disaster day”: Global health simulation teaching. Clin. Teach. 2016, 13, 18–22. [Google Scholar] [CrossRef]
- Denkinger, J.K.; Windthorst, P.; Rometsch-Ogioun El Sount, C.; Blume, M.; Sedik, H.; Kizilhan, J.İ.; Gibbons, N.; Pham, P.; Hillebrecht, J.; Ateia, N. Prevalence and determinants of secondary traumatization in caregivers working with women and children who suffered extreme violence by the “islamic state”. Front. Psychiatry 2018, 9, 234. [Google Scholar] [CrossRef]
- Kindermann, D.; Schmid, C.; Derreza-Greeven, C.; Huhn, D.; Kohl, R.M.; Junne, F.; Schleyer, M.; Daniels, J.K.; Ditzen, B.; Herzog, W. Prevalence of and risk factors for secondary traumatization in interpreters for refugees: A cross-sectional study. Psychopathology 2017, 50, 262–272. [Google Scholar] [CrossRef]
- Figley, C. Compassion Fatigue as Secondary Traumatic Stress Disorder, Compas-Sion Fatigue; Brunner/Mazel: New York, NY, USA, 1995. [Google Scholar]
- Figley, C. Traumatic Stress and the Role of the Family and Social Support System; Serco Marketing: Middlesex, UK, 1983. [Google Scholar]
- McCann, I.L.; Pearlman, L.A. Vicarious traumatization: A framework for understanding the psychological effects of working with victims. J. Trauma. Stress 1990, 3, 131–149. [Google Scholar] [CrossRef]
- Baird, K.; Kracen, A.C. Vicarious traumatization and secondary traumatic stress: A research synthesis. Couns. Psychol. Q. 2006, 19, 181–188. [Google Scholar] [CrossRef]
- Pearlman, L.A.; Saakvitne, K.W. Treating therapists with vicarious traumatization and secondary traumatic stress disorders. Compass. Fatigue Coping Second. Trauma. Stress Disord. Those Who Treat Traumatized 1995, 23, 150–177. [Google Scholar]
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research; Sage publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Creswell, J.W.; Plano Clark, V.L.; Gutmann, M.L.; Hanson, W.E. Advanced mixed methods research designs. Handb. Mix. Methods Soc. Behav. Res. 2003, 209, 240. [Google Scholar]
- Nikendei, C.; Weyrich, P.; Jünger, J.; Schrauth, M. Medical education in Germany. Med. Teach. 2009, 31, 591–600. [Google Scholar] [CrossRef]
- Nikendei, C.; Huhn, D.; Adler, G.; von Rose, P.B.; Eckstein, T.M.; Fuchs, B.; Gewalt, S.C.; Greiner, B.; Günther, T.; Herzog, W. Development and implementation of an outpatient clinic at an initial reception centre for asylum seekers in the german federal state of Baden-Wuerttemberg. Z. Evid. Fortbild. Qual. Gesundheitswes. 2017, 126, 31–42. [Google Scholar] [CrossRef]
- Association, W.M. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191. [Google Scholar]
- Flick, U. Qualitative Research in Psychology: A Textbook; Sage: London, UK, 2002. [Google Scholar]
- Helfferich, C. Qualität Qualitativer Daten – Manual zur Durchführung Qualitativer Einzelinterviews; VS-Verlag: Wiesbaden, Germany, 2005. (In German) [Google Scholar]
- Hill, C.E.; Knox, S.; Thompson, B.J.; Williams, E.N.; Hess, S.A.; Ladany, N. Consensual qualitative research: An update. J. Couns. Psychol. 2005, 52, 196–205. [Google Scholar] [CrossRef]
- Knox, S.; Burkard, A.W. Qualitative research interviews. Psychother. Res. 2009, 19, 566–575. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (coreq): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Mayring, P. Qualitative Inhaltsanalyse. Grundlagen und Techniken, 7th ed.; Deutscher Studien Verlag: Weinheim, Germany, 2000. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Kuckartz, U. Maxqda: Qualitative Data Analysis; Berlin VERBI Software: Berlin, Germany, 2007. [Google Scholar]
- Gibbs, G.R. Analysing Qualitative Data; Sage: London, UK, 2008. [Google Scholar]
- Bloom, B.S. Taxonomy of Educational Objectives. Vol. 1: Cognitive Domain; N. Y. McKay, 1956; pp. 20–24. [Google Scholar]
- Krathwohl, D.R. A revision of bloom’s taxonomy: An overview. Theory Pract. 2002, 41, 212–218. [Google Scholar] [CrossRef]
- Frank, J.R. The Canmeds 2005 Physician Competency Framework. Available online: http://rcpsc.medical.org/canmeds/CanMEDS2005/CanMEDS2005_e.pdf (accessed on 1 January 2005).
