Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review
Abstract
1. Introduction
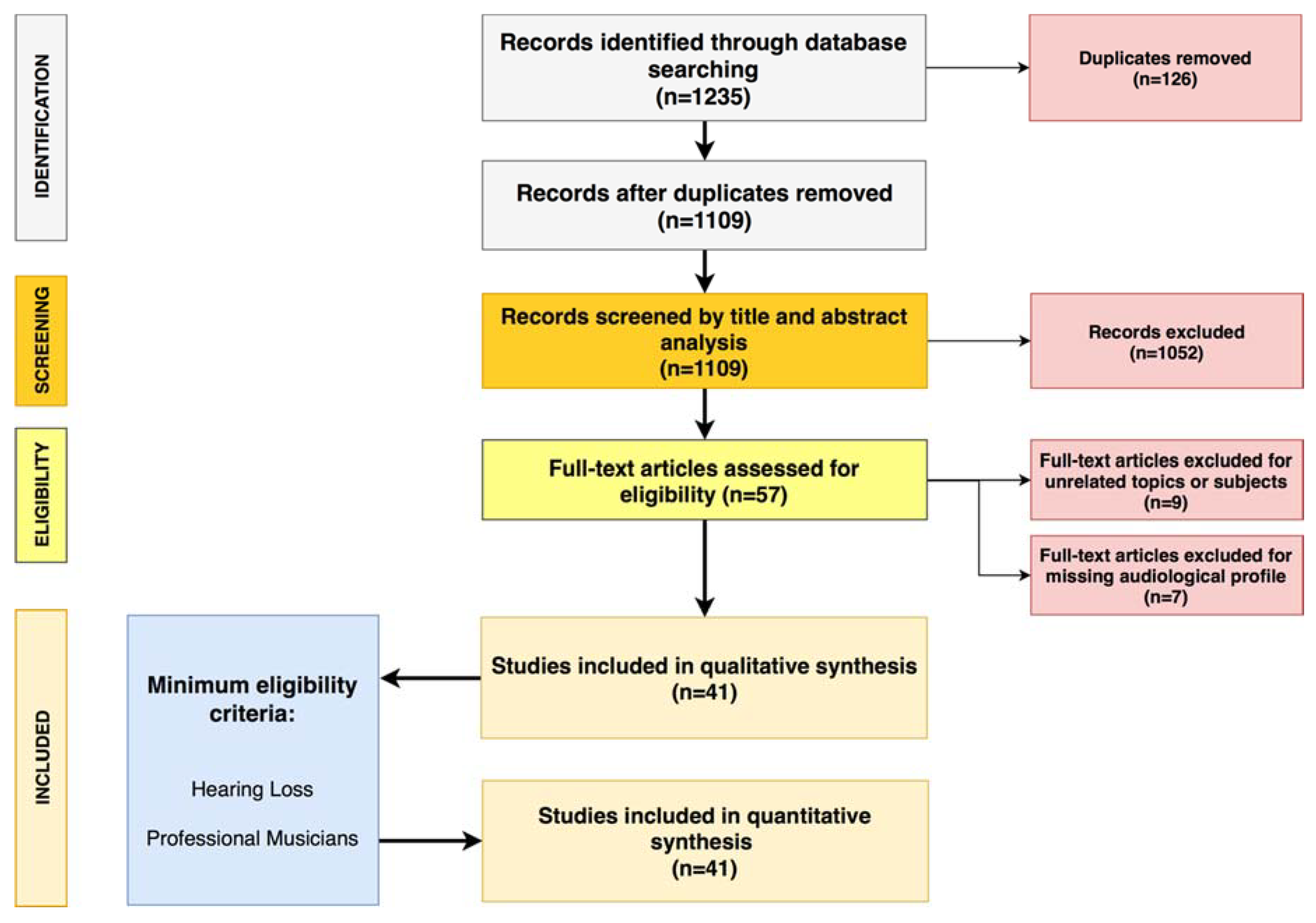
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Data Analysis
3. Results
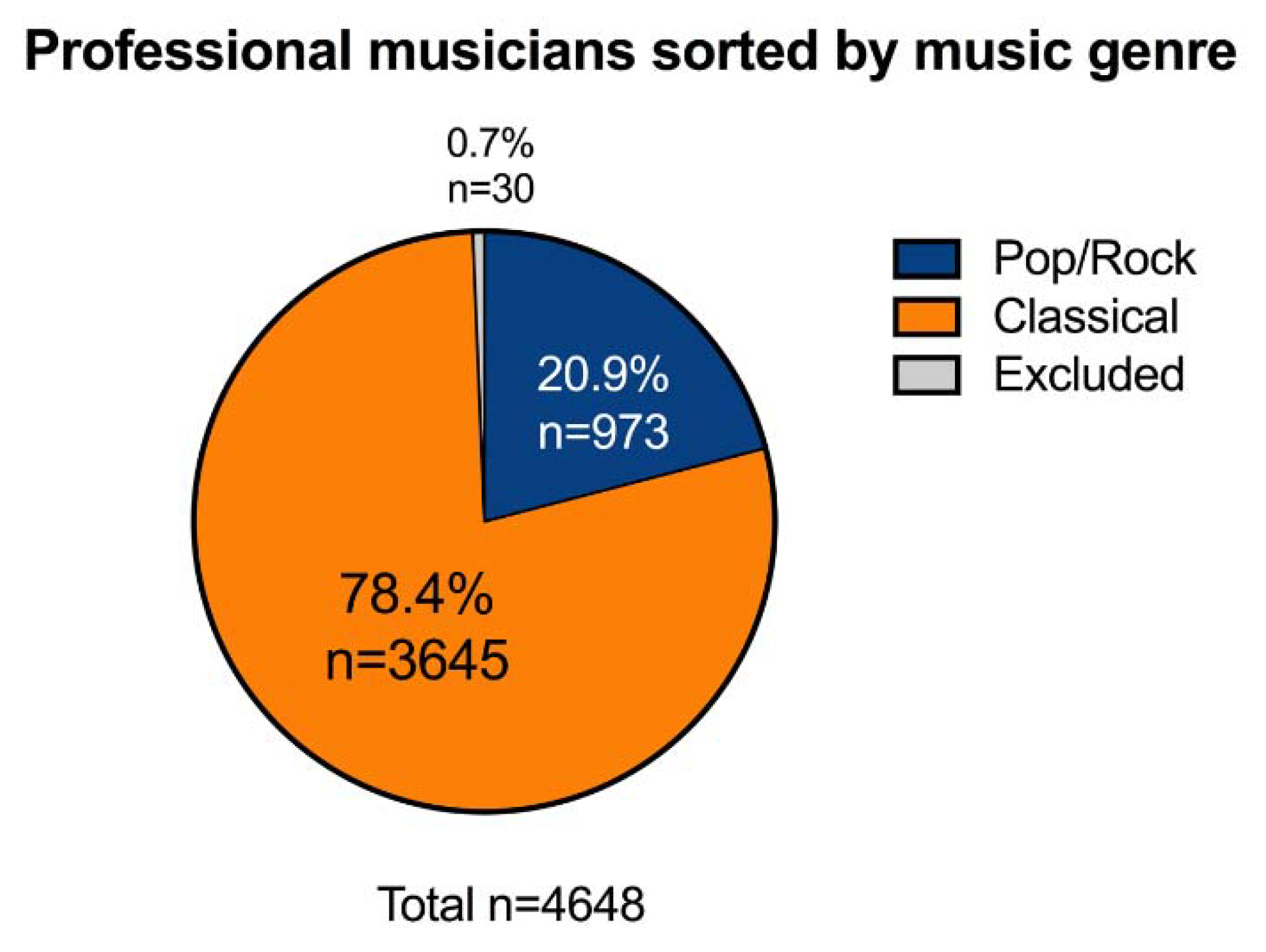
3.1. Articles and Subjects Included in the Systematic Review
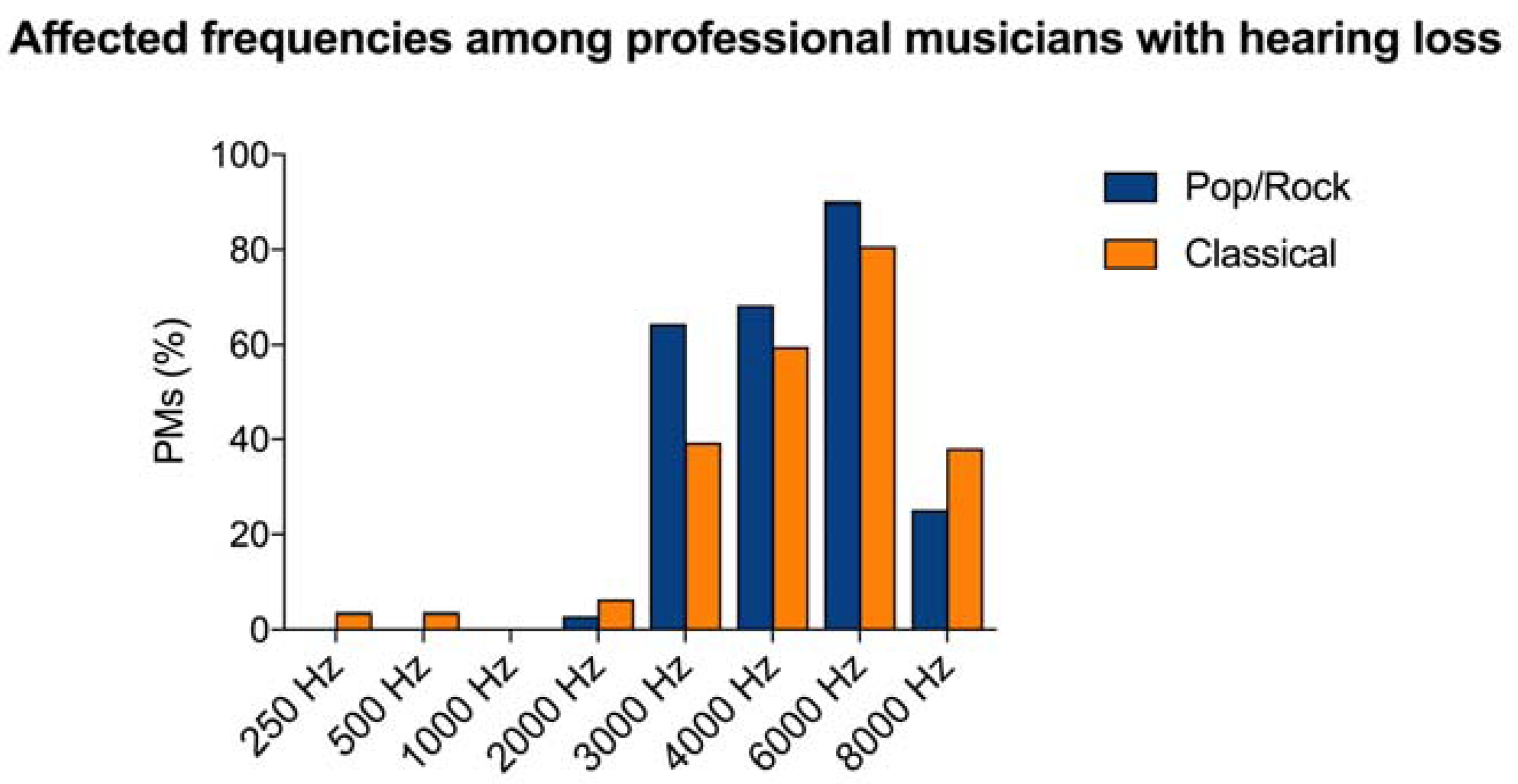
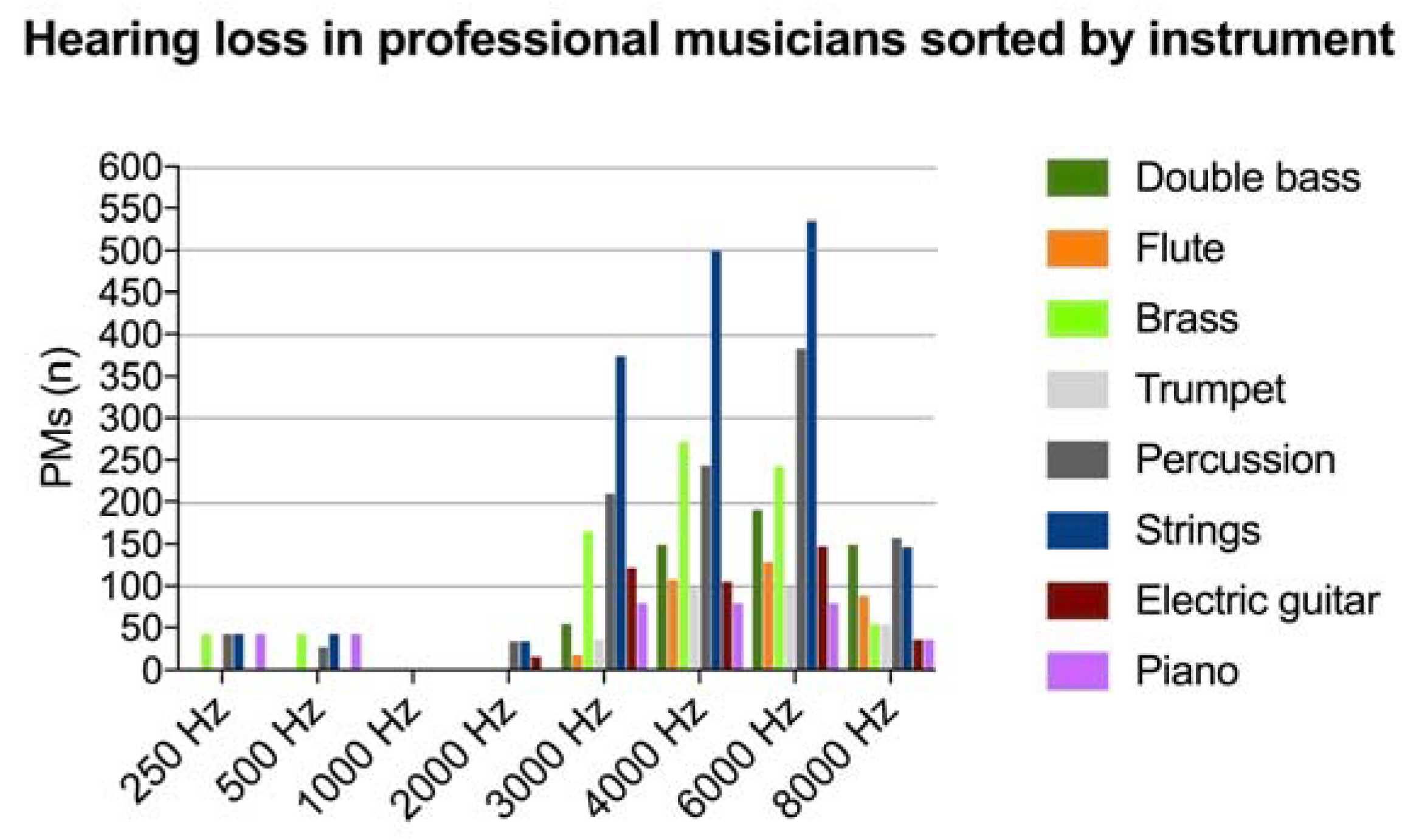
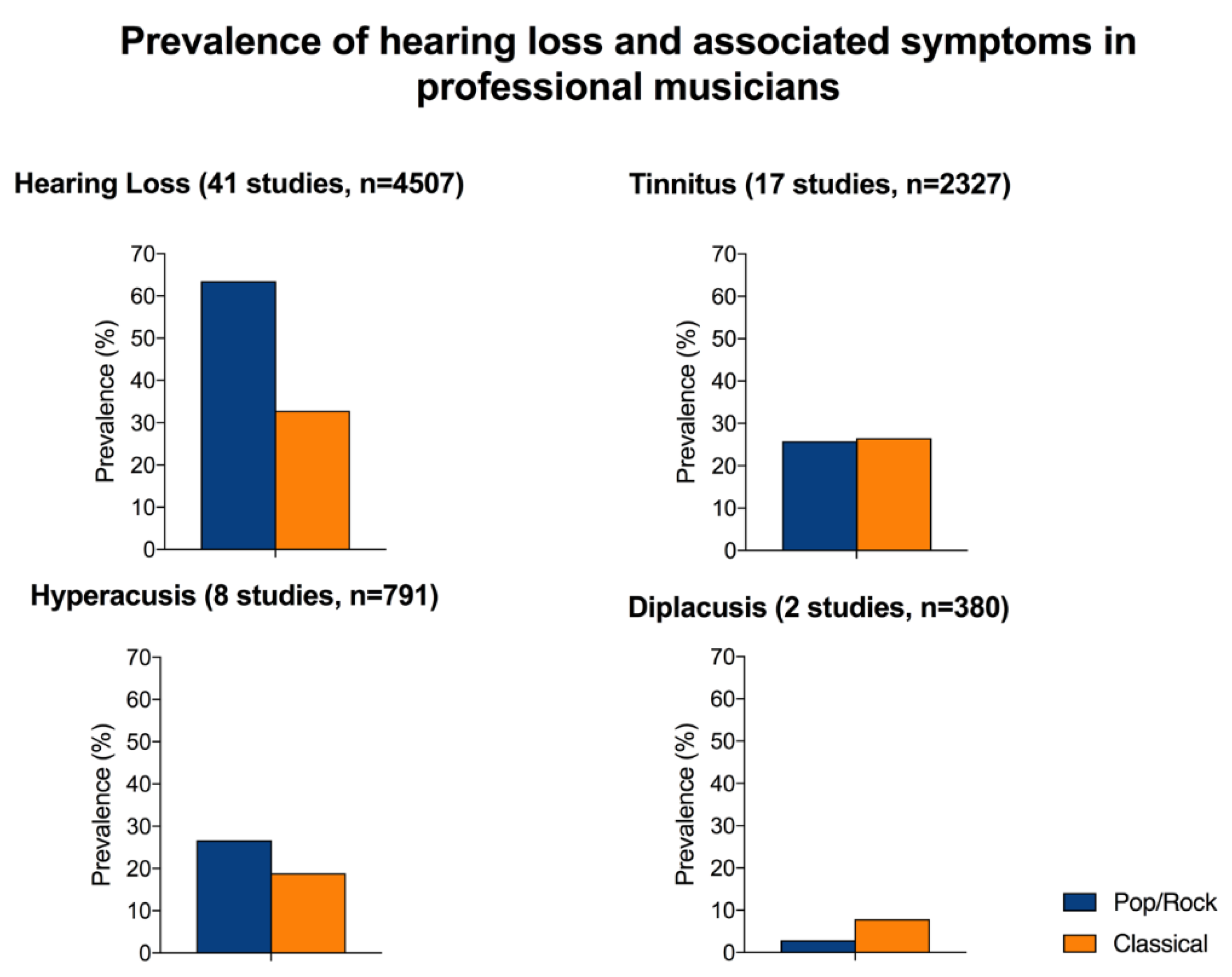
3.2. Hearing Loss and Audiological Symptoms
4. Discussion
4.1. Risk of Developing Hearing Loss Among PR and CL PMs
4.2. Characteristics of Hearing Loss Among PM
4.3. Audiological Symptoms: Tinnitus, Hyperacusis, and Diplacusis
4.4. Limits of Our Study
4.5. Future Perspectives for Early Diagnosis of Hearing Damage in Professional Musicians
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Nelson, D.I.; Nelson, R.Y.; Concha-Barrientos, M.; Fingerhut, M. The global burden of occupational noise-induced hearing loss. Am. J. Ind. Med. 2005, 48, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Tikka, C.; Verbeek, J.H.; Kateman, E.; Morata, T.C.; Dreschler, W.A.; Ferrite, S. Interventions to prevent occupational noise-induced hearing loss. Cochrane Database Syst. Rev. 2017, 7, CD006396. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.; Bielefeld, E.C.; Harris, K.C.; Hu, B.H. The role of oxidative stress in noise-induced hearing loss. Ear Hear. 2006, 27, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Fetoni, A.R.; Ralli, M.; Sergi, B.; Parrilla, C.; Troiani, D.; Paludetti, G. Protective properties of antioxidant drugs in noise-induced hearing loss in the guinea pig. Audiol. Med. 2009, 6, 271–277. [Google Scholar] [CrossRef]
- Fetoni, A.R.; Garzaro, M.; Ralli, M.; Landolfo, V.; Sensini, M.; Pecorari, G.; Mordente, A.; Paludetti, G.; Giordano, C. The monitoring role of otoacoustic emissions and oxidative stress markers in the protective effects of antioxidant administration in noise-exposed subjects: A pilot study. Med. Sci. Monit. 2009, 15, PR1–PR8. [Google Scholar]
- Sliwinska-Kowalska, M.; Zaborowski, K. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Permanent Hearing Loss and Tinnitus. Int. J. Environ. Res. Public Health 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- Masterson, E.A.; Bushnell, P.T.; Themann, C.L.; Morata, T.C. Hearing Impairment Among Noise-Exposed Workers—United States, 2003–2012. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Masterson, E.A.; Tak, S.; Themann, C.L.; Wall, D.K.; Groenewold, M.R.; Deddens, J.A.; Calvert, G.M. Prevalence of hearing loss in the United States by industry. Am. J. Ind. Med. 2013, 56, 670–681. [Google Scholar] [CrossRef] [PubMed]
- Ivory, R.; Kane, R.; Diaz, R.C. Noise-induced hearing loss: A recreational noise perspective. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Katbamna, B.; Flamme, G.A. Acquired hearing loss in adolescents. Pediatr. Clin. N. Am. 2008, 55, 1391–1402. [Google Scholar] [CrossRef] [PubMed]
- Seidman, M.D.; Standring, R.T. Noise and quality of life. Int. J. Environ. Res. Public Health 2010, 7, 3730–3738. [Google Scholar] [CrossRef] [PubMed]
