Road Traffic Noise, Air Pollutants, and the Prevalence of Cardiovascular Disease in Taichung, Taiwan
Abstract
1. Introduction
2. Materials and Methods
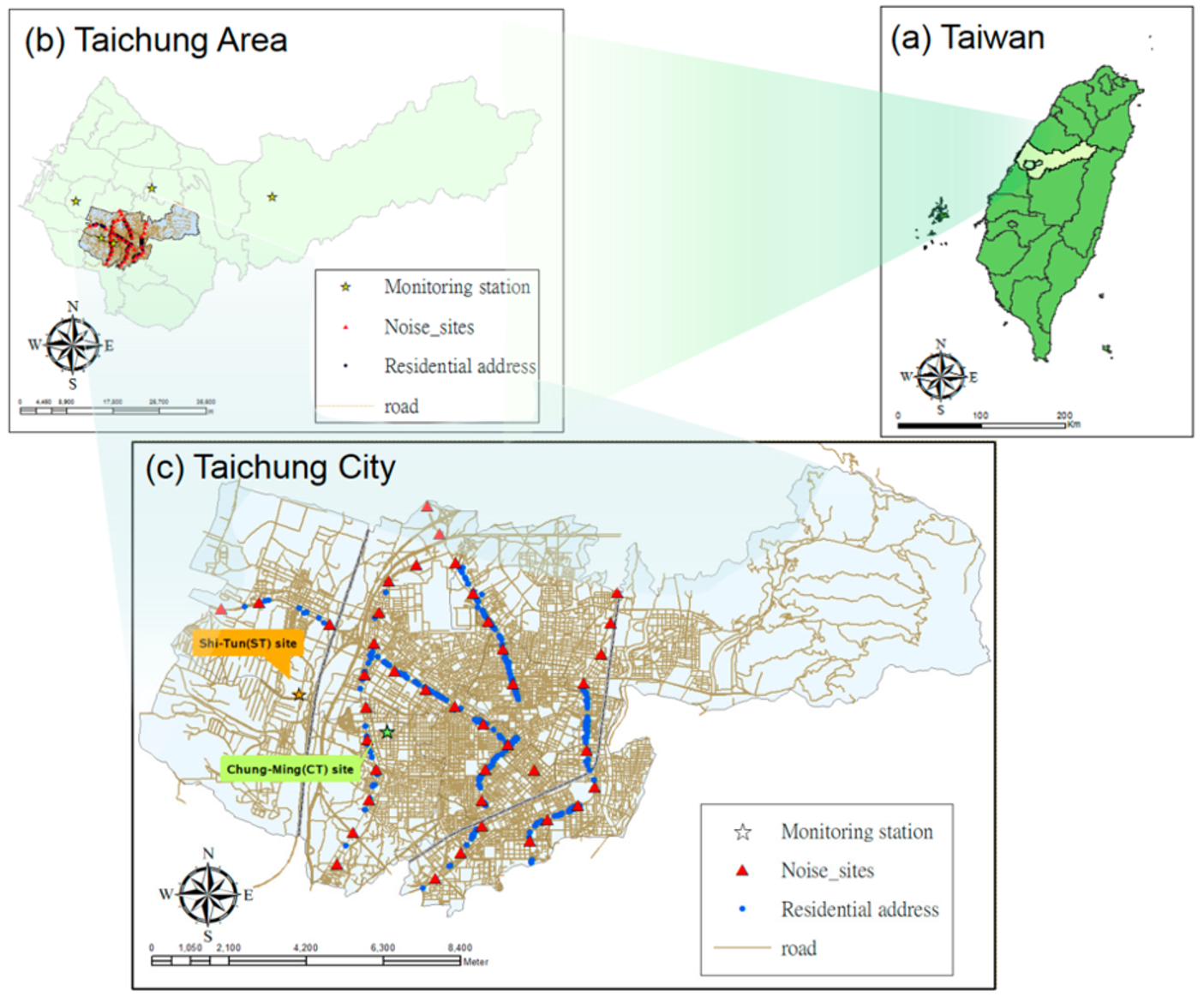
2.1. Study Areas and Population
2.2. Questionnaire and Definition of Cardiovascular Disease
2.3. Road Traffic Noise Measurements and Traffic Calculations
2.4. Air Pollutants Monitoring Levels
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and non-auditory effects of noise on health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- Munzel, T.; Gori, T.; Babisch, W.; Basner, M. Cardiovascular effects of environmental noise exposure. Eur. Heart J. 2014, 35, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Van Kempen, E.; Babisch, W. The quantitative relationship between road traffic noise and hypertension: A meta-analysis. J. Hypertens. 2012, 30, 1075–1086. [Google Scholar] [CrossRef] [PubMed]
- Vienneau, D.; Schindler, C.; Perez, L.; Probst-Hensch, N.; Roosli, M. The relationship between transportation noise exposure and ischemic heart disease: A meta-analysis. Environ. Res. 2015, 138, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.; Zhang, B.; Zhao, X.; Ruan, Y.; Lian, H.; Fan, Z. Effect of exposure to PM2.5 on blood pressure: A systematic review and meta-analysis. J. Hypertens. 2014, 32, 2130–2140, discussion 2141. [Google Scholar] [CrossRef] [PubMed]
- Scheers, H.; Jacobs, L.; Casas, L.; Nemery, B.; Nawrot, T.S. Long-term exposure to particulate matter air pollution is a risk factor for stroke: Meta-analytical evidence. Stroke 2015, 46, 3058–3066. [Google Scholar] [CrossRef] [PubMed]
- Mannsaker, B.; Vikan, T.; Holme, J. Air pollution and cardiovascular disease in Trondheim. Tidsskr. Nor. Laegeforen. 2004, 124, 1381–1383. [Google Scholar] [PubMed]
- Liu, Y.; Chen, X.; Huang, S.; Tian, L.; Lu, Y.; Mei, Y.; Ren, M.; Li, N.; Liu, L.; Xiang, H. Association between air pollutants and cardiovascular disease mortality in Wuhan, China. Int. J. Environ. Res. Public Health 2015, 12, 3506–3516. [Google Scholar] [CrossRef] [PubMed]