- Kroenke, K.; Spitzer, R.L. The phq-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of prime-md: The phq primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (phq-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Löwe, B.; Spitzer, R.L.; Gräfe, K.; Kroenke, K.; Quenter, A.; Zipfel, S.; Buchholz, C.; Witte, S.; Herzog, W. Comparative validity of three screening questionnaires for dsm-iv depressive disorders and physicians’ diagnoses. J. Affect. Disord. 2004, 78, 131–140. [Google Scholar] [CrossRef]
- Löwe, B.; Gräfe, K.; Zipfel, S.; Witte, S.; Loerch, B.; Herzog, W. Diagnosing icd-10 depressive episodes: Superior criterion validity of the patient health questionnaire. Psychother. Psychosom. 2004, 73, 386–390. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The gad-7. Arch. Int. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Int. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The mos 36-item short-form health survey (sf-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Brazier, J.E.; Harper, R.; Jones, N.; O’cathain, A.; Thomas, K.; Usherwood, T.; Westlake, L. Validating the sf-36 health survey questionnaire: New outcome measure for primary care. BMJ 1992, 305, 160–164. [Google Scholar] [CrossRef]
- Ellert, U.; Bellach, B. The sf-36 in the federal health survey--description of a current normal sample. Gesundheitswesen 1999, 61, S184–S190. [Google Scholar]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. Cross-validation of item selection and scoring for the sf-12 health survey in nine countries: Results from the iqola project. International quality of life assessment. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef]
- Daniels, J. Sekundäre traumatisierung. Psychotherapeut 2008, 53, 100–107. (in German). [Google Scholar] [CrossRef]
- Weitkamp, K.; Daniels, J.K.; Klasen, F. Psychometric properties of the questionnaire for secondary traumatization. Eur. J. Psychotraumatol. 2014, 5, 21875. [Google Scholar] [CrossRef]
- Bugaj, T.J.; Müksch, C.; Ehrenthal, J.C.; Köhl-Hackert, N.; Schauenburg, H.; Huber, J.; Schmid, C.; Erschens, R.; Junne, F.; Herzog, W. Stresserleben bei medizinstudierenden: Welche rolle spielen bindungserleben und persönlichkeitsaspekte? Psychother. Psychosom. Med. Psychol. 2016, 66, 88–92. [Google Scholar] [CrossRef]
- Khan, M.S.; Osei-Kofi, A.; Omar, A.; Kirkbride, H.; Kessel, A.; Abbara, A.; Heymann, D.; Zumla, A.; Dar, O. Pathogens, prejudice, and politics: The role of the global health community in the European refugee crisis. Lancet Infect. Dis. 2016, 16, e173–e177. [Google Scholar] [CrossRef]
- Hargreaves, S.; Lönnroth, K.; Nellums, L.B.; Olaru, I.D.; Nathavitharana, R.R.; Norredam, M.; Friedland, J.S. Multidrug-resistant tuberculosis and migration to Europe. Clin. Microbiol. Infect. 2017, 23, 141–146. [Google Scholar] [CrossRef]
- Kamper-Jørgensen, Z.; Andersen, A.B.; Kok-Jensen, A.; Kamper-Jørgensen, M.; Bygbjerg, I.C.; Andersen, P.H.; Thomsen, V.Ø.; Lillebaek, T. Migrant tuberculosis: The extent of transmission in a low burden country. BMC Infect. Dis. 2012, 12, 60. [Google Scholar] [CrossRef]
- Sexton, L. Vicarious traumatisation of counsellors and effects on their workplaces. Br. J. Guid. Couns. 1999, 27, 393–403. [Google Scholar] [CrossRef]
- Krans, J.; Näring, G.; Holmes, E.A.; Becker, E.S. “I see what you’re saying”: Intrusive images from listening to a traumatic verbal report. J. Anxiety Disord. 2010, 24, 134–140. [Google Scholar] [CrossRef]