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Engdahl, B.; Tambs, K. Occupational noise exposure and hearing: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [PubMed]
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef]
- Langguth, B.; Kreuzer, P.M.; Kleinjung, T.; De Ridder, D. Tinnitus: Causes and clinical management. Lancet Neurol. 2013, 12, 920–930. [Google Scholar] [CrossRef]
- Shargorodsky, J.; Curhan, G.C.; Farwell, W.R. Prevalence and characteristics of tinnitus among US adults. Am. J. Med. 2010, 123, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.; Smith, P.A.; Booth, M.; Martin, M. Diagnosing Patients with Age-Related Hearing Loss and Tinnitus: Supporting GP Clinical Engagement through Innovation and Pathway Redesign in Audiology Services. Int. J. Otolaryngol. 2012, 2012, 290291. [Google Scholar] [CrossRef] [PubMed]
- Mrena, R.; Savolainen, S.; Kuokkanen, J.T.; Ylikoski, J. Characteristics of tinnitus induced by acute acoustic trauma: A long-term follow-up. Audiol. Neurootol. 2002, 7, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Nageris, B.I.; Attias, J.; Raveh, E. Test-retest tinnitus characteristics in patients with noise-induced hearing loss. Am. J. Otolaryngol. 2010, 31, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Ricci, S.; Massoni, F.; Di Meo, M.; Petrone, L.; Canitano, N.; Ippoliti, F.; Cinti, M.E. Correlation among measures of stress, indicators of biohumoral nature and medico-legal considerations. Riv. Psichiatr. 2013, 48, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Balla, M.P.; Greco, A.; Altissimi, G.; Ricci, P.; Turchetta, R.; Virgilio, A.; Vincentiis, M.; Ricci, S.; Cianfrone, G. Work-Related Noise Exposure in a Cohort of Patients with Chronic Tinnitus: Analysis of Demographic and Audiological Characteristics. Int. J. Environ. Res. Public Health 2017, 14. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; McFerran, D.; Salvi, R.; Prasher, D.; Jastreboff, M.; Jastreboff, P. Insights from the First International Conference on Hyperacusis: Causes, evaluation, diagnosis and treatment. Noise Health 2014, 16, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Heller, A.J. Classification and epidemiology of tinnitus. Otolaryngol. Clin. N. Am. 2003, 36, 239–248. [Google Scholar] [CrossRef]
- Erlandsson, S.I.; Hallberg, L.R.; Axelsson, A. Psychological and audiological correlates of perceived tinnitus severity. Audiology 1992, 31, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Reiss, L.A.; Shayman, C.S.; Walker, E.P.; Bennett, K.O.; Fowler, J.R.; Hartling, C.L.; Glickman, B.; Lasarev, M.R.; Oh, Y. Binaural pitch fusion: Comparison of normal-hearing and hearing-impaired listeners. J. Acoust. Soc. Am. 2017, 141, 1909–1920. [Google Scholar] [CrossRef] [PubMed]
- Colin, D.; Micheyl, C.; Girod, A.; Truy, E.; Gallego, S. Binaural Diplacusis and Its Relationship with Hearing-Threshold Asymmetry. PLoS ONE 2016, 11, e0159975. [Google Scholar] [CrossRef] [PubMed]
- Clark, W.W. Noise exposure from leisure activities: A review. J. Acoust. Soc. Am. 1991, 90, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Di Stadio, A. Which factors to induce hearing loss in professional musicians? Extensive literature review and histopathology findings can answer it. Hear. Balance Commun. 2017, 15, 63–71. [Google Scholar] [CrossRef]
