Identifying Local and Centralized Mental Health Services—The Development of a New Categorizing Variable
Abstract
1. Introduction
- To create a new coding variable for the ESMS-R mapping tree to categorize MHS into local and centralized categories, for the use of developmental activities in different settings globally.
- To test the feasibility of this new variable as a potential quality indicator for MHS, using a Finnish dataset representing a publicly managed Western service.
- We also set out to test whether a quality indicator for MHS could be developed for ESMS-R, based on the hypothesis that when more MHS without gatekeeping are locally available, less centralized services are required.
2. Methods
2.1. The European Service Mapping Schedule-Revised Instrument and Dataset
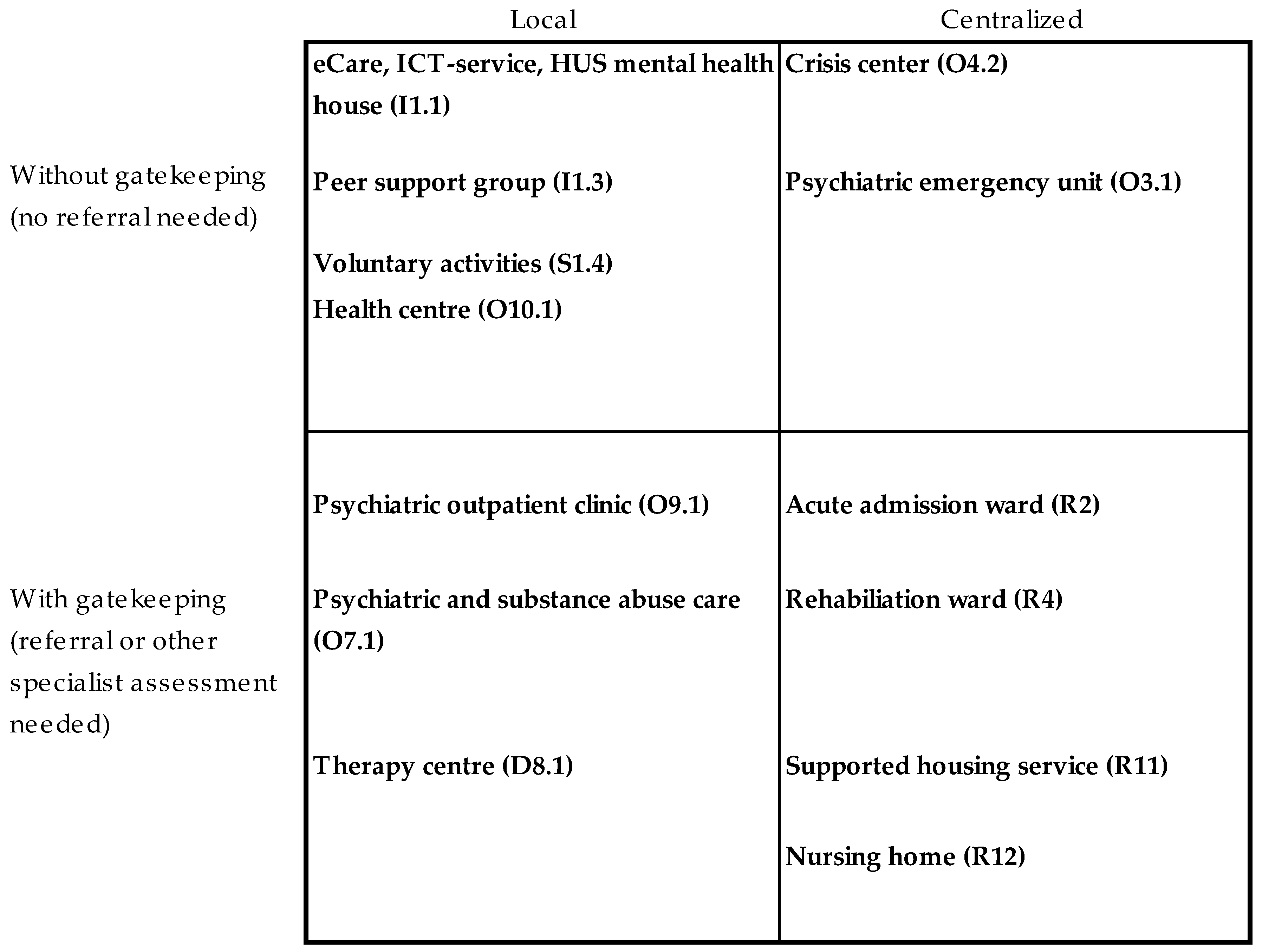
2.2. Creating the New “Local Service” Variable on Local Versus Centralized Services (Part One)
- Phase 1. Two theoretical meetings
- Phase 2. Individual classification (round one)
- Phase 3. Consensus meeting and practical classification
- Phase 4. Individual classification (round two) and final decisions
2.2.1. Phase One: Theoretical Meetings
2.2.2. Phase Two: Individual Classification (Round One)
2.2.3. Phase Three: Consensus Meeting and Preliminary Testing of the Classification
2.2.4 Phase Four: Individual Classification (Round Two) and Final Decisions
2.3. Testing the New European Service Mapping Schedule-Revised-Local Service Variable (Part Two)
- The balance between local and centralized services was explored by comparing:
- (a)
- The proportion of service units classified as local or centralized.