- Beelen, R.; Hoek, G.; Houthuijs, D.; van den Brandt, P.A.; Goldbohm, R.A.; Fischer, P.; Schouten, L.J.; Armstrong, B.; Brunekreef, B. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup. Environ. Med. 2009, 66, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Floud, S.; Blangiardo, M.; Clark, C.; de Hoogh, K.; Babisch, W.; Houthuijs, D.; Swart, W.; Pershagen, G.; Katsouyanni, K.; Velonakis, M; et al. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: A cross-sectional study. Environ. Health Glob. Access Sci. Source 2013, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Recio, A.; Linares, C.; Banegas, J.R.; Diaz, J. The short-term association of road traffic noise with cardiovascular, respiratory, and diabetes-related mortality. Environ. Res. 2016, 150, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.Y.; Liu, C.S.; Bao, B.Y.; Li, S.F.; Chen, T.I.; Lin, Y.J. Characterization of road traffic noise exposure and prevalence of hypertension in central Taiwan. Sci. Total Environ. 2011, 409, 1053–1057. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.Y.; Beelen, R.; Li, S.F.; Chen, T.I.; Lin, Y.J.; Bao, B.Y.; Liu, C.S. Road traffic noise frequency and prevalent hypertension in Taichung, Taiwan: A cross-sectional study. Environ. Health Glob. Access Sci. Source 2014, 13, 37. [Google Scholar] [CrossRef] [PubMed]
- Hwang, B.F.; Lee, Y.L.; Jaakkola, J.J. Air pollution and stillbirth: A population-based case-control study in Taiwan. Environ. Health Perspect. 2011, 119, 1345–1349. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. In Global Update 2005—Summary of Risk Assessment; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Taiwan Environmental Protection Administration. Air Quality Standards; Taiwan Environmental Protection Administration: Taipe, Taiwan, 2012. [Google Scholar]
- Wilkins, J.T.; Ning, H.; Berry, J.; Zhao, L.; Dyer, A.R.; Lloyd-Jones, D.M. Lifetime risk and years lived free of total cardiovascular disease. JAMA 2012, 308, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Nation Heart, Lung, and Blood Institute. What Are the Risk Factors for Heart Disease? Available online: https://www.nhlbi.nih.gov/health/educational/hearttruth/lower-risk/risk-factors.htm (accessed on 26 July 2018).
- World Heart Federation. Risk Factors. Available online: https://www.world-heart-federation.org/resources/risk-factors/ (accessed on 26 July 2018).