- Hoydal, E.H.; Lein Stormer, C.C.; Laukli, E.; Stenklev, N.C. Transient evoked otoacoustic emissions in rock musicians. Int. J. Audiol. 2017, 56, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Mendes, M.H.; Morata, T.C.; Marques, J.M. Acceptance of hearing protection aids in members of an instrumental and voice music band. Braz. J. Otorhinolaryngol. 2007, 73, 785–792. [Google Scholar] [CrossRef]
- Eaton, S.; Gillis, H. Review of orchestra musicians’ hearing loss risks. Can. Acoust. 2002, 2, 5–12. [Google Scholar]
- Halevi-Katz, D.N.; Yaakobi, E.; Putter-Katz, H. Exposure to music and noise-induced hearing loss (NIHL) among professional pop/rock/jazz musicians. Noise Health 2015, 17, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Lindgren, F. Hearing in pop musicians. Acta Otolaryngol. 1978, 85, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Lindgren, F. Hearing in classical musicians. Acta Otolaryngol. Suppl. 1981, 377, 3–74. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Lindgren, F. Pop music and hearing. Ear Hear. 1981, 2, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, K.; Lundquist, P.G.; Olaussen, T. The hearing of symphony orchestra musicians. Scand. Audiol. 1983, 12, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.W.; Sherman, R.E.; Aldridge, J.; Lorraine, A. Extended high frequency hearing sensitivity. A normative threshold study in musicians. Ann. Otol. Rhinol. Laryngol. 1986, 95, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Royster, J.D.; Royster, L.H.; Killion, M.C. Sound exposures and hearing thresholds of symphony orchestra musicians. J. Acoust. Soc. Am. 1991, 89, 2793–2803. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Eliasson, A.; Israelsson, B. Hearing in pop/rock musicians: A follow-up study. Ear Hear. 1995, 16, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Obeling, L.; Poulsen, T. Hearing ability in Danish symphony orchestra musicians. Noise Health 1999, 1, 43–49. [Google Scholar] [PubMed]
- Kahari, K.R.; Axelsson, A.; Hellstrom, P.A.; Zachau, G. Hearing development in classical orchestral musicians. A follow-up study. Scand. Audiol. 2001, 30, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Kahari, K.R.; Axelsson, A.; Hellstrom, P.A.; Zachau, G. Hearing assessment of classical orchestral musicians. Scand. Audiol. 2001, 30, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Kaharit, K.; Zachau, G.; Eklof, M.; Sandsjo, L.; Moller, C. Assessment of hearing and hearing disorders in rock/jazz musicians. Int. J. Audiol. 2003, 42, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Amorim, R.B.; Lopes, A.C.; Santos, K.T.P.; Melo, A.D.P.; Lauris, J.R.P. Auditory alterations for Occupational exposition in musician. Int. Arch. Otorhinolaryngol. 2008, 3, 377–383. [Google Scholar]
- Sayegh Ghoussoub, M.; Ghoussoub, K.; Chaaya, A.; Sleilaty, G.; Joubrel, I.; Rifai, K. Orofacial and hearing specific problems among 340 wind instrumentalists in Lebanon. J. Med. Liban. 2008, 56, 159–167. [Google Scholar] [PubMed]