- (b)
- The proportion of resources measured as full-time equivalents allocated to local services.
- The differences in proportion regarding services provided as local without gatekeeping (in BSIC and FTE) between the areas were explored and considered as a quality indicator.
- The types of services provided by public (primary or secondary health care), private, or third sector providers were explored in order to estimate how different types of local or centralized services integrate horizontally and vertically with other health services.
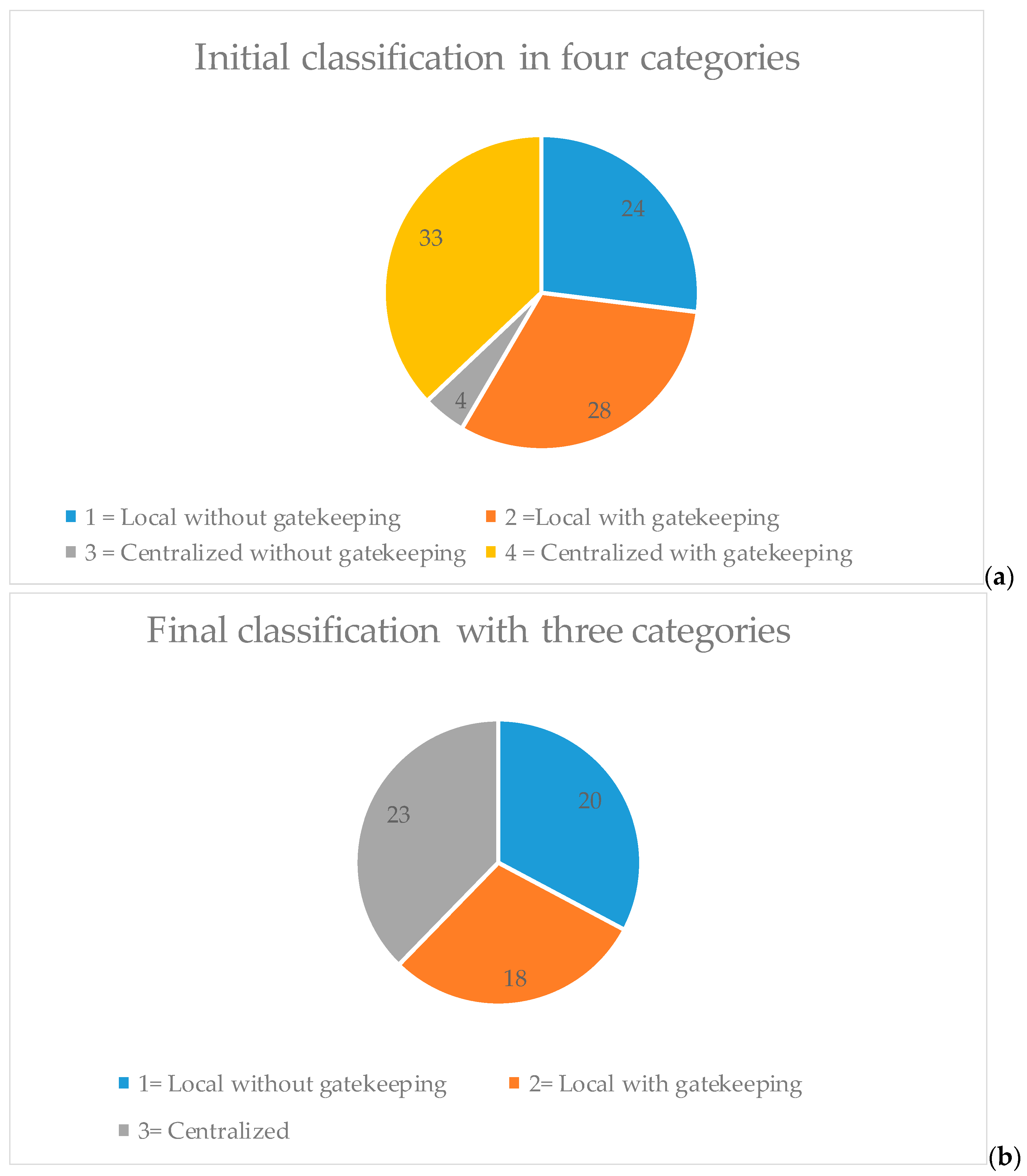
3. Results: Testing the New “Local Service” Variable
3.1. The Balance between Local and Centralized Services
3.2. The Difference between Study Areas in the Proportion of Services Provided as Local Services without Gatekeeping as a Potential Quality Indicator
3.3. The Types of Services Provided by Public or Private Providers, Classified on the Basis of the Level of Horizontal and Vertical Integration with Other Health Services
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Thornicroft, G.; Tansella, M.; Law, A. Steps, challenges and lessons in developing community mental health care. World Psychiatry 2008, 7, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Lora, A.; Cosentino, U.; Gandini, A.; Zocchetti, C. Which community care for patients with schizophrenic disorders? Packages of care provided by Departments of Mental Health in Lombardy (Italy). Epidemiol. Psichiatr. Soc. 2007, 16, 330–338. [Google Scholar] [PubMed]