- Meurer, W.J.; Tolles, J. Logistic regression diagnostics: Understanding how well a model predicts outcomes. JAMA 2017, 317, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Aguilera, I.; Foraster, M.; Basagana, X.; Corradi, E.; Deltell, A.; Morelli, X.; Phuleria, H.C.; Ragettli, M.S.; Rivera, M.; Thomasson, A.; et al. Application of land use regression modelling to assess the spatial distribution of road traffic noise in three European cities. J. Expo. Sci. Environ. Epidemiol. 2015, 25, 97–105. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for Community Noise; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Lee, E.Y.; Jerrett, M.; Ross, Z.; Coogan, P.F.; Seto, E.Y.W. Assessment of traffic-related noise in three cities in the United States. Environ. Res. 2014, 132, 182–189. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Male | Female | Total | p-Value |
|---|---|---|---|---|
| No. of subjects | 256 | 407 | 663 | |
| Age [(years (mean ± SD)] a | 42.4 (23.0) | 45.9 (26.7) | 44.5 (25.4) | 0.3710 |
| BMI [(kg/m2(mean ± SD)] a | 23.7 (3.7) | 21.7 (3.6) | 22.5 (3.8) | <0.0001 |
| Smoking [no. (%)] b | <0.0001 | |||
| Yes (%) | 102 (39.8) | 41 (10.1) | 143 (21.6) | |
| No (%) | 154 (60.2) | 366 (89.9) | 520 (78.4) | |
| Alcohol drinking [no. (%)] b | <0.0001 | |||
| Yes (%) | 51 (19.9) | 18 (4.4) | 69 (10.4) | |
| No (%) | 205 (80.1) | 389 (95.6) | 594 (89.6) | |
| Tea consumption [no. (%)] b | 0.4774 | |||
| Yes (%) | 161 (62.9) | 267 (65.6) | 428 (64.6) | |
| No (%) | 95 (37.1) | 140 (34.4) | 235 (35.4) | |
| Coffee consumption [no. (%)] b | 0.0697 | |||
| Yes (%) | 84 (32.8) | 162 (39.8) | 246 (37.1) | |
| No (%) | 172 (67.2) | 245 (60.2) | 417 (62.9) | |
| Salt intake [no. (%)] b | 0.0309 | |||
| High (%) | 75 (29.3) | 89 (21.9) | 164 (24.7) | |
| Low (%) | 181 (70.7) | 318 (78.1) | 499 (75.3) | |
| Regular exercise [no. (%)] b | <0.0001 | |||
| Yes (%) | 147 (57.4) | 166 (40.8) | 313 (47.2) | |
| No (%) | 109 (42.6) | 241 (59.2) | 350 (52.8) | |
| Family history of hypertension [no. (%)] b | 0.2861 | |||
| Yes (%) | 76 (29.7) | 137 (33.7) | 213 (32.1) | |
| No (%) | 180 (70.3) | 270 (66.3) | 450 (67.9) | |
| Male | Female | Total | p-Value | |
|---|---|---|---|---|
| No. of subjects | 256 | 407 | 663 | |
| LAeq,8h (dBA) a | 0.7422 | |||
| Mean (SD) | 79.5 (3.3) | 79.4 (3.1) | 79.4 (3.2) | |
| Range | 73.9–85.4 | 73.9–85.4 | 73.9–85.4 | |
| Total traffic (vehicle/day) a | 0.7842 | |||
| Mean (SD) | 434 (221) | 442 (200) | 438 (208) | |
| Range | 82–794 | 82–794 | 82–794 | |
| PM10 (µg/m3) a | 0.0898 | |||
| Mean (SD) | 58.4 (0.3) | 58.3 (0.3) | 58.3 (0.3) | |
| Range | 57.6–59.3 | 57.6–59.3 | 57.6–59.3 | |
| NO2 (ppb) a | 0.0898 | |||
| Mean (SD) | 20.2 (0.4) | 20.3 (0.3) | 20.2 (0.3) | |
| Range | 19.2–21.1 | 19.1–21.1 | 19.1–21.1 | |
| PM10 (μg/m3) | NO2 (ppb) | Total Traffic (vehicle/day) | |
|---|---|---|---|
| LAeq,8h (dBA) | 0.068 | −0.068 | 0.593 |
| p-value | 0.0789 | 0.0789 | <0.0001 |
| CVD Case [no. (%)] | Crude OR (95% CI) a | Adjusted OR (95% CI) b | |
|---|---|---|---|
| Model 1 | |||
| High-exposure (noise level ≥ 80 dBA, n = 313) | 27 (8.63) | 1.65 (0.90–3.02) | 1.95 (0.99–3.85) |
| Low-exposure (noise level < 80 dBA, n = 350) | 19 (5.43) | 1.00 | 1.00 |
| Model 2 | |||
| High-exposure (PM10 level ≥ 58 μg/m3, n = 331) | 22 (6.65) | 0.91 (0.50–1.66) | 0.94 (0.49–1.81) |