- Jansen, E.J.; Helleman, H.W.; Dreschler, W.A.; de Laat, J.A. Noise induced hearing loss and other hearing complaints among musicians of symphony orchestras. Int. Arch. Occup. Environ. Health 2009, 82, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Hasson, D.; Theorell, T.; Liljeholm-Johansson, Y.; Canlon, B. Psychosocial and physiological correlates of self-reported hearing problems in male and female musicians in symphony orchestras. Int. J. Psychophysiol. 2009, 74, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.L.; Henrich, V.C.; Mace, S.T. Prevalence of noise-induced hearing loss in student musicians. Int. J. Audiol. 2010, 49, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Pawlaczyk-Luszczynska, M.; Dudarewicz, A.; Zamojska, M.; Sliwinska-Kowalska, M. Evaluation of sound exposure and risk of hearing impairment in orchestral musicians. Int. J. Occup. Saf. Ergon. 2011, 17, 255–269. [Google Scholar] [CrossRef] [PubMed]
- Toppila, E.; Koskinen, H.; Pyykko, I. Hearing loss among classical-orchestra musicians. Noise Health 2011, 13, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Samelli, A.G.; Matas, C.G.; Carvallo, R.M.; Gomes, R.F.; de Beija, C.S.; Magliaro, F.C.; Rabelo, C.M. Audiological and electrophysiological assessment of professional pop/rock musicians. Noise Health 2012, 14, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Raymond, D.M., 3rd; Romeo, J.H.; Kumke, K.V. A pilot study of occupational injury and illness experienced by classical musicians. Workplace Health Saf. 2012, 60, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Russo, F.A.; Behar, A.; Chasin, M.; Mosher, S. Hearing loss in British Army musicians. Occup. Med. 2013, 63, 281–283. [Google Scholar] [CrossRef]
- Russo, F.A.; Behar, A.; Chasin, M.; Mosher, S. Noise exposure and hearing loss in classical orchestra musicians. Int. J. Ind. Ergon. 2013, 43, 474–478. [Google Scholar] [CrossRef]
- Goncalves, C.G.; Lacerda, A.B.; Zeigelboim, B.S.; Marques, J.M.; Luders, D. Auditory thresholds among military musicians: Conventional and high frequency. Codas 2013, 25, 181–187. [Google Scholar] [PubMed]
- Wilson, W.J.; O’Brien, I.; Bradley, A.P. The audiological health of horn players. J. Occup. Environ. Hyg. 2013, 10, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Luders, D.; Goncalves, C.G.; Lacerda, A.B.; Ribas, A.; Conto, J. Music students: Conventional hearing thresholds and at high frequencies. Braz. J. Otorhinolaryngol. 2014, 80, 296–304. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, I.; Ackermann, B.J.; Driscoll, T. Hearing and hearing conservation practices among Australia’s professional orchestral musicians. Noise Health 2014, 16, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.H.; Pedersen, E.R.; Paarup, H.M.; Christensen-Dalsgaard, J.; Andersen, T.; Poulsen, T.; Baelum, J. Hearing loss in relation to sound exposure of professional symphony orchestra musicians. Ear Hear. 2014, 35, 448–460. [Google Scholar] [CrossRef] [PubMed]