- Canfield, J. Secondary traumatization, burnout, and vicarious traumatization: A review of the literature as it relates to therapists who treat trauma. Smith Coll. Stud. Soc. Work 2005, 75, 81–101. [Google Scholar] [CrossRef]
- Schauer, M.; Neuner, F.; Karunakara, U.; Klaschik, C.; Robert, C.; Elbert, T. Ptsd and the building block effect of psychological trauma among West Nile Africans. Eur. Soc. Trauma. Stress Stud. Bull. 2003, 10, 5–6. [Google Scholar]
- Rief, W.; Nanke, A.; Klaiberg, A.; Braehler, E. Base rates for panic and depression according to the brief patient health questionnaire: A population-based study. J. Affect. Disord. 2004, 82, 271–276. [Google Scholar] [CrossRef]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the generalized anxiety disorder screener (gad-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Fabrega, H., Jr. Psychiatric stigma in non-western societies. Compr. Psychiatry 1991, 32, 534–551. [Google Scholar] [CrossRef]
- El Sount, C.R.-O.; Windthorst, P.; Denkinger, J.; Ziser, K.; Nikendei, C.; Kindermann, D.; Ringwald, J.; Renner, V.; Zipfel, S.; Junne, F. Chronic pain in refugees with posttraumatic stress disorder (ptsd): A systematic review on patients’ characteristics and specific interventions. J. Psychosom. Res. 2018, 118, 83–97. [Google Scholar] [CrossRef]
- Maercker, A.; Horn, A.B. A socio-interpersonal perspective on ptsd: The case for environments and interpersonal processes. Clin. Psychol. Psychother. 2013, 20, 465–481. [Google Scholar] [CrossRef]
- Jayawickreme, N.; Jayawickreme, E.; Foa, E.B. Using the Individualism-Collectivism Construct to Understand Cultural Differences in PTSD; Nova Science Publishers: Hauppauge, NY, USA, 2013. [Google Scholar]
- Griswold, K.; Zayas, L.E.; Kernan, J.B.; Wagner, C.M. Cultural awareness through medical student and refugee patient encounters. J. Immigr. Minor. Health 2007, 9, 55–60. [Google Scholar] [CrossRef]
- Godkin, M.A.; Savageau, J.A. The effect of a global multiculturalism track on cultural competence of preclinical medical students. Fam. Med. 2001, 33, 178–186. [Google Scholar]
| Measure | |
| Age (M ± SD) | 24.9 ± 2.6 |
| Gender | |
| Female | 11 (50.0%) |
| Male | 11 (50.0%) |
| Number of semesters already completed (M ± SD) | 9.1 ± 2.0 |
| Nationality | |
| Germany | 18 (81.8%) |
| Turkey | 2 (9.1%) |
| Russia | 1 (4.5%) |
| Austria | 1 (4.5%) |
| Prior medical clerkships | 17 (77.3%) |
| Medical specialization of prior medical clerkships (multiple answers possible) | |
| Surgery | 11 (64.7%) |
| Radiology | 7 (41.2%) |
| Psychiatry | 6 (35.3%) |
| Internal Medicine | 5 (29.4%) |
| Prior education | 7 (31.8%) |
| Special field of prior education (multiple answers possible) | |
| Nursing | 2 (28.6%) |
| Emergency rescue service | 2 (28.6%) |
| Molecular biology | 1 (14.3%) |
| Chemistry | 1 (14.3%) |
| Dentistry | 1 (14.3%) |
| Aspired medical profession (multiple answers possible) | |
| Psychiatry | 6 (27.2%) |
| Neurology | 5 (22.7%) |
| Pediatrics | 4 (18.2%) |
| Surgery | 3 (13.6%) |
| Oncology | 3 (13.6%) |
| Prior voluntary service | 17 (77.3%) |
| Prior journeys to developing countries | 11 (50.0%) |
| Measure | |
|---|---|
| Learning highlights | 125 (Missing: 54) |
| General medicine | 106 (84.8%) |
| Psychosocial medicine | 9 (7.2%) |