- Lora, A.; Bai, G.; Bravi, C.; Bezzi, R.; Bulgarini, F.; Mastroeni, A.; Schena, C.; Terzi, A. Patterns of care in community mental health services in Lombardy. Epidemiol. Psichiatr. Soc. 1998, 7, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Lora, A.; Kohn, R.; Levav, I.; McBain, R.; Morris, J.; Saxena, S. Service availability and utilization and treatment gap for schizophrenic disorders: A survey in 50 low- and middle-income countries. Bull. World Health Organ. 2012, 90, 47–54. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Department of Mental Health and Substance Dependence. Mental Health Action Plan 2013–2020; World Health Organization Department of Mental Health and Substance Dependence: Geneva, Switzerland, 2013; Available online: http://www.who.int/mental_health/action_plan_2013/en/ (accessed on 15 May 2018).
- Prince, M.; Patel, V.; Saxena, S.; Maj, M.; Maselko, J.; Phillips, M.R.; Rahman, A. No health without mental health. Lancet 2007, 370, 859–877. [Google Scholar] [CrossRef]
- The World Health Report 2001-Mental Health: New Understanding, New Hope, 2001. Available online: http://www.mentalhealthpromotion.net/?i=portal.en.policydocuments.929 (accessed on 15 May 2018).
- The WHO Mental Health Policy and Service Guidance Package. Mental Health Action Plan 2013–2020. Available online: http://www.who.int/mental_health/policy/essentialpackage1/en/ (accessed on 15 May 2018).