| Low-exposure (PM10 level < 58 μg/m3, n = 332) | 24 (7.23) | 1.00 | 1.00 |
| Model 3 | |||
| High-exposure (NO2 level ≥ 20 ppb, n = 334) | 24 (7.29) | 1.12 (0.61–2.03) | 1.08 (0.56–2.08) |
| Low-exposure (NO2 level < 20 ppb, n = 329) | 22 (6.59) | 1.00 | 1.00 |
| Number | CVD Case [no. (%)] | Crude OR (95% CI) a | Adjusted OR (95% CI) b | |
|---|---|---|---|---|
| Model 1: | ||||
| Noise ≥ 80 dBA and PM10 ≥ 58 μg/m3 | 140 | 10 (7.14) | 1.67 (0.62–4.51) | 2.20 (0.73–6.62) |
| Noise ≥ 80 dBA and PM10 < 58 μg/m3 | 173 | 17 (9.83) | 2.37 (0.95–5.87) | 2.45 (0.88–6.82) |
| Noise < 80 dBA and PM10 ≥ 58 μg/m3 | 191 | 12 (6.28) | 1.46 (0.56–3.79) | 1.35 (0.47–3.87) |
| Noise < 80 dBA and PM10 < 58 μg/m3 | 159 | 7 (4.40) | 1.00 | 1.00 |
| Model 2: | ||||
| Noise ≥ 80 dBA and NO2 ≥ 20 ppb | 171 | 17 (9.94) | 1.66 (0.77–3.58) | 1.84 (0.79–4.31) |
| Noise ≥ 80 dBA and NO2 < 20 ppb | 142 | 10 (7.04) | 1.14 (0.48–2.71) | 1.60 (0.61–4.18) |
| Noise < 80 dBA and NO2 ≥ 20 ppb | 158 | 7 (4.43) | 0.70 (0.27–1.81) | 0.74 (0.26–2.12) |
| Noise < 80 dBA and NO2 < 20 ppb | 192 | 12 (6.25) | 1.00 | 1.00 |
| Crude OR (95% CI) a | Adjusted OR (95% CI) b | Adjusted OR (95% CI) b | Adjusted OR (95% CI) c | |
|---|---|---|---|---|
| Single-exposure models | ||||
| Per 5-dBA increase in noise | 1.64 (1.02–2.63) * | 2.23 (1.26–3.93) * | — | 2.97 (1.42–6.22) * |
| Per 1 μg/m3 increase in PM10 | 1.29 (0.49–3.38) | 1.26 (0.45–3.54) | — | 1.32 (0.46–3.78) |
| Per 1 ppb increase in NO2 | 0.80 (0.34–1.88) | 0.82 (0.33–2.04) | — | 0.78 (0.31–2.00) |
| Two-exposure model 1 | ||||
| Per 5-dBA increase in noise | — | 2.22 (1.26–3.93) * | 2.96 (1.41–6.23) * | |
| Per 1 μg/m3 increase in PM10 | — | 1.16 (0.40–3.38) | 1.04 (0.36–3.04) | |
| Two-exposure model 2 | ||||
| Per 5-dBA increase in noise | — | 2.22 (1.26–3.93) * | 2.96 (1.41–6.23) * | |
| Per 1 ppb increase in NO2 | — | 0.88 (0.34–2.26) | 0.96 (0.37–2.49) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, W.-T.; Wang, V.-S.; Chang, L.-T.; Chuang, K.-J.; Chuang, H.-C.; Liu, C.-S.; Bao, B.-Y.; Chang, T.-Y. Road Traffic Noise, Air Pollutants, and the Prevalence of Cardiovascular Disease in Taichung, Taiwan. Int. J. Environ. Res. Public Health 2018, 15, 1707. https://doi.org/10.3390/ijerph15081707
Yang W-T, Wang V-S, Chang L-T, Chuang K-J, Chuang H-C, Liu C-S, Bao B-Y, Chang T-Y. Road Traffic Noise, Air Pollutants, and the Prevalence of Cardiovascular Disease in Taichung, Taiwan. International Journal of Environmental Research and Public Health. 2018; 15(8):1707. https://doi.org/10.3390/ijerph15081707
Chicago/Turabian StyleYang, Wei-Ting, Ven-Shing Wang, Li-Te Chang, Kai-Jen Chuang, Hsiao-Chi Chuang, Chiu-Shong Liu, Bo-Ying Bao, and Ta-Yuan Chang. 2018. "Road Traffic Noise, Air Pollutants, and the Prevalence of Cardiovascular Disease in Taichung, Taiwan" International Journal of Environmental Research and Public Health 15, no. 8: 1707. https://doi.org/10.3390/ijerph15081707
APA StyleYang, W.-T., Wang, V.-S., Chang, L.-T., Chuang, K.-J., Chuang, H.-C., Liu, C.-S., Bao, B.-Y., & Chang, T.-Y. (2018). Road Traffic Noise, Air Pollutants, and the Prevalence of Cardiovascular Disease in Taichung, Taiwan. International Journal of Environmental Research and Public Health, 15(8), 1707. https://doi.org/10.3390/ijerph15081707