| Pediatrics | 5 (4.0%) |
| Gynecology | 5 (4.0%) |
| Age of patient (M ± SD) | 31.4 (±11,3) |
| Patient’s gender | 121 (Missing: 58) |
| Female Male | 43 (35.5%) 78 (64.5%) |
| Patient’s nationality | 109 (Missing: 70) |
| Nigeria | 23 (21.1%) |
| The Gambia | 19 (17.4%) |
| Syria | 10 (9.1%) |
| Somalia | 7 (6.4%) |
| Eritrea | 6 (5.5%) |
| Albania | 6 (5.5%) |
| Georgia | 5 (4.5%) |
| Macedonia | 4 (3.6%) |
| Algeria | 3 (2.7%) |
| Iraq | 3 (2.7%) |
| Russia | 3 (2.7%) |
| India | 3 (2.7%) |
| Afghanistan | 2 (1.8%) |
| Tunisia | 2 (1.8%) |
| Turkey | 2 (1.8%) |
| Serbia | 2 (1.8%) |
| Togo | 2 (1.8%) |
| Guinea | 2 (1.8%) |
| Armenia | 1 (0.9%) |
| Bosnia | 1 (0.9%) |
| Iran | 1 (0.9%) |
| Cameroon | 1 (0.9%) |
| Kenya | 1 (0.9%) |
| Student´s function (Multiple answers possible) | 124 (Missing: 55) |
| Observing | 55 (44.4%) |
| Assisting | 67 (54.0%) |
| Independent work | 33 (26.6%) |
| Student’s practical involvement (Multiple answers possible) | 117 (Missing: 62) |
| Communicating | 92 (78.6%) |
| Hands-on | 55 (47.0%) |
| Psychological Assessment—Descriptive Statistics and Comparison of T2 with Norm Sample | |||||||
|---|---|---|---|---|---|---|---|
| Instrument | T1 | T2 | Norm Sample | Significance | |||
| Mean (SD) | Mean (SD) | Mean (SD) | n | t | df | p | |
| FST [31–155] | - | 40.81 (6.31) | 38.52 (7.91) A | 62 | 1.225 | 62 | 0.224 |
| PHQ-9 [0–21] | 2.31 (3.14) | 2.59 (1.97) | 6.03 (4.19) B | 290 | 3.804 | 310 | <0.001 |
| GAD-7 [0–21] | 2.77 (2.00) | 2.70 (1.73) | 5.34 (4.24) B | 290 | 2.897 | 309 | 0.004 |
| SF-12 [0–100] | |||||||
| Physical health score | 56.45 (3.07) | 55.85 (2.32) | 55.06 (5.08) B | 290 | 0.723 | 310 | 0.470 |
| Mental health score | 50.88 (8.78) | 52.94 (4.78) | 45.33 (10.33) B | 290 | 3.424 | 310 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kindermann, D.; Schmid, C.; Derreza-Greeven, C.; Junne, F.; Friederich, H.-C.; Nikendei, C. Medical Clerkship in a State Registration and Reception Center for Forced Migrants in Germany: Students’ Experiences, Teachable Moments, and Psychological Burden. Int. J. Environ. Res. Public Health 2019, 16, 1704. https://doi.org/10.3390/ijerph16101704
Kindermann D, Schmid C, Derreza-Greeven C, Junne F, Friederich H-C, Nikendei C. Medical Clerkship in a State Registration and Reception Center for Forced Migrants in Germany: Students’ Experiences, Teachable Moments, and Psychological Burden. International Journal of Environmental Research and Public Health. 2019; 16(10):1704. https://doi.org/10.3390/ijerph16101704
Chicago/Turabian StyleKindermann, David, Carolin Schmid, Cassandra Derreza-Greeven, Florian Junne, Hans-Christoph Friederich, and Christoph Nikendei. 2019. "Medical Clerkship in a State Registration and Reception Center for Forced Migrants in Germany: Students’ Experiences, Teachable Moments, and Psychological Burden" International Journal of Environmental Research and Public Health 16, no. 10: 1704. https://doi.org/10.3390/ijerph16101704
APA StyleKindermann, D., Schmid, C., Derreza-Greeven, C., Junne, F., Friederich, H.-C., & Nikendei, C. (2019). Medical Clerkship in a State Registration and Reception Center for Forced Migrants in Germany: Students’ Experiences, Teachable Moments, and Psychological Burden. International Journal of Environmental Research and Public Health, 16(10), 1704. https://doi.org/10.3390/ijerph16101704