- Thornicroft, G.; Tansella, M. The balanced care model for global mental health. Psychol. Med. 2013, 43, 849–863. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Boyce, N.; Collins, P.Y.; Saxena, S.; Horton, R. A renewed agenda for global mental health. Lancet 2011, 378, 1441–1442. [Google Scholar] [CrossRef]
- Pirkola, S.; Sund, R.; Sailas, E.; Wahlbeck, K. Community mental-health services and suicide rate in Finland: A nationwide small-area analysis. Lancet 2009, 373, 147–153. [Google Scholar] [CrossRef]
- Wahlbeck, K. Public mental health: The time is ripe for translation of evidence into practice. World Psychiatry 2015, 14, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Thielke, S.; Vannoy, S.; Unutzer, J. Integrating mental health and primary care. Prim. Care 2007, 34, 571–592. [Google Scholar] [CrossRef] [PubMed]
- Secker, J.; Hill, K. Broadening the partnerships: Experiences of working across community agencies. J. Interprof. Care 2001, 15, 341–350. [Google Scholar] [PubMed]
- Woltmann, E.; Grogan-Kaylor, A.; Perron, B.; Georges, H.; Kilbourne, A.M.; Bauer, M.S. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: Systematic review and meta-analysis. Am. J. Psychiatry 2012, 169, 790–804. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Carulla, L.; Costa-Font, J.; Cabases, J.; McDaid, D.; Alonso, J. Evaluating mental health care and policy in Spain. J. Ment. Health Policy Econ. 2010, 13, 73–86. [Google Scholar] [PubMed]
- Johnson, S.; Kuhlmann, R.; EPCAT Group. European Psychiatric Assessment Team: The European Service Mapping Schedule (ESMS): Development of an instrument for the description and classification of mental health services. Acta Psychiatr. Scand. Suppl. 2000, 405, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Kilbourne, A.M.; Irmiter, C.; Capobianco, J.; Reynolds, K.; Milner, K.; Barry, K.; Blow, F.C. Improving integrated general medical and mental health services in community-based practices. Adm. Policy Ment. Health 2008, 35, 337–345. [Google Scholar] [CrossRef] [PubMed]
- The Regional Government, Health and Social Services Reform, 2018. Available online: www.stm.fi/sote-uudistushttp://alueuudistus.fi/en/frontpage (accessed on 15 May 2018).
- Partanen, A.; Moring, J.; Nordling, E.; Bergman, V. (Eds.) National Mental Health and Substance Abuse Plan (From Plan to Action); Finnish National Institution for Health: Helsinki, Finland, 2009. [Google Scholar]
- Knapp, M.; Beecham, J.; McDaid, D.; Matosevic, T.; Smith, M. The economic consequences of deinstitutionalisation of mental health services: Lessons from a systematic review of European experience. Health Soc. Care Community 2011, 19, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Goldman, H.H.; Thelander, S.; Westrin, C.G. Organizing mental health services: An evidence-based approach. J. Ment. Health Policy Econ. 2000, 3, 69–75. [Google Scholar] [CrossRef]
- Salvador-Carulla, L.; Amaddeo, F.; Gutierrez-Colosia, M.R.; Salazzari, D.; Gonzalez-Caballero, J.L.; Montagni, I.; Tedeschi, F.; Cetrano, G.; Chevreul, K.; Kalseth, J.; et al. Developing a tool for mapping adult mental health care provision in Europe: The REMAST research protocol and its contribution to better integrated care. Int. J. Integr. Care 2015, 15, e042. [Google Scholar] [CrossRef] [PubMed]
- Ala-Nikkola, T.; Sadeniemi, M.; Kaila, M.; Saarni, S.; Kontio, R.; Pirkola, S.; Joffe, G.; Oranta, O.; Wahlbeck, K. How size matters: Exploring the association between quality of mental health services and catchment area size. BMC Psychiatry 2016, 16, 289. [Google Scholar] [CrossRef] [PubMed]
- Sadeniemi, M.; Pirkola, S.; Pankakoski, M.; Joffe, G.; Kontio, R.; Malin, M.; Ala-Nikkola, T.; Wahlbeck, K. Does primary care mental health resourcing affect the use and costs of secondary psychiatric services? Int. J. Environ. Res. Public Health 2014, 11, 8743–8754. [Google Scholar] [CrossRef] [PubMed]