- Dudarewicz, A.; Pawlaczyk-Luszczynska, M.; Zamojska-Daniszewska, M.; Zaborowski, K. Exposure to excessive sounds during orchestra rehearsals and temporary hearing changes in hearing among musicians. Med. Pr. 2015, 66, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Stormer, C.C.; Laukli, E.; Hoydal, E.H.; Stenklev, N.C. Hearing loss and tinnitus in rock musicians: A Norwegian survey. Noise Health 2015, 17, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Luders, D.; Goncalves, C.G.; Lacerda, A.B.; Silva, L.S.; Marques, J.M.; Sperotto, V.N. Occurrence of tinnitus and other auditory symptoms among musicians playing different instruments. Int. Tinnitus J. 2016, 20, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Henning, R.L.; Bobholz, K. Distortion product otoacoustic emissions in college music majors and nonmusic majors. Noise Health 2016, 18, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Lüders, D.; Gonçalves, C.G.D.O.; Lacerda, A.B.M.D.; Schettini, S.R.L.; Silva, L.S.G.D.; Albizu, E.J.; Marques, J.M. Hearing and quality of life in musicians of a symphony orchestra. Audiol. Commun. Res. 2016, 21, 1688. [Google Scholar]
- Pouryaghoub, G.; Mehrdad, R.; Pourhosein, S. Noise-Induced hearing loss among professional musicians. J. Occup. Health 2017, 59, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Pawlaczyk-Luszczynska, M.; Zamojska-Daniszewska, M.; Dudarewicz, A.; Zaborowski, K. Exposure to excessive sounds and hearing status in academic classical music students. Int. J. Occup. Med. Environ. Health 2017, 30, 55–75. [Google Scholar] [CrossRef] [PubMed]
- Stormer, C.C.L.; Sorlie, T.; Stenklev, N.C. Tinnitus, Anxiety, Depression and Substance Abuse in Rock Musicians a Norwegian Survey. Int. Tinnitus J. 2017, 21, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Szibor, A.; Hyvarinen, P.; Lehtimaki, J.; Pirvola, U.; Ylikoski, M.; Makitie, A.; Aarnisalo, A.; Ylikoski, J. Hearing disorder from music; a neglected dysfunction. Acta Otolaryngol. 2018, 138, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Behar, A.; Chasin, M.; Mosher, S.; Abdoli-Eramaki, M.; Russo, F.A. Noise exposure and hearing loss in classical orchestra musicians: A five-year follow-up. Noise Health 2018, 20, 42–46. [Google Scholar] [CrossRef] [PubMed]
- da Silva, V.G.; de Oliveira, C.A.; Tauil, P.L.; de Castro Silva, I.M.; Sampaio, A.L. Amplified music exposure carries risks to hearing. Int. J. Pediatr. Otorhinolaryngol. 2017, 93, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Saljo, A.; Bao, F.; Hamberger, A.; Haglid, K.G.; Hansson, H.A. Exposure to short-lasting impulse noise causes microglial and astroglial cell activation in the adult rat brain. Pathophysiology 2001, 8, 105–111. [Google Scholar] [CrossRef]
- Tarabichi, O.; Kozin, E.D.; Kanumuri, V.V.; Barber, S.; Ghosh, S.; Sitek, K.R.; Reinshagen, K.; Herrmann, B.; Remenschneider, A.K.; Lee, D.J. Diffusion Tensor Imaging of Central Auditory Pathways in Patients with Sensorineural Hearing Loss: A Systematic Review. Otolaryngol. Head Neck Surg. 2018, 158, 432–442. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Altissimi, G.; Turchetta, R.; Mazzei, F.; Salviati, M.; Cianfrone, F.; Orlando, M.P.; Testugini, V.; Cianfrone, G. Somatosensory Tinnitus: Correlation between Cranio-Cervico-Mandibular Disorder History and Somatic Modulation. Audiol. Neurootol. 