- Pirkola, S.; Sohlman, B.; Heila, H.; Wahlbeck, K. Reductions in postdischarge suicide after deinstitutionalization and decentralization: A nationwide register study in Finland. Psychiatr. Serv. 2007, 58, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Carulla, L.; Tibaldi, G.; Johnson, S.; Scala, E.; Romero, C.; Munizza, C.; CSRP Group; RIRAG Group. Patterns of mental health service utilisation in Italy and Spain—An investigation using the European Service Mapping Schedule. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Tibaldi, G.; Munizza, C.; Pasian, S.; Johnson, S.; Salvador-Carulla, L.; Zucchi, S.; Cesano, S.; Testa, C.; Scala, E.; Pinciaroli, L. Indicators predicting use of mental health services in Piedmont, Italy. J. Ment. Health Policy Econ. 2005, 8, 95–106. [Google Scholar] [PubMed]
- Rezvyy, G.; Oiesvold, T.; Parniakov, A.; Ponomarev, O.; Lazurko, O.; Olstad, R. The Barents project in psychiatry: A systematic comparative mental health services study between Northern Norway and Archangelsk County. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Carulla, L.; Saldivia, S.; Martinez-Leal, R.; Vicente, B.; Garcia-Alonso, C.; Grandon, P.; Haro, J.M. Meso-level comparison of mental health service availability and use in Chile and Spain. Psychiatr. Serv. 2008, 59, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Okoli, C.; Pawlowski, S.D. The Delphi Method as a research tool: an example, design considerations and applications. Inf. Manag. 2004, 42, 15–29. [Google Scholar] [CrossRef]
- Tuomisto, L.; Erhola, M.; Kaila, M.; Brander, P.E.; Puolijoki, H.; Kauppinen, R.; Koskela, K. Asthma Programme in Finland: High consensus between general practitioners and pulmonologists on the contents of an asthma referral letter. Prim. Care Respir. J. 2004, 13, 205–210. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Campbell, S.M.; Braspenning, J.; Hutchinson, A.; Marshall, M. Research methods used in developing and applying quality indicators in primary care. Qual. Saf. Health Care 2002, 11, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Carulla, L.; Alvarez-Galvez, J.; Romero, C.; Gutierrez-Colosia, M.R.; Weber, G.; McDaid, D.; Dimitrov, H.; Sprah, L.; Kalseth, B.; Tibaldi, G.; et al. Evaluation of an integrated system for classification, assessment and comparison of services for long-term care in Europe: The eDESDE-LTC study. BMC Health Serv. Res. 2013, 13, 218. [Google Scholar] [CrossRef] [PubMed]
- Refinement-Project, 2013. Available online: http://www.refinementproject.eu/ (accessed on 15 May 2018).
- Ala-Nikkola, T.; Pirkola, S.; Kontio, R.; Joffe, G.; Pankakoski, M.; Malin, M.; Sadeniemi, M.; Kaila, M.; Wahlbeck, K. Size matters—Determinants of modern, community-oriented mental health services. Int. J. Environ. Res. Public Health 2014, 11, 8456–8474. [Google Scholar] [CrossRef] [PubMed]
- Thornicroft, G.; Tansella, M. Components of a modern mental health service: A pragmatic balance of community and hospital care: Overview of systematic evidence. Br. J. Psychiatry 2004, 185, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Tello, J.E.; Jones, J.; Bonizzato, P.; Mazzi, M.; Amaddeo, F.; Tansella, M. A census-based socio-economic status (SES) index as a tool to examine the relationship between mental health services use and deprivation. Soc. Sci. Med. 2005, 61, 2096–2105. [Google Scholar] [CrossRef] [PubMed]
- Tucker, C.A.; Escorpizo, R.; Cieza, A.; Lai, J.S.; Stucki, G.; Ustun, T.B.; Kostanjsek, N.; Cella, D.; Forrest, C.B. Mapping the content of the Patient-Reported Outcomes Measurement Information System (PROMIS(R)) using the International Classification of Functioning, Health and Disability. Qual. Life Res. 2014, 23, 2431–2438. [Google Scholar] [CrossRef] [PubMed]
- Madden, R.H.; Dune, T.; Lukersmith, S.; Hartley, S.; Kuipers, P.; Gargett, A.; Llewellyn, G. The relevance of the International Classification of Functioning, Disability and Health (ICF) in monitoring and evaluating Community-based Rehabilitation (CBR). Disabil. Rehabil. 2014, 36, 826–837. [Google Scholar] [CrossRef] [PubMed]
- Prodinger, B.; Cieza, A.; Oberhauser, C.; Bickenbach, J.; Ustun, T.B.; Chatterji, S.; Stucki, G. Toward the International Classification of Functioning, Disability and Health (ICF) Rehabilitation Set: A Minimal Generic Set of Domains for Rehabilitation as a Health Strategy. Arch. Phys. Med. Rehabil. 2016, 97, 875–884. [Google Scholar] [CrossRef] [PubMed]
- WHO Aims 2.0. Available online: http://www.who.int/mental_health/evidence/AIMS_WHO_2_2.pdf (accessed on 15 May 2018).
- Saxena, S.; Lora, A.; Morris, J.; Berrino, A.; Esparza, P.; Barrett, T.; van Ommeren, M.; Saraceno, B. Mental health services in 42 low- and middle-income countries: A WHO-AIMS cross-national analysis. Psychiatr. Serv. 2011, 62, 123–125. [Google Scholar] [CrossRef] [PubMed]
- McPherson, P.; Krotofil, J.; Killaspy, H. What Works? Toward a New Classification System for Mental Health Supported Accommodation Services: The Simple Taxonomy for Supported Accommodation (STAX-SA). Int. J. Environ. Res. Public Health 2018, 15, 190. [Google Scholar] [CrossRef] [PubMed]
- De Silva, M.J.; Lee, L.; Fuhr, D.C.; Rathod, S.; Chisholm, D.; Schellenberg, J.; Patel, V. Estimating the coverage of mental health programmes: A systematic review. Int. J. Epidemiol. 2014, 43, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Brieger, P.; Wetzig, F.; Bocker, F.M. Institutions and services of psychiatric care in Saxony-Anhalt: Assessment with the European Services Mapping Schedule. Eur. Psychiatry 2003, 18, 145–147. [Google Scholar] [CrossRef]
| ESMS-R Main Branch | Local Services Without Gatekeeping | Local Services With Gatekeeping | Centralized Services | BSIC Found n (%) | Different MTC Found/Possible * |
|---|---|---|---|---|---|
| Information for care | 7 | 2 | 0 | 22 (2) | 6/9 |
| Accessibility for care | 3 | 2 | 0 | 6 (1) | 1/5 |
| Self-help and voluntary care | 7 | 1 | 2 | 191 (19) | 6/10 |
| Outpatient care | 3 | 19 | 2 | 279 (28) | 17/24 |
| Day care | 4 | 6 | 12 | 157 (16) | 17/22 |
| Residential care | 0 | 0 | 19 | 331 (34)) | 14/19 |
| Different BSIC found n (%) | 367 (37.2) | 213 (21.6) | 406 (41.2) | 986 | |
| Different MTC found / possible * | 20/24 | 18/30 | 23/35 | 61/89 | |
| Percentage of personnel ** (%) | 11 | 22 | 67 |
| Catchment Areas * | Länsi-Uusi-Maa | Lohja | Hyvin-Kää | Porvoo | Helsinki | Jorvi | Peijas | Kymen-Laakso | Eksote | Turku | Salo | Vakka-Suomi | Turun-Maa | Sum | Weighted Average | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental health index (Finland = 100) | 92.3 | 94 | 92.9 | 89 | 90 | 77.2 | 89.6 | 106.2 | 102.7 | 109.7 | 101 | 102.9 | 101.3 | 96 | 8.9 | |
| Size of catchment areas adult (18+) population (2012) | 35,296 | 70,379 | 139,734 | 74,611 | 501,929 | 230,005 | 187,332 | 143,265 | 109,379 | 151,616 | 128,039 | 81,392 | 18,200 | 1,871,178 | 128,000 (median) | 122,759 |
| Total personell (FTE) | ||||||||||||||||
| Total personnel FTE per 1000 | 3.64 | 4.10 | 2.8827 | 3.10 | 4.01 | 2.80 | 3.46 | 4.17 | 2.98 | 4.82 | 3.31 | 3.67 | 2.93 | 3.63 | 0.61 | |
| a) Providers status | ||||||||||||||||
| Public personnel FTE per 1000 | 2.58 | 2.43 | 1.9642 | 1.52 | 2.69 | 2.06 | 2.51 | 2.38 | 2.43 | 2.58 | 2.03 | 1.87 | 1.94 | 2.35 | 0.35 | |
| Third sector personnel FTE per 1000 | 0.19 | 0.43 | 0.3766 | 0.97 | 1.26 | 0.38 | 0.39 | 1.11 | 0.14 | 0.95 | 0.59 | 0.18 | 0.00 | 0.73 | 0.40 | |