2016, 21, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Greco, A.; Turchetta, R.; Altissimi, G.; de Vincentiis, M.; Cianfrone, G. Somatosensory tinnitus: Current evidence and future perspectives. J. Int. Med. Res. 2017, 45, 933–947. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, J.M.; Lin, H.W.; Bhattacharyya, N. Prevalence, Severity, Exposures, and Treatment Patterns of Tinnitus in the United States. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Moller, A.R. Epidemiology of Tinnitus in Adults. In Textbook of Tinnitus; Springer: New York, NY, USA, 2011; pp. 29–37. [Google Scholar]
- Moller, A.R.; Salvi, R.; De Ridder, D.; Kleinjung, T.; Vanneste, S. Pathology of Tinnitus and Hyperacusis-Clinical Implications. Biomed. Res. Int. 2015, 2015, 608437. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.E.; Eggermont, J.J.; Caspary, D.M.; Shore, S.E.; Melcher, J.R.; Kaltenbach, J.A. Ringing ears: The neuroscience of tinnitus. J. Neurosci. 2010, 30, 14972–14979. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.; Zhou, J.; Koehler, S. Neural mechanisms underlying somatic tinnitus. Prog. Brain Res. 2007, 166, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Greco, A.; Boccassini, A.; Altissimi, G.; Di Paolo, C.; Falasca, V.; De Virgilio, A.; Polimeni, A.; Cianfrone, G.; de Vincentiis, M. Subtyping patients with somatic tinnitus: Modulation of tinnitus and history for somatic dysfunction help identify tinnitus patients with temporomandibular joint disorders. PLoS ONE 2018, 13, e0202050. [Google Scholar] [CrossRef] [PubMed]
- Nondahl, D.M.; Cruickshanks, K.J.; Wiley, T.L.; Klein, R.; Klein, B.E.; Tweed, T.S. Prevalence and 5-year incidence of tinnitus among older adults: The epidemiology of hearing loss study. J. Am. Acad. Audiol. 2002, 13, 323–331. [Google Scholar] [PubMed]
- Salvi, R.J.; Wang, J.; Ding, D. Auditory plasticity and hyperactivity following cochlear damage. Hear. Res. 2000, 147, 261–274. [Google Scholar] [CrossRef]
- Baguley, D.M. Hyperacusis. J. R. Soc. Med. 2003, 96, 582–585. [Google Scholar] [CrossRef] [PubMed]
- Staum, M.J.; Brotons, M. The effect of music amplitude on the relaxation response. J. Music Ther. 2000, 37, 22–39. [Google Scholar] [CrossRef] [PubMed]
- Chanda, M.L.; Levitin, D.J. The neurochemistry of music. Trends Cogn. Sci. 2013, 17, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Mockel, M.; Rocker, L.; Stork, T.; Vollert, J.; Danne, O.; Eichstadt, H.; Muller, R.; Hochrein, H. Immediate physiological responses of healthy volunteers to different types of music: Cardiovascular, hormonal and mental changes. Eur. J. Appl. Physiol. Occup. Physiol. 1994, 68, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.; Hoidis, S.; Smolders, J.W. A physiological frequency-position map of the chinchilla cochlea. Hear. Res. 2010, 268, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Henry, K.S.; Kale, S.; Heinz, M.G. Distorted Tonotopic Coding of Temporal Envelope and Fine Structure with Noise-Induced Hearing Loss. J. Neurosci. 2016, 36, 2227–2237. [Google Scholar] [CrossRef] [PubMed]
- Huss, M.; Moore, B.C. Dead regions and pitch perception. J. Acoust. Soc. Am. 2005, 117, 3841–3852. [Google Scholar] [CrossRef] [PubMed]