| Private company personnel FTE per 1000 | 0.87 | 1.24 | 0.5419 | 0.61 | 0.05 | 0.36 | 0.56 | 0.68 | 0.41 | 1.29 | 0.69 | 1.62 | 0.99 | 0.55 | 0.43 | |
| b) Organizational level | 6784.72 | 3.62 | ||||||||||||||
| Primary health care personnel FTE per 1000 | 0.59 | 1.31 | 1.3203 | 1.14 | 1.28 | 2.05 | 2.04 | 0.72 | 0.23 | 3.22 | 1.90 | 1.85 | 0.28 | |||
| Primary healthcare personnel FTE per 1000 | 2.14 | 2.24 | 1.2661 | 1.92 | 1.87 | 1.30 | 1.78 | 2.37 | 1.01 | 2.51 | 1.98 | 2.37 | 1.22 | 1.83 | 0.49 | |
| Secondary healthcare personnel FTE per 1000 | 1.50 | 1.87 | 1.6165 | 1.17 | 2.14 | 1.50 | 1.68 | 1.80 | 0.18 | 2.31 | 1.33 | 1.30 | 1.71 | 1.69 | 0.52 | |
| Integrate primary and secondary healthcare personnel FTE per 1000 | 1.79 | 195.61 | ||||||||||||||
| c) Local vs centralized service level | ||||||||||||||||
| Local without gatekeeping FTE per 1000 | 0.51 | 0.33 | 0.4835 | 0.20 | 0.22 | 0.17 | 0.37 | 0.06 | 0.25 | 0.92 | 1.01 | 0.71 | 0.77 | 0.46 | 0.30 | |
| Local with gatekeeping FTE per 1000 | 0.46 | 0.90 | 0.6343 | 0.44 | 1.07 | 0.80 | 0.97 | 1.05 | 0.78 | 0.78 | 0.41 | 0.29 | 0.00 | 0.66 | 0.32 | |
| Total local resources (without and with gatekeeping) per 1000 | 0.97 | 1.23 | 1.1178 | 0.64 | 1.29 | 0.97 | 1.33 | 1.11 | 1.03 | 1.70 | 1.41 | 1.00 | 0.77 | 1.12 | ||
| Centralized FTE per 1000 | 2.67 | 2.87 | 1.7648 | 2.45 | 2.72 | 1.83 | 2.12 | 3.06 | 1.95 | 3.12 | 1.89 | 2.67 | 2.17 | 2.40 | 0.48 | |
| Relation of local resources | ||||||||||||||||
| % of local without gatekeeping FTE from total local FTE (per 1000) | 53% | 27% | 0.4325 | 0.32 | 0.17 | 0.18 | 0.28 | 0.05 | 0.24 | 0.54 | 0.71 | 0.71 | 1.00 | 0.41 | ||
| % of local FTE from total resources (per 1000) | 27% | 30% | 0.3878 | 0.21 | 0.32 | 0.35 | 0.39 | 0.27 | 0.34 | 0.35 | 0.43 | 0.27 | 0.26 | 0.31 |
| Spearman‘s Rho (N = 13 Catchment Area) | Total Local Personnel | Local Without Gatekeeping Personnel | Local with Gatekeeping Personnel | Centralized Personnel | |
|---|---|---|---|---|---|
| Total personnel | Correlation Coefficient | 0.063 | 0.058 | 0.408 | 0.911 ** |
| Sig. (2-tailed) | 0.838 | 0.851 | 0.167 | 0.000 | |
| Total local personnel | Correlation Coefficient | 0.960 ** | −0.538 | −0.056 | |
| Sig. (2-tailed) | 0.000 | 0.058 | 0.856 | ||
| Local without gatekeeping personnel | Correlation Coefficient | −0.635 * | −0.044 | ||
| Sig. (2-tailed) | 0.020 | 0.887 | |||
| Local with gatekeeping personnel | Correlation Coefficient | 0.300 | |||
| Sig. (2-tailed) | 0.320 | ||||
| Proportion of Local vs Centralized Services | Sum (BSIC) | BSIC % | Sum FTE/1000 18+ | FTE % | |
|---|---|---|---|---|---|
| a) Provider status (N = 985) | |||||
| Third sector (n = 450) | Local without gatekeeping | 244 | 54.2% | ||
| Local with gatekeeping | 70 | 15.6% | |||
| Centralized | 136 | 30.2% | |||
| Sum | 450 | 100% | 0.73 | 20.1% | |
| Public (n = 416) | Local without gatekeeping | 122 | 29.3% | ||
| Local with gatekeeping | 129 | 31.0% | |||
| Centralized | 165 | 39.7% | |||
| Sum | 416 | 100% | 2.35 | 64.7% | |
| Private (n = 119) | Local without gatekeeping | 1 | 0.8% | ||
| Local with gatekeeping | 14 | 11.8% | |||
| Centralized | 104 | 87.4% | |||
| Sum | 119 | 100% | 0.55 | 15.2% | |
| b) Organizational level (N = 985) | |||||
| Local without gatekeeping | 20 | 10.5% | |||
| Primary care (n = 193) | Local with gatekeeping | 76 | 39.8% | ||
| Centralized | 95 | 49.7% | |||
| Sum | 191 | 100% | 1.83 | 50.4% | |
| Secondary health care (n = 769) | Local without gatekeeping | 337 | 43.8% | ||
| Local with gatekeeping | 130 | 16.9% | |||
| Centralized | 302 | 39.3% | |||
| Sum | 769 | 100% | 1.69 | 46.6% | |
| Integrated health and social care (n = 25) | Local without gatekeeping | 10 | 40.0% | ||
| Local with gatekeeping | 7 | 28.0% | |||
| Centralized | 8 | 32.0% | |||
| Sum | 25 | 100% | 0.10 | 2.8% | |
| Total Sum by provider status | Local without gatekeeping | 367 | 37.3% | 0.46 | 11.0% |
| Local with gatekeeping | 213 | 21.6% | 0.66 | 22.0% | |
| Centralized | 405 | 41.1% | 2.40 | 67.0% | |
| Total Sum N = 985 | Sum | 985 | 100% | 3.63 | 100% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ala-Nikkola, T.; Pirkola, S.; Kaila, M.; Joffe, G.; Kontio, R.; Oranta, O.; Sadeniemi, M.; Wahlbeck, K.; Saarni, S.I. Identifying Local and Centralized Mental Health Services—The Development of a New Categorizing Variable. Int. J. Environ. Res. Public Health 2018, 15, 1131. https://doi.org/10.3390/ijerph15061131
Ala-Nikkola T, Pirkola S, Kaila M, Joffe G, Kontio R, Oranta O, Sadeniemi M, Wahlbeck K, Saarni SI. Identifying Local and Centralized Mental Health Services—The Development of a New Categorizing Variable. International Journal of Environmental Research and Public Health. 2018; 15(6):1131. https://doi.org/10.3390/ijerph15061131
Chicago/Turabian StyleAla-Nikkola, Taina, Sami Pirkola, Minna Kaila, Grigori Joffe, Raija Kontio, Olli Oranta, Minna Sadeniemi, Kristian Wahlbeck, and Samuli I. Saarni. 2018. "Identifying Local and Centralized Mental Health Services—The Development of a New Categorizing Variable" International Journal of Environmental Research and Public Health 15, no. 6: 1131. https://doi.org/10.3390/ijerph15061131
APA StyleAla-Nikkola, T., Pirkola, S., Kaila, M., Joffe, G., Kontio, R., Oranta, O., Sadeniemi, M., Wahlbeck, K., & Saarni, S. I. (2018). Identifying Local and Centralized Mental Health Services—The Development of a New Categorizing Variable. International Journal of Environmental Research and Public Health, 15(6), 1131. https://doi.org/10.3390/ijerph15061131