- Di Stadio, A.; Pegoraro, V.; Giaretta, L.; Dipietro, L.; Marozzo, R.; Angelini, C. Hearing impairment in MELAS: New prospective in clinical use of microRNA, a systematic review. Orphanet J. Rare Dis. 2018, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Fransquet, P.D.; Ryan, J. Micro RNA as a potential blood-based epigenetic biomarker for Alzheimer’s disease. Clin. Biochem. 2018, 58, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Mansoori, B.; Mohammadi, A.; Shirjang, S.; Baradaran, B. Micro-RNAs: The new potential biomarkers in cancer diagnosis, prognosis and cancer therapy. Cell. Mol. Biol. 2015, 61, 1–10. [Google Scholar] [PubMed]
- Patel, M.; Hu, B.H. MicroRNAs in inner ear biology and pathogenesis. Hear. Res. 2012, 287, 6–14. [Google Scholar] [CrossRef] [PubMed]

| Author, Year | Design | Subjects (n) | Age (Range) | Music Genre | Rehearsal Time (hs) | HL (%) | HL (Frequency) | HL (Symmetry) | Tinnitus (%) | Hyperacusis (%) | Diplacusis (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Axelsson, 1978 [33] | PS | 83 | ns | PR | 1:00 | 30% | 3000–6000 Hz | Symmetric | ns | ns | ns |
| Axelsson, 1981 [34] | PS | 38 | 27–33 | PR | 4:30 | 28.9% | 4000–6000 Hz | Symmetric | ns | ns | ns |
| Axelsson, 1981 [35] | PS | 139 | 20–69 | CL | ns | 43.2% | 4000–8000 Hz | Symmetric | ns | ns | ns |
| Karlsson, 1983 [36] | LS | 392 | 20–69 | CL | ns | 25% | 6000–8000 Hz | Asymmetric | ns | ns | ns |
| Johnson, 1986 [37] | CC | 60 | 24–64 | CL | ns | none | ns | ns | ns | ns | ns |
| Royster, 1991 [38] | PS | 59 | 30–69 | CL | 2:30 | 52.5% | 6000 Hz | Asymmetric | ns | ns | ns |
| Axelsson, 1995 [39] | PS | 83 | 20–46 | PR | 3:30 | 10.8% | 3000–6000 Hz | Symmetric | 12% | 9% | ns |
| Obeling, 1999 [40] | PS | 57 | 22–65 | CL | ns | 17.5% | 4000–8000 Hz | Asymmetric | ns | ns | ns |
| Kahari, 2001 [41] | PS | 140 | 23–64 | CL | ns | 52.5% | 6000–8000 Hz | Asymmetric | ns | ns | ns |
| Kahari, 2001 [42] | LS | 56 | 30–50 | CL | ns | 76.8% | 4000–8000 Hz | Symmetric | ns | ns | ns |
| Eaton, 2002 [30] | PS | 53 | 25–60 | CL | 3:00 | 24.5% | 3000-6000 Hz | Symmetric | ns | ns | ns |
| Kahari, 2003 [43] | CSS | 139 | 26–51 | PR | 5:00 | 74.1% | 3000–8000 Hz | Symmetric | 48% | 45% | 2.8% |
| Mendes, 2007 [29] | PS | 34 | ns | PR | ns | 58.8% | 3000–6000 Hz | Symmetric | 47% | ns | ns |
| Beltrao Amorim, 2008 [44] | PS | 30 | 18–40 | PR and CL | 3:50 | 16.7% | 3000–6000 Hz | Symmetric | ns | ns | ns |
| Sayegh, 2008 [45] | PS | 340 | 18–28 | CL | ns | 63.8% | ns | Asymmetric | 28% | ns | ns |
| Jansen, 2009 [46] | PS | 241 | 23–64 | CL | ns | 51.9% | 6000 Hz | Symmetric | 17% | ns | 8.2% |
| Hasson, 2009 [47] | CS | 250 | ns | CL | ns | 6% | ns | ns | 19% | 14% | ns |
| Phillis, 2010 [48] | PS | 329 | 18–25 | PR and CL | 2:00 | 45% | 4000–6000 Hz | Symmetric | ns | ns | ns |
| Pawlaczyk, 2011 [49] | PS | 127 | 22–67 | CL | 4:30 | 26% | 2000–4000 Hz | Symmetric | ns | ns | ns |
| Toppila, 2011 [50] | PS | 63 | 22–52 | CL | ns | 100% | 4000–6000 Hz | Symmetric | 9.5% | 6.3% | ns |
| Samelli, 2012 [51] | CC | 16 | 21–41 | PR | 3:15 | 100% | 2000–3000 Hz | Symmetric | ns | ns | ns |
| Raymond III, 2012 [52] | PS | 32 | 35–64 | CL | ns | 25% | 4000–8000 Hz | Symmetric | ns | ns | ns |
| Patil, 2013 [53] | CC | 84 | 26–47 | CL | ns | none | ns | Symmetric | ns | ns | ns |
| Russo, 2013 [54] | PS | 44 | 41–57 | CL | 4:00 | 100% | 4000–6000 Hz | Symmetric | ns | ns | ns |
| Goncalves, 2013 [55] | CS | 50 | 21–51 | CL | 4:00 | 32% | 2000–16,000 Hz | ns | ns | ns | ns |
| Wilson, 2013 [56] | PS | 144 | 18–60 | CL | 3:15 | 22.9% | 4000–8000 Hz | Symmetric | ns | ns | ns |
| Luders, 2014 [57] | RS | 42 | 18–58 | CL | ns | 7.14% | 250–3000 Hz | Symmetric | ns | ns | ns |
| O’Brien, 2014 [58] | PS | 367 | 35–51 | CL | ns | 42.5% | 2000–8000 Hz | ns | 34% | ns | ns |
| Schmidt, 2014 [59] | CC | 212 | 20–69 | CL | 4:00 | 60.8% | 3000–6000 Hz | Asymmetric | ns | ns | ns |
| Halevi-Katz, 2015 [31] | PS | 44 | 20–64 | PR | 5:15 | 100% | 3000–6000 Hz | Symmetric | 6% | 2% | ns |
| Dudarerewicz, 2015 [60] | PS | 18 | 30–58 | CL | 3:30 | 27.8% | 4000 Hz | ns | ns | ns | ns |
| Stormer, 2015 [61] | CC | 111 | 16–52 | PR | 2:00 | 37.8% | 6000 Hz | Symmetric | 10% | ns | ns |
| Luders, 2016 [62] | PS | 30 | 33–54 | CL | 3:00 | 43.3% | 3000–6000 Hz | Symmetric | 53% | 33% | ns |
| Hennir, 2016 [63] | PS | 28 | 18–25 | CL | 2:00 | 25% | ns | Symmetric | ns | ns | ns |
| Luders, 2016 [64] | PS | 100 | 28–38 | PR and CL | ns | 32% | ns | ns | ns | ns | ns |
| Pouryaghoub, 2017 [65] | CS | 125 | 31–38 | PR and CL | ns | 82.4% | 3000–6000 Hz | Asymmetric | 51.2% | ns | ns |
| Hoydal, 2017 [28] | CC | 111 | 16–52 | PR | ns | 100% | 1500–6000 Hz | Asymmetric | 19.8% | ns | ns |
| Pawlaczyk-Luszczynska, 2017 [66] | CC | 168 | 18–29 | CL | 4:00 | 13.1% | 6000 Hz | Symmetric | 32.1% | 27.4% | ns |
| Stormer, 2017 [67] | CS | 111 | 22–41 | PR | ns | ns | ns | ns | 19.8% | ns | ns |
| Szibor, 2018 [68] | PS | 22 | 18–62 | PR | ns | 95.4% | 6000 Hz | ns | 27.3% | 27.3% | ns |
| Behar, 2018 [69] | LS | 46 | ns | CL | ns | 100% | 4000–8000 Hz | ns | ns | ns | ns |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Stadio, A.; Dipietro, L.; Ricci, G.; Della Volpe, A.; Minni, A.; Greco, A.; De Vincentiis, M.; Ralli, M. Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 2120. https://doi.org/10.3390/ijerph15102120
Di Stadio A, Dipietro L, Ricci G, Della Volpe A, Minni A, Greco A, De Vincentiis M, Ralli M. Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review. International Journal of Environmental Research and Public Health. 2018; 15(10):2120. https://doi.org/10.3390/ijerph15102120
Chicago/Turabian StyleDi Stadio, Arianna, Laura Dipietro, Giampietro Ricci, Antonio Della Volpe, Antonio Minni, Antonio Greco, Marco De Vincentiis, and Massimo Ralli. 2018. "Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review" International Journal of Environmental Research and Public Health 15, no. 10: 2120. https://doi.org/10.3390/ijerph15102120
APA StyleDi Stadio, A., Dipietro, L., Ricci, G., Della Volpe, A., Minni, A., Greco, A., De Vincentiis, M., & Ralli, M. (2018). Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review. International Journal of Environmental Research and Public Health, 15(10), 2120. https://doi.org/10.3390/ijerph15102120









